Bipolar Disorder at Prospective Follow-Up of Adults Who Had Prepubertal Major Depressive Disorder
Abstract
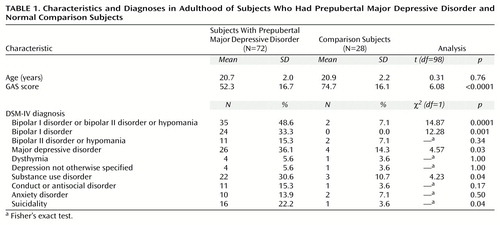
OBJECTIVE: The authors’ goal was to conduct an adult follow-up of subjects who had participated in a study of nortriptyline for childhood depression. METHOD: The study group represented 100 (90.9%) of the original 110 subjects and included 72 subjects who had a prepubertal diagnosis of major depressive disorder and 28 normal comparison subjects. Subjects were assessed with semistructured research interviews given by research nurses who were blind to the subjects’ original diagnoses. RESULTS: In the original study, the mean age of the children with prepubertal major depressive disorder was 10.3 years (SD=1.5); at adult follow-up the mean age of these subjects was 20.7 years (SD=2.0). At follow-up, significantly more of the subjects who had prepubertal diagnoses of major depressive disorder (N=24 [33.3%]) than normal comparison subjects (none) had bipolar I disorder. Subjects who had prepubertal diagnoses of major depressive disorder also had significantly higher rates of any bipolar disorder than normal subjects (48.6% [N=35] versus 7.1% [N=2]), major depressive disorder (36.1% [N=26] versus 14.3% [N=4]), substance use disorders (30.6% [N=22] versus 10.7% [N=3]), and suicidality (22.2% [N=16] versus 3.6% [N=1]). Parental and grandparental mania predicted bipolar I disorder outcomes. CONCLUSIONS: High rates of switching to mania have implications for the treatment of depressed children. The authors discuss the reasons for their finding a higher rate of bipolar disorder in this outcome study than was found in the one other adult outcome study of prepubertal major depressive disorder.
We conducted an adult follow-up of subjects from our study of nortriptyline in childhood (1, 2). The results of the original nortriptyline study and one other study of a tricyclic antidepressant for prepubertal major depressive disorder were negative (3). Possible reasons for the negative outcomes, including child versus adult age differences in relevant neurobiology, have been discussed elsewhere (1, 2).
Another hypothesis, which could be tested by a longitudinal paradigm, is that the children with prepubertal major depressive disorder had bipolar major depressive disorder (i.e., they had not yet had their first manic episode) (1, 2). The reason for considering a high rate of future bipolar disorder among prepubertal children with major depressive disorder was the high rate of positive family histories of major bipolar disorders in the nortriptyline study (1). This hypothesis was supported at the 2–5-year follow-up of subjects in the nortriptyline study (2), when 31.6% of the subjects with prepubertal major depressive disorder had switched to bipolar disorder.
Method
Details of the study design were reported previously (1, 2). In brief, an enriched sample of subjects from the nortriptyline study participants were compared with a group of aggregately matched normal comparison subjects.
In the original study, the 72 children with major depressive disorder were 10.3 years old (SD=1.5); all of these children were prepubertal (Tanner stage II or lower). Inclusion criteria were DSM-III major depressive disorder, duration of illness of 2 months or greater, and severity ratings of definite caseness. Exclusion criteria were pervasive developmental disorder, substance use disorders, schizophrenia, any bipolar disorder, and any major medical disorder. Children with comorbid attention deficit hyperactivity disorder (ADHD) were excluded from the study because the efficacy of tricyclic antidepressants for ADHD had been shown (3) and response of comorbid ADHD to the medication might confound ratings of prepubertal major depressive disorder. Children with psychosis were excluded because of the lack of efficacy of monotherapy with tricyclic antidepressants for psychotic major depressive disorder in adults (4).
The normal comparison children could not have any axis I diagnoses or a parent with recurrent major depressive disorder, any bipolar disorder, or any schizophrenia diagnosis. These low-risk normal comparison subjects were selected to optimize the investigation of normal adolescent behaviors compared with hypomanic symptoms.
At the adult assessment, research nurses with established interrater reliability who were blind to the subjects’ diagnoses interviewed the subjects by telephone. They used the Schedule for Schizophrenia and Affective Disorders—Lifetime Bipolar Version (5) to assess presence or absence of bipolar disorder during the most recent 5 years and the Global Assessment Scale (GAS) (6) to assess the presence or absence of the disorder at its worst. Interrater reliability was established when these interviewers had virtually 100% agreement for diagnoses five consecutive times as both interviewer and listener. Validation of the telephone interviews compared with in-person assessments was not performed; however, the validity of telephone interviews compared with in-person interviews has been reported (7). Diagnoses according to DSM-IV criteria were finalized in consensus conferences.
Interviews with the Family History Research Diagnostic Criteria (FH-RDC) (8) were administered to the mother to assess the proband’s parents and grandparents. Categories of bipolar disorders assessed with the FH-RDC in parents and grandparents were bipolar I disorder, mania, and schizoaffective disorder, manic type. Categories of bipolar II disorder and hypomania were not included because of their lower reliability (8).
The Human Studies Committee of Washington University in St. Louis approved the informed consent form or provided informed telephone consent after the consent form was mailed to them.
Chi-square and t tests were performed on demographic variables. Logistic regression was performed with the diagnosis of bipolar I disorder as the outcome measure among subjects with prepubertal major depressive disorder. Predictors used were proband gender, duration of baseline major depressive disorder episode, any lifetime antidepressant use, and parental and grandparental mania.
Results
The study group of 100 subjects represented 90.9% of the original 110 subjects and included 72 individuals who had prepubertal major depressive disorder and 28 normal comparison subjects. All 106 subjects who had been interviewed at the 2–5-year follow-up were located. Interviews were completed with 72 (91.1%) of the 79 original subjects with prepubertal major depressive disorder and 28 (90.3%) of the 31 original normal comparison subjects. Subjects who refused to participate did not significantly differ demographically from participants. The mean time between baseline and follow-up interviews was 9.9 years (SD=1.5).
Table 1 presents follow-up demographic information and DSM-IV diagnoses of the subjects who had prepubertal major depressive disorder and the normal subjects. In the logistic regression, the statistic for the overall model was χ2=12.16, df=4, p=0.02. Parental and grandparental mania predicted a bipolar I disorder outcome (χ2=5.09, df=1, p=0.02).
Discussion
We found a higher rate of bipolar disorder in this outcome study than was found in the one other published study of adult outcome of prepubertal major depressive disorder (9). This difference may be because the subjects in our study were severely and chronically ill and were from families with high rates of mood disorders (1, 2).
Two factors in the original nortriptyline study would have been expected to lower the rate of bipolar disorder outcomes. Exclusion of comorbid ADHD would be expected to lower the rate of switching to bipolar disorder because ADHD may be an initial manifestation of mania and is frequently comorbid with mania in children (10). Excluding children with psychotic prepubertal major depressive disorder from the original study may have had little effect because psychosis is uncommon in prepubertal major depressive disorder (11), but delusions are a predictor of switching to mania in adolescent major depressive disorder (12). Therefore, excluding psychosis would be expected to lower the rate of bipolar disorder outcomes.
We found higher rates of bipolar disorder in subjects who had prepubertal major depressive disorder than were found in similar outcome studies of adults with major depressive disorder (13). This finding is consistent with the possibility that subjects first examined in adulthood (possibly after switching from prepubertal major depressive disorder to mania in childhood) would simply be counted as having bipolar disorder.
Although the normal comparison subjects were at low risk for affective disorders (see Method section), the rate of major depressive disorder in these subjects at adult follow-up (14.3%) was similar to the rate (15.3%) reported for a community sample of adolescents and young adults (14). The reason for hypomania diagnoses in two of the normal comparison subjects is unclear.
High rates of switching to mania are an important consideration for treatment of prepubertal major depressive disorder because of concerns that antidepressants may worsen childhood mania (15).
 |
Received Dec. 1, 1999; revisions received March 15 and June 27, 2000; accepted July 27, 2000. From the Department of Psychiatry, Washington University School of Medicine. Address reprints to Dr. Geller, Department of Psychiatry, Washington University School of Medicine, 660 South Euclid Ave., Box 8134, St. Louis, MO 63110; [email protected] (e-mail). Supported by NIMH grant MH-40273 (Dr. Geller).
1. Geller B, Cooper TB, Graham DL, Fetner HH, Marsteller FA, Wells JM: Pharmacokinetically designed double-blind placebo-controlled study of nortriptyline in 6- to 12-year-olds with major depressive disorder. J Am Acad Child Adolesc Psychiatry 1992; 31:34–44Crossref, Medline, Google Scholar
2. Geller B, Clark K, Fox LW: Rate and predictors of prepubertal bipolarity during follow-up of 6- to 12-year-old depressed children. J Am Acad Child Adolesc Psychiatry 1994; 33:461–468Crossref, Medline, Google Scholar
3. Geller B, Reising D, Leonard H, Riddle M, Walsh T: Critical review of tricyclic antidepressant use in children and adolescents. J Am Acad Child Adolesc Psychiatry 1999, 38:513–516Google Scholar
4. Quitkin F, Rifkin A, Klein DF: Imipramine response in deluded depressive patients. Am J Psychiatry 1978; 135:806–811Link, Google Scholar
5. Endicott J, Spitzer RL: Use of the Research Diagnostic Criteria and the Schedule for Affective Disorders and Schizophrenia—Lifetime Bipolar. New York, New York State Psychiatric Institute, 1988Google Scholar
6. Endicott J, Spitzer RL, Fleiss JL, Cohen J: The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry 1976; 33:766–771Crossref, Medline, Google Scholar
7. Tausig JE, Freeman EW: The next best thing to being there: conducting the clinical research interview by telephone. Am J Orthopsychiatry 1988; 58:418–427Crossref, Medline, Google Scholar
8. Andreasen NC, Endicott J, Spitzer RL, Winokur G: The family history method using diagnostic criteria: reliability and validity. Arch Gen Psychiatry 1977; 34:1229–1235Google Scholar
9. Weissman MM, Wolk S, Wickramaratne P, Goldstein RB, Adams P, Greenwald S, Ryan ND, Dahl RE, Steinberg D: Children with prepubertal-onset major depressive disorder and anxiety grown up. Arch Gen Psychiatry 1999; 56:794–801Crossref, Medline, Google Scholar
10. Geller B, Zimerman B, Williams M, Bolhofner K, Craney J, DelBello M, Soutullo C: Diagnostic characteristics of 93 cases of a prepubertal and early adolescent bipolar disorder phenotype by gender, puberty and comorbid attention deficit hyperactivity disorder. J Child Adolesc Psychopharmacol 2000; 10:157–164Crossref, Medline, Google Scholar
11. Chambers WJ, Puig-Antich J, Tabrizi MA, Davies M: Psychotic symptoms in prepubertal major depressive disorder. Arch Gen Psychiatry 1982; 39:921–927Crossref, Medline, Google Scholar
12. Geller B, Luby J: Child and adolescent bipolar disorder: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry 1997; 36:1168–1176Google Scholar
13. Clayton P: The epidemiology of bipolar affective disorders. Compr Psychiatry 1981; 22:31–43Crossref, Medline, Google Scholar
14. Kessler RC, Walters EE: Epidemiology of DSM-III-R major depression and minor depression among adolescents and young adults in the National Comorbidity Survey. Depress Anxiety 1998; 7:3–14Crossref, Medline, Google Scholar
15. Geller B, Zimerman B, Williams M, Bolhofner K, Craney J, DelBello M, Soutullo C: Six-month stability and outcome of a prepubertal and early adolescent bipolar disorder phenotype. J Child Adolesc Psychopharmacol 2000; 10:165–173Crossref, Medline, Google Scholar



