Comorbidity, Impairment, and Suicidality in Subthreshold PTSD
Abstract
OBJECTIVE: Reliance on the categorical model of psychiatric disorders has led to neglected study of posttraumatic sequelae that fall short of full criteria for posttraumatic stress disorder (PTSD). Substantial disability and suicidal risk is associated with subthreshold PTSD, but this association has not been well studied. In addition, no studies have examined the role of comorbidity in explaining disability and impairment in subthreshold PTSD. METHOD: On National Anxiety Disorders Screening Day 1997, 2,608 out of 9,358 individuals screened for affective and anxiety disorders at 1,521 sites across the United States reported at least one PTSD symptom of at least 1 month’s duration. Impairment, comorbid anxiety disorders, major depressive disorder, and rates of suicidality were determined and compared for individuals with no, one, two, three, or four (full PTSD) symptoms on a screening questionnaire. Regression analyses examined the relative contribution of subthreshold PTSD and comorbid disorders to impairment and suicidal ideation. RESULTS: Impairment, number of comorbid disorders, rates of comorbid major depressive disorder, and current suicidal ideation increased linearly and significantly with each increasing number of subthreshold PTSD symptoms. Individuals with subthreshold PTSD were at greater risk for suicidal ideation even after the authors controlled for the presence of comorbid major depressive disorder. CONCLUSIONS: Higher numbers of subthreshold PTSD symptoms were associated with greater impairment, comorbidity, and suicidal ideation. Disability and impairment found in previous studies of subthreshold PTSD symptoms may be related in part to the presence of comorbid disorders. However, the presence of subthreshold PTSD symptoms significantly raised the risk for suicidal ideation even after the authors controlled for major depressive disorder. Given the broad public health implications of these findings, more efforts are needed to identify subthreshold PTSD symptoms in clinical populations, epidemiologic surveys, and treatment studies.
Since the identification in 1980 of posttraumatic stress disorder (PTSD) as a diagnosable syndrome, numerous studies have demonstrated a high degree of associated disability, including work-related impairment (1, 2), somatic complaints (3), lower quality of life (4), suicidality (2, 5), medical illness (3), negative body image (6), impaired intimacy (7), increased burden to spouse or partner (8), and social dysfunction (9, 10).
A consequence of reliance on the categorical model of psychiatric disorders, however, is that relatively little attention has been paid to disability and impairment in individuals with PTSD symptoms that fall short of meeting full criteria. Subthreshold PTSD may result from partial recovery from the full syndrome or from the development of subthreshold symptoms after trauma. For methodologic reasons, clinical trials and epidemiologic studies rarely examine subthreshold symptoms (11). The National Comorbidity Study was unable to address the question of partial or subthreshold PTSD because the diagnostic module for PTSD was abandoned if at any point in the interview the individual did not meet criteria for the particular symptom cluster being evaluated.
A few studies have examined the prevalence of subthreshold PTSD and associated impairment. In an epidemiologic study in Canada, Stein et al. (12) found that individuals meeting partial criteria for PTSD reported impairment of occupational, social, and home functioning that was comparable to that observed in full PTSD. Partial PTSD was defined as having at least one symptom in each DSM-IV criterion category. The incidence of current full PTSD in this study was 5.0% for women and 1.7% for men; the incidence of partial PTSD was 5.7% for women and 2.2% for men.
A similar pattern has been found in high-risk groups. The National Vietnam Veterans Readjustment Study (13) found that the lifetime prevalence of full PTSD was 30.9% for male and 26% for female veterans; the prevalence of partial PTSD was 22.5% for male and 21.2% for female veterans. The authors of this study defined a subject as having subthreshold PTSD if the subject’s level of dysfunction was equivalent to that seen in individuals with full PTSD, if criteria were met for two of three symptom clusters (i.e., reexperiencing, avoidance, or hyperarousal), or if most criteria were met in each category (Daniel Weiss, personal communication).
Blanchard et al. (1) longitudinally assessed 132 victims of serious motor vehicle accidents 1–4 months after the accident and found that 39.2% met full PTSD criteria and 28.5% met subthreshold criteria, defined as meeting two of three category requirements. Carlier and Gersons (14) conducted prospective screening assessments of 136 survivors of the Bijlmermeer disaster in the Netherlands (in which a plane crashed into two apartment buildings). Six months after the disaster, 26% of respondents met full criteria for PTSD and 20% met two of three PTSD screening criteria.
Schutzwohl and Maercker (15) assessed PTSD, depressive symptoms, and anxiety symptoms in 146 political prisoners in the former German Democratic Republic compared with symptoms among subjects who had not experienced trauma. When partial PTSD was defined as meeting criteria for reexperiencing and for either avoidance or hyperarousal, the rate of full PTSD was 31% and partial PTSD, 29%. The severity of the psychopathology of subjects with partial PTSD was intermediate between that of the nontraumatized control group and that of the subjects with full PTSD (15). The authors advocated formal recognition of the partial PTSD diagnosis in order to facilitate public health and research efforts with these individuals.
In summary, studies to date have found that subthreshold PTSD, defined in several different ways, is about as common as full PTSD and is associated with substantial impairment. However, given the high rates of comorbid disorder in PTSD and the fact that none of the cited studies assessed comorbidity, it cannot be assumed that such impairment is attributable to PTSD symptoms. This is important because high rates of comorbid psychiatric disorders have been reported in PTSD (16–19). In the National Comorbidity Study (19), 88.3% of men and 79.0% of women with a lifetime history of PTSD met criteria for at least one other disorder. Perhaps functional impairment in subthreshold PTSD might be explained by impairment due to other disorders, as has been observed in dysthymia (20). Psychiatric disorders are consistently associated with greater disability when comorbidity is present (21, 22).
The current study was conducted to investigate the relationships among PTSD symptoms, level of disability, and comorbid psychiatric disorders in a large data set collected on National Anxiety Disorder Screening Day 1997. Our objectives were to 1) characterize symptoms and disability in individuals with subthreshold PTSD, 2) examine the associations between PTSD symptoms and levels of disability, suicidal ideation, and comorbid disorders, and 3) conduct a predictor analysis to examine the contribution of subthreshold PTSD to impairment and suicidal ideation relative to the contribution of other psychiatric diagnoses.
Method
Subjects
National Anxiety Disorders Screening Day is held on a single day once a year across the United States. Its goals are to provide information about anxiety and affective disorders to the public, identify individuals who may be in need of clinical intervention, and provide referrals for treatment. In the 1997 survey, 9,358 individuals who visited one of the 1,521 screening sites first watched a video that illustrated the clinical presentation of PTSD, social phobia, panic disorder, generalized anxiety disorder, obsessive-compulsive disorder (OCD), and major depressive disorder through patients’ testimonial descriptions. Written informed consent was obtained from all participants after the study procedures were explained, and the screening questionnaire (described below) was completed if consent was given. A volunteer health professional from the local community met with each individual, reviewed the screening instrument, and made an appropriate referral recommendation based on the individual’s treatment preference and the volunteer health professional’s clinical judgment.
Screening Questionnaire
A brief screening instrument was developed with the objective of identifying individuals with symptoms of PTSD, panic disorder, social phobia, generalized anxiety disorder, OCD, major depressive disorder, or suicidal ideation. The questionnaire also probes readiness for treatment, history, functional impairment, and demographic characteristics.
Given that the goal of the instrument is to rapidly and reliably identify individuals who may be in need of treatment, a disorder was defined as present on the basis of key features of the disorder. To assess PTSD, the screening instrument first assesses for history of a criterion A trauma with the following question: Have you ever had an extremely frightening, traumatic, or horrible experience like being the victim of a violent crime, seriously injured in an accident, sexually assaulted, seeing someone seriously injured or killed, or been the victim of a natural disaster? The instrument then assesses four symptom clusters: reexperiencing (Did you relive the experience through recurrent dreams, preoccupations, or flashbacks?), withdrawal/loss of interest (Did you seem less interested in important things, not “with it,” or unable to experience or express emotions?), insomnia (Did you have problems sleeping, concentrating, or have a short temper?), avoidance (Did you avoid any place or anything that reminded you of the original horrible event), and duration of symptoms for longer than 1 month. For this study, a subject was included in data analyses if he or she reported a criterion A trauma and reported at least one symptom lasting at least 1 month.
The following definitions were used for the other anxiety disorders. Panic disorder was diagnosed if individuals reported having a sudden, unexplained panic attack, plus two of the following: 1) fear of having more attacks, 2) fear of losing control, having a heart attack, or going crazy, and 3) change in behavior because of the attacks. Generalized anxiety disorder was diagnosed if individuals reported 1) persistent worry about several different things, such as work, school, family, money, and others, and 2) finding it difficult to control the worrying. OCD was diagnosed if individuals reported 1) having persistent senseless thoughts such as thoughts about death, illnesses, aggression, sexual urges, or contamination, and 2) spending more time than was necessary doing things over and over again, such as washing hands, checking things, or counting things. Social phobia was diagnosed if individuals reported 1) fearing being observed by others doing things such as public speaking, eating, performing, or teaching, and 2) feeling uncomfortable at social events. Major depressive disorder was diagnosed if individuals reported four of the following: 1) often feeling sad or depressed, 2) having stopped enjoying the same pleasures enjoyed in the past, 3) experiencing difficulty concentrating, making decisions, or completing tasks, 4) having difficulty sleeping or staying asleep, 5) usually feeling hopeless about the future. To assess suicidal ideation, subjects were asked if they had “recently (during the past month) thought of or are currently thinking of suicide.”
To assess impairment, the following question was asked: During the past month, how much of the time does your anxiety interfere with your daily life? The answer choices were 1) not at all (0%), 2) rarely (5%–10%), 3) some of the time (20%–30%), 4) about half the time (40%–60%), 5) most of the time (70%–80%), and 6) almost all the time (90%–100%).
To assess the screening instrument’s psychometric properties, a subgroup of individuals (N=203) were given the screening questionnaire, followed by a Structured Clinical Interview for DSM-IV. Sensitivity, specificity, and kappa, respectively, for each disorder were as follows: PTSD, 0.62, 0.94, 0.44; OCD, 0.5, 0.91, 0.39; major depressive disorder, 0.80, 0.72, 0.44; generalized anxiety disorder, 0.89, 0.55, 0.34; panic disorder, 0.87, 0.72, 0.50; and social phobia, 0.64, 0.85, 0.46. Mean sensitivity was 0.70, and mean specificity was 0.79. This demonstrates acceptable psychometric properties for a screening instrument (defined by Landis and Koch [23] as kappa between 0.40 and 0.75).
Analysis
Level of impairment, number of comorbid anxiety disorders, and proportion of subjects with comorbid major depressive disorder were calculated for individuals with no, one, two, three, or four (full PTSD) symptoms. These groups were compared by using analysis of variance (ANOVA) with post hoc pairwise comparisons (Scheffé method). The analysis of comorbid major depressive disorder was conducted separately from that of comorbid anxiety disorders for two reasons: 1) the association between major depressive disorder and suicidal ideation is well established; 2) individuals with PTSD are significantly more impaired if they also meet criteria for major depressive disorder (1). Pearson product moment correlations were also calculated. Chi-square analysis was used to compare rates of suicidal ideation for each number of PTSD symptoms.
We performed linear regression to assess the association between the comorbid disorders and level of impairment while controlling for background demographic characteristics, with subthreshold PTSD (defined as having one to three symptoms) entered as a separate disorder. We performed logistic regression to assess the association between subthreshold PTSD symptoms and current suicidal ideation, controlling for background demographic characteristics and for the presence of major depressive disorder. Controlling for major depressive disorder represents a rigorous test of our hypothesis, given the high rate of comorbid major depressive disorder found in PTSD. Results are expressed as adjusted odds ratios with 95% confidence intervals (CIs) for logistic regression or as beta values (labeled as “expected rise in impairment score”) for linear regression.
Results
Table 1 presents demographic data. Of the total study group of 9,358 individuals, 2,608 (27.9%) reported at least one PTSD symptom persisting at least 1 month after a traumatic event. Among the total study group, 844 individuals (9.0%) met full screening criteria for PTSD and 1,764 (18.9%) reported subthreshold symptoms (Table 2).
Impairment, number of comorbid anxiety disorders, and likelihood of meeting screening criteria for major depressive disorder increased significantly with each incremental increase in number of PTSD symptoms from one to four (Table 2). These variables also showed the following positive correlations with number of PTSD symptoms: impairment, r=0.25; number of comorbid disorders r=0.31; presence of comorbid major depressive disorder, r=0.27 (for all correlations, p<0.0001). Numbers of current comorbid anxiety disorders and rates of comorbid major depressive disorder increased significantly with each incremental increase in number of PTSD symptoms from one to four (Table 2).
The ANOVA was highly significant for all three variables, and post hoc comparisons (Scheffé method, data not shown) revealed significant increases in impairment, number of comorbid disorders, and major depressive disorder with each incremental increase in number of PTSD symptoms from one to four (post hoc comparisons are available on request). No significant differences in impairment, comorbid anxiety disorders, or comorbid major depressive disorder were found between the groups with no PTSD symptoms and those with one symptom. When examined separately for men and women, the mean values and patterns were not substantially different.
The proportion of subjects stating that they had thought of suicide in the last month also increased with the number of PTSD symptoms, from 9% for those with no PTSD symptoms to 33% for those with four PTSD symptoms (Table 3). Chi-square was highly significant (χ2=452.53, df=4, p<0.001).
When we applied linear regression to assess the contribution of subthreshold PTSD to impairment after controlling for demographic variables, we found that subthreshold PTSD made a modest, statistically significant contribution to impairment (Table 4).
When we applied logistic regression to assess the contribution of subthreshold PTSD to current suicidal ideation relative to other disorders, controlling for major depressive disorder and demographic variables, we found that age and race were not related to suicidal ideation but that men were 1.6 times more likely than women to report current suicidal ideation. The presence of subthreshold PTSD increased the risk of suicidal ideation by an odds ratio of 1.73 (Table 4, Figure 1). It is notable that this is comparable to the odds ratio for full PTSD (Table 4), which, in turn, has the highest risk for suicidal ideation after major depressive disorder. As expected, major depressive disorder was the largest contributor to risk for suicidal ideation (Table 4).
Discussion
Among individuals in the community seeking information about anxiety disorders, subthreshold PTSD symptoms were associated with incremental increases in degree of impairment, number of comorbid anxiety disorders, rate of major depressive disorder, and rate of current suicidal ideation. About one-fourth (27.9%) of the study group reported at least one PTSD symptom, 9.0% had full PTSD, and 18.9% had from one to three subthreshold PTSD symptoms. Compared with the lifetime prevalence of 7.8% found in the National Comorbidity Survey (19), our study group was more symptomatic, consistent with the fact that the subjects were seeking treatment.
The higher rates of impairment, comorbidity, and suicidal ideation seen with higher numbers of PTSD symptoms were both statistically and clinically significant in this highly symptomatic group of individuals. For example, the rates of impairment, comorbid anxiety disorders, and comorbid major depressive disorder were 31.5%, 68.5%, and 90.7% higher, respectively, among the subjects with four PTSD symptoms than among the subjects with no PTSD symptoms (Table 2).
The finding of high comorbidity in subthreshold PTSD extends findings of the National Comorbidity Survey (19), in which 59% of women and 43% of men who met the full screening criteria for PTSD also met criteria for three or more other disorders. In our study group, meeting the full criteria for PTSD was associated with meeting criteria for an average of 2.7 other diagnoses, despite the fact that only a limited number of disorders was assessed.
To our knowledge, this is the first study to examine comorbidity in subthreshold PTSD and the relative contribution of subthreshold PTSD symptoms to overall impairment relative to comorbid diagnoses. As noted by Stein et al. (12), the absence of comorbidity data has limited interpretation of findings in partial PTSD to date. Our study suggests that comorbidity is common and is an important factor in understanding clinical impairment in subthreshold PTSD. Subthreshold PTSD also contributed independently to level of impairment. Subthreshold PTSD was associated with a significant rise of 0.15 on our impairment scale, comparable to rises of 0.17 for full PTSD and 0.55 for major depressive disorder.
Of more importance, we found that subthreshold PTSD was associated with a significantly higher risk for current suicidal ideation, similar to that of OCD and higher than that of panic disorder or social phobia, after controlling for the presence of major depressive disorder (Table 4). This finding is consistent with previous research documenting subthreshold PTSD as a serious clinical problem (1, 12–14) and contributes to the literature demonstrating that suicidal thinking and attempts are not limited to major depressive disorder (24). More than three times as many individuals with full PTSD reported current suicidal ideation than those with no PTSD symptoms (Table 3). Although greater risk for suicidal ideation and attempts has been shown in both combat-related and non-combat-related PTSD, previous studies have not clearly demonstrated that the relationship between PTSD and suicide is not explained by the presence of depressive symptoms (5, 25–30).
There are several possible interpretations of the high rates of comorbidity observed in full and subthreshold PTSD. First, psychiatric disorder may have preceded the criterion A trauma, leading to greater vulnerability to developing PTSD symptoms (17, 31, 32). Second, comorbid affective and anxiety disorders may be secondary to the traumatic experiences and PTSD (19, 33). Third, and perhaps most important, there may be differences in rates of exposure to traumatic events between patients with and those without psychiatric illness. Individuals with greater comorbidity may have been exposed to more severe and/or recurrent trauma, explaining the higher number of PTSD symptoms in those with greater comorbidity. These questions can be examined in future cross-sectional and longitudinal studies.
There are a number of limitations intrinsic to this study. The screening instrument probe for trauma criterion A listed only five examples of typical traumatic experiences. This approach probably underestimates rates of PTSD symptoms, given that a greater number of trauma criterion A probes would likely further enhance reporting of traumatic events (12, 19). Traumatic events are typically underreported in adult surveys (34).
The lack of data on specific traumatic events and age at onset of symptoms also limits interpretation of our findings. These data will be examined in future Anxiety Disorder Screening Day assessments. Without these data we are unable to determine whether our findings are explained by differences in the type and severity of traumatic experiences and whether the trauma preceded or followed the onset of comorbid anxiety disorders and/or major depressive disorder. Finally, our estimate of impairment relies on self-report and does not assess more specific domains such as social, occupational, or family functioning.
The large number of subjects studied and their broad distribution across the United States are strengths of this study. Although diagnostic interviews would have been preferable, the screening instrument used was compared with structured interview and found to possess acceptable psychometric properties. In addition, we believe the use of videotaped clinical examples and the review of the questionnaire by a volunteer mental health professional enhanced the validity of the data collected.
Our findings, consistent with previous reports on subthreshold PTSD, call attention to the need to expand research beyond the boundaries of full syndromal criteria for PTSD. Our data in fact may be more consistent with a dimensional model of posttraumatic symptoms. In any case, this study provides justification for continued debate regarding nosologic approaches to posttraumatic sequelae (35). The important public health implication of these findings is that substantially greater numbers of individuals experience disability after trauma than is suggested by simply considering rates of full PTSD. This question might be examined in future epidemiologic studies by conducting a complete assessment for traumatic events and PTSD symptoms regardless of diagnostic status. Comorbid disorders and subthreshold symptoms also deserve further study in clinical trials of PTSD.
 |
 |
 |
 |
Received April 5, 2000; revision received Nov. 13, 2000; accepted Feb. 21, 2001. From the New York State Psychiatric Institute, Columbia University College of Physicians and Surgeons, New York; and the Mailman School of Public Health, Columbia University. Address reprint requests to Dr. Marshall, Director of Trauma Studies, Anxiety Disorders Clinic, Unit 69, New York State Psychiatric Institute, 1051 Riverside Dr., New York, NY 10032; [email protected] (e-mail). Supported in part by NIMH grants MH-01412 and MH-15144, a grant from the National Alliance for Research on Schizophrenia and Depression (Dr. Blanco), and the Lowenstein Foundation (Dr. Marshall).
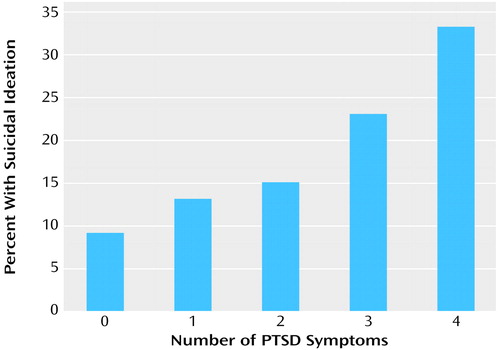
Figure 1. Rates of Suicidal Ideation in the Last Month and Number of PTSD Symptoms Among 9,358 Subjects Screened on National Anxiety Disorders Screening Day 1997a
aTable 4 shows the association between subthreshold PTSD and other psychiatric disorders and current suicidal ideation.
1. Blanchard EB, Hickling EJ, Barton KA, Taylor AE, Loos WR, Jones-Alexander J: One year prospective follow-up of motor vehicle accident victims. Behav Res Ther 1996; 34:775-786Crossref, Medline, Google Scholar
2. Davidson JRT, Hughes D, Blazer D, George LK: Posttraumatic stress disorder in the community: an epidemiological study. Psychol Med 1991; 21:1-19Crossref, Medline, Google Scholar
3. McFarlane AC, Atchison M, Rafalowicz E, Papay P: Physical symptoms in post-traumatic stress disorder. J Psychosom Res 1994; 38:715-726Crossref, Medline, Google Scholar
4. Cordova MJ, Andrykowski MA, Kenady DE, McGrath PC, Sloan DA, Red WH: Frequency and correlates of posttraumatic-stress-disorder-like symptoms after treatment for breast cancer. J Consult Clin Psychol 1995; 63:981-986Crossref, Medline, Google Scholar
5. Ferrada-Noli M, Asberg M, Ormstad K, Lundin T, Sundbom E: Suicidal behavior after severe trauma, part 1: PTSD diagnoses, psychiatric comorbidity, and assessments of suicidal behavior. J Trauma Stress 1998; 11:103-112Crossref, Medline, Google Scholar
6. Wenninger K, Heiman JR: Relating body image to psychological and sexual functioning in child sexual abuse survivors. J Trauma Stress 1998; 11:543-562Crossref, Medline, Google Scholar
7. Riggs DS, Byrne CA, Weathers FW, Litz BT: The quality of the intimate relationships of male Vietnam veterans: problems associated with posttraumatic stress disorder. J Trauma Stress 1998; 11:87-102Crossref, Medline, Google Scholar
8. Beckham JC, Lytle BL, Feldman ME: Caregiver burden in partners of Vietnam war veterans with posttraumatic stress disorder. J Consult Clin Psychol 1996; 64:1068-1072Google Scholar
9. Blanchard EB, Buckley TC, Hickling EJ, Taylor AE: Posttraumatic stress disorder and comorbid major depression: is the correlation an illusion? J Anxiety Disord 1998; 12:21-37Crossref, Medline, Google Scholar
10. Wagner D, Heinrichs M, Ehlert U: Prevalence of symptoms of posttraumatic stress disorder in German professional firefighters. Am J Psychiatry 1998; 155:1727-1732Google Scholar
11. Pincus HA, Davis WW, McQueen LE: Subthreshold mental disorders: a review and synthesis of studies on minor depression and other “brand names.” Br J Psychiatry 1999; 174:288-296Crossref, Medline, Google Scholar
12. Stein MB, Walker JR, Hazen AL, Forde DR: Full and partial posttraumatic stress disorder: findings from a community survey. Am J Psychiatry 1997; 154:1114-1119Google Scholar
13. Weiss DS, Marmar CR, Schlenger WE, Fairbank JA, Jordan BK, Hough RL, Kulka RA: The prevalence of lifetime and partial post-traumatic stress disorder in Vietnam theater veterans. J Trauma Stress 1992; 5:365-376Crossref, Google Scholar
14. Carlier IV, Gersons BP: Partial posttraumatic stress disorder (PTSD): the issue of psychological scars and the occurrence of PTSD symptoms. J Nerv Ment Dis 1995; 183:107-109Crossref, Medline, Google Scholar
15. Schutzwohl M, Maercker A: Effects of varying diagnostic criteria for posttraumatic stress disorder are endorsing the concept of partial PTSD. J Trauma Stress 1999; 12:155-165Crossref, Medline, Google Scholar
16. Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS: Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. New York, Brunner/Mazel, 1990Google Scholar
17. Helzer JE, Robins LN, McEvoy L: Posttraumatic stress disorder in the general population: findings of the Epidemiologic Catchment Area survey. N Engl J Med 1987; 317:1630-1634Google Scholar
18. Breslau N, Davis GC, Andreski P, Peterson E: Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry 1991; 48:216-222Crossref, Medline, Google Scholar
19. Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB: Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995; 52:1048-1060Google Scholar
20. Spitzer RL, Kroenke K, Linzer M, Hahn SR, Williams JBW, deGruy FV III, Brody D, Davies M: Health-related quality of life in primary care patients with mental disorders: results from the PRIME-MD 1000 study. JAMA 1995; 274:1511-1517Google Scholar
21. Olfson M, Fireman B, Weissman MM, Leon AC, Sheehan DV, Kathol RG, Hoven C, Farber L: Mental disorders and disability among patients in a primary care group practice. Am J Psychiatry 1997; 154:1734-1740Google Scholar
22. Ormel J, VonKorff M, Ustun TB, Pini S, Korten A, Oldehinkel T: Common mental disorders and disability across cultures: results from the WHO Collaborative Study on Psychological Problems in General Health Care. JAMA 1994; 272:1741-1748Google Scholar
23. Landis JR, Koch GG: The measurement of observer agreement for categorical data. Biometrics 1977; 33:159-174Crossref, Medline, Google Scholar
24. Weissman MM, Klerman GL, Markowitz JS, Ouellette R: Suicidal ideation and suicide attempts in panic disorder and attacks. N Engl J Med 1990; 321:1209-1214Google Scholar
25. Lundin T: Morbidity following sudden and unexpected bereavement. Br J Psychiatry 1984; 144:84-88Crossref, Medline, Google Scholar
26. Kilpatrick DG, Best CL, Veronen LJ: Mental health correlates of criminal victimization. J Consult Clin Psychol 1985; 53:866-873Crossref, Medline, Google Scholar
27. Miller TW, Martin W, Spiro K: Traumatic stress disorder: diagnostic and clinical issues in former prisoners of war. Compr Psychiatry 1989; 30:139-148Crossref, Medline, Google Scholar
28. Somasundraram D: Psychiatric morbidity due to war in Northern Sri Lanka, in International Handbook of Traumatic Stress Syndromes. Edited by Wilson JP, Raphael B. New York, Plenum, 1993, pp 333-348Google Scholar
29. Kramer TL, Lindy JD, Green BL, Grace MC, Leonard AC: The comorbidity of post-traumatic stress disorder and suicidality in Vietnam veterans. Suicide Life Threat Behav 1994; 24:58-67Medline, Google Scholar
30. Loughrey GC, Curran PS, Bell P: Posttraumatic stress disorder and civil violence in Northern Ireland, in International Handbook of Traumatic Stress Syndromes. Edited by Wilson JP, Raphael B. New York, Plenum, 1992, pp 377-383Google Scholar
31. Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL: Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J Consult Clin Psychol 1993; 61:984-991Crossref, Medline, Google Scholar
32. Davidson JRT, Kudler HS, Saunders WB, Smith SD: Symptom and morbidity patterns in World War II and Vietnam veterans with posttraumatic stress disorder. Compr Psychiatry 1990; 31:162-170Crossref, Medline, Google Scholar
33. Shalev AY, Freedman S, Peri T, Brandes D, Sahar T: Predicting PTSD in trauma survivors: prospective evaluation of self-report and clinician-administered instruments. Br J Psychiatry 1997; 170:558-564Crossref, Medline, Google Scholar
34. Widom C, Morris S: Accuracy of adult recollections of childhood victimization, part 2: childhood sexual abuse. Psychol Assess 1997; 9:34-46Crossref, Google Scholar
35. Marshall RD, Spitzer R, Liebowitz MR: Review and critique of the new DSM-IV diagnosis of acute stress disorder. Am J Psychiatry 1999; 156:1677-1685Google Scholar



