Effect of Clozapine on Caudate Nucleus Volume in Relation to Symptoms of Schizophrenia
Abstract
OBJECTIVE: Studies have found that caudate volume increased after treatment with typical antipsychotics in patients with schizophrenia but decreased after treatment was changed to clozapine. In the current study the authors examined whether this volume decrease was related to clinical improvement. METHOD: Twenty-eight patients with schizophrenia who had not responded to treatment with typical antipsychotics were included in the study; 22 completed the study. Caudate volume was assessed by using magnetic resonance imaging during treatment with typical antipsychotics and after 24 weeks and 52 weeks of clozapine treatment. Symptoms were assessed just before clozapine treatment and once a month thereafter. RESULTS: Clozapine treatment resulted in a significant reduction in left caudate volume in patients who responded to the drug but not in patients who did not respond to clozapine at 52 weeks of treatment. Overall, the degree of reduction in left caudate volume was significantly related to the extent of improvement in positive and general symptoms but not in negative symptoms. CONCLUSIONS: These findings suggest that the caudate nucleus plays a role in the positive and general symptoms of schizophrenia.
According to magnetic resonance imaging (MRI), an increase in the caudate volume of patients with schizophrenia was found after treatment with typical antipsychotics (1, 2), but the clinical relevance of this increase remains unclear. Chakos et al. (2) found no correlation between caudate volume increase and symptom improvement during treatment with typical antipsychotics. However, larger caudate volumes after typical antipsychotic treatment were associated with poorer neuropsychological test performance (1), the deficit syndrome (3), and greater severity of symptoms (4), suggesting that medication-induced hypertrophy of the caudate nucleus may moderate the clinical effects of antipsychotic treatment (4). When patients switched from treatment with typical antipsychotics to treatment with the atypical antipsychotic clozapine, a decrease in caudate volume was found (5, 6).
This study investigated the effects of switching from treatment with typical antipsychotics to clozapine on caudate volume and clinical symptoms after 52 weeks of clozapine treatment in a group of patients with schizophrenia who were not responding to treatment with typical antipsychotics. The current study is an extension of our earlier study (6), which examined patients after treatment with clozapine for 24 weeks. We found a significant decrease in caudate volume in that study, but this decrease was not significantly correlated with symptom improvement. Since the optimal clinical efficacy of clozapine may not be reached until after 6 months of treatment (7), we hypothesized that caudate volume change would be related to change in symptoms after a prolonged period of clozapine treatment (52 weeks).
Method
Twenty-eight patients with schizophrenia (mean age=35 years, SD=10) participated in the study. All patients were treated at the University Medical Center in Utrecht. Patients were evaluated with the Comprehensive Assessment of Symptoms and History interview (8), and all met DSM-IV criteria for schizophrenia. Patients had been treated with typical antipsychotics for a minimum of 4 weeks (mean duration of treatment was 103 months, SD=101, and mean lifetime dose of haloperidol equivalent was 10.4 mg/day, SD=7.1). All had failed to show adequate responses according to criteria described elsewhere (6). Six patients did not complete the study because they refused further participation (N=1) or needed other psychotropic medication (N=5). After a complete description of the study, written informed consent was obtained from all subjects.
Patients were withdrawn from typical antipsychotics and then treated with clozapine for 52 weeks (mean dose of clozapine=346 mg/day, SD=61). MRI was used to assess neuroanatomical variables before the typical antipsychotics were withdrawn, after 24 weeks of clozapine treatment, and after 52 weeks of clozapine treatment. Psychopathology was rated just before clozapine treatment and once a month thereafter by using the Positive and Negative Syndrome Scale (9). A 20% or greater reduction in total Positive and Negative Syndrome Scale score from baseline to week 52 was defined a priori as treatment response. Additional information about assessment and MRI procedures is available in our previous report (6).
Analysis of caudate volume was performed by using repeated measures analysis of variance with the factors time (during typical antipsychotic treatment, after 24 weeks of clozapine treatment, and after 52 weeks of clozapine treatment), side (right and left caudate nucleus), and group (patients who responded to clozapine [N=16] and patients who did not respond to clozapine [N=6]).
Paired t tests were performed to compare change in caudate volume or Positive and Negative Syndrome Scale score at week 24 of clozapine treatment compared with baseline and at week 52 compared with week 24 of clozapine treatment.
Regression analysis was used to examine the relationship between caudate volume change following 24 weeks or 52 weeks of clozapine treatment and degree of psychiatric symptom improvement after 52 weeks of clozapine treatment.
Results
After 52 weeks of clozapine treatment, patients who responded to clozapine showed a significant difference from those who did not respond to clozapine in caudate volume change between the left and right caudate nucleus (F=3.4, df=2, 19, p<0.05). Clozapine treatment significantly reduced left (F=3.9, df=2, 20, p<0.05) but not right (F=2.4, df=2, 20, p=0.11) caudate volume over time. The change in left caudate volume was significant in responders (F=7.8, df=2, 14, p<0.005) but not in nonresponders (F=0.65, df=2, 4, p=0.55). The change in left caudate volume was significant after 24 weeks of clozapine treatment compared with baseline (t=3.1, df=1, 26, p<0.005) but not at week 52 compared with week 24 (t=–0.2, df=1, 21, p=0.85).
Clozapine treatment significantly improved symptoms over time (all symptoms: F=25.2, df=2, 24, p<0.001; positive symptoms: F=22.7, df=2, 24, p<0.001; negative symptoms: F=8.7, df=2, 24, p<0.005; general symptoms: F=15.7, df=2, 24, p<0.001). Post hoc analysis showed a significant improvement in Positive and Negative Syndrome Scale score after 24 weeks of clozapine treatment compared with baseline (t=4.4, df=1, 26, p<0.001) and at week 52 compared with week 24 (t=2.9, df=1, 22, p<0.01).
Across all subjects, change in left caudate volume was significantly related to symptom improvement after 52 weeks of clozapine treatment (F=8.0, df=1, 20, p<0.05) (Figure 1). A significant relationship between left caudate volume change and a reduction in positive symptoms (F=7.1, df=1, 20, p<0.05) and general symptoms (F=8.4, df=1, 20, p<0.01) but not in negative symptoms (F=2.0, df=1, 20, p=0.17) was found.
No relationship was found between caudate volume change after 24 weeks and symptom improvement after 52 weeks of clozapine treatment (F=2.13, df=1, 23, p=0.16).
Discussion
This study revealed that 52 weeks of clozapine treatment significantly reduced left caudate volume in patients with schizophrenia who had been treated previously with typical antipsychotics. This reduction was limited to responders to clozapine treatment. Moreover, the degree of left caudate volume decrease was significantly correlated with the extent of improvement in positive and general symptoms but not in negative symptoms across all subjects. The decrease in left caudate volume occurred at 24 weeks, but symptom improvement continued up to 52 weeks of treatment.
Our data are consistent with those of previous studies reporting a decrease in caudate volume after clozapine treatment (5) and symptom improvement beyond 24 weeks of clozapine treatment (7). The fact that we found no significant relationship between caudate volume reduction after 24 weeks and symptom improvement after 52 weeks suggests that, beyond 24 weeks of clozapine treatment, symptom improvement may reflect a further (although not significant) adaptation of the brain.
Treatment with typical antipsychotics leads to an increase in caudate volume, particularly on the left side (2, 3). This volume increase may be an ineffective adaptation, as was suggested by Gur et al. (4), since large caudate volumes were associated with greater severity of symptoms (1, 3, 4). In contrast, clozapine lowers caudate volume in patients previously treated with typical antipsychotics (5). It may be postulated that this is a restoring effect, “correcting” the unwanted increase after treatment with typical antipsychotics, since caudate volume decrease is associated with symptom improvement.
It should be noted that the present study included only patients who had not responded to typical antipsychotics. Therefore, results may not be generalizable to all patients with schizophrenia.
To conclude, this study found that switching from treatment with typical antipsychotics to clozapine resulted in a significant decrease in the left caudate volume in patients with refractory schizophrenia who responded to clozapine. This reduction was related to improvement in positive and general symptoms when clozapine treatment was extended over 52 weeks. These results suggest that the caudate nucleus may play a role in the positive and general symptoms of schizophrenia.
Received Aug. 7, 2000; revision received Nov. 17, 2000; accepted Nov. 27, 2000. From the University Medical Center, Department of Psychiatry, Utrecht. Address reprint requests to Dr. Scheepers, University Medical Center, Department of Psychiatry (A00.241), P.O. Box 85500, 3508 GA Utrecht, Netherlands; [email protected] (e-mail). Supported in part by Novartis Pharma B.V. medical research department. The authors thank Herman J. Wynne, Ph.D., for statistical advice.
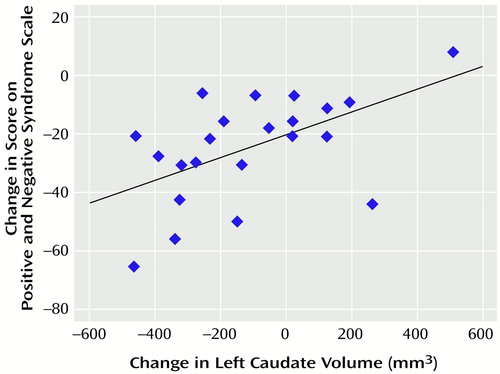
Figure 1. Correlation Between Change in Left Caudate Volume and Improvement of Symptoms in 22 Patients With Schizophrenia After 52 Weeks of Clozapine Treatmenta
ar=0.54, N=22, p<0.01.
1. Hokama H, Shenton ME, Nestor PG, Kikinis R, Levitt JJ, Metcalf D, Wible CG, O’Donnell BF, Jolesz FA, McCarley RW: Caudate, putamen, and globus pallidus volume in schizophrenia: a quantitative MRI study. Psychiatry Res Neuroimaging 1995; 61:209–229Crossref, Medline, Google Scholar
2. Chakos MH, Lieberman JA, Bilder RM, Borenstein M, Lerner G, Bogerts B, Wu H, Kinon B, Ashtari M: Increase in caudate nuclei volumes of first-episode schizophrenic patients taking antipsychotic drugs. Am J Psychiatry 1994; 151:1430–1436Google Scholar
3. Buchanan R, Breier A, Kirkpatrick B, Elkashef A, Munson R, Gellad F, Carpenter W: Structural abnormalities in deficit and nondeficit schizophrenia. Am J Psychiatry 1993; 150:59–65Link, Google Scholar
4. Gur RE, Maany V, Mozley PD, Swanson C, Bilker W, Gur RC: Subcortical MRI volumes in neuroleptic-naive and treated patients with schizophrenia. Am J Psychiatry 1998; 155:1711–1717Google Scholar
5. Chakos MH, Lieberman JA, Alvir J, Bilder R, Ashtari M: Caudate nuclei volumes in schizophrenic patients treated with typical antipsychotics or clozapine. Lancet 1995; 345:456–457Crossref, Medline, Google Scholar
6. Scheepers FE, Gispen de Wied CC, Hulshoff Pol HE, van der Flier W, van der Linden JA, Kahn RS: The effect of clozapine on caudate nucleus volume in schizophrenic patients previously treated with typical antipsychotics. Neuropsychopharmacology 2001; 24:47–54Crossref, Medline, Google Scholar
7. Lieberman JA, Safferman AZ, Pollack S, Szymanski S, Johns C, Howard A, Kronig M, Bookstein P, Kane JM: Clinical effects of clozapine in chronic schizophrenia: response to treatment and predictors of outcome. Am J Psychiatry 1994; 151:1744–1752Google Scholar
8. Andreasen NC, Flaum M, Arndt S: The Comprehensive Assessment of Symptoms and History (CASH): an instrument for assessing diagnosis and psychopathology. Arch Gen Psychiatry 1992; 49:615–623Crossref, Medline, Google Scholar
9. Kay SR, Fiszbein A, Opler LA: The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull 1987; 13:261–276Crossref, Medline, Google Scholar



