Insight Into Illness in Schizophrenia, Schizoaffective Disorder, and Mood Disorders With Psychotic Features
Abstract
OBJECTIVE: Deficits in insight have been found in one study to be more common and severe in patients with schizophrenia than in patients with schizoaffective and major depression with and without psychosis but not more severe than they are in patients with bipolar disorder. The goals of this study were to replicate this finding independently and to clarify whether patients with schizophrenia differ from patients with bipolar disorder in a larger study group. METHOD: Using the Scale to Assess Unawareness of Mental Disorder, the authors evaluated 29 inpatients with schizophrenia, 24 with schizoaffective disorder, and 183 with mood disorders with psychotic features (153 with bipolar disorder and 30 with unipolar depression). RESULTS: Patients with schizophrenia had poorer insight than patients with schizoaffective disorder and patients with psychotic unipolar depression but did not differ from patients with bipolar disorder. CONCLUSIONS: The lack of significant differences between patients with schizophrenia and patients with bipolar disorder was not a result of low statistical power. This replication and more detailed examination of diagnostic group differences in insight have clinical, theoretical, and nosological implications.
Poor insight into illness in schizophrenia has been shown to be associated with neurocognitive deficits, poorer course of illness, and lack of adherence to treatment (1–3). A study conducted by a group involving one of us (X.F.A.) (2) found poor insight into illness to be more common in patients with schizophrenia than in patients with schizoaffective and major depressive disorders with and without psychotic features. This earlier study found that diagnostic group differences existed on nearly every dimension of insight examined and that these differences were not accounted for by severity of psychosis. In addition, less awareness of several aspects of mental disorder was associated with poorer psychosocial functioning in patients with schizophrenia (2–4). A small group of patients with bipolar disorder was also studied (2) and did not differ significantly from the patients with schizophrenia; however, the small number of subjects in this study limits the interpretation of this result.
The aims of the current study were to replicate the findings reported previously and to provide further details on the nature of poor insight in psychotic disorders. The present study, unlike the earlier study (2), included patients with bipolar mixed and bipolar depressed diagnoses. We also examined retrospective insight in addition to current insight and used a newer form of the Scale to Assess Unawareness of Mental Disorders (2, 4). The newer scale has greater sensitivity to differing levels of awareness of illness.
Method
Patients were recruited from the University of Pisa Comorbidity in Psychosis Project. The method of study is described in more detail elsewhere (5). Two hundred thirty-six consecutively hospitalized psychotic patients met the following criteria: 1) age over 16 years and 2) presence of psychotic symptoms (formal thought disorders, delusions, hallucinations, and/or grossly disorganized behavior). Patients were excluded from the study if their psychotic symptoms were secondary to acute intoxication or withdrawal from psychotropic substances or a severe medical condition (epilepsy, dementia, brain vascular disease). Each patient participated voluntarily in this study after providing written informed consent.
Patients were assessed 1 week before hospital discharge with the Structured Clinical Interview for DSM-III-R—Patient Version 1.0 (SCID-P) (6), the Brief Psychiatric Rating Scale (BPRS) (7), and the Hopkins Symptom Checklist (SCL-90) (8). Overall judgment of each patient’s social and occupational functioning was obtained by using the Global Assessment of Functioning Scale (SCID-P axis V). Insight was assessed by using the Scale to Assess Unawareness of Mental Disorders (2, 4), which assesses awareness of mental disorder, awareness of response to medication, awareness of social consequences of mental disorder, and awareness of specific symptoms of the illness. We use the term “insight” to encompass all of the aforementioned dimensions unless otherwise stated. Higher scores on this scale indicate less insight.
The SCID-P interviews and psychopathology ratings were performed by three research psychiatrists. Interrater reliability was assessed for 24 interviews with eight patients. Kappas ranged from 0.90 and 1.00 for diagnoses. The intraclass correlation (ICC) for total BPRS score was 0.85, and ICCs ranged from 0.78 and 0.90 for the three general items of the Scale to Assess Unawareness of Mental Disorders.
The chi-square test was used to analyze categorical variables, and post hoc pairwise comparisons were performed to inspect adjusted standardized residuals. One-way analysis of variance (ANOVA) with post hoc pairwise comparisons and analysis of covariance (ANCOVA) were used to analyze continuous variables. An alpha level of 0.05 was used. The power analysis was conducted by using the program nQuery Advisor 1.0. The effect size (Δ2) for the one-way ANOVAs with unequal sample size was computed as the variance of means divided by the common standard deviation squared.
Results
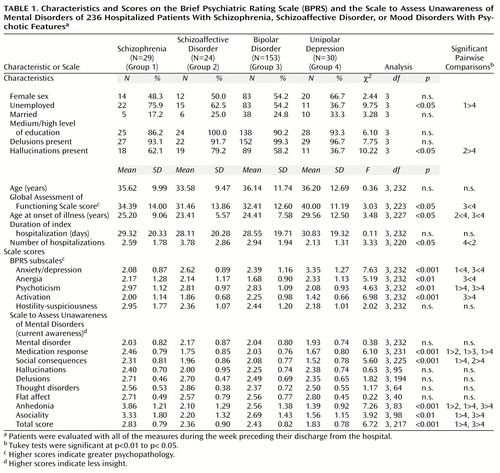
Twenty-nine of the 236 patients met DSM-III-R criteria for schizophrenia, 24 for schizoaffective disorder, 153 for bipolar disorder (67 manic, 46 mixed, 37 depressed, and three with missing subtype), and 30 for unipolar depression. As shown in Table 1, the four groups did not differ significantly in any demographic and clinical characteristics except unemployment status, frequency of hallucinations, Global Assessment of Functioning Scale score, age at onset of illness, and number of hospitalizations.
Table 1 also shows that an ANOVA comparing items from the Scale to Assess Unawareness of Mental Disorders among the four diagnostic groups revealed a main effect of diagnostic group for current awareness of response to medication, social consequences of mental disorder, anhedonia, asociality, and total score (summary of symptoms).
The extant empirical literature indicates that poorer insight and overall level of functioning are often positively correlated independent of diagnosis. To examine whether diagnostic group differences in level of insight could be explained by differences in overall level of functioning, we conducted an ANCOVA comparing insight among the diagnostic groups while controlling for Global Assessment of Functioning Scale scores. A main effect of diagnosis held for awareness of response to medication (F=5.18, df=3, 231, p<0.002), awareness of social consequences of current illness (F=4.38, df=3, 225, p<0.005), awareness of anhedonia (F=6.64, df=3, 83, p<0.001), awareness of asociality (F=3.18, df=3, 98, p<0.05), and the total current awareness score (summary of symptoms) (F=10.83, df=3, 164, p<0.001).
Several dimensions of insight were significantly correlated with Global Assessment of Functioning Scale scores; these ranged from F=–0.33 (df=3, 83, p<0.01) for awareness of anhedonia to F=–0.27 (df=3, 98, p<0.05) for awareness of asociality. All correlations were in the direction of an association between poorer insight and poorer psychosocial functioning.
Compared with patients who had schizoaffective disorder, patients with schizophrenia had poorer retrospective awareness of response to medication (F=3.09, df=3, 186, p<0.03) and poorer retrospective awareness of past mental disorder (F=4.66, df=3, 188, p<0.004). Similarly, compared with patients who had bipolar disorder, patients with schizophrenia had poorer retrospective awareness of previous response to medication (F=3.09, df=3, 186, p<0.03). The patients with schizophrenia also had worse retrospective awareness of past mental disorder (F=4.66, df=3, 188, p<0.002) and past social consequences (F=2.76, df=3, 180, p<0.05) than did patients with unipolar depression with psychotic features.
An ANCOVA comparing diagnostic groups on retrospective insight that controlled for Global Assessment of Functioning Scale scores yielded a main effect of diagnosis for retrospective awareness of mental disorder (F=4.21, df=3, 188, p<0.007), previous response to medication (F=2.88, df=3, 186, p<0.05), and past social consequences of the illness (F=2.90, df=3, 180, p<0.05).
Discussion
The results of the current study replicate nearly every finding of the earlier report by Amador et al. (2). Patients with schizophrenia had poorer insight than patients with schizoaffective disorder and patients with psychotic unipolar depression. The patients with bipolar and unipolar depression in the current study were more heterogeneous than those in the previous study, increasing the generalizability of the results. The BPRS scores indicate that, on the whole, all patient groups were not in an acute episode but were also not entirely symptom free when evaluated. The greater statistical power associated with our larger study group may account for the effects of diagnosis being more pronounced.
As was found in the earlier study (2), patients with bipolar disorder did not differ substantially in level of insight from patients with schizophrenia. However, in the current study, the lack of statistically significant differences was not likely due to low power. In fact, if the conventional effect size of 0.20 is adopted, the power to detect the observed differences at the 0.01 level was 82%, 89%, 99%, and 99%, respectively, for awareness of anhedonia, asociality, medication response, and social consequences of the illness.
This replication and more detailed examination of diagnostic group differences in insight has clinical, theoretical, and nosological value (9–11). Future studies should examine whether patients with bipolar disorder with very poor insight show a pattern of neurocognitive deficit similar to that found in schizophrenia and whether level of insight is related to state versus traits in this group.
There are several limitations to the design of this study. Although raters were blind to the study hypotheses, the assessments were not blinded to one another. In addition, estimates of interrater reliability on principal diagnoses and Scale to Assess Unawareness of Mental Disorders scores were obtained on a small subset of patients. The number of previous hospitalizations differed among groups; whether this was a function of differences in insight or severity of illness could not be addressed.
 |
Received July 6, 1999; revisions received Jan. 27 and June 13, 2000; accepted June 30, 2000. From the Department of Psychiatry, University of Pisa, Pisa, Italy; and the Diagnosis and Treatment Research Core of the NIMH Mental Health Clinical Research Center, New York State Psychiatric Institute. Address reprint requests to Dr. Amador, Department of Psychology, New York State Psychiatric Institute, 1051 Riverside Drive, Unit 2, New York, NY 10032; [email protected] (e-mail). Supported in part by NIMH grant MH-59342 and by grants from the Stanley Foundation, the National Alliance for Research on Schizophrenia and Depression, and Worldwide Clinical Trials. The authors thank Dr. Raymond Goetz for statistical consultation.
1. Young DA, Zakzanis KK, Baily C, Davila R, Griese J, Sartory G, Thom A: Further parameters of insight and neuropsychological deficit in schizophrenia and other chronic mental disease. J Nerv Ment Dis 1998; 186:44–50Crossref, Medline, Google Scholar
2. Amador XF, Flaum M, Andreasen NC, Strauss DH, Yale SA, Clark S, Gorman JM: Awareness of illness in schizophrenia, schizoaffective and mood disorders. Arch Gen Psychiatry 1994; 51:826–836Crossref, Medline, Google Scholar
3. David A, van Os J, Jones P, Harvey I, Foerster A, Fahy T: Insight and psychotic illness: cross-sectional and longitudinal associations. Br J Psychiatry 1995; 167:621–628Crossref, Medline, Google Scholar
4. Amador XF, Strauss DH, Yale SA, Flaum MM, Endicott J, Gorman JM: Assessment of insight in psychosis. Am J Psychiatry 1993; 150:873–879Link, Google Scholar
5. Cassano GB, Pini S, Saettoni M, Rucci P, Dell’Osso L: Occurrence and clinical correlates of psychiatric comorbidity in patients with psychotic disorders. J Clin Psychiatry 1998; 59:60–68Crossref, Medline, Google Scholar
6. Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-III-R—Patient Version 1.0 (SCID-P). Washington, DC, American Psychiatric Press, 1990Google Scholar
7. Overall JE, Gorham DR: The Brief Psychiatric Rating Scale. Psychol Rep 1962; 10:799–812Crossref, Google Scholar
8. Derogatis LR, Lipman RS, Covi L: SCL-90: an outpatient psychiatric rating scale—preliminary report. Psychopharmacol Bull 1973; 9:13–28Medline, Google Scholar
9. Sanz M, Constable G, Lopez-Ibor I, Kemp R, David AS: A comparative study of insight scales and their relationship to psychological and clinical variables. Psychol Med 1998; 28:437–446Crossref, Medline, Google Scholar
10. Lam D, Wong G: Prodromes, coping strategies, insight and social functioning in bipolar affective disorders. Psychol Med 1997; 27:1091–1100Google Scholar
11. Ghaemi NS, Pope HG Jr: Lack of insight in psychotic and affective disorders: a review of empirical studies. Harv Rev Psychiatry 1994; 2:22–33Crossref, Medline, Google Scholar



