Sex Differences in Clinical Predictors of Suicidal Acts After Major Depression: A Prospective Study
Abstract
Objective: Whether sex differences exist in clinical risk factors associated with suicidal behavior is unknown. The authors postulated that among men with a major depressive episode, aggression, hostility, and history of substance misuse increase risk for future suicidal behavior, while depressive symptoms, childhood history of abuse, fewer reasons for living, and borderline personality disorder do so in depressed women. Method: Patients with DSM-III-R major depression or bipolar disorder seeking treatment for a major depressive episode (N=314) were followed for 2 years. Putative predictors were tested with Cox proportional hazards regression analysis. Results: During follow-up, 16.6% of the patients attempted or committed suicide. Family history of suicidal acts, past drug use, cigarette smoking, borderline personality disorder, and early parental separation each more than tripled the risk of future suicidal acts in men. For women, the risk for future suicidal acts was sixfold greater for prior suicide attempters; each past attempt increased future risk threefold. Suicidal ideation, lethality of past attempts, hostility, subjective depressive symptoms, fewer reasons for living, comorbid borderline personality disorder, and cigarette smoking also increased the risk of future suicidal acts for women. Conclusions: These findings suggest that the importance of risk factors for suicidal acts differs in depressed men and women. This knowledge may improve suicide risk evaluation and guide future research on suicide assessment and prevention.
Sex differences in suicidal behavior have long been recognized (1 – 5) . Studies have shown that men have higher suicide rates (1) , while women are at higher risk for suicide attempts (2 , 5) . Possible explanations include differences in the propensity to use lethal means, suicidal intent, and the use of substances within the context of suicidal behavior (3 , 6) .
Few cross-sectional studies have compared sex differences in the characteristics of suicide attempters. Adolescent male suicide victims are more likely to have conduct and substance use disorders, while female adolescents more frequently suffer from mood or anxiety disorders and have attempted suicide before (6) . Among adolescents and young adults (2) , female attempters were more likely to have posttraumatic stress disorder; attempts by males were more often triggered by financial problems. Four prospective studies (7 – 10) have compared risk factors for suicidal behavior in the two genders. Two studies of overlapping study groups examined 1,026 depressed melancholic inpatients and showed that, compared to matched depressed comparison subjects, female suicide victims more often were unmarried, were noncompliant with treatment, and had previously attempted suicide, while suicide in men was related to heredity for psychosis and brittle or sensitive personality (7 , 9) . Another multisite prospective study of 3,130 teenagers assessed anger at oneself, anger at society, and suicidal ideation (8) . Although an initial correlation between self-directed anger and subsequent suicidal ideation was noted in young men only, this correlation diminished over time. Finally, a 10-year prospective study of depressed or bipolar subjects (N=955), most of whom were inpatients, showed similar risk factors for suicidal acts in men and women once differences in the frequency of alcohol and drug abuse and having children under age 18 were taken into account (10) .
Across diagnoses, suicide attempters are typically women (11) . To investigate potential contributors to differences in rates and types of suicidal behavior in the two sexes, we examined the predictive power of putative risk factors for suicidal acts identified in our previous cross-sectional (11) and prospective (12) studies, hoping to identify clinical characteristics for men and women at high risk for suicidal acts at the time they sought treatment for a major depressive episode. We hypothesized that, apart from a history of attempted suicide, variables predicting suicidal acts would differ between the sexes. We postulated that aggression, hostility, and a history of substance use disorders would predict future suicidal behavior in men, while depressive symptoms, childhood history of abuse, fewer reasons for living, and comorbid borderline personality disorder would do so in women.
Method
Subjects
Written informed consent was given by 184 female and 130 male patients, ages 18–75 years, who had major depressive disorder or bipolar disorder according to the Structured Clinical Interview for DSM-III-R and were seeking treatment of a major depressive episode; 80% were inpatients. The exclusion criteria were current substance or alcohol abuse and active medical conditions that could confound characterization of psychopathology and diagnosis. The patients received naturalistic treatment in the community and were evaluated 3 months, 1 year, and 2 years after discharge. There were no differences in age, sex, inpatient status, suicide attempt history, cluster B personality disorder, or depression severity between the patients lost to follow-up and those who completed at least one assessment. Each follow-up interview assessed suicidal behavior during the intervening time period.
Assessment
Ratings were conducted by trained clinicians with at least a master’s degree (including A.K.B.) or by trained psychiatric nurses. Interrater reliability intraclass correlations ranged from 0.80 to 0.96.
The patients were evaluated as previously described (12) . Briefly, the measures included the International Personality Disorder Examination (13) , the Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II) (14) , the 17-item Hamilton Depression Rating Scale (HAM-D), the Beck Depression Inventory (BDI), the Brief Psychiatric Rating Scale (BPRS), the Brown-Goodwin Aggression Scale (15) , the Buss-Durkee Hostility Inventory (16) , the Barratt Impulsivity Scale (17) , the St. Paul-Ramsey Questionnaire for measuring life stressors (unpublished 1978 instrument of A.E. Lumry), the Beck Hopelessness Scale (18) , the Reasons for Living Inventory (19) , and the Global Assessment Scale (GAS) (20) . Childhood physical or sexual abuse and early parental separation were rated present or absent. Cigarette smoking was assessed as present or absent.
A suicide attempt was defined as a self-destructive act with intent to end one’s life. The number, method, and degree of medical damage of suicide attempts were recorded by using the Columbia Suicide History Form (21) . Suicidal ideation was assessed by using the Scale for Suicide Ideation (22) . Intent and severity of medical injury were recorded by using the Suicide Intent Scale (23) and Lethality Rating Scale (23) , respectively.
Statistical Methods
Clinical and demographic characteristics of both sexes at baseline were compared by means of two-sample t tests, nonparametric Wilcoxon tests, and chi-square statistics as appropriate. Second, sex differences in the time to a suicidal act were tested by a Cox proportional hazards regression model. Third, for each sex, the risk of suicide attempt or completion in the 2-year follow-up period was evaluated by using univariate Cox analysis with time to first attempt as the dependent variable and putative risk factors as predictors. Scale and continuous variables were entered as linear effects. Finally, a Cox multivariate analysis with all significant risk factors as predictors assessed the relative importance of these factors in predicting a future suicidal act for men and women separately.
Results
Baseline Characteristics of Subjects
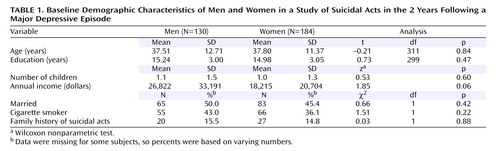
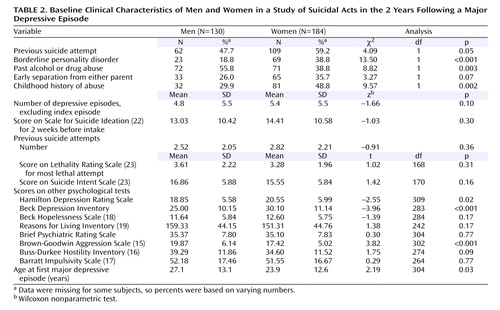
At the initial assessment, men and women did not differ in age, marital status, number of children, educational level, cigarette use, or family history of suicidal acts ( Table 1 ). More depressed women than men had made suicide attempts ( Table 2 ). However, they did not differ in suicidal ideation, suicidal intent, or severity of the medical damage caused by the most lethal attempt. Men and women had similar levels of impulsivity, hopelessness, hostility, reasons for living, psychiatric impairment, and frequency of early parental separation ( Table 2 ).
A higher proportion of depressed men had past alcohol or drug abuse, and men reported more aggression than women. Women had higher rates of childhood abuse and comorbid borderline personality disorder, and they had earlier onsets of major depression and greater severity of both subjective and objective depression.
Follow-Up of Men and Women: Univariate Analyses
During the 2-year follow-up, four subjects completed suicide and 48 attempted suicide, representing 16.6% of the study group. Men and women were followed for similar periods of time, but women were more likely to attempt suicide than men in the follow-up period (hazard ratio=1.8, likelihood ratio χ 2 =4.09, df=1, p<0.05) ( Figure 1 ).
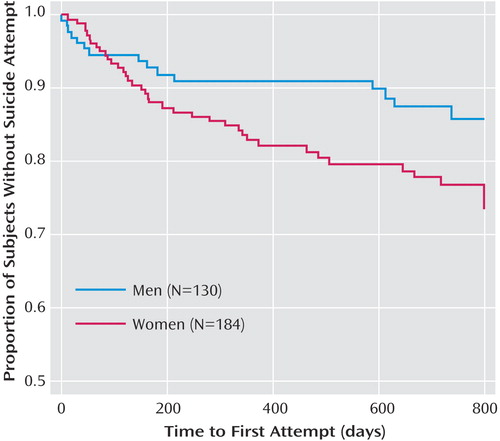
a Only the first 800 days are shown; the last recorded attempt was at 798 days.
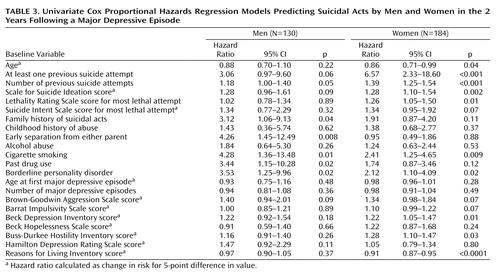
For men, the odds of a future suicidal act were threefold greater if they had made a prior attempt; this increase fell short of statistical significance. Additionally, family history of suicidal acts increased the risk threefold. As hypothesized, drug use and cigarette smoking each more than tripled and quadrupled, respectively, the risk of suicidal acts during follow-up. Comorbid borderline personality disorder and early parental separation also increased the risk of suicidal acts ( Table 3 ). There was a nonsignificant tendency of aggression, but not hostility, to predict future suicidal acts.
Although we hypothesized that depressed women with previous suicide attempts would have a greater risk for future suicidal acts, we did not anticipate the magnitude of this effect: a sixfold increase. Moreover, each prior attempt increased the risk of a future suicidal act by one-third. Suicidal ideation and lethality of past attempts also increased the risk of future suicidal acts for women ( Table 3 ). As hypothesized, greater subjective depression, fewer perceived reasons for living, and borderline personality disorder also increased the risk of a suicide attempt during follow-up. Like men, female cigarette smokers were at greater risk for suicidal acts. Contrary to our prediction, hostility was a significant risk factor in women; aggression and impulsivity tended to increase risk as well.
Follow-Up of Men and Women: Multivariate Analyses
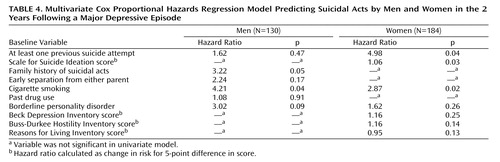
When all significant predictors of suicidal acts for men identified by univariate analyses ( Table 3 ) were evaluated together, cigarette smoking and family history of suicidal acts emerged as the most robust predictors of future suicidal acts ( Table 4 ), but early separation from family, borderline personality disorder, and past drug abuse were no longer predictive. Upon exploring reasons for the decreased effect of drug abuse on future suicidal acts, we found associations between drug abuse in men and smoking (71.1% of men with past drug abuse also smoked, p<0.0001), borderline personality disorder (p<0.0001), early parental separation (p<0.003), and past suicide attempts (p<0.03). In fact, the association between past drug abuse and smoking accounted for most of the predictive power of drug abuse among men (hazard ratio for drug abuse adjusted for smoking history=2.15, p<0.22); the rest of the effect of drug abuse on future risk was accounted for by the other aforementioned variables.
For women, the multivariate analyses revealed that previous attempts, suicidal ideation, and smoking had independent effects on the risk for suicidal acts ( Table 4 ). The presence of multiple suicide attempts, borderline personality disorder, greater subjective depression, fewer perceived reasons for living, and hostility were no longer significant. The effect of borderline personality disorder on future risk found in the univariate analyses was due to its close association with past attempts (hazard ratio for borderline personality disorder adjusted for previous attempt=1.35, p<0.39). Most of the depressed women with borderline personality disorder (81.2%) had past suicide attempts. However, we were unable to demonstrate the effects of hostility in the multivariate analysis, probably because of limitations in statistical power. The predictive power of hostility was not explained by its association with previous attempt history, borderline personality disorder, or any other variable from the model, despite hostility’s significant association with both borderline personality disorder and previous suicide attempts. Instead, the hazard ratio for hostility in the multivariate model was close to that from the univariate analysis, but the statistical significance of its predictive power decreased as more variables were added, ultimately resulting in a nonsignificant effect. This statistical limitation also appeared to be at work in the case of reasons for living.
Discussion
A previous suicide attempt is a powerful predictor of future suicidal acts (12 , 24) . In this study, men with past suicidal behavior had a threefold, but nonsignificantly, greater risk for future attempts. Women had a significant, sixfold higher risk of a future suicide attempt if they had made past attempts. The large effect among depressed women may be due to the earlier onset of depression among women, perhaps hampering the development of coping skills and rendering them more vulnerable to suicidal behavior. Alternatively, because men often use more lethal means than women, they may be more likely to die as a consequence of suicidal behavior, thus skewing clinical groups toward men with fewer, less lethal attempts.
Risk Factors for Men
Substance abuse has been reported to predict suicide attempts and completed suicide by people with mood disorders in general (25) . In this study group, past drug abuse predicted suicidal behavior in men only, a finding that is consistent with the observation that suicide deaths among men frequently occur within the context of substance use disorders (26) . Drug and alcohol misuse may predispose men to suicidal behavior in the setting of disruptions in important relationships (26) . Whether disinhibition (11) , serotonergic dysfunction (11) due to drug abuse, interpersonal factors, or a combination of these mediate the effect of drug abuse on future risk in men requires further study.
We expected aggression and hostility to affect future suicidal behavior in men. Our data suggest a 7% increase in risk for future suicidal acts for each point on the aggression scale, but the finding did not reach significance, nor did hostility predict suicidal acts. Although in this group, men reported more aggressive behavior than women, perhaps more aggressive depressed men at risk for suicidal acts do not seek treatment. We do not have data to address this possibility. Nonetheless, it has been noted that anger at oneself predicts suicidal ideation, not acts, in young men living in the community (8) . The relationship between anger at oneself and aggression is likely to be complex.
Family history of suicidal acts tripled the risk of future suicidal acts only for the men in our study. Suicidal behaviors cluster in families (27) , independent of the transmission of psychiatric conditions (28) . A large epidemiologic study (29) showed that a family history of psychiatric disorders increased the risk for suicide completion in both sexes, but it indicated a more robust effect of familial suicide on females than males. Whether family history affects males and females differently is unknown but could be related to genetic contributions from X-linked genes or mitochondrial DNA or differences in child rearing between the sexes. Moreover, the heritability of suicide attempts and completions in the two sexes may differ, resulting in these apparently contradictory results.
For men, early parental separation increased the risk of suicidal acts more than threefold. Early parental loss is a risk factor for suicide in adolescents and young adults regardless of sex (30 , 31) . One retrospective study (32) demonstrated that early loss, separation, or inadequate child rearing in young men was more strongly associated with death by suicide than with death from car accidents. Differential effects by sex may relate to genetic or rearing differences; perhaps girls can attach to new caretakers more easily in the absence of a parent.
Multivariate analyses uncovered that among depressed men, the predictive power of several of the variables could be explained by their relationship to the increased risk ascribable to cigarette smoking. This finding underscores the need for studies that have comprehensive clinical assessments so that such relationships can be uncovered, leading to accurate predictive models for suicidal behavior.
Risk Factors for Women
We hypothesized that women with more subjective depression, fewer perceived reasons for living, borderline personality disorder, or a history of childhood abuse would be more likely to engage in future suicidal behavior. Except for childhood abuse, these factors were predictive in univariate analyses. Each point increase on the BDI increased the risk for suicidal acts in women by 4%. We previously reported that subjective depression severity is a risk factor for suicidal acts (12) . Several studies have examined the predictive capacity of depressive subtype (33 – 36) , but none has focused on sex differences. The 1993 National Mortality Followback Survey (37) found that, compared to women with natural deaths, women who completed suicide had endorsed depressive symptoms at all ages; however, depression was only a factor among older male suicide victims, implying that other conditions, such as alcoholism or substance abuse, are associated with suicide in younger men, such as those included in our study group (mean age=38 years), and that depression as a risk factor for suicide by men appears later in life.
There was an inverse relationship between risk for suicidal behavior and scores on the Reasons for Living Inventory for women. Women may attach more importance to their responsibilities toward children, an important factor assessed by the Reasons for Living Inventory. Studies show that being married is protective for men, whereas having a child under the age of 2 is protective for women (10 , 29 , 38) . Among women, the protective effect of marriage against suicide has been attributed to the effect of having children (38 , 39) .
For women, the number of previous suicide attempts, suicidal ideation, lethality of prior attempts, and hostility all increased the risk for suicidal acts. Each previous suicide attempt increased the risk of subsequent attempts by over 30%. These findings are consistent with the findings from two prospective studies, in which women who committed suicide had previously attempted suicide but men had not (7 , 9) . Indeed, despite the similarity between men and women in the levels of suicidal intent, women’s use of less lethal means may result in more frequent survival of attempts.
Several (40 – 42) , but not all (12 , 43) , prospective studies have implicated suicidal ideation as a risk factor for future suicidal acts. Some cross-sectional studies showed greater suicidal ideation in female teens (44 , 45) , while others showed no sex differences in suicidal ideation, despite higher prevalences of suicidal behavior in women, younger persons, those living alone, and women in urban areas (46) . Thus, the predictive capacity of suicidal ideation requires further study.
We found that in women, for each increment in medical damage from the most lethal attempt, future suicidal risk increased by 26%, suggesting that lethality and frequency of suicidal behavior are related in women. This is of concern in light of reports that the proportions of men and women who make medically serious suicide attempts are similar despite the fact that twice as many women use nonlethal methods (47) . Examining the medical consequences of attempts made by women may help guide assessment of risk for future suicidal acts.
For women, greater hostility increased the risk for a suicidal act. Hostility in association with depression has been linked to suicidal behavior (11 , 48) , although why it should be predictive for women only is not clear. As mentioned previously, it is possible that more aggressive, hostile men at risk are not represented in clinical samples.
As was the case among men, multivariate analyses revealed that some of the predictive variables found in the univariate analyses owed their robustness to their association with other variables. Among women, past suicidal behavior explained the effect of borderline personality disorder on the future risk of suicidal acts. The complexity of finding appropriate predictors for rare events cannot be overstated.
Risk Factors Affecting Men and Women
We predicted that borderline personality disorder would increase the risk for suicidal acts in women. However, it also increased the risk for depressed men. Men and women with both major depression and borderline personality disorder have more suicide attempts and objective planning than do those with either diagnosis alone (49) . This was the case for the subjects in this study: 81% of the patients with borderline personality disorder had previous attempts. Among the female subjects, a history of suicide attempts accounted for the predictive power of borderline personality disorder. However, for men, the predictive power of borderline personality disorder was only partially explained by previous attempts. An association between “sensitive/brittle” personality and later suicide in depressed men but not women has been reported (7 , 9) . Brittleness and sensitivity are perhaps more typical of narcissistic personality disorder but may also be consistent with borderline personality disorder. Although borderline personality disorder is less often diagnosed in men, its presence alongside depression may pose incremental risk for future suicidal behavior.
The only other risk factor that significantly predicted future suicidal behavior in both sexes was cigarette smoking. Cigarette smoking increases the risk for suicidal acts (12 , 41 , 50) independent of the effects of major depression, alcohol abuse, or drug use (51) , and smokers are reported to have more aggressive or impulsive behaviors. Current smokers but not former smokers (52) have lower monoamine oxidase activity, which may result in serotonergic dysregulation, mediating the association of cigarette smoking with depression and suicide (11) .
Limitations
The inclusion of individuals treated at a university clinic and exclusion of current substance and alcohol users hamper the generalizability of our findings. For example, the exclusion of current substance abusers may explain our finding that aggression and hostility do not predict suicidal behavior in men. We followed the patients for 2 years only, although this is the period of highest risk for suicidal acts. The naturalistic design means that potentially relevant variables, such as the intensity of antidepressant treatment, presence of treatment refractoriness, and the time-varying nature of depressive symptoms, cannot be addressed.
Another limitation is that the statistical analyses to assess sex differences in the hazard ratios by using interaction terms (variable by sex) showed that the interaction terms lacked statistical significance, except in the case of parental separation. These results are reflected in the overlap in confidence intervals for the hazard ratio for women compared to men. It is possible that the smaller number of subjects and fewer future suicidal acts among men led to large differences in the hazard ratio estimates with wide confidence intervals for the two sexes, thus leading to nonsignificant differences. However, we think it is useful to document the hazard ratios within each sex because the order of importance of the individual risk factors differs in men and women. Moreover, in the multivariate models, while previous suicide attempts is an independent predictor for women, among men it is not driving the risk, just “standing in” for other factors.
From a clinical standpoint, the relative lack of protection afforded by reasons for living in men, compared to women, is notable. Furthermore, despite the well-documented fact that men are at greater risk for completed suicide, depressed female suicide attempters appear at relatively greater risk for repeated suicidal behavior. Thus, clinical evaluation may be enhanced by considering the difference between the sexes in the importance of risk factors for suicidal acts.
1. Oquendo MA, Ellis SP, Greenwald S, Malone KM, Weissman MM, Mann JJ: Ethnic and sex differences in suicide rates relative to major depression in the United States. Am J Psychiatry 2001; 158:1652–1658Google Scholar
2. Wunderlich U, Bronisch T, Wittchen HU, Carter R: Gender differences in adolescents and young adults with suicidal behavior. Acta Psychiatr Scand 2001; 104:332–339Google Scholar
3. Hawton K: Sex and suicide—gender differences in suicidal behavior. Br J Psychiatry 2000; 177:484–485Google Scholar
4. Weissman MM, Bland RC, Canino GJ, Greenwald S, Hwu H-G, Joyce PR, Karam EG, Lee C-K, Lellouch J, Lepine J-P, Newman SC, Rubio-Stipec M, Wells JE, Wickramaratne PJ, Wittchen H-U, Yeh E-K: Prevalence of suicide ideation and suicide attempts in nine countries. Psychol Med 1999; 29:9–17Google Scholar
5. Molnar BE, Shade SB, Kral AH, Booth RE, Watters JK: Suicidal behavior and sexual/physical abuse among street youth. Child Abuse Negl 1998; 22:213–222Google Scholar
6. Brent DA, Baugher M, Bridge J, Chen T, Chiappetta L: Age- and sex-related risk factors for adolescent suicide. J Am Acad Child Adolesc Psychiatry 1999; 38:1497–1505Google Scholar
7. Berglund M, Nilsson K: Mortality in severe depression: a prospective study including 103 suicides. Acta Psychiatr Scand 1987; 76:372–380Google Scholar
8. Goldney RD, Winefield A, Saebel J, Winefield H, Tiggeman M: Anger, suicidal ideation, and attempted suicide: a prospective study. Compr Psychiatry 1997; 38:264–268Google Scholar
9. Bradvik L, Berglund M: Risk factors for suicide in melancholia: a case-record evaluation of 89 suicides and their controls. Acta Psychiatr Scand 1993; 87:306–311Google Scholar
10. Young MA, Fogg LF, Scheftner WA, Fawcett JA: Interactions of risk factors in predicting suicide. Am J Psychiatry 1994; 151:434–435Google Scholar
11. Mann JJ, Waternaux C, Haas GL, Malone KM: Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry 1999; 156:181–189Google Scholar
12. Oquendo MA, Galfalvy H, Russo S, Ellis SP, Grunebaum MF, Burke A, Mann JJ: Prospective study of clinical predictors of suicidal acts after a major depressive episode in patients with major depressive disorder or bipolar disorder. Am J Psychiatry 2004; 161:1433–1441Google Scholar
13. Loranger AW, Sartorius N, Andreoli A, Berger P, Buchheim P, Channabasavanna SM, Coid B, Dahl A, Diekstra RFW, Ferguson B, Jacobsberg LB, Mombour W, Pull C, Ono Y, Regier DA: The International Personality Disorder Examination: the World Health Organization/Alcohol, Drug Abuse, and Mental Health Administration International Pilot Study of Personality Disorders. Arch Gen Psychiatry 1994; 51:215–224Google Scholar
14. Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II). Washington, DC, American Psychiatric Press, 1990Google Scholar
15. Brown GL, Goodwin FK, Ballenger JC, Goyer PF, Major LF: Aggression in humans correlates with cerebrospinal fluid amine metabolites. Psychiatry Res 1979; 1:131–139Google Scholar
16. Buss AH, Durkee A: An inventory for assessing different kinds of hostility. J Consult Psychol 1957; 21:343–349Google Scholar
17. Barratt ES: Factor analysis of some psychometric measures of impulsiveness and anxiety. Psychol Rep 1965; 16:547–554Google Scholar
18. Beck AT, Weissman A, Lester D, Trexler L: The measurement of pessimism: the Hopelessness Scale. J Consult Clin Psychol 1974; 42:861–865Google Scholar
19. Linehan MM, Goodstein JL, Nielsen SL, Chiles JA: Reasons for staying alive when you are thinking of killing yourself: the Reasons for Living Inventory. J Consult Clin Psychol 1983; 51:276–286Google Scholar
20. Endicott J, Spitzer RL, Fleiss JL, Cohen J: The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry 1976; 33:766–771Google Scholar
21. Oquendo MA, Halberstam B, Mann JJ: Risk factors for suicidal behavior: the utility and limitations of research instruments, in Standardized Evaluation in Clinical Practice. Edited by First MB. Arlington, Va, American Psychiatric Publishing, 2003, pp 103–130Google Scholar
22. Beck AT, Kovacs M, Weissman A: Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol 1979; 47:343–352Google Scholar
23. Beck AT, Beck R, Kovacs M: Classification of suicidal behaviors, I: quantifying intent and medical lethality. Am J Psychiatry 1975; 132:285–287Google Scholar
24. Leon AC, Keller MB, Warshaw MG, Mueller TI, Solomon DA, Coryell W, Endicott J: Prospective study of fluoxetine treatment and suicidal behavior in affectively ill subjects. Am J Psychiatry 1999; 156:195–201Google Scholar
25. Maser JD, Akiskal HS, Schettler P, Scheftner W, Mueller T, Endicott J, Solomon D, Clayton P: Can temperament identify affectively ill patients who engage in lethal or near-lethal suicidal behavior? a 14-year prospective study. Suicide Life Threat Behav 2002; 32:10–32Google Scholar
26. Rich CL, Ricketts JE, Fowler RC, Young D: Some differences between men and women who commit suicide. Am J Psychiatry 1988; 145:718–722Google Scholar
27. Brent DA, Oquendo MA, Birmaher B, Greenhill L, Kolko DJ, Stanley B, Zelazny J, Brodsky B, Bridge J, Ellis S, Salazar JO, Mann JJ: Familial pathways to early-onset suicide attempt: a high-risk study. Arch Gen Psychiatry 2002; 59:801–807Google Scholar
28. Egeland JA, Sussex JN: Suicide and family loading for affective disorders. JAMA 1985; 254:915–918Google Scholar
29. Qin P, Agerbo E, Mortensen PB: Suicide risk in relation to socioeconomic, demographic, psychiatric, and familial factors: a national register-based study of all suicides in Denmark, 1981–1997. Am J Psychiatry 2003; 160:765–772Google Scholar
30. Andrews JA, Lewinsohn PM: Suicidal attempts among older adolescents: prevalence and co-occurrence with psychiatric disorders. J Am Acad Child Adolesc Psychiatry 1992; 31:655–662Google Scholar
31. Benjaminsen S, Krarup G, Lauritsen R: Personality, parental rearing behaviour and parental loss in attempted suicide: a comparative study. Acta Psychiatr Scand 1990; 82:389–397Google Scholar
32. Duggan CF, Sham P, Lee AS, Murray RM: Can future suicidal behaviour in depressed patients be predicted? J Affect Disord 1991; 22:111–118Google Scholar
33. Grunebaum MF, Galfalvy HC, Oquendo MA, Burke AK, Mann JJ: Melancholia and the probability and lethality of suicide attempts. Br J Psychiatry 2004; 184:534–535Google Scholar
34. Brodaty H, MacCuspie-Moore CM, Tickle L, Luscombe G: Depression, diagnostic sub-type and death: a 25 year follow-up study. J Affect Disord 1997; 46:233–242Google Scholar
35. Lehmann HE, Fenton FR, Deutsch M, Feldman S, Engelsman F: An 11-year follow-up study of 110 depressed patients. Acta Psychiatr Scand 1988; 78:57–65Google Scholar
36. Thornicroft G, Sartorius N: The course and outcome of depression in different cultures: 10-year follow-up of the World Health Organization Collaborative Study on the Assessment of Depressive Disorders. Psychol Med 1993; 23:1023–1032Google Scholar
37. Kung HC, Pearson JL, Liu X: Risk factors for male and female suicide decedents ages 15–64 in the United States: results from the 1993 National Mortality Followback Survey. Soc Psychiatry Psychiatr Epidemiol 2003; 38:419–426Google Scholar
38. Qin P, Agerbo E, Westergard-Nielsen N, Eriksson T, Mortensen PB: Gender differences in risk factors for suicide in Denmark. Br J Psychiatry 2000; 177:546–550Google Scholar
39. Durkheim E: Suicide. Translated by Spaulding JA, Simpson G. New York, Free Press, 1951Google Scholar
40. Fawcett J, Scheftner W, Clark D, Hedeker D, Gibbons R, Coryell W: Clinical predictors of suicide in patients with major affective disorders: a controlled prospective study. Am J Psychiatry 1987; 144:35–40Google Scholar
41. Angst J, Clayton PJ: Personality, smoking and suicide: a prospective study. J Affect Disord 1998; 51:55–62Google Scholar
42. Schneider B, Philipp M, Muller MJ: Psychopathological predictors of suicide in patients with major depression during a 5-year follow-up. Eur Psychiatry 2001; 16:283–288Google Scholar
43. Gladstone GL, Mitchell PB, Parker G, Wilhelm K, Austin MP, Eyers K: Indicators of suicide over 10 years in a specialist mood disorders unit sample. J Clin Psychiatry 2001; 62:945–951Google Scholar
44. Allison S, Roeger L, Martin G, Keeves J: Gender differences in the relationship between depression and suicidal ideation in young adolescents. Aust NZ J Psychiatry 2001; 35:498–503Google Scholar
45. Rich AR, Kirkpatrick-Smith J, Bonner RL, Jans F: Gender differences in the psychosocial correlates of suicidal ideation among adolescents. Suicide Life Threat Behav 1992; 22:364–373Google Scholar
46. Renberg ES: Self-reported life-weariness, death-wishes, suicidal ideation, suicidal plans and suicide attempts in general population surveys in the north of Sweden 1986 and 1986. Soc Psychiatry Psychiatr Epidemiol 2001; 36:429–436Google Scholar
47. Beautrais AL, Joyce PR, Mulder RT, Fergusson DM, Deavoll BJ, Nightingale SK: Prevalence and comorbidity of mental disorders in persons making serious suicide attempts: a case-control study. Am J Psychiatry 1996; 153:1009–1014Google Scholar
48. Weissman M, Fox K, Klerman GL: Hostility and depression associated with suicide attempts. Am J Psychiatry 1973; 130:450–455Google Scholar
49. Soloff PH, Lynch KG, Kelly TM, Malone KM, Mann JJ: Characteristics of suicide attempts of patients with major depressive episode and borderline personality disorder: a comparative study. Am J Psychiatry 2000; 157:601–608Google Scholar
50. Tanskanen A, Viinamäki H, Hintikka J, Koivumaa-Honkanen H-T, Lehtonen J: Smoking and suicidality among psychiatric patients. Am J Psychiatry 1998; 155:129–130Google Scholar
51. Breslau N, Schultz LR, Johnson EO, Peterson EL, Davis GC: Smoking and the risk of suicidal behavior. Arch Gen Psychiatry 2005; 62:328–334Google Scholar
52. Whitfield JB, Pang D, Bucholz KK, Madden PAF, Heath AC, Statham DJ, Martin NG: Monoamine oxidase: associations with alcohol dependence, smoking and other measures of psychopathology. Psychol Med 2000; 30:443–454Google Scholar