Comorbid Dysthymia and Substance Disorder: Treatment History and Cost
Abstract
Objective:The purpose of this study was to determine the treatment history and cost of previous treatment among patients with comorbid substance-related disorder and dysthymia, as compared to patients with substance-related disorder only. Method:Retrospective data were obtained regarding past treatment. Treatment cost was calculated on the basis of the 1996 cost of various treatment modalities. The setting was alcohol-drug programs located within departments of psychiatry in two centers. A total of 642 patients were assessed, of whom 39 had substance-related disorder and dysthymia and 308 had substance-related disorder only (the remaining patients had other comorbid conditions). Data collection instruments included an interview-based questionnaire regarding previous psychiatric and substance abuse treatment. Current cost of treatment in various settings was assessed on the basis of a survey of facilities used by patients in this area.Results:Patients with substance-related disorder and dysthymia had received more substance-related disorder treatment in 18 of 20 measures. Patients with substance-related disorder and dysthymia used 4.7 times more substance-related disorder treatment dollars than patients with substance-related disorder only, although their demographic characteristics were similar. Past self-help activities and pharmacotherapy were remarkably similar for both groups. Although substance-related disorder treatment differed considerably between the two groups of patients, other types of psychiatric treatment (i.e., non-substance-related treatment) did not differ between the two groups.Conclusions:Patients with substance-related disorder and dysthymia are referred to (or seek) substance-related disorder treatment more often than patients with substance-related disorder only but are referred to (or seek) non-substance-related psychiatric treatment no more often than patients with substance-related disorder only. The cost of previous substance-related disorder treatment was several times higher for the patients with substance-related disorder and dysthymia. Am J Psychiatry 1998; 155: 1556-1560
Comorbid substance-related disorder and mood disorder have been well studied, but comorbid substance-related disorder and dysthymia has received little attention (1). In part, this is probably because of the fact that major depressive disorder and mania involve more recognizable symptoms than dysthymia, which can resemble uncomplicated early sobriety (2). In addition, diagnostic criteria for mania and major depressive disorder require sobriety for only 1 and 2 weeks, respectively, whereas symptoms of dysthymia must be present for at least 2 years. Diagnosis of the DSM-IV condition substance-induced mood disorder is also more easily made and requires only 1 month of symptoms. For these reasons, comorbid substance-related disorder and dysthymia is seldom diagnosed and rarely studied.
Despite the apparent rarity of this comorbid condition, we have encountered patients in whom the symptoms of dysthymia had occurred during previous 2-year periods of sobriety or during current periods of abstinence lasting 2 years or more. We also noted that many of these patients would maintain sobriety for several months with considerable support and structured substance-related disorder treatment but would then relapse when their mood symptoms persisted. An important factor in recognizing these cases was our following patients throughout their first year of sobriety. In addition, we invited referrals of atypical patients, thereby encountering cases with greater morbidity or diagnostic complexity.
It was our informal clinical impression that patients with comorbid substance-related disorder and dysthymia had received more non-substance-related psychiatric treatment than patients with substance-related disorder only. We therefore posited that patients with substance-related disorder and dysthymia would resemble patients with substance-related disorder only in regard to substance-related disorder treatment and substance-related self-help activities but that patients with substance-related disorder and dysthymia would differ from patients with substance-related disorder only in having had more non-substance-related psychiatric treatment.
METHOD
Definition of Dysthymia
In keeping with the best estimate procedure recommended by Kosten and Rounsaville (3), we made the diagnosis of dysthymia if one of the following conditions were present: 1) past history of dysthymia over a minimum of 2 years, during which the patient was continuously abstinent, plus dysthymia during the previous 6 months of sobriety; or 2) current history of dysthymia over a minimum of 2 years, during which the patient was continuously abstinent. An exclusion criterion for this study was a current episode of major depressive disorder. We also excluded those with a past history suggestive of dysthymia but with no current symptoms.
None of the patients with substance-related disorder and dysthymia had previously received that diagnosis, although some had been advised that they might be “depressed.” Only two patients diagnosed with dysthymia met the second criterion, i.e., 2 years of continuous abstinence before the current clinical evaluation (a 45-year-old man who had been abstinent for 5 years and a 28-year-old graduate student who had been abstinent for 3 years). All other patients met the first criterion, i.e., 2 years of dysthymia during past abstinence periods plus 6 months of observation by us, during which they continued to manifest dysthymia while abstinent from alcohol and drugs of abuse.
Patients
A total of 642 patients were studied at two alcohol-drug programs located in psychiatry departments at two university settings. Patients with both a substance-related disorder and dysthymia (N=39) and patients with substance-related disorder only (N=308) were selected for the study; patients with other comorbid psychiatric disorders (N=295) were excluded. Upon entry into the alcohol-drug program for assessment, the patients provided written informed consent to the scientific use of these data in an anonymous and confidential fashion.
Data Collection
Trained research associates obtained the following information: 1) treatment history of substance-related disorder: types of treatment, number of previous admissions, and total number of visits or days in treatment; 2) treatment history of non-substance-related psychiatric disorder: types of treatment, number of admissions, and total number of visits or days in treatment; 3) pharmacotherapy with seven medications (two substance-related disorder medications and five psychiatric medications); and 4) self-help activities related to substance-related disorder: changing substance, dose, frequency of use, friends, residency, job/school; and joining a self-help group.
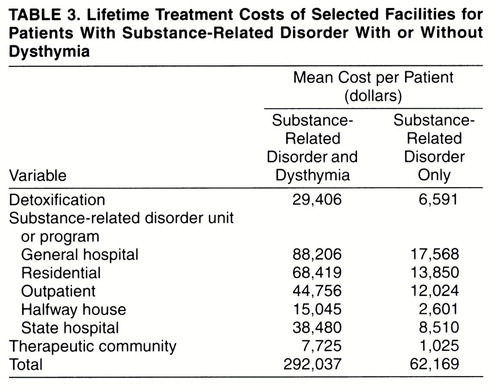
Costs for substance-related disorder treatment were obtained for 1996 by using data from the following sources: 1) detoxification at two private/urban, one public/urban, and one rural facility in Minnesota; mean cost=$570/day; 2) general hospital units for substance-related disorder at two private/urban hospitals; mean cost=$366/day; 3) residential substance-related disorder units at one private/urban, one public/urban, and two out-of-state facilities; mean cost=$277/day; 4) outpatient substance-related disorder programs at three private/urban programs; mean cost=$167/day; 5) halfway house for substance-related disorder at one private/urban program and two public/ urban programs; mean cost=$51/day; 6) state hospital substance-related disorder unit at one state hospital; cost=$185/day; and 7) therapeutic community at two public/urban locations; mean cost=$25/day.
Statistical Analyses
The statistical measures included chi-square analysis with correction for continuity; t test; Fisher’s exact test, two-tailed, for data in which the expected number in any one cell fell below 5; and Mann-Whitney U/Wilcoxon rank sum W test, two-tailed. Level of statistical significance was set at 0.01 in order to reduce the likelihood of false positives, given the number of comparisons.
RESULTS
Demography
Note in table 1 that the group with substance-related disorder and dysthymia showed a greater propensity to be currently living with parents (36% versus 16%) and not living with a spouse (3% versus 17%) versus “other” residence (i.e., living with friends, living alone, living in an institutional setting, homeless). However, the two groups of patients did not differ in five other demographic characteristics (age, gender, education, marital status, and employment).
Category of Substance of Abuse
The patients with substance-related disorder and dysthymia and patients with substance-related disorder only did not differ at statistically significant levels in their axis I abuse or dependence diagnoses for the following substances of abuse: alcohol (74% versus 78%) (χ2=0.12, df=1, p=0.73), opioids (8% versus 21%) (χ2=2.88, df=1, p=0.09), cocaine (8% versus 15%) (χ2=1.05, df=1, p=0.30), amphetamines (8% versus 10%) (χ2=0.06, df=1, p=0.81), sedatives (8% versus 7%) (χ2=0.00, df=1, p=1.00), or hallucinogens (0% versus 3%) (p=0.61, Fisher’s exact test). The two groups did differ significantly with regard to cannabis abuse/dependence, with the patients with substance-related disorder and dysthymia abusing less of this substance (10% versus 38%) (χ2=10.75, df=1, p<0.001).
Type of substance being abused did not affect the treatment and cost data between patients with substance-related disorder and dysthymia and patients with substance-related disorder only.
Substance-Related Treatment History
Data were obtained on history of treatment for substance-related disorder before the current treatment (table 1). Of the 20 variables related to locus of treatment, 17 showed significant differences between the patient groups, with patients with substance-related disorder and dysthymia receiving significantly more care. Those treatments showing significant differences included the following.
1. Greater lifetime history was present for five categories of treatment setting (i.e., detoxification, general hospital substance-related disorder unit, residential substance-related disorder treatment, substance-related disorder halfway house, and substance-related disorder therapeutic community).
2. Number of admissions to the program type in previous lifetime was greater for six treatment settings; only number of detoxification admissions were not significantly different.
3. Total number of days in all seven treatment settings was greater for patients with substance-related disorder and dysthymia.
The average length of stay (i.e., dividing the total number of days by the number of admissions) was shorter for the group with substance-related disorder and dysthymia in five of the six treatment methods (excluding detoxification, which was identical for both groups). However, none of the differences was statistically significant, according to nonparametric testing.
The number of lifetime days per facility was spread over the entire group for purposes of comparison. Although the number of total days is only an average, it does provide another quantitative means of comparing the resources used by both groups, as shown in table 2.
Some patients were in more than one type of program at one time. An example would be attendance at a day program while living in a halfway house. Thus, the total number of days was slightly less than the total number of days spent per patient in treatment. The patients with substance-related disorder and dysthymia had appreciably more treatment days in all seven categories; they had spent about 4.5 years in treatment. The patients with substance-related disorder only had spent an average of 0.9 years in treatment. In sum, the patients with substance-related disorder and dysthymia spent five times as many days in treatment for substance-related disorder as the patients with substance-related disorder only.
We estimated the cost of lifetime treatment by using the daily estimates described in the Method section. Lifetime treatment costs (excluding the current treatment episode) for the entire two groups (i.e., averaged across all patients in both groups) are shown in table 3. The lifetime cost of treatment for substance-related disorder was 4.7 times higher for patients with substance-related disorder and dysthymia than for patients with substance-related disorder only.
Non-Substance-Related Psychiatric Treatment History
Lifetime prevalence of psychiatric treatment not related to substance disorder was assessed for four different treatment settings: i.e., outpatient (including day/evening/weekend programs and outpatient clinics), general hospital, state hospital, and other (e.g., residential, halfway house). There were no significant differences between the two groups of subjects in previous history of admission, number of admissions, and total lifetime number of days in treatment (table 1).
Medication
Two substance-related disorder medications were assessed: disulfiram (5% ever used in substance-related disorder and dysthymia versus 14% in substance-related disorder only) and methadone (3% ever used in substance-related disorder and dysthymia versus 20% in substance-related disorder only). Neither medication showed a significant difference between the two groups. There also was no difference between the groups in lifetime treatment with any of the following five psychotropic medications: antidepressants (46% in substance-related disorder and dysthymia versus 33% in substance-related disorder only), benzodiazepines (44% versus 44%), neuroleptics (28% versus 25%), lithium (18% versus 11%), and anticonvulsants (15% versus 12%).
Substance-Related-Disorder Self-Help Activities
On their own, many patients had attempted to reduce their psychoactive substance use. The two groups did not differ in regard to any of seven self-help activities: i.e., joining a self-help group (62% of 39 patients with substance-related disorder and dysthymia versus 48% of 308 patients with substance-related disorder only), reducing frequency of use (60% versus 58%), reducing dose or amount used per time (59% versus 57%), changing type of psychoactive substance (46% versus 44%), changing friends (37% versus 40%), changing residence (17% versus 31%), and changing job or school (16% versus 17%).
DISCUSSION
Our unpublished data on comorbid substance-related disorder and major depressive disorder and comorbid substance-related disorder and bipolar disorder have shown that these comorbid mood disorders did not produce overutilization of substance-related disorder treatment, although these patients used more non-substance-related psychiatric treatment. Unexpectedly, the group with substance-related disorder and dysthymia showed a propensity to seek out more substance-related disorder treatment settings, to be admitted to those settings more often, and to have more total days in treatment. The pattern resembles “institutionalization on the installment plan” for many patients with substance-related disorder and dysthymia.
Another surprising finding was the large amount of treatment dollars consumed by patients with substance-related disorder and dysthymia—almost five times that of patients with substance-related disorder only. This expense suggests that a modest amount spent on screening for this comorbid condition during the first half-year of care might be a good investment, both from humanitarian and fiscal perspectives. Use of computer assessment offers promise for low-cost screening for comorbid substance-related disorder and other psychiatric disorders (4, 5). Prospective research on this problem is warranted.
Other studies have also shown a strong correlation between depressive symptoms and greater morbidity in patients with substance-related disorder, as compared to patients with substance-related disorder only. For example, Ravndal and Vaglum (6) found that depressive symptoms were associated with higher dropout rates from a therapeutic community. Wolpe and co-workers (7) observed that cocaine abusers with greater depressive symptoms were less compliant with treatment recommendations. In a study of psychiatric patients with mixed diagnoses, Haywood and co-workers (8) noted that alcohol/drug problems were associated with a higher frequency of hospitalization among several diagnostic groups, including those with affective problems. Gogek (9) has proposed that continued minor depressive symptoms might contribute to the “dry drunk” syndrome—i.e., the patient’s unwillingness (or inability) to “work the [recovery] program.”
Contrary to our predictions, the patients with substance-related disorder and dysthymia did not seek out or receive non-substance-related psychiatric treatment to a greater extent than the patients with substance-related disorder only. None of our 39 patients with substance-related disorder and dysthymia had even been told they had dysthymia; this could account for the relatively low rate of non-substance-related psychiatric care. Lack of benefit from non-substance-related psychiatric treatment could be a reason for their seeking out substance-related disorder treatment—which, despite its long-term failure, at least provided temporary relief of acute problems associated with substance-related disorder. Another cause for non-substance-related psychiatric treatment failure may be the absence of diagnostic efforts to detect substance-related disorder problems in many psychiatric settings—a well-described problem (10).
Physicians did not prescribe medications more frequently for patients with substance-related disorder and dysthymia. Use of substance-related disorder self-help activities was similar in both groups. Our patients with substance-related disorder and dysthymia joined self-help groups about as often as 87 “dual disorder” patients studied by Ries and co-workers (11). In sum, these patients with substance-related disorder and dysthymia were not averse to these modalities but also did not appear to derive much benefit from them.
Received May 6, 1996; revisions received Oct. 2, 1997, and March 6 and April 21, 1998; accepted May 15, 1998. From the Minneapolis VA Medical Center and the Department of Psychiatry, University of Minnesota, Minneapolis. Address reprint requests to Dr. Westermeyer, Minneapolis VA Medical Center, University of Minnesota, 1 Veterans Dr., Minneapolis, MN 55417. Supported in part by the Laureate Foundation of Tulsa.Dr. James Halikas, Mr. John Neider, and Mr. Greg Carlson collaborated in the collection of these data.
 |
 |
 |
1. Kell MJ: Opiate dependence, comorbidity and seasonality of birth. J Addict Disord 1995; 14:19–34Crossref, Medline, Google Scholar
2. Powell BJ, Penick EC, Nickel EJ, Liskow BI, Riesenmy KD, Campion SL, Brown SF: Outcomes of co-morbid alcohol men: a 1-year follow-up. Alcohol Clin Exp Res 1992; 16:131–138Crossref, Medline, Google Scholar
3. Kosten TA, Rounsaville BJ: Sensitivity of psychiatric diagnosis based on the best estimate procedure. Am J Psychiatry 1992; 149:1225–1227Link, Google Scholar
4. Rost K, Burnam MA, Smith GR: Development of screeners for depressive disorders and substance disorder history. Med Care 1993; 31:189–200Crossref, Medline, Google Scholar
5. Schrader G: Chronic depression: state or trait? J Nerv Ment Dis 1994; 182:552–555Google Scholar
6. Ravndal E, Vaglum P: Self-reported depression as a predictor of dropout in a hierarchical therapeutic community. J Subst Abuse Treat 1994; 11:471–479Crossref, Medline, Google Scholar
7. Wolpe PR, Gorton G, Serota R, Sanford B: Predicting compliance of dual diagnosis inpatients with aftercare treatment. Hosp Community Psychiatry 1993; 44:45–49Abstract, Google Scholar
8. Haywood TW, Kravitz HM, Grossman LS, Cavanaugh JL Jr, Davis JM, Lewis DA: Predicting the “revolving door” phenomenon among patients with schizophrenic, schizoaffective, and affective disorders. Am J Psychiatry 1995; 152:856–861Link, Google Scholar
9. Gogek EB: The dry drunk syndrome: subtype of depression? (letter). Am J Psychiatry 1994; 151:947–948Medline, Google Scholar
10. Milling RN, Faulkner LR, Craig JM: Problems in the recognition and treatment of patients with dual diagnoses. J Subst Abuse Treat 1994; 11:267–271Crossref, Medline, Google Scholar
11. Ries R, Mullin M, Cox G: Symptom severity and utilization of treatment resources among dually diagnosed inpatients. Hosp Community Psychiatry 1994; 45:562–568Abstract, Google Scholar



