Forty-Year Psychiatric Outcomes Following Assessment for Internalizing Disorder in Adolescence
Abstract
Objective: The aim of this study was to define the long-term psychiatric outcomes of adolescent internalizing disorder in the general population, using data collected over 40 years from a national birth cohort. Method: A total of 3,279 members of the Medical Research Council National Survey of Health and Development (the 1946 British birth cohort) underwent assessments of psychiatric symptoms, primarily anxiety and depression, at ages 13 and 15. Adolescents who had internalizing disorder at both ages 13 and 15 and those who had internalizing disorder at one of the two ages were compared with mentally healthy adolescents on various psychiatric outcomes in adulthood (ages 26–53), including the prevalence of mental disorders, self-reported trouble with “nerves,” suicidal ideation, and treatment for psychiatric disorders. Results: About 70% of adolescents who had internalizing disorder at both ages 13 and 15 had mental disorder at age 36, 43, or 53, compared with about 25% of the mentally healthy adolescents. They were also more likely than healthy adolescents to have self-reported “nervous trouble” and to have been treated for psychiatric disorder during adulthood. None of these effects was apparent among subjects who had internalizing disorder at only one of the two adolescent assessments. Conclusions: The long-term psychiatric outcome for adolescents with persistent or recurrent internalizing disorder was poor, whereas the outcome for those who had a single episode was better than expected. The association between adolescent internalizing disorder and poor psychiatric outcomes in adulthood may be mediated by persistence or severity of symptoms in adolescence.
Internalizing disorders are common in adolescence. The population prevalence of recent adolescent depression is between 1.5% and 4.9%, and the prevalence of recent adolescent anxiety is in the range of 5.7% to 10.8% (1 – 4) .
Adolescent internalizing disorder is associated with a range of psychosocial difficulties, such as impaired personal relationships (5 , 6) , poor school performance (5) , and lower global functioning (2) . In addition, adolescent internalizing disorder has been linked to more serious psychiatric difficulty, such as conduct or behavioral disorder (1 , 3) , substance abuse (3 , 7) , and suicidal behavior (6 , 7) .
Prospective cohort studies have consistently shown that adolescent internalizing disorder is also associated with adverse mental health outcomes in early adulthood (8 – 16) . Most commonly, adolescent internalizing disorder predicts anxiety and depression in early adulthood (8 – 13 , 15 , 16) . Adolescent internalizing disorder has also been linked to other outcomes associated with adult mental disorders, including suicidal behavior (8 , 14 , 16) , psychiatric treatment (13 , 16) , use of psychotropic medications (13) , psychiatric hospitalizations (8 , 13) , and social impairment (8 , 9) .
Some studies have followed child and adolescent psychiatric patients as far as age 43 (13 , 17 , 18) , but because they concentrate on clinical samples, they are biased toward more severe mental disorders. This bias is avoided in several population-based cohort studies, although, to date, such studies have followed adolescents with internalizing disorder only into early adulthood (10 – 12 , 15 , 16) . As yet, it is unclear whether the poor adult outcomes observed in adolescents from population-based studies will continue into later adulthood.
The aim of this investigation was to define the long-term psychiatric outcomes of adolescent internalizing disorder in the general population, using data from ages 13 to 53 in a national birth cohort.
Method
Subjects
The study used data from the Medical Research Council National Survey of Health and Development (NSHD). The NSHD originally included every child born in England, Scotland, and Wales during the week of March 3–9, 1946 (19) . A stratified sample of 5,362 individuals was selected from all singleton births to married women by taking a random 1 in 4 of all births to wives of manual workers and all births to wives of nonmanual and agricultural workers. This sample has been prospectively studied on 17 occasions up to age 26 and additionally at ages 31, 36, 43, and 53 (19 , 20) . Analyses have shown few significant biases between those who remain in the study and those who do not (21) , and comparisons with census data show that the remaining cohort (N=3,673 at age 53) is broadly representative of all native-born adults currently resident in England, Scotland, and Wales (20) .
In this study, we report on 3,279 cohort members (61.2% of the original cohort) whose mental health was assessed at ages 13 and 15.
Adolescent Internalizing Disorder
Assessment of adolescent internalizing disorder was based on questionnaires completed by teachers when the children were 13 and 15 years of age, describing personality, behavior, and attitudes. These questionnaires have previously been subjected to factor analysis, in which anxiety/depression and internalizing emotions and behaviors were identified as one factor (22 – 25) . Teachers rated individual items as more than, the same as, or less than other children in the class. Items that loaded onto the internalizing factor were “timid child,” “rather frightened of rough games,” “extremely fearful,” “always tired and washed out,” “usually gloomy and sad,” “avoids attention,” “very anxious,” “unable to make friends,” “diffident about competing,” “frequently daydreams in class,” and “becomes unduly miserable or worried in response to criticism.” Cronbach’s alpha was calculated for the scale at both ages 13 and 15, with scores of 0.68 and 0.71, respectively, indicating that the scale was reliable.
Adolescents were considered to have internalizing disorder if they scored above the 95th percentile (or the cutoff closest to the 95th percentile) on the internalizing factor. The 95th percentile was chosen because a prevalence of 5% corresponds to reported prevalences of adolescent depression and anxiety (1 – 4) .
Baseline Measures
Several variables describing early childhood were available to compare adolescents who had internalizing disorder with those who had no mental disorder at baseline. Such variables included gender, father’s social class when the cohort was age 15, cognitive ability, conduct problems, neuroticism, and extroversion. Cognitive ability was measured at age 15 with reading, vocabulary, and arithmetic tests normalized to a mean of 100 with a standard deviation of 15. A scale measuring conduct problems at ages 13 and 15 was conceived using the factor analysis described above (22 – 24) . Finally, the Pintner Aspects of Personality Inventory was used to measure neuroticism and extroversion at age 13 (26 , 27) .
Outcomes
Mental Disorder in Adulthood
The presence of mental disorder in adulthood was assessed with the Present State Examination (28) at age 36, the Psychiatric Symptom Frequency scale (29) at age 43, and the 28-item General Health Questionnaire (30) at age 53. The Present State Examination is a thorough clinical examination that assesses the frequency and severity of a variety of psychiatric symptoms in the preceding month (28) . The Psychiatric Symptom Frequency scale, which is based on items from the Present State Examination, is a self-administered 18-item scale that assesses symptoms of anxiety and depression during the preceding year (29) . The 28-item General Health Questionnaire is a self-administered questionnaire that focuses on symptoms of anxiety and depression in the preceding 4 weeks; it correlates highly with the Present State Examination (31) . Respondents were identified as having mental disorder at age 36 if they scored 5 or higher on the index of definition of the Present State Examination (32) , 23 or higher on the Psychiatric Symptom Frequency scale (29) , and 6 or higher on the General Health Questionnaire (33) .
Self-Reported History of “Nervous Trouble.”At ages 26, 36, and 43, cohort members were asked if they had ever suffered from “nervous trouble.”
Suicidal Ideation and Completed Suicide
Suicidal ideation and behavior were ascertained by responses to specific items in the questionnaires administered at ages 36, 43, and 53. Cohort members were classified as having suicidal ideation if they responded that they had “deliberately considered suicide” in the Present State Examination, responded that they had “thought about taking their own life” in the Psychiatric Symptom Frequency scale, or responded that they had “definitely thought about making away with themselves” or “definitely found that the idea of taking their life kept coming into their minds” in the General Health Questionnaire. Death by suicide was ascertained by notifications routinely sent by the Office of National Statistics to the NSHD office for every cohort member death in the U.K.
Physician Treatment for “Nerves.”At ages 36 and 43, cohort members were asked if they had visited a physician in the previous year for treatment of “nerves.”
Treatment With Psychotropic Medications
Cohort members reported all prescription medication use at ages 31, 36, 43, and 53. Psychotropic medications included any drug listed in the British National Formulary, section 4.1 (hypnotics and anxiolytics), section 4.2 (drugs used in psychoses and related disorders), or section 4.3 (antidepressant drugs) (34) .
Hospital Admissions for Psychiatric Treatment
Hospital admissions of NSHD cohort members have been identified through cohort questionnaires throughout their lifetime and subsequently verified through hospital records by NSHD researchers. All admissions for mental disorders (ICD-9 codes 290–314 and ICD-10 codes F10–F69 and F90–F98) and suicidal behavior (ICD-9 codes E950–E959 and ICD-10 codes X6000–X8499) were considered hospital admissions for psychiatric treatment.
Missing Data
Complete information for the teacher rating questionnaire items at ages 13 and 15 was required for an assessment of adolescent internalizing disorder. After exclusion of subjects who had missing data on any item, a sample of 3,279 remained. Sample sizes for each comparison in the analysis depended on the number of subjects responding to the survey at various times in adulthood; cohort members were included in the study even if they missed an outcome assessment in adulthood, as long as they had the original assessment in adolescence. Of the sample of 3,279, a total of 2,320 (70.8%) respondents participated in the assessments at age 36, 2,253 (68.7%) at age 43, and 2,064 (62.9%) at age 53.
Statistical Methods
Subjects were divided into three groups: those who had internalizing disorder at both ages 13 and 15 (“persistent” disorder); those who had internalizing disorder at either age 13 or age 15 (“single-episode” disorder); and those who did not have internalizing disorder at either age 13 or 15 (no disorder). The three groups were compared on several baseline and early childhood measures with chi-square tests for proportions and Mann-Whitney U tests for means. Within each group, similar tests were used to compare individuals for whom complete data were available for the entire follow-up period with those for whom data were incomplete in order to assess for bias.
The prevalence of psychiatric outcomes at several adult ages is presented for adolescents with persistent internalizing disorder, those with single-episode internalizing disorder, and those with no disorder. Odds ratios and 95% confidence intervals (CIs) were used to compare adolescents with persistent disorder and single-episode disorder with those who had no disorder. Odds ratios were adjusted for sex and father’s social class at age 15. In addition, odds ratios were adjusted for the presence of conduct problems at ages 13 and 15, because conduct disorder among adolescents has been shown to modify the effect between adolescent depression and adult psychiatric outcomes (10 , 17 , 18) . Stata, release 8.0 (Stata Corp., College Station, Tex., 2003), was used for all analyses.
Results
Of the 3,279 cohort members in the sample, 46 (1.4%) were identified as having persistent internalizing disorder in adolescence, 231 (7.0%) as having single-episode internalizing disorder, and 3,002 (91.6%) as having no disorder.
Table 1 summarizes the demographic and clinical characteristics of the three groups. Adolescents with internalizing disorder were more likely to be girls, to have a father from a manual social class, to have lower cognitive ability, to have a more neurotic and less extroverted personality, and to have conduct problems. All of these likelihoods were highest among adolescents with persistent disorder, and those with single-episode disorder were at an intermediate location between those with no disorder and those with persistent disorder.
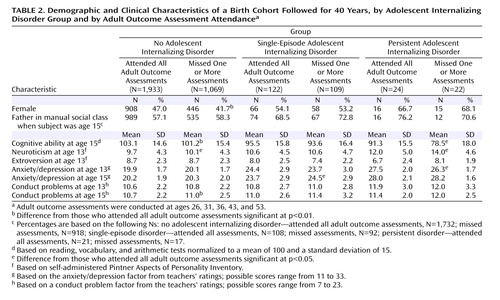
Table 2 compares those who provided information at all assessments in each group with those who missed one or more assessments. There were few significant differences between these two groups. Those who did not provide information at all assessments had lower mean scores on tests of cognitive ability and had slightly higher mean neuroticism scores; there were also some indications that they scored slightly higher on average on a scale measuring conduct problems. There were no indications that those who did not provide information at all assessments scored higher on average on scales assessing the presence of mental disorder compared with those who completed all interviews.
Mental Disorder in Adulthood
Adolescents with persistent internalizing disorder were significantly more likely than those with no disorder to have mental disorder in adulthood; no statistically significant differences were observed between the single-episode group and the no disorder group. While 25.2% of the no disorder group and 33.3% of the single-episode group had mental disorder at one of the adult assessments, 70.6% of the persistent disorder group had mental disorder at one or more of the adult assessments ( Table 3 ).
At ages 36, 43, and 53, the prevalence of mental disorder was not significantly higher in the single-episode group in comparison with the no disorder group ( Table 3 ). The prevalence of adulthood mental disorder in the persistent disorder group was significantly higher at ages 36 and 43 compared with the no disorder group. The prevalence of mental disorder at age 53 was elevated in the persistent disorder group, although this difference was not statistically significant.
In addition, adolescents with persistent disorder were significantly more likely to have multiple occurrences of mental disorder in adulthood; there was no significant difference between the single-episode group and the no disorder group ( Table 3 ).
Self-Reported History of “Nervous Trouble”
The frequency of reporting a history of nervous trouble at ages 26, 36, and 43 was not significantly different between the single-episode group and the no disorder group ( Table 3 ). However, it was significantly more common in the persistent disorder group at all three adult ages in comparison with the no disorder group, with odds ratios as high as 9.7.
Suicidal Ideation and Completed Suicide
Suicidal ideation was reported rarely at the three relevant enquiries (prevalence was less than 2% at ages 36, 43, and 53). Suicidal ideation was significantly more common in the single-episode group at age 36 (odds ratio=6.0; 95% CI=1.9–19.4) in comparison with the no disorder group, but not at ages 43 or 53. No significant differences were noted between the persistent disorder group and the no disorder group. Deaths by suicide were rare, with five suicides in the no disorder group, none in the single-episode group, and one in the persistent disorder group. The presence of one suicide among subjects in the persistent disorder group resulted in a significant increase in the odds of suicide in comparison with the no disorder group (odds ratio=13.5, 95% CI=1.5–118, unadjusted).
Physician Treatment for “Nerves”
There were no significant differences in frequency of physician treatment for nervous trouble at ages 36 and 43 between the single-episode group and the no disorder group, but physician treatment for nervous trouble at these ages was significantly more common in the persistent disorder group ( Table 4 ).
Treatment With Psychotropic Medications
Use of psychotropic medication at ages 31, 36, 43, and 53 was not significantly different between the single-episode group and the no disorder group ( Table 4 ). However, in the persistent disorder group, the proportion using psychotropic medication was significantly higher at ages 31, 36, and 43 in comparison with the no disorder group, with odds ratios in the range of 5.3 to 6.7. Use of psychotropic medications at age 53 was not significantly different between the persistent disorder group and the no disorder group.
Hospital Admissions for Psychiatric Treatment
Hospital admissions for psychiatric treatment were relatively rare throughout the follow-up period ( Table 4 ). Subjects in the persistent disorder group were significantly more likely than those in the no disorder group to have admissions for psychiatric treatment between ages 26 and 29. There were no significant differences between the groups at other ages.
Discussion
In this prospective, population-based follow-up study, persistent or recurrent internalizing disorder in adolescence was strongly associated with poor psychiatric outcomes in adulthood, while episodic or transient symptoms in adolescence were associated with fewer negative adult outcomes. These associations remained consistent over a 40-year follow-up period.
The long-term outcome for adolescents who had persistent or recurrent internalizing disorder was markedly poor, with odds ratios for mental disorder in adulthood as high as 9.5 when compared with adolescents with no disorder. Prospective studies of adolescent depression have reported higher rates of depression in adulthood for those whose symptoms were more persistent in comparison with those who had more transient episodes (35 , 36) . Our study shows similar results and confirms them across several ages and several different outcomes, including questionnaire-assessed and self-reported mental disorder as well as physician treatment and use of psychotropic medications for mental disorder.
The outcome for adolescents with a single episode of internalizing disorder, however, was not as negative as expected. There was little indication of any increase in frequency of poor adult outcomes across numerous measures, including mental disorder, self-reported nervous trouble, physician treatment for mental disorder, and use of psychotropic medications, compared with adolescents who had no internalizing disorder. These results challenge those from several studies that found poor adult mental health outcomes for adolescents with depression (8 – 14) and anxiety (10 , 15) .
There are several possible explanations for why our results differ from those of other studies. First, other studies did not stratify by duration of adolescent symptoms, which suggests that the association between adolescent depression and anxiety and poor adult mental health may be accounted for by adolescents with the most persistent symptoms. Second, several of the comparable studies used clinical samples of adolescents, who may be those most likely to suffer persistent symptoms.
A third explanation is that our study used teachers’ ratings of the adolescents’ mental health. Studies using the Rutter B2 scale (37) , in which teachers use a method similar to the scale used in our study to assess adolescent symptoms and behavior, have found that teachers may identify mental disorder in children more accurately than parents or the children themselves (38) and that teacher-rated mental disorder more accurately predicts future mental disorder than mental disorder based on parent or child ratings (39) . Nevertheless, it is possible that the outcome of teacher-identified adolescent internalizing disorder may differ from that of self-reported adolescent internalizing disorder.
A final possibility is that the adolescents with episodic mental disorder may have been misclassified. It is possible that these adolescents had other, unreported episodes and belong in the persistent disorder group. Alternatively, misclassification could have occurred as a result of regression to the mean between the two measurements in adolescence or of measurement error leading to some cases being classified as just below threshold when in fact they were just over the threshold; again, true persistent illness would have been wrongly classified as single-episode illness.
Misclassification tends to dilute observed differences between groups. This might explain why we found nonsignificant differences between the single-episode group and the no disorder group. However, one would expect a similar bias to exist in other, comparable studies. Furthermore, this effect would not explain why the persistent disorder group had a markedly worse prognosis than the other two groups; rather, the bias would have led to them to appear more similar.
While we obtained some mixed results on the question of whether adolescents who had a single episode of internalizing disorder had a higher risk of mental disorder in adulthood, it is clear that for the majority of these adolescents, the prognosis for adulthood was positive. Two-thirds of those in the single-episode group did not have mental disorder at any of the three adult ages at which they were tested. Furthermore, the prevalence of most mental disorder and psychiatric treatment outcomes at specific ages was less than 20%.
Mental disorder in early life, particularly depression, may differ according to age at onset. It has been suggested that even within the category of juvenile-onset depression, prepubertal-onset depression may differ from postpubertal-onset depression (40 , 41) . This theoretical framework has been supported by studies showing that the risk of poor adult mental health outcomes differs according to onset time of depression (prepubertal versus postpubertal) (13 , 40) . We did not have sufficient information to assess mental disorder in prepubertal childhood and were unable to stratify adolescents with mental disorder according to their onset age; thus, we may have combined two clinically distinct groups. We did compare adult outcomes for those with mental disorder at age 13 and those with mental disorder at age 15 and found few statistically significant differences (data not shown); however, this is unlikely to be a precise measure of child versus adolescent onset.
Most other follow-up studies of adolescent mental disorder have used DSM-type diagnoses in adolescence or adulthood, studying cohorts of adolescents with major depressive disorder, for example. Our cohort data did not provide us with precise enough information to make such diagnoses, which may limit our ability to compare our results with those of these other studies. Nevertheless, our results provide important information about the associations between severe internalizing disorder in adolescence and in adulthood.
A final limitation lies with sample attrition over the follow-up period, particularly among those who had adolescent internalizing disorder; almost half of these cohort members had left the study by age 53, a significantly larger proportion than the remainder of the cohort. This would introduce a bias if those who dropped out differed markedly from those who remained in the study. Analyses of those who left the study indicated few differences between those who completed all interviews and those who did not. Most important, there was no evidence that those who left the study were more likely to be those with more severe adolescent internalizing disorder. This suggests that those who stayed in the study should be representative of all the adolescents with internalizing disorder and that our associations were not biased.
In the face of these potential limitations, this study had several methodological strengths. The first is that the NSHD is a population-based sample representative of the population of England, Scotland, and Wales born in the post-Second World War period. The second is that the sample is large and allowed for follow-up of 277 adolescents with mental disorder, considerably more than most comparable studies. Third, because the NSHD is one of the oldest prospective cohort studies, it provides follow-up data much further into adult life than other epidemiological studies of adolescent depression. Finally, because the cohort members were born in 1946, the NSHD represents the postwar baby-boom generation that will be responsible for the imminent boom in the population of the elderly.
A remarkable aspect of this study is that assessment of mental disorder is based on data collected in 1959 and 1961, when clinicians widely believed that affective disorder did not exist in childhood and adolescence (42) . Yet, by using such relevant historical data, we were able to identify subjects with internalizing disorder in numbers similar to those that would be expected today (1 – 3) .
The results of this study suggest differing trajectories of mental disorder across the life course, with some adolescents with internalizing disorder proceeding to a life with persistent mental health problems while others conform to general population trends. Data of this type support a call for the incorporation of a longitudinal perspective into classifying phenotypes of mental disorder (43) as well as investigations into causation. Ongoing prospective studies such as the NSHD are likely to continue to be important in this regard.
1. Costello EJ, Angold A, Burns BJ, Stangl DK, Tweed DL, Erkanli A, Worthman CM: The Great Smoky Mountains Study of Youth: goals, design, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psychiatry 1996; 53:1129–1136Google Scholar
2. Verhulst FC, van der Ende J, Ferdinand RF, Kasius MC: The prevalence of DSM-III-R diagnoses in a national sample of Dutch adolescents. Arch Gen Psychiatry 1997; 54:329–336Google Scholar
3. Fergusson DM, Horwood LJ, Lynskey MT: Prevalence and comorbidity of DSM-III-R diagnoses in a birth cohort of 15 year olds. J Am Acad Child Adolesc Psychiatry 1993; 32:1127–1134Google Scholar
4. Ford T, Goodman R, Meltzer H: The British Child and Adolescent Mental Health Survey 1999: the prevalence of DSM-IV disorders. J Am Acad Child Adolesc Psychiatry 2003; 42:1203–1211Google Scholar
5. Puig-Antich J, Kaufman J, Ryan ND, Williamson DE, Dahl RE, Lukens E, Todak G, Ambrosini P, Rabinovich H, Nelson B: The psychosocial functioning and family environment of depressed adolescents. J Am Acad Child Adolesc Psychiatry 1993; 32:244–253Google Scholar
6. Flament MF, Cohen D, Choquet M, Jeammet P, Ledoux S: Phenomenology, psychosocial correlates, and treatment seeking in major depression and dysthymia of adolescence. J Am Acad Child Adolesc Psychiatry 2001; 40:1070–1078Google Scholar
7. Glied S, Pine DS: Consequences and correlates of adolescent depression. Arch Pediatr Adolesc Med 2002; 156:1009–1014Google Scholar
8. Weissman MM, Wolk S, Goldstein RB, Moreau D, Adams P, Greenwald S, Klier CM, Ryan ND, Dahl RE, Wickramaratne P: Depressed adolescents grown up. JAMA 1999; 281:1707–1713Google Scholar
9. Rao U, Ryan ND, Birmaher B, Dahl RE, Williamson DE, Kaufman J, Rao R, Nelson B: Unipolar depression in adolescents: clinical outcome in adulthood. J Am Acad Child Adolesc Psychiatry 1995; 34:566–578Google Scholar
10. Pine DS, Cohen P, Gurley D, Brook J, Ma Y: The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Arch Gen Psychiatry 1998; 55:56–64Google Scholar
11. Fergusson DM, Woodward LJ: Mental health, educational, and social role outcomes of adolescents with depression. Arch Gen Psychiatry 2002; 59:225–231Google Scholar
12. Lewinsohn PM, Rohde P, Klein DN, Seeley JR: Natural course of adolescent major depressive disorder, I: continuity into young adulthood. J Am Acad Child Adolesc Psychiatry 1999; 38:56–63Google Scholar
13. Harrington R, Fudge H, Rutter M, Pickles A, Hill J: Adult outcomes of childhood and adolescent depression, I: psychiatric status. Arch Gen Psychiatry 1990; 47:465–473Google Scholar
14. Harrington R, Bredenkamp D, Groothues C, Rutter M, Fudge H, Pickles A: Adult outcomes of childhood and adolescent depression, III: links with suicidal behaviours. J Child Psychol Psychiatry 1994; 35:1309–1319Google Scholar
15. Woodward LJ, Fergusson DM: Life course outcomes of young people with anxiety disorders in adolescence. J Am Acad Child Adolesc Psychiatry 2001; 40:1086–1093Google Scholar
16. Fergusson DM, Horwood LJ, Ridder EM, Beautrais AL: Subthreshold depression in adolescence and mental health outcomes in adulthood. Arch Gen Psychiatry 2005; 62:66–72Google Scholar
17. Fombonne E, Wostear G, Cooper V, Harrington R, Rutter M: The Maudsley long-term follow-up of child and adolescent depression, 1: psychiatric outcomes in adulthood. Br J Psychiatry 2001; 179:210–217Google Scholar
18. Fombonne E, Wostear G, Cooper V, Harrington R, Rutter M: The Maudsley long-term follow-up of child and adolescent depression, 2: suicidality, criminality, and social dysfunction in adulthood. Br J Psychiatry 2001; 179:218–223Google Scholar
19. Wadsworth MEJ: The Imprint of Time. Oxford, UK, Oxford University Press, 1991Google Scholar
20. Wadsworth ME, Butterworth SL, Hardy RJ, Kuh DJ, Richards M, Langenberg C, Hilder WS, Connor M: The life course prospective design: an example of benefits and problems associated with study longevity. Soc Sci Med 2003; 57:2193–2205Google Scholar
21. Wadsworth ME, Mann SL, Rodgers B, Kuh DJ, Hilder WS, Yusuf EJ: Loss and representativeness in a 43-year follow-up of a national birth cohort. J Epidemiol Community Health 1992; 46:300–304Google Scholar
22. Rodgers B: Behaviour and personality in childhood as predictors of adult psychiatric disorder. J Child Psychol Psychiatry 1990; 31:393–414Google Scholar
23. Jones P, Rodgers B, Murray R, Marmot M: Child development risk factors for adult schizophrenia in the British 1946 birth cohort. Lancet 1994; 344:1398–1402Google Scholar
24. Jones P, Murray R, Rodgers B: Childhood risk factors for adult schizophrenia in a general population birth cohort at age 43 years, in Neural Development and Schizophrenia. Edited by Mednick SA, Hollister JM. New York, Plenum, 1995, pp 151–176Google Scholar
25. van Os J, Jones P, Lewis G, Wadsworth M, Murray R: Developmental precursors of affective illness in a general population birth cohort. Arch Gen Psychiatry 1997; 54:625–631Google Scholar
26. Pintner R, Loftus JJ, Forlano G, Alster B: Aspects of Personality Inventory: Test and Manual. Yonkers, NY, World Book Co, 1937Google Scholar
27. Pintner R, Forlano G: Four retests of a personality inventory. J Educational Psychol 1938; 29:93–100Google Scholar
28. Wing JK, Cooper JE, Sartorius N: The measurement and classification of psychiatric symptoms. Cambridge, UK, Cambridge University Press, 1974Google Scholar
29. Lindelow M, Hardy R, Rodgers B: Development of a scale to measure symptoms of anxiety and depression in the general UK population: the Psychiatric Symptom Frequency Scale. J Epidemiol Community Health 1997; 51:549–557Google Scholar
30. Goldberg DP, Hillier VF: A scaled version of the General Health Questionnaire. Psychol Med 1979; 9:139–145Google Scholar
31. Banks MH: Validation of the General Health Questionnaire in a young community sample. Psychol Med 1983; 13:349–353Google Scholar
32. Wing JK, Mann SA, Leff JP, Nixon JM: The concept of a “case” in psychiatric population surveys. Psychol Med 1978; 8:203–217Google Scholar
33. Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, Rutter C: The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 1997; 27:191–197Google Scholar
34. British Medical Association and the Royal Pharmaceutical Society of Great Britain: British National Formulary. Beccles, Suffolk, William Clowes, 2002Google Scholar
35. Kovacs M, Akiskal HS, Gatsonis C, Parrone PL: Childhood-onset dysthymic disorder: clinical features and prospective naturalistic outcome. Arch Gen Psychiatry 1994; 51:365–374Google Scholar
36. Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH: Natural course of adolescent major depressive disorder in a community sample: predictors of recurrence in young adults. Am J Psychiatry 2000; 157:1584–1591Google Scholar
37. Rutter M: A children’s behaviour questionnaire for completion by teachers: preliminary findings. J Child Psychol Psychiatry 1967; 8:1–11Google Scholar
38. Kresanov K, Tuominen J, Piha J, Almqvist F: Validity of child psychiatric screening methods. Eur Child Adolesc Psychiatry 1998; 7:85–95Google Scholar
39. Sourander A, MultimAki P, Santalahti P, Parkkola K, Haavisto A, Helenius H, Nikolakaros G, Piha J, Tamminen T, Moilanen I, Kumpulainen K, Aronen ET, Linna SL, Puura K, Almqvist F: Mental health service use among 18-year-old adolescent boys: a prospective 10-year follow-up study. J Am Acad Child Adolesc Psychiatry 2004; 43:1250–1258Google Scholar
40. Weissman MM, Wolk S, Wickramaratne P, Goldstein RB, Adams P, Greenwald S, Ryan ND, Dahl RE, Steinberg D: Children with prepubertal-onset major depressive disorder and anxiety grown up. Arch Gen Psychiatry 1999; 56:794–801Google Scholar
41. Weissman MM: Juvenile-onset major depression includes childhood- and adolescent-onset depression and may be heterogeneous. Arch Gen Psychiatry 2002; 59:223–224Google Scholar
42. Parry-Jones WL: Historical aspects of mood and its disorders in young people, in The Depressed Child and Adolescent. Edited by Goodyer IM. Cambridge, UK, Cambridge University Press, 2001, pp 1–23Google Scholar
43. Colman I, Jones PB: Birth cohort studies in psychiatry: beginning at the beginning. Psychol Med 2004; 34:1375–1383Google Scholar