Assessment of Four Stakeholder Groups’ Preferences Concerning Outpatient Commitment for Persons With Schizophrenia
Abstract
OBJECTIVE: Study findings indicating that involuntary outpatient commitment can improve treatment outcomes among persons with severe mental illness remain controversial. Opponents of outpatient commitment argue that its coerciveness is unacceptable even given its arguable benefits. However, it is unclear to what extent the public debate surrounding outpatient commitment represents the preferences of persons with a stake in the benefit or harm resulting from outpatient commitment. This study examines and compares views of outpatient commitment among four stakeholder groups: 1) persons in treatment for schizophrenia and related disorders, 2) family members of persons with these disorders, 3) clinicians treating persons with these disorders, and 4) members of the general public. METHOD: Subjects from the Piedmont region of North Carolina who were members of the four stakeholder groups were presented with short vignettes that depicted potential outcomes that were associated alternatively with outpatient commitment and with voluntary treatment. Subjects rated each vignette according to how positively or negatively they viewed the overall situation for the individual described. Multivariate regression techniques were used to estimate preference weights for each stakeholder group. RESULTS: With some exceptions, each group gave the highest preference to avoiding involuntary hospitalization, followed by avoiding interpersonal violence and maintaining good interpersonal relationships. No group gave appreciable importance to outpatient commitment, which suggests that avoiding its coerciveness is a lesser concern compared to other outcomes. CONCLUSIONS: The findings suggest that these stakeholders are willing to accept the coerciveness of outpatient commitment to gain improved outcomes for certain persons with schizophrenia and related disorders.
Involuntary outpatient commitment is a civil procedure whereby a judge orders a person with mental illness to comply with outpatient treatment or risk sanctions such as being forcibly brought to treatment by law enforcement officers. The use of outpatient commitment to reduce high rates of relapse and related negative outcomes among persons with severe mental illness has generated considerable controversy among mental health policy makers, clinicians, and patient advocate groups (1–11). Critics of outpatient commitment, especially patient advocate groups, have claimed that its potential therapeutic benefits are negated by its coercive effects (1). However, in the midst of this heated public policy debate, there has been little effort to assess systematically representative stakeholders’ views about outpatient commitment. This study examines how key stakeholders appraise the benefits and detriments of outpatient commitment by assessing four stakeholder groups’ preferences concerning the procedure.
Several studies conducted before 1995 reported that patients in outpatient commitment programs had a number of positive outcomes, including lower hospital readmission rates, diminished lengths of stay, and better access to community-based services (12–19). Two randomized, controlled trials of outpatient commitment were conducted after 1995 in North Carolina and New York City. The North Carolina study (20–23) found that subjects randomly assigned to outpatient commitment experienced reduced hospital admissions, compared with subjects released from outpatient commitment. Moreover, subjects who received sustained periods of outpatient commitment in combination with frequent outpatient services had significantly better treatment adherence, were less likely to be violent, and were less likely to be criminally victimized, compared to subjects who received an equal or greater number of treatment service events, but without sustained outpatient commitment. Benefits were most apparent for persons with psychotic disorders.
The randomized trial in New York City evaluated a pilot outpatient commitment program at Bellevue Hospital (8). Subjects were randomly assigned to court-ordered outpatient commitment or release, but all received enhanced treatment services. Although the evaluation found that subjects benefited from enhanced services, there was no evidence that the court order per se improved outcomes. The study’s authors reported that under New York’s newly initiated outpatient commitment statute, enforcement was not fully operational, which limited the interpretation of the findings. In addition, the number of subjects in this study was too small to allow evaluation of potential benefits among subgroups of interest.
Irrespective of empirical findings about outpatient commitment’s effectiveness or lack thereof, many mental health clients and mental health law advocates have strongly opposed court-ordered mental health treatment as coercive, stigmatizing, harmful to therapeutic relationships, and discouraging to those seeking voluntary treatment (1, 24–26). Despite these claims, little empirical research has addressed stakeholders’ assessment of the potential benefits or drawbacks of outpatient commitment. In a study of students’ attitudes toward involuntary hospitalization, respondents reported that they would prefer being hospitalized for 3 days or more to being violently victimized (27).
Although outpatient commitment is of greatest concern to persons with mental illness, other groups—family members, clinicians, and the public at large—have an important stake in the effectiveness of a legal procedure that involves community treatment as well as judicial and law enforcement resources. Patients have opinions about which outcomes have the greatest importance to them, and their family members have similar interests and concerns. Clinicians who use and apply outpatient commitment have their own perspectives about the importance of outcomes associated with the procedure, as do members of the general public. For a more comprehensive appraisal of the effectiveness of outpatient commitment, researchers must account for the relative importance of different outcomes under outpatient commitment, as well as differences across stakeholder groups in the willingness to accept certain tradeoffs that may be inherent in outpatient commitment.
Medical decision analysts have developed strategies for quantifying preferences or utilities for health outcomes (28–31). Such methods permit estimation of preferences or importance weights for outcome domains, which can be used to quantify preference-weighted outcomes by multiplying a score on an outcome measure by the preference weight for that outcome and summing the results.
Several investigators have recently examined preference measurement for schizophrenia outcomes (32–35). Most studies have focused on preferences for health status associated with antipsychotic medication—especially therapeutic gains versus side effects (32–34, 36, 37). To our knowledge, no studies have applied these methods to evaluate preferences for mandated community treatment.
The present study quantifies preferences for four outcome domains in schizophrenia treatment: involuntary outpatient commitment, involuntary rehospitalization, interpersonal violence, and interpersonal relationships. We examine the preferences of four stakeholder groups and examine the extent to which different stakeholders have different outcome preferences. We also examine how much importance stakeholders assign to coercive treatment under outpatient commitment, given the potential tradeoffs of other treatment outcomes.
Method
Subjects
To examine how different stakeholder groups weight the importance of outpatient commitment in relation to other outcomes, we collected data from persons with schizophrenia and related disorders (subjects with psychoses), family members of persons with schizophrenia and related disorders, members of the general public, and clinicians. All participants were from the Piedmont region of North Carolina. After complete description of the study to the participants, written informed consent was obtained.
Subjects with psychoses
The subjects with schizophrenia and related disorders (including schizoaffective and schizophreniform disorders) had recently completed an observational study of schizophrenia treatment under “usual-care” conditions. Eligible subjects included all adult patients within a defined geographic region who were in treatment for a recently documented DSM-IV diagnosis of schizophrenia, schizoaffective disorder, or schizophreniform disorder.
Even after giving informed consent to participate, a small number of subjects demonstrated potential difficulty comprehending the relatively complex interview. Those subjects were assessed by using the Short Portable Mental Status Questionnaire (38). If the subject committed four or more errors, the interview was stopped and the data were not used. In addition, at the end of the interview, the interviewers rated the respondents’ level of comprehension of the detailed and cognitively demanding study instrument; data for subjects who were rated as not understanding the interview were also excluded. Eleven subjects were excluded from the study on the basis of these criteria. A total of 104 subjects with psychoses were included in the final study group (Table 1).
Family members
Family members were recruited by asking potential subjects with schizophrenia for permission to contact a family member, even if the person with schizophrenia did not wish to participate. Subjects who gave informed consent to contact a family member provided one to three family contacts, ordered by the closeness of the subject’s relationship with the family member. The family members with the closest relationship to the subject were approached first. To maximize diversity among the family members in the study, we recruited additional family members through advertisements placed in a local daily newspaper and in the newsletters of area chapters of the National Alliance for the Mentally Ill (NAMI). Family members who had worked as mental health clinicians in the past 2 years were excluded, as were family members who reported being hospitalized for mental health problems in the past 5 years (N=2). The same comprehension standards used for the subjects with psychoses were also used for the family members. Only one family member was excluded because of comprehension difficulties.
Forty-nine family members (59.0%) were recruited through contacts with study subjects, and 34 (41.0%) were recruited through the newspaper and NAMI newsletter advertisements. The two groups of family members did not differ by gender or age, but they did differ by race (73.5% of the family members recruited through the study subjects were African American, compared with 38.2% of the group recruited through the advertisements; χ2=10.30, df=1, 83, p<0.005) and in their mean number of years of education (11.8 years for the family members recruited through the study subjects, compared with 15.6 years for the group recruited through the advertisements; t=–6.39, df=81, p<0.0001).
Members of the general public
Members of the general public were recruited through a list of research volunteers maintained at the Center for the Study of Aging and Human Development at Duke University Medical Center and through advertisements placed in the local daily newspapers. To ensure demographic diversity, the general public group was stratified by gender and age on the basis of gender and age distributions in the 1990 census data. Persons who had worked as mental health clinicians in the previous 2 years were excluded, as were persons who reported having ever been hospitalized for mental health problems (N=3). None of the 59 participants in the general public group was excluded on the basis of poor comprehension.
Clinicians
The clinician subjects (N=85) were selected from the staff rosters of community mental health centers and the psychiatric wards of general hospitals in the local area and from among psychiatrists in private practice in the region who treated patients with schizophrenia and related disorders. The clinicians were surveyed with a mailed questionnaire version of the interview adapted for self-administration; those who did not return the questionnaire were sent three reminders. This method yielded a response rate of 85%. The clinicians had an average of 12.85 years of experience (SD=8.82) in the mental health field (excluding time spent in training). Twenty-seven respondents were employed at a state hospital, 37 at a community mental health program, 10 at a health center, 11 at a Veterans Affairs hospital, 19 at a medical school, 16 in private practice, five in a correctional facility, and five in other settings. (Clinicians could list more than one employer.) Forty-four clinicians had a medical degree, two had a doctoral degree, 25 had a master’s degree in social work or another master’s degree, three were registered nurses, nine had a bachelor’s-level degree, and two were caseworkers with less than a bachelor’s degree. A majority of clinicians (N=51, 60%) reported that 25% or more of their caseload consisted of patients with schizophrenia, and only 18 (21.2%) reported less than 10% of their caseload consisted of patients with schizophrenia. Data for two clinicians who did not complete all questionnaire items were excluded.
Procedures
Trained field research interviewers described the study, obtained informed consent, and conducted interviews with participants with psychoses, family members, and members of the general public. The interviewers were trained to repeat questions as often as needed and to use neutral probes if answers were inconsistent or seemed confused. The average length of an interview was 1.5 hours for the participants with schizophrenia, 1.1 hours for the family members, and 0.8 hours for the general public. As mentioned, clinicians’ responses were obtained by using a self-administered survey; informed consent was obtained by return of the survey.
Instruments
To assess the preferences of participants, we described a hypothetical person with schizophrenia, Mr. Smith, and provided a brief description of outpatient commitment. Mr. Smith was introduced as having had problems with drug and alcohol abuse and as being released from the hospital after an involuntary admission for threatening strangers on the street. This description of Mr. Smith, i.e., as an individual with schizophrenia, substance use problems, and a history of threatening behavior, was intended to reflect the population in which outpatient commitment is most frequently applied.
This introduction was followed by eight vignettes, each of which described a different set of outcomes that Mr. Smith could experience after leaving the hospital at the end of an involuntary psychiatric hospitalization. The eight vignettes were constructed by using four possible outcome domains presented in the following order: involuntary outpatient commitment, interpersonal relationships, interpersonal violence, and involuntary rehospitalization. Within each domain, two levels of outcome—a “good” and a “bad” outcome—were possible. Placing outpatient commitment first was necessary for the temporal and causal ordering assumed in the vignettes, but this placement also served to ensure that outpatient commitment was less likely to be overlooked by the participant. The vignettes were presented in random order. See Figure 1 for the description of Mr. Smith and a summary of the vignettes.
For the outpatient commitment domain, the vignettes contained either a statement that Mr. Smith was discharged without any legal requirement to continue outpatient treatment or a statement that Mr. Smith was discharged with the requirement that he enter involuntary outpatient commitment. Outpatient commitment was described as being ordered by a judge to comply with mental health treatment, including taking medication. Because the North Carolina outpatient commitment statute does not allow forcible administration of medications, the vignettes did not describe forcible administration of medications.
For the interpersonal relationships domain, the two levels consisted of getting along well with his family, friends, and other people versus arguing with them. For the interpersonal violence domain, the two levels were the absence or presence of assault by Mr. Smith against a stranger who Mr. Smith believed was threatening him. For involuntary hospitalization, the two levels were the presence or absence of worsening symptoms leading to an involuntary rehospitalization lasting 7 days or more.
After hearing the entire vignette (or reading it, in the case of the clinicians), the participants were asked to assign a score representing how good or bad they thought that entire situation was for Mr. Smith. Possible scores were presented on a scale from 0 to 10, with 0 being the worst possible situation for Mr. Smith and 10 being the best. The participants were asked to imagine themselves in Mr. Smith’s situation when making this rating.
With four domains, each of which had two possible states, a full factorial design would be unworkably burdensome and repetitive for the participants. A fractional factorial design allowed us to reduce the number of vignettes presented (39–41). This design allowed us to determine the main effects in each of the four domains as well as the first-order interaction between outpatient commitment and the other three domains (42). Each participant was asked to rate eight vignettes.
After rating the vignettes, all participants also completed a preference-ordering task, in which they were asked to place the following items in order of importance, if they had a serious mental illness like schizophrenia: 1) being free to participate in treatment or not; 2) staying out of the hospital; 3) being safe; 4) being “clean and sober”; 5) getting along with family, friends, and other people; 6) and feeling well, thinking clearly, and not hearing voices. Participants with schizophrenia, family members, and members of the general public gave their rating as part of a card-sort task, and the clinicians used a printed list. These importance ratings were included both as a validation check for the utilities data generated from the responses to the vignettes and to allow exploration of additional domains that were not included in the vignette design.
Statistical Analysis
We used conjoint analysis to determine the utility and preference weights for participants’ responses. In conjoint analysis, linear regression, stratified by participant, is employed to determine the utility and preference weights. Scores given by the respondent for each vignette formed the dependent variables. Independent variables were formed from a set of proxy variables representing each outcome domain (e.g., outpatient commitment), and the regression coefficients for these dummy variables were the utilities. The null conditions were defined as being placed in outpatient commitment, arguing with family and friends, being violent, and being involuntarily rehospitalized. Within the coding scheme, positive coefficients denoted a positive utility for avoiding outpatient commitment, not arguing with family and friends, avoiding violence, and avoiding rehospitalization. The utilities denoted by the regression coefficients represented the change in the vignette score attributable to the endorsement of a positive outcome for that domain. For example, a coefficient of 0.5 for interpersonal violence indicated that the importance attached to avoiding violence raises or improves the vignette score by one-half point, on average, when the vignette specifies no violence.
The preference weight for each domain was calculated as the magnitude (absolute value) of the coefficient for that domain divided by sum of the magnitudes of the coefficients for all four domains. The weights conveyed how important each domain was in the participant’s assessment of Mr. Smith’s situation, regardless of the direction of the influence of that domain. For each participant, the preference weights sum to 100 and can be thought of as the relative percentage of influence for each domain.
Averages of the utilities and preference weights were calculated for all participants combined and for each group of subjects separately. Analysis of variance was used to make between-group comparisons, and the Tukey-Kramer adjustment was used to correct for multiple comparisons.
Results
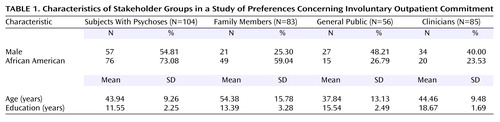
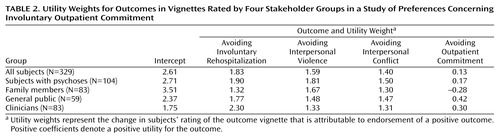
Table 1 presents a demographic profile of each stakeholder group. Table 2 presents the average utilities for all participants and for each stakeholder group separately. Avoiding involuntary rehospitalization had the highest utility for subjects with psychoses, members of the general public, and clinicians, and avoiding violence had the highest utility for family members. Avoiding outpatient commitment had the lowest utility of any domain for all four stakeholder groups.
For the outpatient commitment domain, the family members’ utility for avoiding outpatient commitment was significantly lower than that of the general public (t=–2.82, df=140, p<0.05). The family members’ utility for avoiding involuntary hospitalization was significantly less than that of the clinicians (t=–3.60, df=174, p<0.005). The cohorts did not differ on utilities for the domains of interpersonal relationships or violence. The coefficient for the intercept shows, for each stakeholder group, the value of the base situation (i.e., in which Mr. Smith is hospitalized, is violent, has poor interpersonal relationships, and is placed in outpatient commitment). On the intercept, the subjects with psychoses rated Mr. Smith’s base situation higher than the clinicians (t=2.87, df=185, p<0.05), and the family members rated his situation higher than the general public (t=–2.95, df=140, p<0.05) and the clinicians (t=–4.99, df=164, p<0.0001).
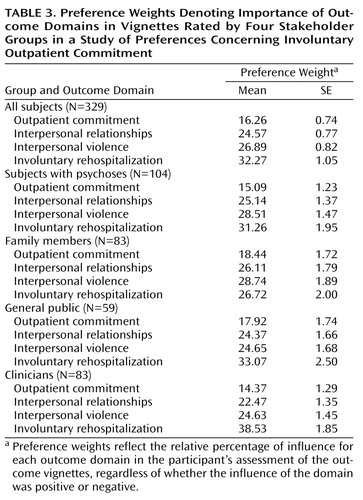
Preference Weights
Preference weights by stakeholder group are listed in Table 3. Because the weights reflect the magnitude of the coefficients but not the direction, the preference weight for outpatient commitment is greater than its utility. Outpatient commitment was consistently rated as less important than other domains. The clinicians’ preference weights for rehospitalization were significantly higher than those of the family members (t=–4.09, df=164, p<0.0005) and the subjects with psychoses (t=–2.65, df=185, p<0.05).
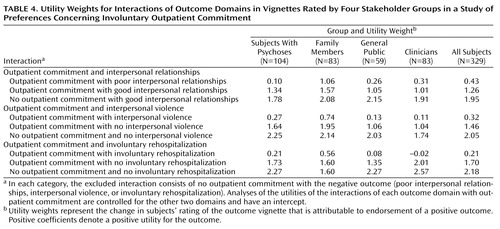
Interaction of Outpatient Commitment With the Other Domains
The results of the analysis of the interaction of outpatient commitment with other domains are shown in Table 4. The excluded category for each model was no outpatient commitment and a bad outcome (poor interpersonal relationships, violence, or rehospitalization). All models controlled for the main effect of the two domains not involved in the interaction. As expected, the highest utility in each analysis was for avoiding outpatient commitment while having a good outcome. The lowest utility in each instance was for being placed in outpatient commitment and still having a bad outcome. Despite these overall findings, the average utility for outpatient commitment with a bad outcome was still positive for most cases, except for the clinicians’ views of the interaction between outpatient commitment and rehospitalization. That is, none of the participant groups rated the adverse effects of outpatient commitment highly.
Preference Order
Participants ordered six items from most to least important. The preference order of this ranking was calculated for each group for each item. With one exception, the rankings from most important to least important in every group were 1) feeling well, thinking clearly, and not hearing voices; 2) being safe; 3) getting along with family, friends, and other people; 4) staying out of the hospital; 5) being clean and sober; 6) and being free to participate in treatment or not. The only exception was that the general public group considered being clean and sober to be more important than staying out of the hospital. These findings confirm the analyses based on utility and preference weights, i.e., reducing symptoms, avoiding interpersonal conflict, and avoiding rehospitalization outrank avoidance of outpatient commitment as areas of concern.
Discussion
We found that four stakeholder groups—subjects with schizophrenia and related disorders, family members of persons with these disorders, clinicians, and members of the general public—have remarkably similar views about preferred outcomes in treatment of schizophrenia. Presented with a vignette-rating task depicting a patient at high risk for relapse and rehospitalization, stakeholders generally gave greatest importance to avoiding involuntary hospitalization, interpersonal violence, and interpersonal conflict; avoiding involuntary outpatient commitment was of relatively little importance. The results of the preference-ordering task were similar, suggesting that stakeholders viewed outpatient commitment as less noxious than other negative outcomes. The concordance of the latter results with the conjoint analyses also indicates that the stakeholders understood the vignette-rating task and provided internally consistent ratings.
One caveat is that these results refer to particular vignettes depicting a clinically unstable patient with schizophrenia and do not necessarily generalize to situations involving more stable patients or patients with other psychiatric disorders. Enforcement of outpatient commitment was not depicted in the vignettes due to interviewing time constraints. Adding details about enforcement of outpatient commitment by law officers might have influenced the views of stakeholders, although actual enforcement by law officers has been rare (22). As a further caveat, the respondents with psychoses in our study were selected from an established longitudinal research cohort of persons who had been treated for schizophrenia. Their views may not be representative of the views of persons who avoid treatment or who refuse to participate in research. The North Carolina stakeholders in the present study may not be representative of persons in other regions of the country and may reflect more deference to medical authority than is found in other regions. In future analyses, we hope to compare the attitudes toward mental illness and treatment of the North Carolina stakeholders to those of a nationally representative sample.
The views of the stakeholders, who found outpatient commitment less deleterious and restrictive than hospitalization, were consistent with the intent of outpatient commitment statutes. It is important to note that the statutory intent of using outpatient commitment as a means to avoid and minimize involuntary inpatient treatment often appears to be overlooked by its critics. Our findings, based on a systematic assessment of stakeholders’ opinions, suggest that some of those criticisms may be misplaced.
We have reported elsewhere the results of studies showing that outpatient commitment, particularly when applied for extended periods and in conjunction with frequent outpatient services, is associated with a range of positive outcomes, including reduced hospitalization, reduced violence, better treatment adherence, and improved quality of life among persons with schizophrenia and related disorders (23). Nevertheless, the empirical evidence of such benefits does not by itself support an unqualified endorsement of outpatient commitment without adequate consideration of concurrent costs, including curtailment of personal autonomy in mental health treatment. The findings presented here inform these cost issues by providing a subjective context for the positive outcomes previously reported.
Data on the subjective value that persons assign to the potential benefits of outpatient commitment, compared to the value they assign to avoiding the undesirable features of outpatient commitment, has heretofore been missing from the literature on outpatient commitment outcomes. Given that all four groups in our study considered the benefits to outweigh the potential downside of outpatient commitment (at least outpatient commitment as represented by the vignettes we used), the findings would seem to support a recommendation that outpatient commitment be implemented under the conditions and within the populations in which research has shown that it is likely to be effective.
Of course, deontological and other ethical arguments against outpatient commitment have been made. Some opponents of outpatient commitment view coercion as intrinsically unjust and illegitimate outside the limited confines of the police powers of the state. To such arguments, stakeholders’ opinions are as irrelevant as outcome studies showing benefits—just as they would be to strong, morally based arguments against any legal procedures regarded as intrinsically immoral. However, if one assumes that outpatient commitment in principle involves a utilitarian question of balancing means and ends, then the present paper suggests that, under certain conditions, these stakeholders believe the ends do justify the means.
 |
 |
 |
 |
Received Sept. 24, 2002; revision received Jan. 7, 2003; accepted Jan. 9, 2003. From the Services Effectiveness Research Program, Department of Psychiatry and Behavioral Sciences, Duke University Medical Center; and the Department of Psychiatry, San Francisco General Hospital and the University of California, San Francisco, San Francisco. Address reprint requests to Dr. Swartz, Department of Psychiatry and Behavioral Sciences, Duke University Medical Center, Box 3173, Durham, NC 27710; [email protected] (e-mail). Supported by NIMH grants MH-48103 and MH-51410 and by the MacArthur Foundation Initiative on Mandated Community Treatment.
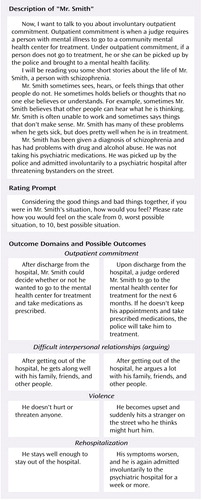
Figure 1. Outcomes for a Hypothetical Person With Schizophrenia That Were Rated in a Study of Preferences Concerning Involuntary Outpatient Commitment
1. Allen M, Smith VF: Opening Pandora’s box: the practical and legal dangers of involuntary outpatient commitment. Psychiatr Serv 2001; 52:342-346Link, Google Scholar
2. Appelbaum PS: Thinking carefully about outpatient commitment. Psychiatr Serv 2001; 52:347-350Link, Google Scholar
3. Gerbasi JB, Bonnie RJ, Binder RL: Resource document on mandatory outpatient treatment. J Am Acad Psychiatry Law 2000; 28:145-148Medline, Google Scholar
4. Kress K: An argument for assisted outpatient treatment for persons with serious mental illness illustrated with reference to a proposed statute for Iowa. Iowa Law Rev 2000; 85:1269-1386Google Scholar
5. Lamb HR, Weinberger LE: A major advance in the laws pertaining to community treatment for persons with severe mental illness. J Am Acad Psychiatry Law 2000; 28:127-144Medline, Google Scholar
6. Mattison E: The law of unintended consequences. J Am Acad Psychiatry Law 2000; 28:127-144Medline, Google Scholar
7. Mulvey EP, Geller JL, Roth LH: The promise and peril of involuntary outpatient commitment. Am Psychol 1987; 42:571-584Crossref, Medline, Google Scholar
8. Steadman HJ, Gounis K, Dennis D, Hopper K, Roche B, Swartz M, Robbins PC: Assessing the New York City outpatient commitment pilot program. Psychiatr Serv 2001; 52:330-336Link, Google Scholar
9. Stein LI, Diamond RJ: Commentary: a “systems”-based alternative to mandatory outpatient treatment. J Am Acad Psychiatry Law 2000; 28:159-164Medline, Google Scholar
10. Swartz MS, Monahan J: Special section on involuntary outpatient commitment: introduction. Psychiatr Serv 2001; 52:323-324Link, Google Scholar
11. Torrey EF, Zdanowicz M: Outpatient commitment: what, why, and for whom. Psychiatr Serv 2001; 52:337-341Link, Google Scholar
12. Fernandez GA, Nygard S: Impact of involuntary outpatient commitment on the revolving-door syndrome in North Carolina. Hosp Community Psychiatry 1990; 41:1001-1004Abstract, Google Scholar
13. Hiday VA: Coercion in civil commitment: process, preferences, and outcome. Int J Law Psychiatry 1992; 15:359-377Crossref, Medline, Google Scholar
14. Hiday VA, Scheid-Cook TL: The North Carolina experience with outpatient commitment: a critical appraisal. Int J Law Psychiatry 1987; 10:215-232Crossref, Medline, Google Scholar
15. Hiday VA, Scheid-Cook TL: A follow-up of chronic patients committed to outpatient treatment. Hosp Community Psychiatry 1989; 40:52-59Abstract, Google Scholar
16. Hiday VA, Scheid-Cook TL: Outpatient commitment for “revolving door” patients: compliance and treatment. J Nerv Ment Dis 1991; 179:83-88Crossref, Medline, Google Scholar
17. Keilitz I: Empirical studies of involuntary outpatient civil commitment: is it working? Ment Phys Disabil Law Rep 1990; 14:368-379Google Scholar
18. Moloy A: Analysis: Critiquing the Empirical Evidence: Does Involuntary Outpatient Commitment Work? Washington, DC, Mental Health Policy Resource Center, 1992Google Scholar
19. Swartz MS, Burns BJ, Hiday VA, George LK, Swanson J, Wagner HR: New directions in research on involuntary outpatient commitment. Psychiatr Serv 1995; 46:381-385Link, Google Scholar
20. Swanson JW, Swartz MS, Borum R, Hiday VA, Wagner HR, Burns BJ: Involuntary outpatient commitment and reduction of violent behaviour in persons with severe mental illness. Br J Psychiatry 2000; 176:324-331Crossref, Medline, Google Scholar
21. Swanson JW, Borum R, Swartz MS, Wagner HR, Burns BJ, Hiday VA: Can involuntary outpatient commitment reduce arrests among persons with severe mental illness? Crim Justice Behav 2001; 28:156-189Crossref, Google Scholar
22. Swartz MS, Swanson JW, Wagner HR, Burns BJ, Hiday VA, Borum R: Can involuntary outpatient commitment reduce hospital recidivism? findings from a randomized trial with severely mentally ill individuals. Am J Psychiatry 1999; 156:1968-1975Abstract, Google Scholar
23. Swartz MS, Swanson JW, Hiday VA, Wagner HR, Burns BJ, Borum R: A randomized controlled trial of outpatient commitment in North Carolina. Psychiatr Serv 2001; 52:325-329Link, Google Scholar
24. Campbell J, Shraiber R: In Pursuit of Wellness: The Well-Being Project 6. Sacramento, California Department of Mental Health, 1989Google Scholar
25. Schwartz SJ, Costanzo CE: Compelling treatment in the community: distorted doctrines and violated values. Loyola of Los Angeles Law Rev 1987; 20:1329-1429Medline, Google Scholar
26. Stefan S: Preventive commitment: the concept and its pitfalls. Ment Phys Disabil Law Rep 1987; 11:288-302Google Scholar
27. Mossman D, Hart KJ: How bad is civil commitment? a study of attitudes toward violence and involuntary hospitalization. Bull J Am Acad Psychiatry Law 1993; 21:181-184Medline, Google Scholar
28. Froberg DG, Kane RL: Methodology for measuring health-state preferences, I: measurement strategies. J Clin Epidemiol 1989; 42:345-354Crossref, Medline, Google Scholar
29. Froberg DG, Kane RL: Methodology for measuring health-state preferences, II: scaling methods. J Clin Epidemiol 1989; 42:459-471Crossref, Medline, Google Scholar
30. Froberg DG, Kane RL: Methodology for measuring health-state preferences, III: population and context effects. J Clin Epidemiol 1989; 42:585-592Crossref, Medline, Google Scholar
31. Froberg DG, Kane RL: Methodology for measuring health-state preferences, IV: progress and a research agenda. J Clin Epidemiol 1989; 42:675-685Crossref, Medline, Google Scholar
32. Lee TT, Ziegler JK, Commi R, Sugar C, Mahmoud R, Lenert LA: Comparison of preferences for health outcomes in schizophrenia among stakeholder groups. J Psychiatr Res 2000; 34:201-210Crossref, Medline, Google Scholar
33. Lenert LA, Ziegler J, Lee T, Sommi R, Mahmoud R: Differences in health values among patients, family members, and providers for outcomes in schizophrenia. Med Care 2000; 38:1011-1021Crossref, Medline, Google Scholar
34. Revicki DA, Shakespeare A, Kind P: Preferences for schizophrenia-related health states: a comparison of patients, caregivers and psychiatrists. Int Clin Psychopharmacol 1996; 11:101-108Medline, Google Scholar
35. Shumway M: Preference weights for cost-outcome analyses of schizophrenia treatments: comparison for four stakeholder groups. Schizophr Bull (in press)Google Scholar
36. Awad AG, Voruganti LP: Cost-utility analysis in schizophrenia. J Clin Psychiatry 1999; 60(suppl 3):22-26Google Scholar
37. Chouinard G, Albright PS: Economic and health state utility determinations for schizophrenia patients treated with risperidone or haloperidol. J Clin Psychopharmacol 1997; 17:298-307Crossref, Medline, Google Scholar
38. Pfeiffer E: A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 1975; 23:433-441Crossref, Medline, Google Scholar
39. Cadman D, Goldsmith C: Construction of social value or utility-based health indices: the usefulness of factorial experimental design plans. J Chronic Dis 1986; 39:643-651Crossref, Medline, Google Scholar
40. Anderson NH: Foundations of Information Integration Theory. New York, Academic Press, 1981Google Scholar
41. Barron FH, Person HB: Assessment of multiplicative utility functions via holistic judgments. Organ Behav Hum Perform 1979; 24:147-166Crossref, Google Scholar
42. Kuhfed W: Conjoint Analysis Examples. Cary, NC, SAS Institute, 2002Google Scholar



