An Empirical Study of the Classification of Eating Disorders
Abstract
OBJECTIVE: The nosology for eating disorders, despite having been extensively revised over time, may not capture the natural clustering of eating-related pathology as it occurs in general population samples.METHOD: Detailed information about anorectic and bulimic behaviors was assessed through personal interviews of 2,163 Caucasian female twins from a population-based registry. Latent class analysis was applied to nine eating disorder symptoms to develop an empirically based typology. Demographic, comorbidity, personality, and co-twin diagnosis data were used to validate the resultant classes.RESULTS: A six-class solution provided the best fit. One class displayed distorted eating attitudes without low body weight. Two classes demonstrated low weight without the psychological features of eating disorders. Three classes broadly resembled the DSM-IV classifications of anorexia nervosa, bulimia nervosa, and binge-eating disorder. For all classes, and especially for the three that reflected current diagnoses of eating disorders, monozygotic twins resembled one another much more in terms of class membership than did dizygotic twins.CONCLUSIONS: The authors found within a community sample, and through an empirical method, classes of eating-related pathology that broadly resembled the current classifications of anorexia nervosa, bulimia nervosa, and binge-eating disorder. Additional classes were marked by either the psychological features of eating disorders or low body weight. Individuals in the three eating-disorder classes had similar personality profiles but displayed differences in symptom expression and co-twin risk for anorexia nervosa, bulimia nervosa, and obesity.
The nosology for eating disorders has undergone extensive revision in a brief period of time. Anorexia nervosa was the first eating disorder identified (1, 2). Heterogeneity became evident as Beumont et al. (3) noted differences between “dieters” and “vomiters and purgers,” and Russell (4) identified bulimia nervosa as “an ominous variant of anorexia nervosa.” Although Russell reported cases of binging and purging in the absence of a history of anorexia nervosa, at first he viewed the symptoms of bulimia as part of the anorexia nervosa syndrome. DSM-III established “bulimia” as the second eating disorder and included an underspecified category, “atypical eating disorder.” With only two eating disorders, this system did not capture the full range of eating-disordered behavior (5–7). By DSM-III-R, the category “eating disorder not otherwise specified” was expanded and given greater specificity. Anchored by early observations of binge eating (8), and amid substantial controversy (9–11), binge-eating disorder has been proposed as the fourth eating disorder.
Despite the increase in diagnostic choices, it is unclear whether these changes represent an improvement over earlier diagnostic schemata. There are important limitations to the evolution of nosology. First, the data used to support diagnostic change came primarily from clinical samples, which reflect only a subset of affected individuals, since relatively few women with eating disorders seek treatment (12, 13). Furthermore, evidence of referral bias exists in these samples (14–16). A more comprehensive typology of eating disorders may emerge from epidemiological samples (17, 18). Second, the DSM criteria sets were derived through expert consensus. This approach has a number of limitations (19) and has resulted in diagnostic criteria for eating disorders that remain controversial (20, 21). For example, the criteria for bulimia nervosa require that an individual binges and purges twice a week for 3 months, despite evidence that individuals who binge once a week are similar on most relevant dimensions (22–24).
Several fundamental questions remain regarding the nosology of eating disorders. First, how many eating disorders are there? Second, to what extent are the syndromes distinct or overlapping? Third, what are the optimal criteria and diagnostic thresholds? Finally, given the fluidity of the boundaries delineating these syndromes, how can we best account for the changes in symptomatic presentation over time?
The goal of this study was to address the first two of these fundamental questions with data from a large cohort of female twins from a population-based registry. We attempted to determine a naturally occurring empirical typology of eating disorders through latent class analysis of nine lifetime symptoms of DSM-III-R anorexia nervosa and bulimia nervosa. We first asked how many naturally occurring classes can be identified and then examined the eating disorder symptoms that characterized those classes. We then validated the resultant classes empirically by using additional data not included in the latent class analysis: demographic information, eating behavior, weight history, comorbidity, twin resemblance, and personality and attitudinal measures.
Method
Sample
Caucasian female twins (N=2,163) were ascertained through the Virginia Twin Registry, a population-based registry formed from a systematic review of all birth records in Virginia. Twins were eligible if they were born between 1934 and 1971 and both members had previously responded to a mailed questionnaire. The average age of the twins was 30.1 years (SD=7.6, range=17–55 years). The core sample for the present study is from the first interview wave, during which the lifetime history of anorexia nervosa and bulimia nervosa was assessed. We assessed 92% (N=2,163) of the eligible individuals, 90% face-to-face and the remainder by telephone. Since one subject had missing data for all eating disorders questions, the effective total sample was 2,162. Interviewer characteristics have been described in detail elsewhere (25). Interviewers were blind to information about the co-twin. Written informed consent was obtained before face-to-face interviews.
Assessment
The data used for this study span three waves of assessment. Lifetime history of anorexia nervosa, bulimia nervosa, major depression, alcohol dependence, panic disorder, phobias, and generalized anxiety disorder were assessed during the first interview wave (1987–1989) with an adapted version of the Structured Clinical Interview for DSM-III-R (26). Demographic and self-report data were also used from the first interview wave. Additional diagnostic information on bulimia nervosa was collected during the third interview wave (1992–1995) as was information on nicotine dependence. Diagnostic information on psychoactive substance abuse and dependence were obtained during the fourth interview wave (1997–1998).
Latent Class Analysis
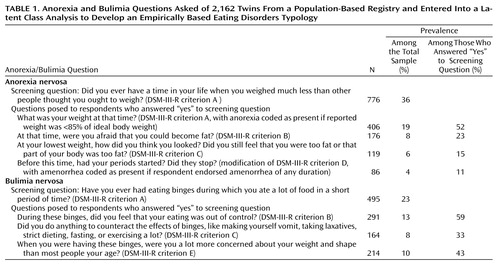
We used latent class analysis (27, 28) to determine empirically the typologies of eating and weight symptom profiles. Briefly, latent class analysis attempts to determine the number and composition of the unobserved latent classes that give rise to the observed data. The latent class analysis does not utilize twin status. By means of a FORTRAN program (29), we applied latent class analysis to the data matrix, which consisted of 1,071 twins who responded positively to one or both of the eating disorder screening questions (Table 1). The remaining 1,091 individuals who responded negatively to both of the eating disorder screening questions were not included in the latent class analysis and formed a comparison group.
The procedure for latent class analysis was to fit a one-class solution first, followed by two-, three-, and four-class solutions and so on until the best solution was obtained. This best solution was determined by two criteria. First, the difference between the log-likelihood of the previous and current class approximated a chi-square distribution; if this difference was greater than the critical chi-square statistic, then the current class provided a better fit to the data than the previous class. Second, the NAG subroutine (E04UCF) (29) used by the latent class analysis program for maximum likelihood minimization must have reached a valid solution (i.e., the E04UCF IFAIL parameter returned as zero).
Validation of the Classes
Demographic data, eating- and weight-related variables, comorbid psychiatric and psychoactive substance use disorders, personality and attitudinal measures, and co-twin risk and twin resemblance were used to validate the resultant classes.
Demographic data included years of education, years of education of the parents, financial status, and size of the community in which the individual lived at the time of interview. For the eating- and weight-related variables, we examined the percentage of women in each class who met criteria for the narrow and broad definitions of anorexia nervosa or bulimia nervosa as determined by computer algorithm. For both disorders, the narrow definition corresponded to the DSM-III-R criteria.
The broad definition of anorexia nervosa excluded the amenorrhea criterion. We excluded this criterion because of potential problems with accurate recall of duration of amenorrhea and because amenorrhea can be masked in individuals using birth control pills. In addition, previous analyses have indicated that there appears to be a spectrum of anorexia-like behaviors with no clear qualitative difference between the narrow definition of anorexia nervosa and broad anorexia-like syndromes (30). The broad definition of bulimia nervosa excluded the frequency/duration criterion. We excluded this criterion because prior analyses have indicated that it may be inappropriately restrictive (24). The third eating- and weight-related validator was whether the individual’s lifetime highest body mass index was greater than 30.0 kg/m2.
Lifetime comorbidity validators included major depression (31), generalized anxiety disorder (32), panic disorder, any phobia, alcohol dependence (33, 34), nicotine dependence (defined as a total score ≥7 on the Fagerstrom Tolerance Questionnaire [35]), and DSM-IV lifetime cannabis, stimulant, or cocaine abuse or dependence. In addition, given that we have found previously that the lifetime diagnosis of bulimia nervosa is of low reliability (36), we included diagnostic information on bulimia nervosa collected 5 years later as a validator.
Personality and attitudinal validators included neuroticism and extroversion (37), altruism and empathy (38), interpersonal dependency (39), locus of control (40), mastery (41), dispositional optimism (42), and the Rosenberg Self-Esteem Scale (43).
Statistical Comparisons
In the validation step, we first compared each of the six classes identified by best-fitting latent class analysis solution to the comparison group, followed by selected comparisons across the six latent-class-analysis-derived classes. For the lifetime diagnoses of psychiatric disorders, we calculated the odds ratios and 95% confidence intervals (CIs) by means of logistic regression for each class relative to the comparison group. Continuous variables for the six classes relative to the comparison group were compared by means of multiple regression. Given that our sample consisted of twins, the assumption of independent sampling was violated. We used generalized estimating equation modeling (44) to adjust standard errors for nonindependent observations as operationalized in the GENMOD procedure of SAS version 6.12 (45).
Results
Latent Class Analysis
After fitting a single-class model, the addition of further classes resulted in significant improvements in fit up through six classes. Neither the seven-class nor the eight-class solution significantly improved the fit. Individual participants were assigned to class membership on the basis of the likelihood of their response profile.
Of the total sample, 1,071 women responded positively to at least one of the eating disorders screening questions. Table 2 depicts the frequency of the nine DSM-III-R eating disorder symptoms for the six classes identified by the best-fitting latent class analysis solution as well as the eating- and weight-related validators. On the basis of these characteristics, we developed the following descriptions of the six classes.
In class 1 (3.6% of the sample; mean age=29.4 years, SD=7.4), all of the women reported weighing less than other people thought they should have weighed. However, none had actually ever been <85% of their ideal body weight. Despite this, fear of fatness and body image distortion were frequently endorsed. Secondary amenorrhea was present in a small percentage. Approximately one-quarter of these women endorsed binge eating; however, feeling out of control and excessive concerns with shape and weight were uncommon, and compensatory behaviors were relatively rare. A lifetime history of anorexia or bulimia, no matter how defined, was extremely rare in members of this class. Obesity (defined as having a body mass index of 30 kg/m2 or more) was also uncommon. On the basis of these characteristics, this class was referred to as “shape/weight preoccupied.”
In class 2 (1.9% of the sample; mean age=29.4 years, SD=6.8), all members reported having weighed less than others thought they should have weighed, and most actually had been <85% of their ideal body weight. None of the women in this class endorsed the psychological features of anorexia nervosa, although approximately one-quarter reported amenorrhea when thin. Although all of the women in class 2 reported having binged, none ever had felt out of control, and all denied having excessive shape and weight concerns. Compensatory behaviors occurred in 21% of this class. None of the women met diagnostic criteria for any definition of anorexia or bulimia, and no one in this class was obese. We called this group the “low weight with binging” class.
In class 3 (21.9% of the sample; mean age=31.6 years, SD=7.8), all members reported weighing less than others thought they should have weighed, and slightly over half had actually weighed <85% of their ideal body weight. The psychological features of anorexia were mostly absent, and amenorrhea was uncommon. Episodes of binge eating and compensatory behaviors were also rare in this class. Anorexia nervosa did not occur in this class, and obesity and a lifetime diagnosis of bulimia nervosa, narrow or broad definition, were rare. This group was the “low weight without binging” class.
In class 4 (3.4% of the sample; mean age=28.1 years, SD=6.1), all of the women said they had weighed less than others thought they should have weighed, and all reported weights that were <85% of their ideal body weight. Fear of fatness was nearly ubiquitous; one-half felt they looked fat even when thin, and secondary amenorrhea was present in over one-quarter of the women. Episodes of binge eating were reported by one-fifth of the women in this class, but purging was infrequent. Approximately half of the women in this class met criteria for the broad definition of anorexia nervosa, while 11% met the narrow anorexia definition. Lifetime bulimia nervosa was absent in this class, and obesity was rare. This group was the “anorexic” class.
In class 5 (4.6% of the sample; mean age=28.4 years, SD=6.8), although many of the women reported having weighed less than others thought they should weigh, few reported weights <85% of their ideal body weight. The psychological features of anorexia nervosa were common, and secondary amenorrhea was reported occasionally. Binge eating, compensatory behaviors, and excessive concern with shape and weight were nearly universal, and the majority reported feeling out of control while binging. Nine percent of women in this class met lifetime criteria for the broad definition of anorexia nervosa, while a substantial majority met criteria for the broad definition of bulimia nervosa. Obesity was reported by 6%. We called this group the “bulimic” class.
In class 6 (14.1% of the sample; mean age=29.7 years, SD=7.6), nearly one-quarter of the women reported having weighed less than others thought they should have weighed, but very few had actually been <85% of their ideal body weight. The psychological features of anorexia nervosa and amenorrhea were rarely endorsed. In contrast, all of these women reported episodes of binge eating, with over one-half reporting having felt out of control. Purging was rarely endorsed, and excessive concerns with shape and weight were also uncommon. None of the women in this class met criteria for either definition of anorexia or bulimia. Obesity was markedly more common in this class than in any other. We called this group the “binge-eating” class.
Classes 4, 5, and 6 were referred to as “eating disorder classes,” since they represented more severe clusters of disordered eating.
Validators
Demographic
There were no significant differences across the six classes and the comparison group on education, parental education, financial status, or size of community in which the individual lived.
Lifetime prevalence of other psychiatric and psychoactive substance use disorders
Comorbidity data used to validate the classes are presented in Table 3. The odds ratios for a bulimia diagnosis at the wave 3 assessment were higher for the shape/weight preoccupied, low weight with binging, binge-eating, and especially for the bulimic class. Members of all six classes were significantly more likely to have comorbid major depression, phobias, and alcohol dependence. The odds ratios for comorbid generalized anxiety disorder and nicotine dependence were significantly higher for all but the bulimic class. Panic disorder and stimulant abuse or dependence were significantly more likely for all subjects except those in the shape/weight preoccupied and bulimic classes. The odds ratios for cannabis abuse or dependence were significantly higher in the low weight with and without binging classes, whereas only the bulimic class had a higher odds ratio for lifetime cocaine abuse or dependence. These results reflect robust differences across the six classes relative to the comparison group, since the probability of obtaining 43 significant results out of 60 comparisons at the p<0.05 level is <0.0007 (46).
Personality and attitudes
The eating disorder classes (classes 4, 5, and 6) exhibited the most deviant scores on the personality and attitudinal measures (Table 4). In contrast to the comparison group, individuals in these classes exhibited higher dependency and lower mastery, optimism, and self-esteem. In addition, all of the classes derived from the latent class analysis (except class 2) had elevated levels of neuroticism. Excluding the comparison group and examining post hoc comparisons across the six classes, the bulimic and binge-eating classes scored higher on dependency and neuroticism and lower on mastery and self-esteem than the low weight without binging class. In addition, women in the anorexic class scored significantly lower on self-esteem and higher on neuroticism than the low weight without binging class. These results are also robust, since the probability of obtaining 18 significant results out of 48 comparisons at the p<0.05 level is <0.0001 (46). After isolating the three eating disorder groups (classes 4, 5, and 6), we found no significant differences for any personality measures (data not shown).
Lifetime history of eating disorders and obesity in co-twins
Table 5 presents the lifetime risk of bulimia nervosa, anorexia nervosa, and obesity for the co-twin of twins in each class, compared to the co-twins of the twins in the comparison group. Co-twins of twins in the bulimic and binge-eating classes were at significantly greater risk for lifetime history of bulimia nervosa. Co-twins of twins in the shape/weight preoccupied, low weight without binging, and anorexic classes were at significantly greater risk for lifetime anorexia nervosa. Only co-twins of twins in the binge-eating class were at significantly greater risk for obesity; having a co-twin in the low weight without binging class was protective against obesity.
Monozygotic-dizygotic concordance
The monozygotic twins showed greater concordance for class membership across the seven classes (the six classes derived from the latent class analysis and the comparison group) (χ2=112.0, df=36, p<0.0001; contingency coefficient=0.40) than did the dizygotic twins (χ2=59.8, df=36, p<0.008; contingency coefficient=0.34). In addition, there were 103 monozygotic and 74 dizygotic twins for whom both members of the twin pair were in classes 4, 5, or 6 (the eating disorder classes). The monozygotic twins demonstrated substantially greater concordance for class membership (χ2=56.9, df=4, p<0.0001; contingency coefficient=0.60) than did the dizygotic twins (χ2=9.1, df=4, p=0.06; contingency coefficient=0.33).
Severity of and reasons for low weight
In addition to the anorexic class, there were two classes marked by periods of significantly low body weight. When controlling for age, the mean lifetime lowest body mass index reported across the three classes differed significantly. Women in the anorexic and low weight with binging classes reported lower lifetime minimum body mass indexes (mean=16.6 kg/m2 [SD=1.1] and 16.5 kg/m2 [SD=2.0], respectively) than women in the low weight without binging class (mean=17.4 kg/m2, SD=2.0) (F=8.5, df=2, 544, p=0.0002).
We then reviewed the original interview forms in which the “reason for low weight” had been recorded for all women in class 2 and 50% of those in class 3. The reasons endorsed for low weight included constitutional thinness; weight loss secondary to depression, interpersonal loss, or anxiety; weight loss secondary to medical illness or procedures; and an array of infrequently endorsed reasons. There were significantly more women in class 2 than in class 3 who reported weight loss secondary to depression, anxiety, or interpersonal loss (22% versus 14%) (χ2=4.22, df=1, p<0.04). Given that the odds ratios for nicotine dependence were similarly higher in all but the bulimic class, it does not seem that low weight in this group would be fully accounted for by an excess of individuals who were dependent on nicotine.
Discussion
The latent class analysis of nine items reflecting DSM-III-R criteria for anorexia nervosa and bulimia nervosa provided an interpretable six-class solution that clarifies the natural clustering of eating disorder symptoms in the community. The first three classes did not appear to reflect clinical eating disorders. Two of these classes included individuals with low weight without the psychological features of anorexia nervosa, and one was marked by the presence of shape and weight preoccupations in the absence of low weight. The three remaining classes broadly reflected current conceptualizations of anorexia nervosa, bulimia nervosa, and binge-eating disorder. These three-eating disorder classes displayed similar personality profiles, yet there were clear differences in symptom expression and co-twin risk for eating disorders and obesity.
Characteristics of the Eating Disorder Classes
We examined the characteristics of each of the three eating disorder classes and found substantial similarities with the DSM-IV diagnostic schemata as well as notable differences. By comparing the clinical characteristics of the classes that emerged from the latent class analysis with the DSM-IV diagnostic criteria, we could address the extent to which the DSM criteria reflect the natural clustering of symptoms in the population. However, the nature of our data do not enable commentary on the diagnostic thresholds for the determination of caseness.
Anorexia
We found convergence between the anorexic class derived from the latent class analysis and the DSM criteria for the symptoms of weight loss and fear of fatness, as those items were nearly ubiquitously reported. In this population-based sample, however, the symptoms of feeling fat even when thin and amenorrhea were less universally endorsed. That only half of the women endorsed body image distortion squares with clinical observations of individuals who present with clear anorexic syndromes but whose body image disturbance fluctuates. Thus, the broadening of this criterion in DSM-IV to include undue influence of shape and weight on self-evaluation or denial of seriousness of the illness may have been warranted.
It is of interest to note that amenorrhea was not a unifying criterion for any one class. The symptom was equally present in the anorexic class and in the low weight with binging (but without the psychological features of anorexia nervosa) class. Moreover, a number of women in the anorexic class did not report amenorrhea at the time of low weight, despite the presence of the full array of other anorexia nervosa symptoms. Whether amenorrhea should be included as a defining criterion for anorexia nervosa requires further study. Our data cannot answer that question but can confirm the natural clustering of individuals with clinical features of anorexia nervosa with and without amenorrhea.
Bulimia
We compared the symptom profiles of the bulimic class with the DSM-IV criteria for bulimia nervosa and found reasonable convergence for three of the four criteria explored. Nearly all of the women in this class endorsed binge eating, compensatory behaviors, and excessive shape and weight concerns. This class reported significantly more purging than the other classes, and the most frequent methods were strict dieting and exercise followed by fasting, vomiting, and laxatives. A lifetime history of anorexia nervosa (broad definition) was reported in 9% of the women in this class, which is consistent with the observations of clinical samples (47–49).
The “out of control” criterion was less defining of the bulimic class. This criterion was new to DSM-III-R and was carried over to DSM-IV. The DSM-III criterion was that the individual had to be aware that the eating behavior was abnormal and have a fear of not being able to stop eating voluntarily. Studies on the nature of a binge have suggested that episodes in which an individual eats an abnormally large amount of food but does not feel out of control are best conceptualized as overeating episodes (50). Our data suggest that further validation of this criterion is warranted.
Binge-eating disorder
The fate of binge-eating disorder as a diagnostic category is undecided. Our data reflect a relatively large class of individuals, distinct from women with bulimia nervosa, whose primary behavioral manifestation is binge eating without compensatory behaviors. In this class, all members endorsed binge eating. However, only about half reported feeling out of control—which supports our recommendation for further inquiry into the relationship between the behavioral symptom of binge eating and the cognitive feature of feeling out of control. These women differed from those in the bulimic class, not only in terms of the relative absence of compensatory behaviors but also in terms of their greater propensity toward obesity—which is consistent with observed associations between binge-eating disorder and obesity (51–57).
Characteristics of the Other Classes of Eating-Related Pathology
The three additional classes reveal interesting variations on the eating and weight disorders continuum and may shed light on the poorly understood category of eating disorder not otherwise specified. The shape/weight preoccupied class displayed the psychological features of anorexia nervosa in the absence of significant weight loss. This class may reflect a subclinical group of women who are preoccupied with their shape and weight but who have not engaged in the behaviors associated with clinically significant disordered eating. They may be at higher risk for the development of frank eating disorders—a hypothesis supported by the observation that they were at greater risk for bulimia nervosa 5 years later.
Classes 2 and 3, in contrast, displayed low weight and, for class 2, a comparable rate of amenorrhea to that of the anorexic class but without evidence of the psychological features of anorexia nervosa. The two classes differed in their reasons for low weight, with class 2 displaying more anorexia of depression. Indeed, summing across all relevant validators, class 2 carried a greater burden of comorbidity than class 3, with higher rates of major depression, alcohol dependence, and stimulant abuse.
Validators: Comorbidity
Comorbidity profiles indicated that all six classes had greater comorbidity than the comparison group. Of particular note are the markedly elevated odds ratios for major depression and alcohol dependence in class 2, which reflects the larger proportion of women in this class who reported low weight secondary to depression or interpersonal loss. Also noteworthy are the very high odds ratios for stimulant abuse in the low weight with binging and anorexic classes, although we could not determine whether stimulants were taken primarily for weight loss. Of the three eating disorder classes, the bulimic class reported lower comorbidity, which is at odds with clinical observations (58–60) but consistent with findings of lesser comorbidity in community than clinical samples (14). This class did, however, show stability across time, with the odds ratios for both broadly and narrowly defined bulimia nervosa at the third interview wave being significantly elevated.
Validators: Psychological Measures
The fact that the anorexia, bulimia, and binge-eating classes represent more severe conditions was reflected in the self-report validators. The differences between the eating disorder classes and the other classes, including the comparison group, arose in self-esteem, mastery, dependency, and neuroticism. The fact that the three eating disorder classes did not differ significantly from each other on any personality or attitudinal measure raises the hypothesis that a particular constellation of personality features may predispose an individual to an eating disorder and that other factors—perhaps genetic susceptibility to obesity or binge eating or possibly environmental factors—may influence the type of eating disturbance that emerges. Alternatively, having an eating disorder, regardless of its nature, could lead to changes in personality and attitudinal features such as a sense of low mastery and self-esteem.
Twin Class Membership and Twin Risk for Anorexia Nervosa, Bulimia Nervosa, and Obesity
Monozygotic twins showed a more significant concordance for class membership than did dizygotic twins, particularly for classes 4, 5, and 6. This suggests that the factors that influence the type of eating disorder symptoms are at least partially genetically determined. We were also able to examine the extent to which the odds ratio of a co-twin having anorexia nervosa, bulimia nervosa, and obesity was higher given the class membership of the index twin. We found some specificity of risk: co-twins of twins in the shape and weight preoccupied, low weight without binging, and anorexic classes were at greater risk for anorexia nervosa; co-twins of twins in the bulimic and binge-eating classes were at greater risk for bulimia nervosa; and co-twins of twins in the binge-eating class were at greater risk for obesity. Thus, there may be some specificity in the transmissibility of disordered eating subtypes.
Limitations
When considering these results, several methodological limitations must be considered. First, as in factor analysis, the resultant classes are contingent on the variables put into the latent class analysis. Different eating disorders symptoms might have yielded a different solution.
Second, the interview did not allow individuals who had not endorsed binge eating to be questioned about compensatory behaviors. Thus, we could not identify individuals who purged in the absence of binging. However, in a prior latent class analysis of bulimic behaviors conducted on a different interview in which purging was assessed independent of binging, no such class emerged (24). Thus, although clinicians may encounter this presentation in clinical settings, these individuals are relatively rare and do not appear to comprise a discrete class in community samples.
Third, latent class analysis class membership is based on maximum likelihood estimation and does not prove membership in a particular class, nor can it prove the existence of these six classes.
Finally, the purpose of this study was to develop an empirically based typology. Such an approach is valuable in understanding naturally occurring clusters of behavior; however, the latent class analysis as presented here was not designed to test various thresholds in the determination of caseness.
Conclusions
These findings support the existence of three general classes of disordered eating behavior. These classes broadly resemble current classifications of anorexia nervosa, bulimia nervosa, and binge-eating disorder. Three additional atypical classes were also identified that may to some extent represent individuals at risk for the subsequent development of clinical eating disorders. The data also support the continued evaluation of diagnostic criteria such as amenorrhea and body image distortion for anorexia nervosa and a sense of loss of control during binging for both bulimia nervosa and binge-eating disorder. As only a small proportion of women with eating disorders ever seek treatment (12, 13), clinical samples only allow us to investigate a very select portion of the population of afflicted individuals. Community studies such as this are therefore preferred when addressing etiological factors or typology, and they allow us to view the disorders as they occur naturally in the population.
 |
 |
 |
 |
 |
Presented in part at the annual meeting of the Eating Disorders Research Society, Boston, Nov. 6–7, 1998. Received May 10, 1999; revision received Aug. 26, 1999; accepted Nov. 18, 1999. From the Department of Psychiatry, Virginia Institute for Psychiatric and Behavioral Genetics, Medical College of Virginia of Virginia Commonwealth University. Address reprint requests to Dr. Bulik, Department of Psychiatry, Virginia Institute for Psychiatric and Behavioral Genetics, Medical College of Virginia of Virginia Commonwealth University, P.O. Box 980126, Richmond, VA 23298-0126. Supported by a Research Scientist Development Award (MH-01553) from NIMH to Dr. Bulik and NIMH grants MH-01277, MH-40828, and National Institute on Alcohol Abuse and Alcoholism grant AA-09095 to Dr. Kendler.
1. Gull WW: Anorexia nervosa (apepsia hysterica, anorexia hysterica). Transactions of the Clin Society of London 1874; 7:22–28Google Scholar
2. Las禵e E-C: On hysterical anorexia. Med Times and Gazette 1873, pp 265–266, 367–369Google Scholar
3. Beumont PJV, George GCW, Smart DE: “Dieters” and “vomiters and purgers” in anorexia nervosa. Psychol Med 1976; 6:617–622Crossref, Medline, Google Scholar
4. Russell GFM: Bulimia nervosa: an ominous variant of anorexia nervosa. Psychol Med 1979; 9:429–448Crossref, Medline, Google Scholar
5. Garfinkel PE, Lin E, Goering P, Spegg C, Goldbloom DS, Kennedy S, Kaplan AS, Woodside DB: Purging and nonpurging forms of bulimia nervosa in a community sample. Int J Eat Disord 1995; 20:231–238Crossref, Google Scholar
6. Garner DM, Garfinkel PE, O’Shaughnessey M: The validity of the distinction between bulimia with and without anorexia nervosa. Am J Psychiatry 1985; 142:581–587Link, Google Scholar
7. Thompson JK: Similarities among bulimia nervosa patients categorized by current and historical weight: implications for the classification of eating disorders. Int J Eat Disord 1988; 7:185–189Crossref, Google Scholar
8. Stunkard AJ: Eating patterns and obesity. Psychiatr Q 1959; 33:284–295Crossref, Medline, Google Scholar
9. Fairburn CG, Welch SL, Hay PJ: The classification of recurrent overeating: the “ binge eating disorder” proposal. Int J Eat Disord 1993; 13:155–159Crossref, Medline, Google Scholar
10. Spitzer RL, Yanovski S, Wadden T, Wing R, Marcus MD, Stunkard A, Devlin M, Mitchell J, Hasin D, Horne RL: Binge eating disorder: its further validation in a multisite study. Int J Eat Disord 1993; 13:137–153Crossref, Medline, Google Scholar
11. Spitzer RL, Stunkard A, Yanovski S, Marcus MD, Wadden T, Wing R, Mitchell J, Hasin D: Binge eating disorder should be included in DSM-IV: a reply to Fairburn et al’s “The classification of recurrent overeating: the binge eating disorder proposal.” Int J Eat Disord 1993; 13:161–169Crossref, Medline, Google Scholar
12. Fairburn CG, Cooper JP: Self-induced vomiting and bulimia nervosa: an undetected problem. Br Med J 1982; 284:1153–1155Google Scholar
13. Welch SL, Fairburn CG: Sexual abuse and bulimia nervosa: three integrated case control comparisons. Am J Psychiatry 1994; 151:402–407Link, Google Scholar
14. Bushnell JA, Wells E, McKenzie JM, Hornblow AR, Oakley-Browne MA, Joyce PR: Bulimia comorbidity in the general population and in the clinic. Psychol Med 1994; 24:605–611Crossref, Medline, Google Scholar
15. Fairburn CG, Welch SL, Norman PA, O’Connor ME, Doll HA: Bias and bulimia nervosa: how typical are clinic cases? Am J Psychiatry 1996; 153:386–391Google Scholar
16. Welch SL, Fairburn CG: Childhood sexual and physical abuse as risk factors for the development of bulimia nervosa: a community-based case control study. Child Abuse Negl 1996; 20:633–642Crossref, Medline, Google Scholar
17. Hay P, Fairburn C, Doll H: The classification of bulimic eating disorders: a community-based cluster analysis study. Psychol Med 1996; 26:801–812Crossref, Medline, Google Scholar
18. Eaton WW, Dryman A, Sorenson A, McCutcheon A: DSM-III major depressive disorder in the community: a latent class analysis. Br J Psychiatry 1989; 155:48–54Crossref, Medline, Google Scholar
19. Kendler KS: Toward a scientific psychiatric nosology. Arch Gen Psychiatry 1990; 47:969–973Crossref, Medline, Google Scholar
20. Wilson G, Eldredge K: Frequency of binge-eating in bulimic patients: diagnostic validity. Int J Eat Disord 1991; 10:557–561Crossref, Google Scholar
21. Garfinkel P, Kennedy S, Kaplan A: Views on classification and diagnosis of eating disorders. Can J Psychiatry 1996; 40:445–456Google Scholar
22. Garfinkel PE, Lin E, Goering P, Spegg C, Goldbloom DS, Kennedy S, Kaplan AS, Woodside DB: Bulimia nervosa in a Canadian community sample: prevalence and comparison of subgroups. Am J Psychiatry 1995; 152:1052–1058Google Scholar
23. Walsh BT, Wilson GT, Loeb KL, Devlin MJ, Pike KM, Roose SP, Fleiss J, Waternaux C: Medication and psychotherapy in the treatment of bulimia nervosa. Am J Psychiatry 1997; 154:523–531Link, Google Scholar
24. Sullivan PF, Bulik CM, Kendler KS: The epidemiology of bulimia nervosa: symptoms, syndromes and diagnostic thresholds. Psychol Med 1998; 28:599–610Crossref, Medline, Google Scholar
25. Kendler KS, MacLean C, Neale M, Kessler R, Heath A, Eaves L: The genetic epidemiology of bulimia nervosa. Am J Psychiatry 1991; 148:1627–1637Google Scholar
26. Spitzer RL, Williams JBW, Gibbon M, First MB: The Structured Clinical Interview for DSM-III-R (SCID), I: history, rationale, and description. Arch Gen Psychiatry 1992; 49:624–629Crossref, Medline, Google Scholar
27. McCutcheon AL: Latent Class Analysis. Beverly Hills, Calif, Sage Publications, 1987Google Scholar
28. Eaves LJ, Silberg JL, Hewitt JK, Rutter M, Meyer JM, Neale MC, Pickles A: Analyzing twin resemblance in multisymptom data: genetic applications of a latent class model for symptoms of conduct disorder in juvenile boys. Behav Genet 1993; 23:5–19Crossref, Medline, Google Scholar
29. Group NA: NAG FORTRAN Library Manual. Oxford, UK, Numerical Algorithms Group, 1993Google Scholar
30. Walters EE, Kendler KS: Anorexia nervosa and anorexic-like syndromes in a population-based female twin sample. Am J Psychiatry 1995; 152:64–71Link, Google Scholar
31. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ: A population-based twin study of major depression in women: the impact of varying definitions of illness. Arch Gen Psychiatry 1992; 49:257–266Crossref, Medline, Google Scholar
32. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ: Major depression and generalized anxiety disorder: same genes, (partly) different environments? Arch Gen Psychiatry 1992; 49:716–722Google Scholar
33. Kendler KS, Heath AC, Neale MC, Kessler RC, Eaves LJ: Alcoholism and major depression in women. Arch Gen Psychiatry 1993; 50:690–698Crossref, Medline, Google Scholar
34. Kendler KS, Walters EE, Neale MC, Kessler RC, Heath AC, Eaves LJ: The structure of the genetic and environmental risk factors for six major psychiatric disorders in women: phobia, generalized anxiety disorder, panic disorder, bulimia, major depression, and alcoholism. Arch Gen Psychiatry 1995; 52:374–383Crossref, Medline, Google Scholar
35. Fagerstrom K-O: Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addict Behav 1978; 3:235–241Crossref, Medline, Google Scholar
36. Bulik CM, Sullivan PF, Kendler KS: Heritability of binge-eating and broadly defined bulimia nervosa. Biol Psychiatry 1998; 44:1210–1218Google Scholar
37. Eysenck HJ, Eysenck SBG: Manual of the Eysenck Personality Questionnaire. London, Hodder and Stoughton, 1975Google Scholar
38. Casper RC, Eckert ED, Halmi KA, Goldberg SC, Davis JM: Bulimia: its incidence and clinical importance in anorexia nervosa. Arch Gen Psychiatry 1980; 37:1030–1035Google Scholar
39. Hirschfeld RMA, Klerman GL, Gough HR, Barrett J, Korchin SJ, Chodoff P: A measure of interpersonal dependency. J Pers Assess 1977; 41:610–618Crossref, Medline, Google Scholar
40. Peterson C, Semmel A, Von Baeyer C, Abramson LY, Metalsky CI, Seligman MEP: The Attributional Style Questionnaire. Cognitive Therapy and Res 1982; 6:287–300Crossref, Google Scholar
41. Maddi SR, Kobasa SC, Hoover M: An alienation test. J Humanist Psychol 1979; 19:73–76Crossref, Google Scholar
42. Scheier MG, Carver CS: Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychol 1985; 4:219–247Crossref, Medline, Google Scholar
43. Rosenberg M: Society and the Adolescent Self-Image. Princeton, NJ, Princeton University Press, 1965Google Scholar
44. Zeger SL, Liang KY, Albert PS: Models for longitudinal data: a generalized estimating equation approach. Biometrics 1988; 44:1049–1060Google Scholar
45. SAS/STAT Software: Changes and Enhancements Through Release 6.11. Cary, NC, SAS Institute, 1996Google Scholar
46. Field H, Armenakis A: On use of multiple tests of significance in psychological research. Psychol Rep 1974; 35:427–431Crossref, Google Scholar
47. Sullivan PF, Bulik CM, Carter FA, Gendall KA, Joyce PR: The significance of a prior history of anorexia in bulimia nervosa. Int J Eat Disord 1996; 20:253–261Crossref, Medline, Google Scholar
48. Eckert ED, Halmi KA, Marchi P, Grove W, Crosby R: Ten-year follow-up of anorexia nervosa: clinical course and outcome. Psychol Med 1995; 25:143–156Crossref, Medline, Google Scholar
49. Gillberg IC, Rastam M, Gillberg C: Anorexia nervosa outcome: six-year controlled longitudinal study of 51 cases including a population cohort. J Am Acad Child Adol Psychiatry 1994; 33:729–739Crossref, Medline, Google Scholar
50. Beglin SJ, Fairburn CG: What is meant by the term “binge”? Am J Psychiatry 1992; 149:123–124Google Scholar
51. Striegel-Moore RH, Wilson GT, Wilfley DE, Elder KA, Brownell KD: Binge eating in an obese community sample. Int J Eat Disord 1998; 23:27–37Crossref, Medline, Google Scholar
52. Adami GF, Gandolfo P, Scopinaro N: Binge eating in obesity. Int J Obes Relat Metab Disord 1996; 20:793–794Medline, Google Scholar
53. Bruce B, Wilfley D: Binge eating among the overweight population: a serious and prevalent problem. J Am Diet Assoc 1996; 96:58–61Crossref, Medline, Google Scholar
54. Telch CF, Agras WS: Obesity, binge eating and psychopathology: are they related? Int J Eat Disord 1994; 15:53–61Google Scholar
55. de Zwaan M, Mitchell JE: Binge eating in the obese. Ann Med 1992; 24:303–308Crossref, Medline, Google Scholar
56. Arnow B, Kenardy J, Agras WS: Binge eating among the obese: a descriptive study. J Behav Med 1992; 15:155–170Crossref, Medline, Google Scholar
57. Marcus MD, Wing RR, Lamparski DM: Binge eating and dietary restraint in obese patients. Addict Behav 1985; 10:163–168Crossref, Medline, Google Scholar
58. Braun DL, Sunday SR, Halmi KA: Psychiatric comorbidity in patients with eating disorders. Psychol Med 1994; 24:859–867Crossref, Medline, Google Scholar
59. Hudson JI, Pope HG Jr, Yurgelun-Todd D, Jonas JM, Frankenburg FR: A controlled study of lifetime prevalence of affective and other psychiatric disorders in bulimic outpatients. Am J Psychiatry 1987; 144:1283–1287Google Scholar
60. Herzog DB, Keller MB, Sacks NR, Yeh CJ, Lavori PW: Psychiatric comorbidity in treatment-seeking anorexics and bulimics. J Am Acad Child Adol Psychiatry 1992; 31:810–818Crossref, Medline, Google Scholar



