Deficient Attentional Modulation of the Startle Response in Patients With Schizotypal Personality Disorder
Abstract
OBJECTIVE: Attentional deficits have been identified as an abnormality that individuals with schizotypal personality disorder share with schizophrenia patients. The purpose of this study was to examine automatic sensorimotor gating and controlled attentional modulation of the startle eye blink response in unmedicated subjects with schizotypal personality disorder. METHOD: Eighteen unmedicated patients with schizotypal personality disorder and 16 healthy individuals were assessed in an acoustic attention-to-prepulse paradigm. The participants performed a selective attention task involving the presentation of attended, ignored, and novel tones that served as prepulse tones. Acoustic startle probes were presented at short and long lead intervals after the onset of tones and occasionally during the intertone interval. RESULTS: The comparison subjects showed greater prepulse inhibition and prepulse facilitation during the attended than the ignored prepulses, demonstrating early and later attentional modulation of startle eye blink response. In contrast, the subjects with schizotypal personality disorder failed to show this pattern. CONCLUSIONS: Subjects with schizotypal personality disorder have deficits in controlled attentional processing, as indexed by modification of the startle eye blink response, that are similar to those observed in patients with schizophrenia.
Studying schizotypal personality disorder is important, not only in furthering our understanding of this personality disorder but also in providing key insights into our understanding of schizophrenia. Research into schizotypal personality disorder is of key importance in overcoming methodological weaknesses of schizophrenia research (1). For example, psychotic symptoms may mask the more subtle cognitive impairments underlying the schizophrenia spectrum, and they also create difficulty in ensuring that schizophrenia patients fully understand and comply with the experimental protocol. Individuals with schizotypal personality disorder may have some genetic vulnerability for schizophrenia, but they do not have many of the confounding variables (medication effects, chronic illness, and multiple hospitalizations) seen in schizophrenia patients, making them a unique study population (2).
Psychophysiological research using modification of the startle eye blink response indicates that schizophrenia patients and putatively psychosis-prone individuals have deficient controlled attentional processing (3–6). In the startle eye blink modification paradigm, the startle eye blink is reliably modified in humans and other species by presenting a nonstartling stimulus (prepulse tone) shortly before a startling stimulus (7). When the lead interval between the onset of the prepulse tone and the onset of the startle stimulus is short, approximately 250 msec or less, the magnitude of the startle eye blink response is reduced compared with the eye blink elicited by the startle stimulus alone. This short-lead-interval prepulse inhibition is thought to reflect the action of an automatic sensorimotor gating system that is protective of early preattentive processing of the prepulse (7, 8). In contrast, if a nonstartling prepulse tone precedes the startle stimulus by a long interval (e.g., 2000–4500 msec), the startle eye blink reflex is often enhanced (termed “prepulse facilitation”) (9). Prepulse facilitation is thought to reflect a combination of arousal and sustained attention elicited by the prepulse. Therefore, prepulse inhibition and prepulse facilitation represent two different neurocognitive processes (7, 10).
Both prepulse inhibition and prepulse facilitation have been shown to be modulated by attention to the prepulse tone in normal individuals (10). We and others have reported that schizophrenia patients (3–5) and putatively psychosis-prone individuals (6) exhibit deficient attentional modulation of both prepulse inhibition and prepulse facilitation. In an attention-to-prepulse paradigm, subjects were instructed to attend to one type of prepulse (e.g., a high-pitched tone) and to ignore the other prepulse types. In each of these studies, the normal subjects showed significantly greater prepulse inhibition after the attended prepulse tones than the ignored prepulses only at the 120-msec lead interval. They showed greater prepulse facilitation after the attended prepulses than the ignored prepulses at long lead intervals (2000–4500 msec), suggesting that the attention-to-prepulse paradigm taps time-locked attentional processes in normal subjects. In contrast, the patients and putatively at-risk individuals in these studies failed to show this pattern of differential prepulse inhibition and prepulse facilitation during the attended and ignored prepulses, suggesting an impairment in controlled cognitive processing.
Previous work has also shown that schizophrenia patients (8), patients with schizotypal personality disorder (11, 12), and college students putatively at-risk for psychosis (13) exhibited impaired prepulse inhibition to a passively attended prepulse. Impaired prepulse inhibition during passive attention paradigms has been interpreted as reflecting an impairment in automatic, preattentive sensorimotor gating relevant to the vulnerability to schizophrenia (8). However, to our knowledge, controlled attentional modulation of startle eye blink modification has not previously been examined in subjects with schizotypal personality disorder.
The goal of the present study was to examine prepulse inhibition and prepulse facilitation in subjects with schizotypal personality disorder during an active auditory selective attention task, which has previously revealed controlled attentional impairments in patients with relatively remitted schizophrenia (3, 4) and in patients with unmedicated schizophrenia (5). Use of the active attention task would allow us to determine whether anomalies in prepulse inhibition in subjects with schizotypal personality disorder are limited to automatic attentional processing deficits and/or whether controlled attentional processing deficits exist (10).
On the basis of previous startle eye blink modification research in schizophrenia patients, we made the following hypotheses: 1) subjects with schizotypal personality disorder will exhibit deficient early and later attentional modulation of prepulse inhibition, suggesting abnormal controlled attentional processing, 2) subjects with schizotypal personality disorder will exhibit normal prepulse inhibition during the ignored prepulse, suggesting that automatic processing during an active attention task is intact.
Method
Participants
Eighteen unmedicated individuals with schizotypal personality disorder (14 men and four women, mean age=43.3 years, SD=10.9; mean education=14.1 years, SD=2.7; 11 never medicated, seven received no psychotropic medications during the past year) were recruited from advertisements. These individuals met DSM-III-R and DSM-IV diagnostic criteria on the basis of interviews from the Schedule for Schizophrenia and Affective Disorders (14) and the Structured Interview for DSM-III-R Personality Disorders (15).
Sixteen healthy volunteers (12 men and four women; mean age=41.3 years, SD=12.2; mean education=17.1 years, SD=2.5) were recruited by advertisement and evaluated for pathology with the Comprehensive Assessment of Symptoms and History (16) to exclude psychiatric illness in themselves and their first-degree relatives and the Structured Interview for DSM-III-R Personality Disorders, which was modified for administration to normal comparison subjects to screen out those with personality disorders.
A medical history, results of a physical examination, and laboratory test results were obtained for all participants. Individuals with a history of substance abuse in the previous 6 months or any history of substance dependence, neurological disorders, or head trauma were excluded. All participants provided written informed consent and were paid for their participation.
Procedure
The experimental methods for the startle eye blink modification paradigm employed in the present study were identical to those employed in our previous study with schizophrenia patients (5) and are briefly summarized here. The participants were instructed that their task was to listen closely to a series of high- and low-pitched tones presented through headphones, to count silently the number of long high-pitched tones, and to ignore the low-pitched tones (attended pitch was counterbalanced). The participants were 1) told that the standard tone was 5 seconds in duration and that the longer tone was 8 seconds in duration, 2) told that a brief noise would be presented occasionally throughout the task but that it was unrelated to the task and should be ignored, and 3) not given any instructions about the novel tone. To emphasize the importance of the task, a monetary reward ($10.00) was offered for a correct count of the longer-than-usual tones of the designated pitch.
After the instructions, a 3-minute resting baseline startle response level was recorded, at the end of which the participants were given three presentations of the noise burst alone to calibrate eye blink amplitude in microvolts. One example of the high tone and one example of the low tone was then presented; the participants were told that each of these examples was the standard 5 seconds in duration. All participants confirmed that they could discriminate between the high and low tones.
The main portion of the experiment consisted of a 32-minute startle paradigm that involved 52 tone trials: 22 high tones, 22 low tones, and eight novel tones in a mixed, fixed semirandom order, with intertone intervals of 29–39 seconds (mean=34). Of the 22 high or low tones, 12 included the startle-eliciting stimulus. Of the 12 trials, there were four presentations of the noise burst at each of three lead intervals: 120 msec, 240 msec, and 4500 msec. The remaining 10 trials without a noise burst were intermixed. There were eight presentations of the novel tone, with four presentations of the noise burst at each of two lead intervals: 120 msec and 4500 msec.
In addition to the noise burst being presented at critical lead intervals, it was also presented at preselected times during 30 of the intertone intervals to provide a baseline measurement of startle amplitude.
Experimental Stimuli
The startle-eliciting stimulus was a 104 dB SPL(A) white noise burst of 40 msec in duration with a near-instantaneous (<1 msec) rise/fall time. The attended and ignored prepulses consisted of 70 dB SPL(A) 800-Hz and 1200-Hz tones that were 5 or 8 seconds in duration. The novel prepulse was a 70 dB SPL(A) 500-Hz tone of 5 seconds in duration.
Physiological Recording and Scoring
Startle eye blink responses were measured and scored as described in our previous study with schizophrenia patients (5). Startle eye blink amplitude scores were converted to microvolts, and differences were then computed between the mean baseline intertone interval eye blink amplitude and the intratone eye blink amplitudes. Because the difference scores given in microvolts were correlated with baseline startle eye blink amplitude, the difference scores were converted to percentage change units, which removed dependence on baseline measures for the present data.
Results
Short-Lead-Interval Prepulse Inhibition
Figure 1 shows the mean startle eye blink modification scores for the healthy comparison subjects, the patients with schizotypal personality disorder, and the patients with schizophrenia for the attended, ignored, and novel prepulse tones at the 120-msec lead interval.
To determine whether differential startle eye blink modification occurred at the short lead intervals, a series of analyses of variance (ANOVAs) was performed. An orthogonal set of individual planned comparisons was then performed to determine for each group at which lead intervals differential startle eye blink modification had occurred. We performed a two (group: comparison versus schizotypal personality disorder)-by-three (prepulse type: attended, ignored, novel) ANOVA that resulted in a significant group-by-prepulse type interaction, indicating that the subjects with schizotypal personality disorder differed significantly from the comparison subjects in their pattern of prepulse inhibition during the attended, ignored, and novel prepulses at the 120-msec lead interval (F=9.76, df=2, 64, p<0.01). However, there was no main effect of group, indicating that the schizotypal personality disorder group did not differ from the healthy comparison subjects in overall prepulse inhibition.
Differences in startle eye blink modification between attended and ignored prepulses at the 120-msec lead interval provided an estimate of early predominantly controlled attentional modulation of the startle eye blink response (3). To evaluate controlled attentional processing, we performed a two (group)-by-two (prepulse: attended, ignored) ANOVA on the startle eye blink modification scores at the 120-msec lead interval. Consistent with our previous schizophrenia findings (3–5), this analysis revealed a significant group-by-prepulse interaction (F=26.27, df=1, 32, p<0.01). Follow-up simple effects tests confirmed that the comparison group showed significantly greater prepulse inhibition during the attended prepulse than during the ignored prepulse (F=61.99, df=1, 15, p<0.01), consistent with our previous findings in healthy subjects (3–6). In contrast, the subjects with schizotypal personality disorder failed to show differential inhibition of the startle eye blink response at the 120-msec lead interval (p=0.22, simple effects test). To confirm this interpretation, we examined between-group difference scores at the 120-msec lead interval. The group with schizotypal personality disorder exhibited significantly less differential prepulse inhibition than the comparison group at the 120-msec lead interval during the attended and ignored prepulses (t=5.13, df=32, p<0.01).
There was neither a group main effect nor an interaction effect, indicating that the subjects with schizotypal personality disorder did not differ from the comparison subjects in prepulse inhibition following the attended and ignored prepulses at the 240-msec lead interval.
Long-Lead-Interval Prepulse Facilitation
The startle eye blink modification scores for the 4500-msec lead interval were subjected to a two (group)-by-three (prepulse type: attended, ignored, novel) ANOVA (Figure 1), which revealed a significant group-by-prepulse type interaction (F=6.16, df=2, 64, p=0.01). This interaction indicated that the subjects with schizotypal personality disorder differed from the healthy comparison subjects in their prepulse facilitation pattern during the attended, ignored, and novel prepulses at the 4500-msec lead interval. However, there was no group main effect, indicating that the group with schizotypal personality disorder did not differ from the comparison subjects in overall prepulse facilitation.
Differences in startle eye blink modification between the attended and ignored prepulses at the 4500-msec lead interval should provide an estimate of late predominantly controlled attentional modulation of startle eye blink response during the attended prepulse tones. To evaluate whether the subjects with schizotypal personality disorder exhibited abnormal controlled attentional modulation of startle response at the 4500-msec lead interval, we performed a two (group)-by-two (prepulse: attended, ignored) ANOVA on the startle eye blink modification scores. This analysis revealed a significant group-by-prepulse type interaction (F=11.07, df=1, 32, p<0.01), reflecting group differences in differential prepulse facilitation during the attended and ignored prepulses. An orthogonal set of individual planned comparisons confirmed that the normal comparison group showed significantly greater prepulse facilitation during the attended prepulse than during the ignored prepulse tones (F=24.95, df=1, 15, p<0.01), consistent with previous findings (3–6). In contrast, the subjects with schizotypal personality disorder failed to show differential prepulse facilitation at the 4500-msec lead interval during the attended and ignored prepulses. To confirm this, we examined between-group difference scores at the 4500-msec lead interval. This analysis also demonstrated that the group with schizotypal personality disorder exhibited significantly less differential prepulse facilitation during the attended and ignored prepulses than did the comparison group (t=3.33, df=32, p<0.01).
Startle Eye Blink Modification During Novel Prepulse Tones
To evaluate whether the subjects with schizotypal personality disorder exhibited abnormal controlled attentional processing resources during the novel prepulse tones, we performed a two (group)-by-two (prepulse type: novel, ignored) ANOVA on prepulse inhibition at the 120-msec lead interval and on prepulse facilitation at the 4500-msec lead interval. Similar to the analysis conducted for the attended prepulse, differences in startle eye blink modification between the novel and the ignored prepulses at the 120-msec lead interval should provide an estimate of early predominantly controlled attentional modulation of the startle eye blink response during the novel prepulses.
At the 120-msec lead interval, the main effect of group was not significant; however, there was a significant group-by-prepulse type interaction (F=4.94, df=1, 32, p=0.03), indicating that the comparison subjects showed greater prepulse inhibition during the novel prepulse tones than during the ignored prepulses, while the subjects with schizotypal personality disorder showed the opposite pattern (Figure 1). Simple effects tests confirmed that the healthy comparison group exhibited significantly greater prepulse inhibition at the 120-msec lead interval during the novel prepulses than the ignored prepulse tones (F=7.85, df=1, 15, p=0.01). In contrast, the subjects with schizotypal personality disorder did not show differential prepulse inhibition during the novel and ignored prepulses at the 120-msec lead interval. Analysis of between-group difference scores at the 120-msec lead interval demonstrated that the patients with schizotypal personality disorder exhibited significantly less differential prepulse facilitation during the novel and ignored prepulse tones than did the comparison group (t=2.22, df=32, p=0.03).
At the 4500-msec lead interval, neither the main effect of group nor the group-by-prepulse type interaction reached significance (p=0.62, simple effects test), indicating that neither group exhibited differential prepulse facilitation during the novel and ignored prepulses.
Startle Eye Blink Modification During Ignored Prepulse Tones
Startle eye blink modification scores during the ignored prepulses were examined with a two (group)-by-two (lead interval: 120 msec, 240 msec) ANOVA. The main effect of group was not significant, however, there was a significant group-by-lead interval interaction (F=6.13, df=1, 32, p=0.02). This interaction effect indicated that the comparison subjects exhibited greater prepulse inhibition at the 240-msec than the 120-msec lead interval while the subjects with schizotypal personality disorder showed the opposite pattern. However, simple effects tests conducted for each of the early probe positions separately failed to confirm significant group differences for prepulse inhibition during the ignored prepulses at each lead interval time. There was no difference between the groups in prepulse facilitation at the 4500-msec lead interval during the ignored prepulses.
Baseline Startle Eye Blink
Analysis of the mean startle eye blink amplitude during the intertone interval showed no significant between-group difference (comparison subjects: mean=80.97 μV, SD=53.90; patients with schizotypal personality disorder: mean=83.00 μV, SD=51.07) (t=0.11, df=32, p=0.91).
Performance on Tone-Length Judgment Task
For each participant, we recorded the accuracy of the count made of the longer (i.e., 8-second versus 5-second) attended prepulse tones to determine if there were differences among the groups in the motivation or ability to perform this selective attention task. The average error score for the subjects with schizotypal personality disorder did not differ from that of the comparison group (comparison subjects: mean=1.4 errors, SD=3.5, range=0–14; subjects with schizotypal personality disorder: mean=2.5 errors, SD=3.6, range=0–14) (H=3.56, df=1, p=0.06, Kruskal-Wallis nonparametric test).
Discussion
The present findings among subjects with schizotypal personality disorder indicate that their impairments in the attentional modulation of prepulse inhibition and prepulse facilitation bear a striking resemblance to those previously reported in schizophrenia patients (3–5). The schizotypal personality disorder and schizophrenia groups both failed to show attentional modulation of early inhibition at 120 msec or later facilitation. This similarity between the startle modification deficits of subjects with schizotypal personality disorder and those of schizophrenia patients suggests that the two groups share common dysfunctions in controlled modulation of sensory stimuli, which may constitute a trait-like vulnerability factor related to schizophrenia disorders (17).
The present startle eye blink modification findings in subjects with schizotypal personality disorder are also similar to those found in individuals putatively at risk for psychosis studied by Schell and coworkers (6). Their at-risk group was identified by use of the Chapman scales for physical anhedonia, perceptual aberrations, and magical ideation. These scales identify subjects who demonstrate behaviors and experiences similar to those of schizophrenia patients and who have a greater likelihood of future diagnosis of psychosis, although not necessarily schizophrenia (18, 19). Similar to the subjects with schizotypal personality disorder in the current study, Schell et al. (6) reported that both the perceptual aberration–magical ideation and anhedonia groups failed to exhibit attentional modulation of prepulse inhibition at the 120-msec lead interval compared to age- and sex-matched college students. At the long lead interval, which is thought to reflect sustained attentional processes, the perceptual aberration–magical ideation group failed to show enhancement of long-lead-interval facilitation during the attended prepulses. The subjects with anhedonia required more trials before the development of attentional modulation of prepulse facilitation appeared. Taken together, the findings of similar attentional modulation deficits in prepulse inhibition and prepulse facilitation in individuals putatively at risk for psychosis, schizotypal personality disorder, and schizophrenia support the use of startle response as a potential biological marker in studies of schizophrenia spectrum disorders (20). The pattern of abnormal attentional modulation of startle eye blink modification that we reported here in subjects with schizotypal personality disorder and previously in individuals putatively at risk for psychosis (6) lend support to the idea that persons demonstrating a large number of schizotypal personality traits may have an underlying neurobiological dysfunction similar to schizophrenia. The fact that startle eye blink modification abnormalities are present in the normal population in subjects with high schizotypal traits, as measured by psychometric scales, as well as in individuals diagnosed with schizotypal personality disorder indicates the varying degrees to which the symptoms of schizophrenia may be expressed.
In the present study, the group with schizotypal personality disorder did not differ from the comparison subjects at any lead interval in inhibition or facilitation during the to-be-ignored prepulses, suggesting that automatic processing affecting prepulse inhibition and prepulse facilitation appears to be normal in schizotypal personality disorder in the context of this attention-to-prepulse paradigm. This finding seems contrary to the previous findings of Cadenhead et al. (11, 12) in subjects with schizotypal personality disorder. However, it must be noted that our paradigm differs from the so-called passive attention paradigm because sufficient attention must be allocated to the to-be-ignored prepulse to identify it as the irrelevant stimulus. Thus, the difference between our results and those of Cadenhead et al. is likely due to the type of attentional task employed. The tasks that have provided evidence suggesting a deficit in automatic processing have been passive attention tasks, whereas those that have suggested deficits in controlled processing have been active selective attention tasks that are more demanding of the outlay of processing resources. In our patients with schizotypal personality disorder and our patients with schizophrenia, the additional effort and activation demanded to perform a selective attention task may normalize the operation of the purely automatic aspects of the sensory gating process, while leaving a deficit in the modulation of that process by higher-level (cortical) brain regions. This concept is supported by our previous [18F]fluorodeoxyglucose positron emission tomography finding that among healthy individuals, greater prepulse inhibition during attended prepulse tones is significantly correlated with higher relative glucose metabolism in medial and lateral prefrontal cortex regions (5). In contrast, schizophrenia patients showed this relationship only in a much smaller portion of the prefrontal cortex (left Brodmann’s area 10). Work in single photon emission computer tomography has also shown that in relation to comparison subjects, subjects with schizotypal personality disorder showed abnormal patterns of prefrontal activation (21).
The schizotypal personality disorder and comparison groups did not differ significantly in behavioral performance on the tone-length judgment task. Thus, deficient attentional modulation of startle eye blink modification task was exhibited by some subjects with schizotypal personality disorder whose task performance was normal. In previous schizophrenia studies (3–5), patients exhibited both behavioral and startle eye blink modification abnormalities in relation to healthy comparison subjects. Yet, consistent with the present study, startle eye blink modification impairments were found even in subgroups of schizophrenia patients who performed well on the task. These findings suggest that the failures to attentionally modulate startle eye blink are more sensitive to subtle psychopathology than is behavioral performance on the counting task.
In conclusion, the subjects with schizotypal personality disorder in this study demonstrated an abnormal pattern in the attentional modulation of startle response that was similar to those found in patients with schizophrenia. This finding suggests the continued value of startle eye blink modification response in identifying cognitive deficits and potential risk markers for schizophrenia. Future studies might improve on the current study by investigating both schizotypal personality disorder and schizophrenia patients within one study to learn more about the boundaries of schizophrenia. For example, it will be important to determine whether the attentional modulation of startle eye blink modification abnormalities observed in the subjects with schizotypal personality disorder in the current study represent a continuous variable, with individuals with schizotypal personality disorder falling between normal healthy subjects and schizophrenia patients, or instead, a discrete variable with schizotypal personality disorder and schizophrenia groups not different from each other but both significantly different from normal subjects. Future studies will also need to improve on the current study by investigating the functional correlates of these startle eye blink modification abnormalities through the use of concurrent technologies. For example, we have reported that in schizophrenia patients, low frontal lobe glucose metabolism (termed “hypofrontality”) is associated with deficient attentional modulation of prepulse inhibition (22), and in healthy individuals, greater blood-oxygen-level-dependent response, as measured by functional magnetic resonance imaging, is observed in the thalamus during attended prepulses compared with ignored prepulses (23). An important next step is to understand the underlying neuroanatomical correlates of startle eye blink modification abnormalities in subjects with schizotypal personality disorder and regarding the schizophrenia spectrum.
Received Oct. 12, 2001; revision received Dec. 4, 2002; accepted March 19, 2003. From the Department of Psychiatry, Mount Sinai School of Medicine; and the Department of Psychiatry, Bronx Veterans Affairs Medical Center, the Bronx, New York. Address reprint requests to Dr. Hazlett, Department of Psychiatry, Box 1505, Mount Sinai School of Medicine, New York, NY 10029; [email protected] (e-mail). Funded in part by NIH grant RR-0071 from the Division of Research Resources to Mount Sinai School of Medicine Clinical Research Center and NIMH grant MH-58673 to Dr. Hazlett.
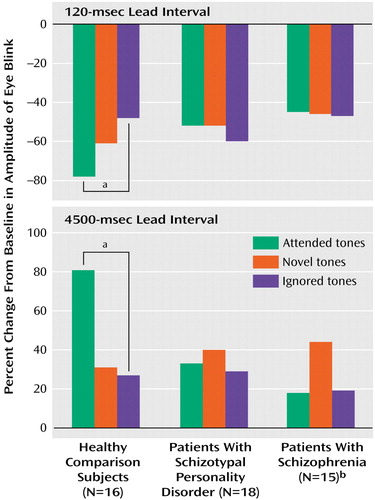
Figure 1. Effects on Startle Eye Blink of Prepulse Type and Interval Between Prepulse and Acoustic Startle Probe Presented to Healthy Comparison Subjects, Patients With Schizotypal Personality Disorder, and Patients With Schizophrenia
aSignificant difference between attended and ignored prepulses (p<0.01, simple effects test).
bThese bars represent scores for patients with schizophrenia from an earlier study of ours (5) and are presented for comparison. The data are reprinted with the permission of Cambridge University Press.
1. Raine A, Lencz T: Conceptual and theoretical issues in schizotypal personality research, in Schizotypal Personality. Edited by Raine A, Lencz T, Mednick SA. New York, Cambridge University Press, 1995, pp 3–15Google Scholar
2. Cadenhead KS, Light GA, Geyer MA, McDowell JE, Braff DL: Neurobiological measures of schizotypal personality disorder: defining an inhibitory endophenotype? Am J Psychiatry 2002; 159:869–871Link, Google Scholar
3. Dawson ME, Hazlett EA, Filion DL, Nuechterlein KH, Schell AM: Attention and schizophrenia: impaired modulation of the startle reflex. J Abnorm Psychol 1993; 102:633–641Crossref, Medline, Google Scholar
4. Dawson ME, Schell AM, Hazlett EA, Nuechterlein KH, Filion DL: On the clinical and cognitive meaning of impaired sensorimotor gating in schizophrenia. Psychiatry Res 2000; 96:187–197Crossref, Medline, Google Scholar
5. Hazlett EA, Buchsbaum MS, Hazneder MM, Singer MB, Germans MK, Schnur DB, Jimenez EA, Buchsbaum BR, Troyer BT: Prefrontal cortex glucose metabolism and startle eye blink modification abnormalities in unmedicated schizophrenic patients. Psychophysiology 1998; 35:186–198Crossref, Medline, Google Scholar
6. Schell AM, Dawson ME, Hazlett EA, Filion DL: Attentional modulation of startle in psychosis-prone college students. Psychophysiology 1995; 32:266–273Crossref, Medline, Google Scholar
7. Graham FK: The more or less startling effects of weak prestimulation. Psychophysiology 1975; 12:238–248Crossref, Medline, Google Scholar
8. Braff DL, Stone C, Callaway E, Geyer M, Glick I, Bali L: Prestimulus effects on human startle reflex in normals and schizophrenics. Psychophysiology 1978; 15:339–343Crossref, Medline, Google Scholar
9. Putnam LE, Vanman EJ: Long lead interval startle modification, in Startle Modification: Implications for Neuroscience, Cognitive Science, and Clinical Science. Edited by Dawson ME, Schell AM, Böhmelt AH. New York, Cambridge University Press, 1999, pp 72–92Google Scholar
10. Filion DL, Dawson ME, Schell AM: The psychological significance of human startle eye blink modification: a review. Biol Psychol 1998; 47:1–43Crossref, Medline, Google Scholar
11. Cadenhead KS, Swerdlow NR, Shafer KM, Diaz M, Braff DL: Modulation of the startle response and startle laterality in relatives of schizophrenic patients and in subjects with schizotypal personality disorder: evidence of inhibitory deficits. Am J Psychiatry 2000; 157:1660–1668; correction, 157:1904Link, Google Scholar
12. Cadenhead KS, Geyer MA, Braff DL: Impaired startle prepulse inhibition and habituation in patients with schizotypal personality disorder. Am J Psychiatry 1993; 150:1862–1867Link, Google Scholar
13. Simons RF, Giardina BD: Reflex modification in psychosis-prone young adults. Psychophysiology 1992; 29:8–16Crossref, Medline, Google Scholar
14. Endicott J, Spitzer RL: A diagnostic interview: the Schedule for Affective Disorders and Schizophrenia. Arch Gen Psychiatry 1978; 35:837–844Crossref, Medline, Google Scholar
15. Pfohl B, Blum N, Zimmerman M, Stangl D: Structured Interview for DSM-III-R Personality, Revised (SIDP-R). Iowa City, University of Iowa College of Medicine, Department of Psychiatry, 1989Google Scholar
16. Andreasen NC, Flaum M, Arndt S: The Comprehensive Assessment of Symptoms and History (CASH): an instrument for assessing diagnosis and psychopathology. Arch Gen Psychiatry 1992; 49:615–623Crossref, Medline, Google Scholar
17. Dawson ME, Schell AM, Hazlett EA, Filion DL, Nuechterlein KH: Attention, startle-eye blink modification and psychosis proneness, in Schizotypal Personality. Edited by Raine A, Lencz T, Mednick SA. New York, Cambridge University Press, 1995, pp 250–271Google Scholar
18. Chapman LJ, Chapman JP: The search for symptoms predictive of schizophrenia. Schizophr Bull 1987; 13:497–503Crossref, Medline, Google Scholar
19. Chapman LJ, Chapman JP, Kwapil TR, Eckblad M, Zinser MC: Putative psychosis-prone subjects 10 years later. J Abnorm Psychol 1994; 103:171–183Crossref, Medline, Google Scholar
20. Siever LJ: Biological markers in schizotypal personality disorder. Schizophr Bull 1985; 11:564–574Crossref, Medline, Google Scholar
21. Buchsbaum MS, Trestman RL, Hazlett EA, Siegel BV, Schaefer CH, Luu-Hsia C, Tang C, Herrera S, Solimando AC, Losonczy M, Serby M, Silverman J, Siever LJ: Regional cerebral blood flow during the Wisconsin Card Sort Test in schizotypal personality disorder. Schizophr Res 1997; 27:21–28Crossref, Medline, Google Scholar
22. Hazlett EA, Buchsbaum MS: Sensorimotor gating deficits and hypofrontality in schizophrenia. Front Biosci 2001; 6:D1069-D1072Google Scholar
23. Hazlett EA, Buchsbaum MS, Tang CY, Fleischman MB, Wei TC, Byne W, Haznedar MM: Thalamic activation during an attention-to-prepulse startle modification paradigm: a functional MRI study. Biol Psychiatry 2001; 50:281–291Crossref, Medline, Google Scholar



