Three-Year Trials of Personal Therapy Among Schizophrenic Patients Living With or Independent of Family, II: Effects on Adjustment of Patients
Abstract
OBJECTIVE: Previous analyses of the personal and social adjustment of outpatients with schizophrenia have either relied on the assessment of unrepresentative patients who survived without relapse or used analyses that included relapse assessments, a potential confound when different rates of relapse existed among treatment conditions. The authors' goal was to conduct a study of the effects of personal therapy on outcome that was designed to take into consideration the effects of relapse. METHOD: They evaluated the effectiveness of personal therapy over 3 years after hospital discharge among 151 patients with schizophrenia or schizoaffective disorder. The patients were randomly assigned to receive personal therapy or contrasting therapies in one of two concurrent trials. One trial included patients who were living with family (N=97); the other included patients who were living independent of family (N=54). Patients were assessed at 6-month intervals over 3 years of treatment on measures of personal and social adjustment; patients who relapsed and restabilized and those who did not relapse were included. RESULTS: Personal therapy had positive effects on broad components of social adjustment (role performance) but had few differential effects on symptoms, and patients receiving personal therapy remained more anxious than patients who received family or supportive therapy. For patients who were living with family, personal therapy led to better outcomes in overall performance than did the other treatments. Although family therapy had only one positive effect on patients' social adjustment, the personal adjustment (residual symptoms) of patients who received family therapy appeared to improve more than that of patients receiving personal or supportive therapy. For patients not living with family, personal therapy was more successful than supportive therapy in improving work performance and relationships out of the home. Longitudinal effects of personal therapy on symptoms were similar to those of family and supportive therapies, particularly in the first 2 years, but personal therapy effect sizes increased over time on measures of social adjustment. CONCLUSIONS: Personal therapy has pervasive effects on the social adjustment of patients with schizophrenia that are independent of relapse prevention. Supportive therapy, with or without family intervention, produces adjustment effects that peak at 12 months after discharge and plateau thereafter. However, personal therapy, a definitive psychosocial intervention, continues to improve the social adjustment of patients in the second and third years after discharge. Brief treatment would appear to be less effective than a long-term, disorder-relevant intervention for schizophrenia. (Am J Psychiatry 1997; 154:1514–1524)
The addition of psychosocial treatment to maintenance antipsychotic drug therapy has frequently reduced the risk of schizophrenic relapse (e.g., references 1–6), but it remains unclear whether there are pervasive effects of psychosocial treatment on the personal and social adjustment of patients that are independent of this strong prophylactic effect (7).
Reports on “adjustment” often reflect clinical status (8), most often symptom improvement among hospitalized inpatients; extensive studies of the effects of social skills training and cognitive remediation provide characteristic examples (9–11). Many long-term maintenance outpatient studies that enrolled patients with schizophrenia immediately following an index hospital discharge (of which our own past efforts [1–3, 7, 12] are representative), systematically removed patients from study when they experienced their first severe psychotic exacerbation. Therefore, subsequent attempts to detect treatment effects on adjustment often evolved to the analyses of periodic status reports of patients who survived without an interim relapse (2, 7, 12). In the face of differential relapse rates by treatment, such “survivor” analyses would, by definition, include subjects who were not representative of the original study group. The statistical power needed to reliably detect treatment effects would be decreased accordingly. The alternative for investigators has been to perform analyses in which the adjustment ratings of relapsed patients are combined with the assessments of nonrelapsed subjects. Since relapse assessments invariably reflect more severe dysfunction, these analyses might become redundant (confounded) statements of the earlier prophylactic effect if there were significant differences in relapse rates between experimental and control conditions (7).
One suggested solution to this impasse is to recruit patients who are at minimal risk for decompensation (13); this is a tenuous solution at best given the imprecision of predictors. The solution applied by Schooler et al. in the National Institute of Mental Health (NIMH) Treatment Strategies in Schizophrenia Study (14) was to reenter relapsed subjects into the initial, randomized treatment condition when these subjects recovered. The rationale for this solution was that even though differential relapse rates might accumulate by treatment condition over the years of study, the absolute number of relapsed patients at any interval assessment would, a priori, be smaller than the cumulative total, would exclude between-interval relapses, and would thus be minimally different between treatment conditions. To attempt the most definitive test possible concerning the independent effects of psychosocial treatment on patient adjustment, we also chose to reenter relapsed patients into their original treatment condition on recovery.
METHOD
Design
The design of the personal therapy studies is described in part I of this study (in this issue of the Journal). The design involved the random assignment of 97 newly discharged patients with schizophrenia who lived with family to personal therapy, family psychoeducation/management (family therapy), a combination of personal therapy and family psychoeducation/management (combination personal and family therapy), or supportive therapy (trial 1). Fifty-four patients who lived independent of family were randomly assigned to either supportive or personal therapy (trial 2). All patients were maintained on the minimum effective dose of antipsychotic medication. The resources of an NIMH MERIT award provided the unique opportunity to extend the assessment of adjustment through a third year of controlled treatment. All patients provided informed, signed consent after the benefits and risks had been fully explained.
Assessments
Table 1 lists the clinician, patient, and family rating instruments and their component subscales that were used to assess social adjustment (role performance), personal adjustment (symptoms), and family ratings among patients who participated in both trials. These assessments were completed at baseline and again at 6-month intervals over the 3 years of study. All measures of social adjustment were derived from standard scales and included the Global Assessment Scale (GAS) single score (15), the seven global judgments from the Major Role Adjustment Inventory (12), and the six global judgments and four factor scores from the Social Adjustment Scale II (16). The Social Adjustment Scale II was the primary measure of social adjustment used to predict differential treatment effects. Unlike the other clinician assessments, which were based on a focused interview and observation, the Social Adjustment Scale II was completed following a structured interview with the patient and thus more closely represented the patients' own reports of the quality and quantity of instrumental and expressive role performance in the preceding 2 months.
Standard measures of personal adjustment provided by the treating clinicians included eight measures derived from the Brief Psychiatric Rating Scale (BPRS) (17) as well as the total score on the Raskin Depression Scale (18), the Covi Anxiety Scale (19), and the Wing Negative Symptom Scale (20). Two patient self-reports of personal adjustment included the six factors from the Subjective Response Questionnaire (21) and five measures from a new instrument called the Everyday Worries Scale. The latter scale contained four factors and one intuitively constructed cluster that represented the most frequently endorsed patient worries. The factors were derived from a principal components analysis, with rotation, of 700 ratings obtained during the study. Loadings ranged from 0.35 to 0.65 across the 10 to 13 items contained in each factor.
The principal family ratings were derived from a standard scale that represented a relative's assessment of the patient's adjustment in trial 1—the Katz Adjustment Scale form R2, which rated the patient's performance of expected social roles (22)—and a discrepancy score calculated as the difference between observed and expected role performance according to Katz scale scores. Another 16 family variables represented experimental measures designed for this study that were found not to yield consistent treatment effects in trial 1; these variables were excluded from further consideration. Although all treatments were patient centered, nearly all family variables represented attempts to detect indirect effects of treatment on family functioning and attitudes. The absence of consistent effects could have reflected the inability of treatment effects to generalize to family functioning, the questionable reliability and validity of these new measures, or both.
Finally, at the termination of the study, patients rated their levels of satisfaction with their respective treatment experiences.
Additional assessments were made either once, semiannually, annually, or monthly during the study. These assessments are more properly viewed as independent variables than as outcome measures and, therefore, are not included in the adjustment analyses. These ratings represented components of the treatment process (attempts to identify variables that might ultimately explain the relapse and adjustment outcomes) and included the practice principles applied and goals achieved; the patient's personality, intelligence, and locus of control; retrospective evaluations of developmental experiences; and a brief schedule of community stressors unique to patients who lived independent of family. These assessments will be the subject of a future, detailed analysis of the treatment process.
Ninety-seven percent of the clinician assessments of patients' adjustment were obtained while patients remained in the study, before early termination or successful completion of the protocol; approximately 86% of the patient assessments and 90% of the family assessments were also obtained while patients remained in the study. The number of patients available for the adjustment analyses that were common to both trials ranged from 150 patients at 6 months to 124 patients at 36 months for clinician ratings and from 131 to 111 patients for patient ratings. Since missing data were relatively few and not different among treatment conditions, only the data collected were analyzed. Among these completed assessments, only 11% of clinician ratings and 7% of patient ratings represented the assessment of subjects who were experiencing a recurrent schizophrenic episode (relapse) at the time of assessment, and there were no significant differences among treatment conditions at any rating period. The small number and equal distribution of relapse assessments among treatment conditions at each rating period ensures that the adjustment effects being measured were not redundant measures of the differential relapse rates reported in part I of this study (in this issue of the Journal).
Ongoing reliability checks were not made of the raters because of their cost, but the clinical raters had been trained and had a great deal of experience in the use of these standard scales. Attempts to further enhance reliability were undertaken through the process of random assignment, the consistency of the same clinical rater across periods for 140 of the 151 patients, and statistical attempts to develop more reliable measures such as the construction of composite indexes.
Composite Indexes
Faced with numerous, often intercorrelated, yet imperfect measures of personal and social adjustment, we sought a more reliable and hence more powerful test of these dimensions. The availability of a multivariately derived composite measure for each dimension of personal and social adjustment not only would aid in the understanding and interpretation of treatment effects but also would guard against the probability of inflating type I errors (overestimating positive effects), which often follow univariate testing of individual scale outcomes. The availability of such a composite measure would also militate against the need for Bonferroni correction of the univariate tests that could exaggerate type II errors (underestimating positive effects), a questionable approach to the initial test of a new treatment. A composite that was shown to be comprehensive, broad, and statistically different between the treatment conditions would lend legitimacy to the examination of the effects of the individual component measures and allow us to place greater confidence in the interpretation of these univariate tests as well. A composite that was shown to be narrowly defined yet significantly different between treatments would mean that there would be less need to examine the individual component measures.
From the 42 outcome variables shown in table 1, 27 were selected for a factor analysis that broadly reflected the dimensions of interest from the perspectives of clinician, patient, and family raters. Given the number of variables entered, factor analysis at a single time period did not contain a sufficient number of cases for reliable factoring. Because it was inappropriate to pool data from the same patients at several (seven) time periods, correlations were computed for each period and then averaged as the basis for factoring. Global and total scores were most often selected for this factor analysis rather than the factor scores that were embodied in the global measures.
An analysis of principal factors yielded two composites that clearly reflected the personal and social adjustment dimensions. The first was a broadly defined social adjustment composite comprising 11 variables that were largely drawn from the Major Role Adjustment Inventory, Social Adjustment Scale II global scores, and the GAS; the factor loadings ranged from 0.54 to 0.84 (table 1). (Although the global illness measure on the BPRS intuitively seemed to be a measure of personal adjustment and is listed under personal adjustment in table 1, it loaded highly on the social adjustment composite and was scored accordingly.)
The second factor represented a more narrowly defined personal adjustment composite comprising five variables with loadings from 0.36 to 0.51. This factor included the BPRS minor (affective) symptoms, factors from the patient's Subjective Response Questionnaire (sluggishness and dysthymia), and total scores on the Covi Anxiety Scale and the Raskin Depression Scale. Other Subjective Response Questionnaire factors also loaded on this composite but were not included because of unwanted redundancy and oversampling of the scale.
The family rating of the patient's performance of expected social roles (Katz Adjustment Scale form R2), while split loading on the social adjustment composite, was also identified as a separate dimension of singular importance in the interpretation of patient role performance from the perspective of family members. (The discrepancy measure was excluded because of its high correlation with the Katz Adjustment Scale R2 score.) The decision to test the Katz Adjustment Scale R2 score itself rather than include it in the social adjustment composite was influenced by the fact that its absence in trial 2 (and therefore in the combined trials analyses) would render comparisons of the composite across trials more equivocal.
Analyses
Cross-sectional analysis. Following a traditional approach (23, 24), we used regression analyses to perform the repeated analyses of covariance on the dependent variables that were assessed at each semiannual period over the 3 years of treatment. The initial assessment of a variable (most often an intake evaluation) served as the covariate for each of the semiannual analyses of the variable. Given the random assignment design, this approach was chosen not only as a way to adjust posttreatment means for random initial differences but also as a way to control for the influence of other independent variables on outcome and to reduce error variance. Performing a general linear model of analysis, with covariates, by way of regression allowed precise control of the order in which we evaluated effects: first the main effects of treatment, controlling for the initial level covariate, followed by the test of a possible interaction between personal or family therapy and the dichotomized independent variables of gender, age (≤30 or >30), race (Caucasian or African American), chronicity (age ≤23 or >23 at first psychosis), and, in trial 1, a rating of household expressed emotion (high or low). Controlling for main effects, we considered only the simple interaction between a treatment condition and an independent variable and ignored the effects of higher-order interactions because of the ambiguity associated with their interpretation.
The significant treatment effects presented in tables 2–4 represent the results of t tests on the treatment-respective regression coefficients; these tests controlled for the effects of all independent variables in the analyses of the combined trials and the trial involving patients living with family. Given the smaller number of subjects and a reduced probability of achieving orthogonality for the independent variables, only the initial level covariate was controlled in the analyses for the patients living independent of family. The corresponding effect sizes (i.e., the clinically meaningful differences between the adjusted posttreatment means) were calculated as Cohen's d from the regression t tests (25) and expressed in standard deviation units.
Evidence that personal therapy produced an effect on the social adjustment composite factor in the combined trials analysis, and that family therapy had a positive effect on the personal adjustment composite factor (trial 1), provided justification for univariate testing of each outcome variable listed in table 1 at each semiannual period. However, as a further guide against the possibility of type I error, only those effects which satisfied our definition of a pattern are listed in tables 2–4. We defined a significant pattern for an outcome variable as p≤0.04 for the regression t test at two or more periods in the combined trials analysis or p≤0.06 at two or more periods in the linear regression analyses of separate trials, where the numbers of subjects were smaller. (Data in tables 2–4 indicate the presence of an additional nonsignificant indication in the same direction at other periods.) A seventh rating period represents the combined (average score) regression t test for a variable across the six semiannual assessments, i.e., the rating for all months in tables 2–4.
This alternative to multivariate testing (such as a repeated measures analysis of variance) was chosen because there were missing data, which might violate the assumptions of typical multivariate approaches. Since the significant effects of univariate testing numbered in the hundreds, we believe that the pattern definitions derived from an examination of the results are the most conservative yet accurate summations of the robust and consistent main effects of treatment.
The reader should keep in mind the order of testing because it was intended not only to guide inference making but also to minimize the chance for error associated with the large number of outcome measures (N=40 to N=44), rating periods (N=7), trials (two individual and one combined), and, therefore, the number of tests performed (N=868). The primary test was whether a significant treatment effect was observed on one or both multivariately derived composite indexes or the Katz Adjustment Scale R2 score. If so, the second test sought confirmation of a significant overall effect (another multivariate approach) on each component outcome measure associated with the significant composite effect. Finally, the individual (univariate) tests of the component outcome measures would need to meet criteria for significance at multiple time periods, i.e., would satisfy the definition of a pattern. Greater confidence in results would follow affirmation of all three tests. A note of caution in the interpretation of results will be offered whenever the three conditions are not met.
Longitudinal analyses. Independent of whether a variable was shown in the linear regression analysis to be statistically significant at one or more rating period, each outcome measure common to both trials was identified that showed a clinically meaningful change (i.e., an effect size of 0.50 standard deviation or greater) between clinic intake (baseline) and 36 months for either or both of the three combined personal therapy conditions (N=74) or the three no-personal-therapy conditions (N=77). For example, the GAS was included because there was a 1.15-standard-deviation change for the personal therapy condition and a 1.06-standard-deviation change for the no-personal-therapy condition over the 3 years, even though there were no significant differences between treatments at any of the individual rating periods. An improvement of 0.50 standard deviation on an outcome measure has long been accepted as clinically and statistically meaningful (26). This analysis was designed to illustrate both the magnitude and the temporal course of symptomatic improvement and social recovery.
RESULTS
Treatment Main Effects
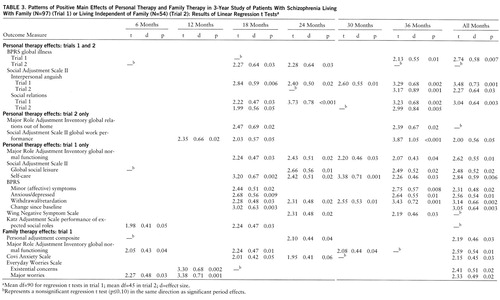
From tables 2 and 3 it is clear that most of the important main effects occurred in the second and third years of treatment rather than in the first year. Regarding positive personal therapy effects that were derived from the combined trials regression analyses (i.e., variables that showed the patients in the three personal therapy conditions to be more improved than patients in the three no-personal-therapy conditions), a significant effect on the social adjustment composite was reflected in the extensive effect patterns across outcome measures that were associated with this variable (table 2). The significant univariate patterns included the normalization of functioning in expressive (relationship) and instrumental (activity) roles, decreasing levels of manifest illness, and the resolution of negative symptoms. Further, all but two of these patterns were protected by a significant overall effect. However, the significant univariate patterns associated with the two measures of negative symptoms should be viewed cautiously because personal therapy had no effect on the personal adjustment composite.
Three of the combined trial effects of personal therapy were still associated with social adjustment when applied to each trial individually (table 3). In order of magnitude, the first represented significantly less impairment on the Social Adjustment Scale II factor of interpersonal anguish. This important dimension reflected less impairment among personal therapy recipients regarding the aspects of friction and distress experienced in their primary work role (as wage earner, homemaker, or student), worry, guilt, and feelings of being wronged within the family household (for patients living with family) or extended family, as well as sensitivity in relationships, loneliness, and self-appraisal. The effect of personal therapy on the Social Adjustment Scale II factor of social relations was also significant; indicating improvement in leisure activities as well as the depth of activities and frequency of contact, together with a reduction in conflict, communication difficulties, and friction in these social contexts. A decrease in BPRS global illness over time represents the remaining personal therapy effect that was common to both trials.
Regarding patients who lived independent of family (trial 2), global judgments of enhanced work performance as well as the quality of relationships outside the home were specific effects for these patients. By contrast, the effects of personal therapy among patients who lived with family (trial 1) were more frequent yet specific for activities other than work performance. These included improved global functioning and change over time as well as the enhancement of leisure activities and self-care. Most reassuring was the independent family rating of improved role performance among personal therapy recipients (Katz Adjustment Scale R2 score). The reduction in negative symptoms, minor symptoms, and anxious depression, however, must again be viewed cautiously in the absence of a personal therapy effect on the personal adjustment composite.
There are selected effects, independent of those found in the combined trials or in trial 2, that were reserved for trial 1 participants in the family therapy condition. These effects are shown in table 3. Primarily, there was significant improvement in the personal adjustment composite among family therapy recipients, which is supported by the overall and pattern effects associated with less observed anxiety (Covi Anxiety Scale) and self-reported worries (Everyday Worries Scale). The one positive effect of family therapy on social adjustment (global normal functioning) should be viewed cautiously because family therapy had no effect on the social adjustment composite.
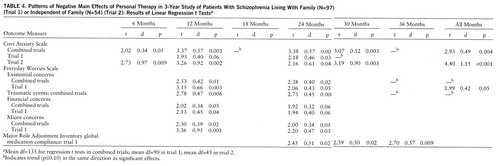
Unfortunately, personal therapy was not without negative effects, as shown in table 4. Family therapy improved the personal adjustment composite (including observed and self-reported anxiety), but anxiety as reported by clinicians (COVI Anxiety Scale) and by patients (Everyday Worries Scale) remained significantly higher and persistent across rating periods among personal therapy recipients than among patients who did not receive personal therapy. Although medication noncompliance was infrequent overall, late-occurring problems in the regularity of medication taking among personal therapy recipients who were living with family suggests denial of the need for continuing medication among patients who increasingly feel better and recover role functions (7).
Regarding negative effects of family therapy, a consistent but often nonsignificant negative effect of family therapy on the independent family rating (not shown in table 4) is worthy of comment, not only because of an absence of positive effects of family therapy on social adjustment but also because the Katz Adjustment Scale R2 score was itself a one-item composite. Family members in trial 1 reported significantly enhanced role performance among personal therapy recipients, but family members of patients in family therapy consistently reported more underperformance of expected roles among patients than did family members of patients not in family therapy. Nonsignificant indicators of lower performance among family therapy patients (p≤0.10) occurred at four rating periods, and a negative effect was significant at 24 months (t=2.15, df=85, p=0.04) in the analyses that controlled for the initial level covariate. This observation also appears to support the absence of positive effects of family therapy on social adjustment according to the role performance ratings provided by clinicians and patients.
Finally, although treatment main effects occurred for the two composite indexes and 21 of the individual outcome measures, effects were not detected on more than 400 tests of the remaining 21 dependent variables in these cross-sectional analyses. Most noteworthy was the absence of a differential treatment effect pattern on measures of positive psychotic symptoms, patient reports of subjective well-being, quality of relationships in the home, and selected measures of global adjustment (GAS) and depression (Raskin Depression Scale). However, as indicated in the longitudinal analysis described later in this paper, patients often improved on these measures over time, independent of treatment condition.
Summary of Treatment Interactive Effects
Our sole interest in the effects of gender, race, age, chronicity, and expressed emotion (in trial 1) was limited to determining whether the significant treatment main effect patterns shown in tables 2 through 4 could be explained by the presence of potentially confounding variables. We found none. We shall only summarize the nature and scope of the more important interactions that occurred at three or more periods when the regression t test p values were ≤0.05, provided that the direction of the interactive effect was consistent. Again, any indication that personal therapy improved symptoms or that family therapy improved social adjustment must be viewed very cautiously.
Only six interactions met criteria in the combined trials analyses, and these indicated significantly greater improvement among men who received personal therapy than among men who did not receive personal therapy on the social adjustment composite, minor symptoms, anxious depression, and overall change variables. Nonwhite personal therapy recipients worked more hours each week than nonwhite patients who did not receive personal therapy, and social leisure activity improved more for white personal therapy recipients than for white patients who did not receive personal therapy. For patients who were living independent of family, only four interactions met criteria: nonwhite patients who received personal therapy had improved relationships with their external family but were more withdrawn and dysthymic than nonwhite patients who did not receive personal therapy. Most interactions that met criteria were found among the patients living with family: 19 interactions involving personal therapy and 11 involving family therapy met criteria. The most robust of the interactions involving personal therapy represented improved role performance of male patients, less depression among young patients, and enhanced normative function for nonwhite patients who received personal therapy compared with male patients, young patients, and nonwhite patients, respectively, who did not receive personal therapy.
Regarding family therapy, improvement on the personal adjustment composite found in this treatment condition was more pronounced among female patients than among male patients, as measured by a variety of affective symptom measures. However, young patients who did not receive family therapy had greater improvement in work performance according to clinicians and family members than did young patients who did receive family therapy, a likely explanation of the consistent negative indication noted on the Katz Adjustment Scale rating of the patient's performance of expected social roles. Patients receiving personal therapy alone improved more on global assessments of major role performance than did patients in the personal therapy plus family therapy condition.
Regarding expressed emotion, aspects of personal and social adjustment improved more among personal therapy recipients who lived in households with low ratings for expressed emotion than among personal therapy recipients who lived in households with high ratings for expressed emotion. However, in households with high ratings for expressed emotion, relatives of patients who received family therapy expressed more positive comments than did relatives of patients who did not receive family therapy, while in households with low ratings for expressed emotion, relatives of patients who received family therapy expressed fewer positive comments than did relatives of patients who did not receive family therapy.
Longitudinal Effects
Table 5 illustrates the pattern of change for the symptom measures that satisfied criteria for a change of 0.50 standard deviation or more between baseline and 36 months. In the first year, symptom measures in both treatment conditions (personal therapy versus no personal therapy) improved dramatically and identically as patients likely continued the resolution of their index psychotic episode. Slight but continuing symptom improvement again characterized both treatment conditions in year 2. These observations tend to underscore the relative absence of an additive psychosocial treatment effect on symptom measures at 1 and 2 years as reported in the cross-sectional analyses of previous outpatient studies (2, 7, 12), when experimental and control subjects were maintained on antipsychotic medication. It is primarily in the third treatment year that a meaningful difference emerged as improvement in residual symptoms selectively continued in the personal therapy condition.
These observations are more dramatically illustrated in the data reported for the measures of improvement in adjustment in table 5, outcomes for which a psychosocial treatment effect would likely be expected. Again, patients who received personal therapy and those who did not improved in the first year, and the magnitude of the difference between the patients was not significant (tables 2 and 3), consistent with findings of past studies of psychosocial treatment (2, 7, 12). However, by years 2 and 3, incremental and clinically meaningful improvements in adjustment accrued to patients who received personal therapy, but patients who did not receive personal therapy clearly reached a plateau, an outcome that is also reflected in the cross-sectional analyses.
Patient Satisfaction
Personal therapy was preferentially endorsed by patients, not only in terms of the exceptional compliance reported in part I of this study (in this issue of the Journal) but also in ratings of perceived value. Only 16% of all study subjects found their treatment assignment to be of little or no help (most of these patients were in the supportive therapy conditions). Sixty-seven percent (N=32) of the patients who received personal therapy alone found the treatment to be very helpful, compared with 51% (N=27) of the patients who received supportive therapy and 37% (N=18) of the patients who received family therapy (χ2=8.70, df=2, p=0.01).
DISCUSSION
Conclusions
We conclude that personal therapy improves broad areas of social adjustment that are independent of relapse. For patients who live independent of family, effects are more specific to the enhancement of work performance and relationships with external family. For patients who live with family, effects are specific to improved intrapersonal competence and interpersonal effectiveness and an inclination toward fewer negative symptoms and withdrawal. As is likely true of nonpatients, the greater role performance of personal therapy recipients occurred in the context of a clinically observed and self-reported anxiety that was, perhaps, indicative of more active involvement in life rather than a psychiatric disorder. Conversely, family therapy recipients (particularly women) were more personally comfortable than personal therapy and supportive therapy patients, a clinical state that might accrue to those who are less engaged in the performance of appropriate social roles.
It also appears that only modest improvement in social adjustment accrued over time to patients who did not receive personal therapy and that this improvement was limited to the first 12 months of treatment. For personal therapy patients, however, social adjustment not only increased incrementally with time but did not seem to reach a plateau at 36 months. It is possible that these patients would have continued to experience improvement in social adjustment if their treatment exposure had not been limited to the period of research support. While encouraging, these observations might constitute a dilemma (8) for the proponents of either the managed care or brief treatment of chronically and severely mentally ill individuals. Many public and private insurers reimburse only a limited number of yearly sessions for medication management and nonspecific support for maintenance schizophrenia treatment. The dramatic gains in symptom remission associated with medication and support in the first 2 years after discharge could justify a claim of cost-effective treatment. However, this justification does not acknowledge the unrealized potential for continued recovery of social functions, although the requisite psychosocial treatment would be long-term and undoubtedly more costly than supportive therapy.
Part I of our study (in this issue of the Journal) revealed that personal therapy provoked relapse among some patients living in unstable residences independent of family, but it also showed that personal therapy clearly improved the adjustment of these older and more persistently ill patients. However, there were fewer effects of personal therapy on patients who were living independent of family than on patients who were living with family. Clinicians felt that the absence of greater effects for the patients not living with family might have been related to the fact that clinicians had to spend a portion of therapy hours securing the resources needed to sustain the day-to-day existence, a testimonial to the services provided by the families of patients with schizophrenia.
The patients' endorsement of personal therapy as being more helpful than family therapy could contain important clinical implications. Family therapy approaches are often justifiably valued by families (27), but it is possible that compulsory participation in family therapy might be less enthusiastically valued by the adult patient with schizophrenia than a personalized, individual therapy.
Finally, our findings regarding the effects of personal therapy are particularly encouraging in view of the fact that study clinicians were faced with the challenge of stabilizing partially remitted patients who were discharged following hospitalizations measured in days or weeks rather than the months that characterized hospitalizations of patients in earlier studies.
Qualifications
Potential policy implications of these findings need to be tempered by the constraints imposed by controlled clinical trials. First, independent replication is clearly indicated, a distinct challenge in the light of the limited resources available for the conduct of expensive, controlled, and sufficiently large psychosocial clinical trials. Second, the application of personal therapy was provided by experienced, credentialed, and well-trained clinicians whose full-time caseloads did not exceed 30 patients. Third, a cost-benefit analysis was precluded because much of the budget was committed to research functions. However, with a treatment-resistant disorder such as schizophrenia, the investigative challenge is first to determine whether any treatment initiative, provided under optimal conditions, can improve the outcome of schizophrenia beyond what is possible with existing interventions. Whether equivalent gains for personal therapy are possible with more inclusive patient samples, less trained providers, larger caseloads, or less frequent patient contact are appropriate questions reserved to a second generation of studies. Fourth, the adjustment gains observed most often resulted from the ratings of treating clinicians who were not blind to the treatment conditions, thereby raising the question of rater bias. However, since patients were admitted sequentially to the study over a period of 5 years (i.e., at any given time study patients were at different rating periods), it would be difficult to accept that there was a systematic bias for effects that were otherwise consistent by selective periods, multiple raters, treatment conditions, patient characteristics, trials, directions (both positive and negative), and, at times, observers (patient, family, and clinician). Nonetheless, results should be viewed cautiously in the absence of independent and blind clinical assessors.
Finally, we conclude with the caveat that although relative gains in adjustment were clearly achieved, in absolute terms most recipients of personal therapy were still recovering from a severe mental disorder. For example, on the 100-point GAS, the mean score of personal therapy recipients changed from 47 (SD=13) at baseline (indicating serious symptoms or impairment in functioning), to 64 (SD=14) at year 3 (indicating mild symptoms or some difficulty in several areas of functioning, although the patient would not appear sick to the untrained observer). Similarly, on a 7-point global measure of major role performance (as a wage earner, homemaker, or student), improvement increased from a mean score of 6.2 (SD=0.98) at baseline (6=moderately below best previous performance) to 4.8 (SD=1.78) at year 3 (5=slightly below best previous performance). These clinically meaningful but relative improvements would not qualify as optimal recovery from schizophrenia. Our speculation on the potential constraints against a more complete recovery followed case debriefings after the study. These obstacles included persistent residual symptoms that precluded participation in the advanced phase of personal therapy (28) for more than 40% of the patients (part I of the study in this issue of the Journal). They also implied pervasive disabilities in social cognition that often seemed to conspire against a more complete clinical and social recovery. The latter appear to include failures in taking a second-person perspective (29) and difficulties in reading the informal, abstract rules of conduct that often characterize the unpredictable changes found in diverse or novel social contexts (30, 31). Future psychosocial treatment initiatives might be profitably directed to these possible rate-limiting factors.
 |
 |
 |
 |
 |
Received Jan. 31, 1996; revisions received Dec. 18, 1996, and Feb. 26 and May 30, 1997; accepted June 2, 1997. From the Department of Psychiatry, University of Pittsburgh School of Medicine. Address reprint requests to Professor Hogarty, Western Psychiatric Institute and Clinic, 3811 O'Hara St., Pittsburgh, PA 15213. Supported by a MERIT extension of NIMH grant MH-30750. The authors thank G. Alexander, M.D., P. Bartone, M.S.N., A. Garrett, Ph.D., K. Hammill, M.S.N., H. Levin, M.D., D. Reiss, Ph.D., and E. Venditti, Ph.D., for their assistance in conducting the studies.
1. Hogarty GE, Goldberg SC, Schooler NR, Ulrich RF: Drug and sociotherapy in the aftercare of schizophrenic patients, II: two-year relapse rates. Arch Gen Psychiatry 1974; 31:603–608Crossref, Medline, Google Scholar
2. Hogarty GE, Schooler NR, Ulrich RF, Mussare F, Herron E, Ferro P: Fluphenazine and social therapy in the aftercare of schizophrenic patients: relapse analyses of a two-year controlled study of fluphenazine decanoate and fluphenazine hydrochloride. Arch Gen Psychiatry 1979; 36:1283–1294Google Scholar
3. Hogarty GE, Anderson CM, Reiss DJ, Kornblith SJ, Greenwald DP, Javna CD, Madonia MJ: Family psychoeducation, social skills training, and maintenance chemotherapy in the aftercare treatment of schizophrenia, I: one-year effects of a controlled study on relapse and expressed emotion. Arch Gen Psychiatry 1986; 43:633–642Crossref, Medline, Google Scholar
4. Leff J, Kuipers L, Berkowitz R, Sturgeon D: A controlled trial of social intervention in the families of schizophrenic patients: two-year follow-up. Br J Psychiatry 1985; 146:594–600Crossref, Medline, Google Scholar
5. Falloon IRH, Boyd JL, McGill CW, Williamson W, Razoni J, Moss HB, Gilderman AM, Simpson GM: Family management in the prevention of morbidity of schizophrenia. Arch Gen Psychiatry 1985; 42:887–896Crossref, Medline, Google Scholar
6. Tarrier N, Barrowclough C, Vaughn C, Bamrak JS, Porceddu K, Watts S, Freeman H: Community management of schizophrenia: a two-year follow-up of a behavioural intervention with families. Br J Psychiatry 1989; 154:625–628Crossref, Medline, Google Scholar
7. Hogarty GE, Anderson CM, Reiss DJ, Kornblith SJ, Greenwald DP, Ulrich RF, Carter M: Family psychoeducation, social skills training, and maintenance chemotherapy in the aftercare treatment of schizophrenia, II: two-year effects of a controlled study on relapse and adjustment. Arch Gen Psychiatry 1991; 48:340–347Crossref, Medline, Google Scholar
8. Lehman AF, Carpenter WT, Goldman H, Steinwachs DM: Treatment outcomes in schizophrenia: implications for practice, policy, and research. Schizophr Bull 1995; 21:669–675Crossref, Medline, Google Scholar
9. Benton MK, Schroeder HE: Social skills training with schizophrenics: a meta-analytic evaluation. J Consult Clin Psychol 1990; 58:741–747Crossref, Medline, Google Scholar
10. Corrigan PW: Social skills training in adult psychotic populations: a meta-analysis. Behav Ther Exp Psychol 1991; 22:203–210Crossref, Medline, Google Scholar
11. Hodel B, Brenner HD: Cognitive therapy with schizophrenic patients: conceptual basis, present state, future direction. Acta Psychiatr Scand 1994; 90:108–115Crossref, Google Scholar
12. Hogarty GE, Goldberg SC, Schooler NR, Collaborative Study Group: Drug and sociotherapy in the aftercare of schizophrenic patients, III: adjustment of nonrelapsed patients. Arch Gen Psychiatry 1974; 31:609–618Crossref, Medline, Google Scholar
13. Shader R: Discussion: sources of variance in studies of drug and other therapies, in Evaluation of Psychological Therapies. Edited by Spitzer RL, Klein DF. Baltimore, Johns Hopkins University Press, 1976, pp 294–300Google Scholar
14. Schooler NR, Keith SF, Severe JB, Matthews S: Acute treatment response and short-term outcome in schizophrenia: first results of the NIMH Treatment Strategies in Schizophrenia Study. Psychopharmacol Bull 1989; 25:331–335Medline, Google Scholar
15. Endicott J, Spitzer RL, Fleiss JL, Cohen J: The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry 1976; 33:766–771Crossref, Medline, Google Scholar
16. Schooler N, Hogarty GE, Weissman MM: Social Adjustment Scale II, in Resource Materials for Community Mental Health Program Evaluators: DHEW Publication 79-328. Edited by Hargraves WA, Atkinson CC, Sorenson JE. Washington, DC, US Government Printing Office, 1979, pp 290–303Google Scholar
17. Overall JE, Gorham DR: The Brief Psychiatric Rating Scale. Psychol Rep 1962; 10:799–812Crossref, Google Scholar
18. Raskin A, Schulterbrant J, Reatig N, McKeon JJ: Replication of factors of psychopathology in interview, ward behavior, and self-report ratings of hospitalized depressives. J Nerv Ment Dis 1969; 148:87–98Crossref, Medline, Google Scholar
19. Covi L, Lipman RS: Primary depression or primary anxiety? a possible psychometric approach to a diagnostic dilemma. Clin Neuropsychopharmacol 1984; 7:924–925Google Scholar
20. Wing JK: A simple and reliable subclassification of chronic schizophrenia. J Ment Sci 1961; 107:862–875Crossref, Medline, Google Scholar
21. Hogarty GE, McEvoy JP, Ulrich RF, DiBarry AL, Bartone P, Cooley S, Hammill K, Carter M, Munetz MR, Perel J: Pharmacotherapy of impaired affect in recovering schizophrenic patients. Arch Gen Psychiatry 1995; 52:29–41Crossref, Medline, Google Scholar
22. Katz MM, Lyerly SF: Methods for measuring adjustment and social behavior in the community, I: rationale, description, discriminative validity and scale development. Psychol Rep 1963; 13:503–535Crossref, Google Scholar
23. Cohen J, Cohen P: Multiple Regression/Correlation Analysis for the Behavioral Sciences. Hillsdale, NJ, Lawrence Erlbaum Associates, 1983Google Scholar
24. Kerlinger FN, Redhazur EJ: Multiple Regression in Behavioral Research. New York, Holt, Rinehart, Winston, 1973Google Scholar
25. Cohen J: Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ, Lawrence Erlbaum Associates, 1988Google Scholar
26. Cohen J: The statistical power of abnormal-social psychological research: a review. J Abnorm Soc Psychol 1962; 65:145–153Crossref, Medline, Google Scholar
27. Anderson CM, Reiss DJ, Hogarty GE: Schizophrenia and the Family: A Practitioner's Guide to Psychoeducation and Management. New York, Guilford Press, 1986Google Scholar
28. Hogarty GE, Kornblith SF, Greenwald D, DiBarry AL, Cooley S, Flesher S, Reiss D, Carter M, Ulrich R: Personal therapy: a disorder-relevant psychotherapy for schizophrenia. Schizophr Bull 1995; 21:379–393Crossref, Medline, Google Scholar
29. Baldwin MH: Relational schemas and the process of social information. Psychol Bull 1992; 112:461–484Crossref, Google Scholar
30. Brim OG: Socialization through the life cycle, in Socialization After Childhood. Edited by Brim OG, Wheeler S. New York, John Wiley & Sons, 1966, pp 3–49Google Scholar
31. Hay DF: Prosocial development. J Child Psychol Psychiatry 1994; 35:29–71Crossref, Medline, Google Scholar



