The Caregiving Environments Provided to Children by Depressed Mothers With or Without an Antisocial History
Abstract
Objective: Many depressed women have a history of antisocial behavior, but research into maternal depression has not ascertained if this has implications for children of depressed mothers. This study compared the developmental outcomes in and caregiving environments provided to children by depressed mothers with or without an antisocial history. Method: In the Environmental Risk Longitudinal Twin Study, a nationally representative study of 1,106 families, mothers were administered the Diagnostic Interview Schedule for Major Depressive Disorder and interviewed about their lifetime history of antisocial personality disorder symptoms. Mothers and teachers provided information regarding the children’s behavior problems at 5 and 7 years of age. The authors assessed the quality of the caregiving environment through maternal reports and interviewer observations. Results: Compared with children of mothers with depression only, the children of depressed and antisocial mothers had significantly higher levels of antisocial behavior and rates of DSM-IV conduct disorder, even after the authors controlled for numbers of symptoms and chronicity of maternal major depressive disorder. The children of depressed and antisocial mothers were at an elevated risk of experiencing multiple caregiving abuses, including physical maltreatment, high levels of maternal hostility, and exposure to domestic violence. Conclusions: If one ignores the common co-occurrence of an antisocial history in depressed mothers, it may obscure the significantly elevated risks in children’s development. Clinicians treating women’s depression should be aware that children of depressed and antisocial mothers constitute a group at extremely high risk for early-onset psychopathology.
We previously reported that children of mothers with major depressive disorder and a history of antisocial personality disorder symptoms had the highest levels of antisocial behavior (1) . The present descriptive study, with data from a representative population-based sample of 1,116 mothers and their children, compared developmental outcomes in children and caregiving environments provided to children by depressed mothers with or without an antisocial history.
Studying the association between mothers’ depression and antisocial personality and the caregiving environments they provide is valuable for three reasons. First, estimates suggest that up to 10% of teenage girls meet diagnostic criteria for conduct disorder (2 , 3) and at least three-fourths of girls with conduct disorder are likely to experience major depression in adulthood (4 , 5) . Therefore, ignoring this common pattern of comorbidity can result in misleading conclusions about the risks maternal depression poses to children (6) . Second, the co-occurrence of antisocial behavior and depression in mothers may constitute a meaningfully distinctive disorder that deserves research attention (6) . Third, if risks faced by children of depressed mothers with or without an antisocial history differ, this knowledge can have useful implications for treatment.
Mental health problems that have their first onset early in life tend to signal a poor prognosis. Virtually all children with early-onset conduct disorder have mental disorders and poor functioning in adulthood (7) , and a considerable proportion of adults who have a psychiatric disorder have a history of childhood conduct disorder (8) . Internalizing problems in childhood may be a marker for early-onset depression, which tends to recur in adulthood (9) . To assess the degree to which children of depressed mothers in the community are at risk for early-onset psychopathology, we tested whether the children of depressed and antisocial mothers had significantly higher rates of DSM-IV conduct disorder, antisocial behavior, and internalizing problems, compared to children of mothers with depression only.
There is evidence that both maternal depression and maternal antisocial personality influence children’s psychopathology through a psychosocial process (1) . Researchers have proposed that these psychosocial risks include sociodemographic characteristics, a stressful family environment, and maladaptive parenting (10 , 11) , which are correlated with maternal depression. A chaotic family environment and poor parenting are also common in mothers with a history of antisocial behavior (2 , 12 , 13) . In the present study, we investigated whether the co-occurrence of depression and an antisocial history in a community sample of mothers was associated with a more stressful family environment and inadequate parenting, relative to that in mothers with depression only. This knowledge can generate hypotheses regarding the extreme elevation in behavioral problems among children of depressed and antisocial mothers.
Depressed women with or without an antisocial history may differ in terms of the type, number, and severity of depressive symptoms (14) . Accordingly, significant differences between the two groups in children’s mental health outcomes and aspects of the caregiving environment might be explained, not by maternal comorbidity status per se but by depression severity. Therefore, we addressed this possibility by controlling for the number of symptoms of major depressive disorder and chronicity in comparisons of depressed mothers with and without an antisocial history.
Method
Participants
The participants were members of the Environmental Risk Longitudinal Twin Study (E-Risk). The E-Risk sampling frame was two consecutive birth cohorts (1994 and 1995) of a birth register of twins born in England and Wales (15) . Of the 15,906 twin pairs born in these 2 years, 71% joined the register. Bias from nonresponse was corrected as follows.
The E-Risk Study probability sample was drawn by using a high-risk stratification sampling procedure. High-risk families were those in which the mother had her first birth when she was 20 years of age or younger. We used this sampling 1) to replace high-risk families who were selectively lost to the register through nonresponse and 2) to ensure sufficient base rates of children growing up in at-risk environments. Age at first childbearing was used as the risk-stratification variable because it was recorded for virtually all families in the register, it is relatively free of measurement error, and early childbearing is a known risk factor for children’s problem behaviors (16 , 17) . The sampling strategy resulted in a final sample in which one-third of the study mothers (younger only: N=314) constituted a 160% oversample of mothers who were at high risk based on their young age at the first birth (15–20 years). The other two-thirds of the study mothers (N=802) accurately represented all mothers in the general population (ages 15–48) in England and Wales in 1994–1995 (estimates derived from the General Household Survey [18] ). To provide unbiased statistical estimates that can be generalized to the population of British families with children born in the 1990s, the data reported in this article were corrected with weighting to represent the proportion of young mothers in that population.
The E-Risk Study sought a sample size of 1,100 families to allow for attrition in future years of the longitudinal study while retaining statistical power. An initial list of families who had same-sex twins was drawn from the register to target for home visits. Of the families from the initial list, 1,116 (93%) participated in home-visit assessments when the twins were age 5 years, forming the base sample for the study: 4% of the families refused, and 3% could not be reached after many attempts. Written informed consent was obtained from the mothers. With the parents’ permission, questionnaires were posted to the children’s teachers, and the teachers returned questionnaires for 94% of the cohort children. The mothers were, on average, 33 years old at the first assessment (SD=5 years and 10 months).
A follow-up home visit was conducted 18–24 months after the children’s age-5 assessment (hereafter called the age-7 follow-up). Follow-up data were collected for 98% of the 1,116 families in the E-Risk Study. At this follow-up, teacher questionnaires were obtained for 91% of the 2,232 children in the E-Risk Study (93% of those taking part in the follow-up). The E-Risk Study received ethical approval from the Maudsley Hospital Ethics Committee.
Maternal Psychopathology Measures
At the first assessment, the mothers’ major depressive disorder was assessed with the Diagnostic Interview Schedule (20) according to DSM-IV criteria. Unweighted, the prevalence of maternal lifetime major depressive disorder was 35% (N=390, 33% when weighted to represent the population). With a life event calendar to aid recall (20) , the mothers who met criteria for major depressive disorder specified whether they experienced episodes of depression at any time during the twins’ first 5 years of life. Unweighted, 317 of the mothers (28%) had a major depressive disorder during the twins’ first 5 years of life (26% when weighted to represent the population). The chronicity of major depressive disorder was a count of developmental periods during the twins’ first 5 years of life (i.e., the first year, between ages 1 and 4, and between ages 4 and 5 years) that mothers reported having had a depressive episode.
At the first assessment, the mothers reported on their own antisocial history. Questions were derived from the Diagnostic Interview Schedule (20) that assessed the lifetime presence of antisocial personality disorder symptoms, supplemented by items from the Young Adult Behavior Checklist (21) . The DSM-IV symptom criteria for antisocial personality disorder covered illegal behavior, deceitfulness, impulsivity, aggressiveness, recklessness, and irresponsibility. The seventh symptom, lack of remorse, was not asked of mothers about themselves because valid self-reports of remorse are difficult to obtain. A symptom was considered to be present if the mother reported behavioral items representing the symptom as being “very true or often true.” Symptom counts ranged from 0 to 6 (mean=0.56, SD=1.05). The mothers were considered to have some evidence of an antisocial history if they had one or more lifetime antisocial personality disorder symptoms (N=373, 33%; 29% when weighted to represent the population).
Maternal Psychopathology Groups
We created four groups of women according to their major depressive disorder diagnosis during their children’s first 5 years of life and their lifetime antisocial personality disorder symptoms:
The comparison group (N=572) had no major depressive disorder and no antisocial personality disorder symptoms.
The depressed group (N=165) had major depressive disorder but no antisocial personality disorder symptoms.
The antisocial group (N=217) had no major depressive disorder but had one or more antisocial personality disorder symptoms.
The comorbid group (N=152) had both major depressive disorder and one or more antisocial personality disorder symptoms.
Other Measures
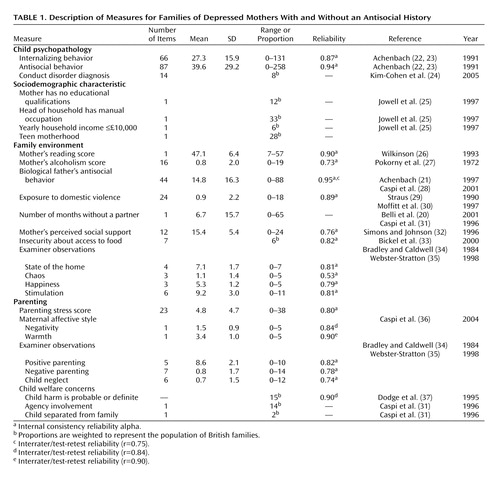
All dependent variables in this study were obtained at the first and follow-up assessments. Distributions and prevalence rates in this cohort for these measures are summarized in Table 1 and have been reported elsewhere (17 , 24) . (An appendix with detailed descriptions is available at http://psych.wisc.edu/moffitt/kim-cohen2006.htm or by request from the first author.) Reliability coefficients for all but one measure exceeded 0.70. All continuous variables were transformed into z scores.
Statistical Analysis
Planned contrast analyses (38) were used to compare depressed and antisocial mothers with mothers who were depressed only on dependent variables. Group differences were evaluated with odd ratios (for dichotomous variables) and t tests (for continuous variables).
Statistical analysis was complicated by the fact that our twin study contained two children from each family. Thus, for dependent variables that were measured separately for each twin (e.g., physical maltreatment), we analyzed data on all available children with tests based on the sandwich or Huber-White variance estimator (39 , 40) , a method available in Stata 8.0 (41) that adjusts estimated standard errors to account for the dependence in the data due to analyzing two children per family. For dependent variables that were the same within twin pairs (e.g., family income), we analyzed data for all available families.
Results
Child Psychopathology
Compared with children of mothers who were depressed only, the children of mothers who were depressed and antisocial (hereafter called comorbid) had significantly higher levels of antisocial behavior but similar levels of internalizing behavior problems ( Table 2 ). Compared with children of mothers who were antisocial only, the children of comorbid mothers had significantly higher levels of antisocial and internalizing problems.
The children of comorbid mothers were significantly more likely to meet diagnostic criteria for conduct disorder than the children of mothers who were depressed only ( Figure 1 ) (odds ratio adjusted for sex=2.2, 95% confidence interval [CI]=1.2–3.8) and the children of mothers who were antisocial only (adjusted odds ratio=1.8, 95% CI=1.1–2.9). Sex of the child was controlled in analyses predicting child psychopathology. Interactions of maternal psychopathology by child sex were nonsignificant.

Sociodemographic Characteristics
Compared with depressed and antisocial mothers, comorbid mothers were significantly more likely to have family income levels below £10,000 (British) per year, despite having similar levels of maternal education and head-of-household occupational status ( Table 2 ). Compared with mothers with depression only, comorbid mothers were significantly more likely to have been adolescent mothers.
Family Environment
Compared with mothers with depression only, comorbid mothers were poorer readers and reported significantly more alcohol-related problems, more insecurity about having enough food, more antisocial behavior in the biological fathers of their children, higher levels of domestic violence, and more months with no partner in the home ( Table 2 ). Examiners who were blind to maternal psychopathology grouping rated home environments of comorbid mothers as significantly more chaotic than the homes of mothers with depression only.
Compared with mothers who were antisocial only, comorbid mothers reported more alcohol problems, more insecurity about having enough food, more antisocial behavior in the biological fathers of their children, and less social support.
Parenting
Compared with depressed or antisocial mothers, comorbid mothers self-reported significantly higher levels of parenting stress ( Table 2 ). On measures of expressed emotion, comorbid mothers were rated by blinded coders as expressing significantly less warmth and more negativity toward their children than mothers with depression only, and more negativity than antisocial mothers. Compared with depressed mothers, comorbid mothers engaged in significantly more negative parenting, as rated by observers.
Compared with children of mothers with depression only, the children of comorbid mothers were 2.2 times (95% CI=1.3–3.8) more likely to have experienced physical maltreatment. Compared with children of mothers who were antisocial only, the children of comorbid mothers were significantly more likely to have been separated from their families and were 2.7 times (95% CI=1.6–4.6) more likely to have experienced physical maltreatment.
Maternal Depressive Symptoms
The profiles of major depressive disorder symptoms in depressed women with or without an antisocial history were similar, with the exception that psychomotor agitation, feelings of guilt or worthlessness, and suicidal thoughts were significantly more prevalent among depressed and antisocial women ( Table 3 ). Comorbid women had significantly higher numbers of depressive symptoms and periods of depression compared with women with depression only. The two groups did not differ on self-rated levels of impairment or help seeking from a professional for depression.
Does Maternal Comorbidity Account for Group Differences, or Are They Accounted for by Maternal Symptoms and Chronicity?
After we controlled for the number of maternal symptoms of major depressive disorder and the chronicity of major depressive disorder, externalizing behavior problems in children of comorbid mothers remained significantly higher compared with those in the children of mothers with depression only (antisocial behavior scale: t=2.11, df=673, p<0.05) (conduct disorder diagnosis—adjusted odds ratio=1.9, 95% CI=1.1–3.4). After we controlled for the number of maternal symptoms of major depressive disorder and the chronicity of major depressive disorder, all significant group contrasts in the family environment and parenting remained significant (p≤0.05) ( Table 2 ), with the exception of insecurity about having enough food and parenting stress.
Although not a primary focus of this study, we found that compared with mothers who were antisocial only, comorbid mothers had significantly more antisocial personality disorder symptoms (mean=1.78, SD=0.94, versus mean=2.38, SD=1.31) (F=4.65, df=1, 367, p<0.001). After we controlled for the number of antisocial personality disorder symptoms, the significant group differences reported for children’s internalizing and antisocial behavior problems, the diagnosis of conduct disorder, insecurity about having enough food, maternal expressed negativity, and separation from the family were no longer significant. After we controlled for the number of antisocial personality disorder symptoms, group differences remained significant (at p<0.05) for maternal alcoholism, maternal social support, parenting stress, and child physical harm.
Discussion
Over 20 years ago, Rutter and Quinton (44) emphasized the importance of assessing personality functioning in addition to a parent’s primary disorder to better understand the associated risks for children’s psychopathology. The present study demonstrated that the family and parenting experiences of children of depressed mothers with one or more symptoms of antisocial personality disorder differ markedly from those of children whose depressed mothers have no antisocial history.
Compared with children of mothers with depression only, the children of comorbid mothers in our study were more likely to live under financial hardship, to be exposed to domestic violence, and to have a mother with drinking problems who was also at an elevated risk for suicide. These children received low levels of maternal warmth and high levels of maternal hostility and were at a high risk of physical maltreatment. Such social-contextual factors are well-established risks for conduct disorder (45) , so it may not be surprising that nearly 20% of the children of depressed and antisocial mothers met diagnostic criteria for conduct disorder by age 7. Despite the greater degree of risks in their caregiving contexts, however, the children of comorbid mothers had similar levels of internalizing problems compared with the children of mothers with depression only. Thus, externalizing comorbidity in depressed mothers appears to elevate risk, specifically for young children’s externalizing problems.
Depressed and antisocial mothers are likely to bear children with highly antisocial men who may also contribute substantially to a risk for children’s antisocial behavior. However, previous research has demonstrated that antisocial fathers are often absent from the family and tend to be uninvolved in child rearing (46) . Moreover, we have shown previously that even after we controlled for fathers’ antisocial history (an index of both genetic and environmental risk), mothers’ depression and antisocial personality disorder symptoms were still significant risks for their children’s antisocial behavior (1) .
Although the patterns of depressive symptoms were largely the same in comorbid mothers compared with mothers with depression only, comorbid mothers were significantly more likely to report suicidal ideation and suicide attempts. Previous research has shown that depressed and conduct-disordered individuals have higher rates of suicide attempts than individuals with depression only (47) . For women especially, internalizing and externalizing psychopathology has been shown to interact to increase the risk for suicide attempts (48) . Suicidal behavior is familial (49) , and a past suicide attempt by a depressed mother is among the strongest predictors of suicidal behavior in children (50) . Taken together, these findings heighten concern regarding future suicide risk in children of depressed and antisocial mothers.
This study’s findings should be interpreted in light of five limitations. First, we could not assess the impact of maternal antisocial personality disorder diagnoses because we did not have access to the mothers’ histories of conduct disorder in childhood, which is a criterion for DSM-IV antisocial personality disorder. In any case, women meet the full criteria for antisocial personality disorder so seldom that even in our sample of 1,116 mothers, studying a diagnostic group would have presented problems of statistical power. Second, we could not determine the possible role of maternal bipolar disorder or borderline personality disorder because they were not assessed. Future research should examine whether women who are comorbid for major depressive disorder and antisocial traits have illnesses that resemble bipolar or borderline characteristics. Third, some women who are antisocial only may be at risk for eventually developing depression (4) and may need to be reclassified into the comorbid group. However, the risk of new-onset depression decreases with age (8) , and their children may grow out of the early developmental risk period by that time. Fourth, we did not diagnose children’s depression because of their young age. However, we will follow up this sample of children to obtain their depression diagnoses in future assessments. Fifth, we cannot be certain that our findings, based on a sample of twins and their mothers in England and Wales, will generalize to mothers and their singletons elsewhere. However, our prevalence estimates of childhood conduct disorder, maternal major depressive disorder, and maternal antisocial traits are comparable to epidemiological studies in other countries (51 – 54) .
Clinical Implications
Previous research has shown that when maternal depression co-occurs with axis II symptoms, such as antisocial personality disorder, at least four factors distinguish it from pure depression. First, depressed adults with personality disorder symptoms have been shown to have an earlier age of onset of major depressive disorder (55) . Second, when a personality disturbance is present, depressive symptoms tend to persist and to be chronic (56) . Third, the risk for suicide is significantly elevated among women with depression and antisocial personality (48) , suggesting that comorbid mothers should be carefully screened for the risk of suicide. Fourth, comorbid depression is less likely to respond to treatments that are effective with primary depression (55) .
The present study suggests a fifth distinguishing factor: depressed and antisocial mothers are at particular risk of providing offspring with suboptimal caregiving environments, and the children of depressed and antisocial mothers are at extremely high risk for early-onset psychopathology. The multiple caregiving risks in families of depressed and antisocial mothers identified in this study suggest that a child-centered approach to treatment will fall short of addressing their needs. Therefore, a multipronged approach that combines child-focused problem-solving and parent-focused child management skills with an additional parent-focused stress management component is recommended (57) . Given that depression and antisocial behavior are familial over multiple generations (9 , 12) , intervening to improve mental health functioning in children of depressed and antisocial mothers represents an important prevention opportunity.

1. Kim-Cohen J, Moffitt TE, Taylor A, Pawlby SJ, Caspi A: Maternal depression and children’s antisocial behavior: nature and nurture effects. Arch Gen Psychiatry 2005; 62:172–181Google Scholar
2. Pajer KA: What happens to “bad” girls? a review of the adult outcomes of antisocial adolescent girls. Am J Psychiatry 1998; 155:862–870Google Scholar
3. Zoccolillo M: Gender and the development of conduct disorder. Dev Psychopathol 1993; 5:65–78Google Scholar
4. Moffitt TE, Caspi A, Rutter M, Silva P: Sex Differences in Antisocial Behaviour. Cambridge, UK, Cambridge University Press, 2001Google Scholar
5. Zoccolillo M: Co-occurrence of conduct disorder and its adult outcomes with depressive and anxiety disorders: a review. J Am Acad Child Adoles Psychiatry 1992; 31:547–556Google Scholar
6. Rutter M: Comorbidity: concepts, claims and choices. Crim Behav Ment Health 1997; 7:265–285Google Scholar
7. Moffitt TE: Life-course-persistent and adolescence-limited antisocial behavior: a 10-year research review and research agenda, in Causes of Conduct Disorder and Juvenile Delinquency. Edited by Lahey BB, Moffitt TE, Caspi A. New York, Guilford, 2003, pp 49–74Google Scholar
8. Kim-Cohen J, Caspi A, Moffitt TE, Harrington HL, Milne BJ, Poulton R: Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry 2003; 60:709–717Google Scholar
9. Weissman MM, Jensen P: What research suggests for depressed women with children. J Clin Psychiatry 2004; 63:641–647Google Scholar
10. Goodman SH, Gotlib IH: Children of Depressed Parents. Washington, DC, American Psychological Association, 2002Google Scholar
11. Johnson JG, Cohen P, Kasen S, Smailes E, Brook JS: Association of maladaptive parental behavior with psychiatric disorder among parents and their offspring. Arch Gen Psychiatry 2001; 58:453–460Google Scholar
12. Serbin L, Karp J: Intergenerational studies of parenting and the transfer of risk from parent to child. Curr Directions Psychol Sci 2003; 4:138–142Google Scholar
13. Jaffee SR, Belsky J, Harrington HL, Caspi A, Moffitt TE: When parents have a history of conduct disorder: how is the caregiving environment affected? J Abnorm Psychol 2006 (in press)Google Scholar
14. Fombonne E, Wostear G, Cooper V, Harrington R, Rutter M: The Maudsley long-term follow-up of child and adolescent depression, I: psychiatric outcomes in adulthood. Br J Psychiatry 2001; 179:210–217Google Scholar
15. Trouton A, Spinath FM, Plomin R: Twins Early Development Study (TEDS): a multivariate, longitudinal genetic investigation of language, cognition, and behavior problems in childhood. Twin Res 2002; 5:444–448Google Scholar
16. Maynard RA: Kids Having Kids: Economic Costs and Social Consequences of Teen Pregnancy. Washington, DC, Urban Institute Press, 1997Google Scholar
17. Moffitt TE, the E-Risk Study Team: Teen-aged mothers in contemporary Britain. J Child Psychol Psychiatry 2002; 43:727–742Google Scholar
18. Bennett N, Jarvis L, Rowlands O, Singleton N, Haselden L: Living in Britain: Results From the General Household Survey. London, Her Majesty’s Stationery Office, 1996Google Scholar
19. Belli RF, Shay WL, Stafford FP: Event history calendars and question list surveys: a direct comparison of interviewing methods. Public Opin Q 2001; 65:45–74Google Scholar
20. Robins L, Cottler L, Bucholz K, Compton W: Diagnostic Interview Schedule for DSM-IV. St Louis, Washington University School of Medicine, 1995Google Scholar
21. Achenbach TM: Manual for the Young Adult Self-Report and Young Adult Behavior Checklist. Burlington, University of Vermont, Department of Psychiatry, 1997Google Scholar
22. Achenbach TM: Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington, University of Vermont, Department of Psychiatry, 1991Google Scholar
23. Achenbach TM: Manual for the Teacher’s Report Form and 1991 Profile. Burlington, University of Vermont, Department of Psychiatry, 1991Google Scholar
24. Kim-Cohen J, Arseneault L, Caspi A, Tomas MP, Taylor A, Moffitt TE: Validity of DSM-IV conduct disorder in 4–5-year-old children: a longitudinal epidemiological study. Am J Psychiatry 2005; 162:1108–1117Google Scholar
25. Jowell R, Cutice J, Park A, Brook L, Thomson K, Bryson C: British Social Attitudes: the 14th Report. Aldershot, UK, Ashgate, 1997Google Scholar
26. Wilkinson GS: The Wide Range Achievement Test, 3rd ed. Wilmington, Del, Wide Range, 1993Google Scholar
27. Pokorny AD, Miller BA, Kaplan HB: The brief MAST: a shortened version of the Michigan Alcoholism Screening Test. Am J Psychiatry 1972; 129:342–345Google Scholar
28. Caspi A, Taylor A, Smart M, Jackson J, Moffitt TE: Can women provide reliable information about their children’s fathers? cross-informant agreement about men’s lifetime antisocial behaviour. J Child Psychol Psychiatry 2001; 42:915–920Google Scholar
29. Straus MA: Measuring intrafamily conflict and violence: the Conflict Tactics (CT) Scales, in Physical Violence in American Families: Risk Factors and Adaptations to Violence in 8,145 Families. Edited by Straus MA, Gelles RJ. New Brunswick, NJ, Transaction, 1990, pp 403–424Google Scholar
30. Moffitt TE, Caspi A, Krueger RF, Magdol L, Margolin G, Silva PA, Sydney R: Do partners agree about abuse in their relationship? a psychometric evaluation of interpartner agreement. Psychol Assess 1997; 9:47–56Google Scholar
31. Caspi A, Moffitt TE, Thornton A, Freedman D, Amell JW, Harrington H: The life history calendar: a research and clinical assessment method for collecting retrospective event-history data. Int J Methods Psychiatr Res 1996; 6:101–114Google Scholar
32. Simons RL, Johnson C: The impact of marital and social network support on quality of parenting, in Handbook of Social Support and the Family. Edited by Pierce GR, Sarason BR, Sarason IG. New York, Plenum, 1996, pp 269–287Google Scholar
33. Bickel G, Nord M, Price C, Hamilton W, Cook J: Guide to Measuring Household Food Security. Alexandria, Va, Office of Analysis, Nutrition, and Evaluation, Food and Nutrition Service, US Department of Agriculture, 2000Google Scholar
34. Bradley RH, Caldwell BM: The home inventory and family demographics. Dev Psychol 1984; 20:315–320Google Scholar
35. Webster-Stratton C: Preventing conduct problems in Head Start children: strengthening parenting competencies. J Consult Clin Psychol 1998; 66:715–730Google Scholar
36. Caspi A, Moffitt TE, Morgan J, Rutter M, Taylor A, Arseneault L, Tully L, Jacobs C, Kim-Cohen J, Polo-Tomas M: Maternal expressed emotion predicts children’s antisocial behavior problems: using monozygotic-twin differences to identify environmental effects on behavioral development. Dev Psychol 2004; 40:149–161Google Scholar
37. Dodge KA, Pettit GS, Bates JE, Valente E: Social information-processing patterns partially mediate the effect of early physical abuse on later conduct problems. J Abnorm Psychol 1995; 104:632–643Google Scholar
38. Rosenthal R, Rosnow RL, Rubin DB: Contrasts and Effect Sizes in Behavioral Research: A Correlational Approach. Cambridge, UK, Cambridge University Press, 2000Google Scholar
39. Rogers WH: Regression standard errors in clustered samples. Stata Tech Bull 1993; 13:19–23Google Scholar
40. Williams RL: A note on robust variance estimation for cluster-correlated data. Biometrics 2000; 56:645–646Google Scholar
41. Stata Statistical Software: Release 8.0. College Station, Tex, Stata Corp, 2003Google Scholar
42. Cohen J: A power primer. Psychol Bull 1992; 112:155–159Google Scholar
43. Rao JNK, Scott AJ: On chi-square tests for multiway contingency tables with cell proportions estimated from survey data. Ann Stat 1984; 12:46–60Google Scholar
44. Rutter M, Quinton D: Parental psychiatric disorder: effects on children. Psychol Med 1984; 14:853–880Google Scholar
45. Lahey BB, Moffitt TE, Caspi A: Causes of Conduct Disorder and Juvenile Delinquency. New York, Guilford, 2003Google Scholar
46. Jaffee SR, Moffitt TE, Caspi A, Taylor A: Life with (or without) father: the benefits of living with two biological parents depend on the father’s antisocial behavior. Child Dev 2003; 74:109–126Google Scholar
47. Fombonne E, Wostear G, Cooper V, Harrington R, Rutter M: The Maudsley long-term follow-up of child and adolescent depression, 2: suicidality, criminality and social dysfunction in adulthood. Br J Psychiatry 2001; 179:218–223Google Scholar
48. Verona E, Sachs-Ericsson N, Joiner TE Jr: Suicide attempts associated with externalizing psychopathology in an epidemiological sample. Am J Psychiatry 2004; 161:444–451Google Scholar
49. Brent DA, Bridge JA, Johnson BA, Connolly J: Suicidal behavior runs in families: a controlled family study of adolescent suicide victims. Arch Gen Psychiatry 1996; 53:1145–1152Google Scholar
50. Klimes-Dougan B, Free K, Ronsaville D, Stilwell J, Welsh CJ, Radke-Yarrow M: Suicidal ideation and attempts: a longitudinal investigation of children of depressed and well mothers. J Am Acad Child Adolesc Psychiatry 1999; 38:651–659Google Scholar
51. Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A: Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry 2003; 60:837–844Google Scholar
52. Kendler KS, Prescott CA, Myers J, Neale MC: The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry 2003; 60:929–937Google Scholar
53. Lahey BB, Loeber R, Quay HC, Applegate B, Shaffer D, Waldman I, Hart EL, McBurnett K, Frick PJ, Jensen PS, Dulcan MK, Canino G, Bird HR: Validity of DSM-IV subtypes of conduct disorder based on age of onset. J Am Acad Child Adolesc Psychiatry 1998; 37:435–442Google Scholar
54. Zoccolillo M, Price R, Ji THC, Hwu H: Antisocial personality disorder: comparisons of prevalence, symptoms, and correlates in four countries, in Historical and Geographical Influences on Psychopathology. Edited by Cohen P, Slomkowski C, Robins L. Mahwah, NJ, Lawrence Erlbaum Associates, 1999, pp 249–277Google Scholar
55. Black DW, Bell S, Hulbert J, Nasrallah A: The importance of axis II in patients with major depression: a controlled study. J Affect Disord 1988; 14:115–122Google Scholar
56. Rothschild L, Zimmerman M: Personality disorders and the duration of depressive episode: a retrospective study. J Personal Disord 2002; 16:293–303Google Scholar
57. Kazdin AE, Whitley MK: Treatment of parental stress to enhance therapeutic change among children referred for aggressive and antisocial behavior. J Consult Clin Psychol 2003; 71:504–515Google Scholar