Three-Year Trials of Personal Therapy Among Schizophrenic Patients Living With or Independent of Family, I: Description of Study and Effects on Relapse Rates
Abstract
OBJECTIVE: The study of individual psychotherapeutic approaches to the treatment of schizophrenia has yielded equivocal findings, partly because of methodologic problems. Further, the ability of psychosocial treatments to prevent psychotic relapse appears to lessen over time. The authors' goal was to develop and test a demonstrably effective individual therapy for schizophrenia. METHOD: Using a study design that addressed previous methodologic issues, the authors evaluated personal therapy specifically designed to forestall late relapse in patients with schizophrenia. They evaluated the effectiveness of personal therapy over a period of 3 years after hospital discharge among 151 patients with schizophrenia or schizoaffective disorder diagnosed according to Research Diagnostic Criteria. The patients were randomly assigned to receive either personal therapy or contrasting therapies in one of two concurrent trials. One trial studied patients who were living with family (N=97); the other studied patients who were living independent of family (N=54). RESULTS: All of the patients had extensive psychiatric histories, but only 44 (29%) experienced recurrent psychotic episodes over the 3-year study period, and only 27 (18%) prematurely terminated the study; most of those who left the study were in the no-personal-therapy conditions. Among patients living with family, personal therapy was more effective than family and supportive therapies in preventing psychotic and affective relapse as well as noncompliance. However, among patients living independent of family, those who received personal therapy had significantly more psychotic decompensations than did those who received supportive therapy. CONCLUSIONS: Personal therapy had a positive effect on adverse outcomes among patients who lived with family. However, personal therapy increased the rate of psychotic relapse for patients living independent of family. The application of personal therapy might best be delayed until patients have achieved symptom and residential stability. (Am J Psychiatry 1997; 154:1504–1513)
The individual “psychological” therapy of schizophrenia has a legacy of variable findings. Four approaches have been studied: psychodynamic psychotherapy, supportive psychotherapy, case management, and behavioral skills training or cognitive problem-solving approaches. All have been extensively reviewed by others and are only summarized here.
Psychodynamic psychotherapy has generally been either ineffective or less effective than contrasting conditions. Critiques have traced the equivocal findings to problems of therapist experience, absence of control subjects or random assignment, high dropout rate, or the conceptual relevance of dynamic therapy to schizophrenia (1–8).
Supportive psychotherapy, although intuitively appealing in descriptive reports (9), has been the subject of only a few experimental studies in schizophrenia (10). All studies suffered methodologic problems, but the best-designed trial (11) demonstrated positive effects on recidivism and role performance for supportive psychotherapy compared with an insight-oriented approach. However, patient attrition in that study constrained inference making. In studies comparing supportive therapy with experimental psychosocial approaches such as family psychoeducation, skills training, or major role therapy (12–18), recipients of supportive therapy have typically experienced significantly poorer outcomes than patients in the experimental conditions.
Case management, often a support system designed to enhance patient access to appropriate interventions, has yielded both positive and negative results (19, 20). When used as a component of assertive community programs, intensive case management appears to engage and maintain patients and reduce use of inpatient facilities, but the effects of case management on quality of life and level of functioning have been either ignored or reported as variable (21).
Social skills training (22, 23) has been found to have significant effects on forestalling early relapse and improving adjustment (the latter most often among inpatients) (8), but many of the areas of functioning affected represented more “micro” than “macro” aspects (24). Questions concerning the generalization of skills training to “real-life” settings are also in need of further study (8). Treatment exposure and the effects of skills training, including effects reported in the largest prospective study that we have conducted to date (12), are often of limited duration (5). An earlier, atheoretical, problem-solving approach that we tested (major role therapy) (17, 25) proved useful for better-recovered patients but had negative effects for certain vulnerable or unmedicated patients. In recent years, the integrated psychological treatment of Brenner et al. (26), a sequenced application of basic cognitive remediation and social skills training or problem-solving techniques, has been evaluated in six completed (27) and two ongoing (28, 29) trials. Published results cited improvement in attention and symptoms, but less apparent effects were observed on higher-order cognitive functioning and social adjustment. More traditional cognitive behavior therapy is only now being described or tested among patients with schizophrenia (30–32).
Our interest in the development of a more disorder-relevant, individual psychological approach to schizophrenia arose not only from an awareness of these methodological constraints but also from our observation that a maintenance skills training approach and a family psychoeducation intervention that we developed appeared to be of decreasing effectiveness against late relapse in the second year after discharge (12). We found that these treatments had very limited effects on the adjustment of nonrelapsed patients. Further, existing studies of psychosocial treatment were constrained by diagnosis, sample size, treatment definition, and the relevance and comprehensiveness of assessments (8).
In late-twentieth-century America, it appears that the maintenance of patients with schizophrenia might increasingly become the responsibility of a single primary clinician as necessary mental health services become less available, inaccessible, or “downsized” by the policies of cost containment and managed care. Furthermore, psychosocial interventions that focus on family approaches do not help the sizable number of patients who live independent of family (33). Until the methodologic problems of past studies are addressed and the crucial prerequisites to psychotherapy of schizophrenia are accommodated, the recommendation that there be a “moratorium” on the study and practice of various forms of “dynamic” psychotherapy (7) seems premature. The prerequisites include control of antipsychotic medication route and dose and the provision of needed services related to housing, financial assistance, nutrition, and health care. More central to the treatment of schizophrenia is the requirement that psychological treatment accommodate important neuropsychological impairments as well as the timing of treatment components to reflect the patients' level of clinical recovery (34). Negative effects of dynamic psychotherapy found in past studies might have represented the imposition of cognitive demands that exceeded the patients' capacities at different stages of recovery. Finally, no controlled study of an individual psychotherapeutic approach exceeded a period of 2 years, a constraint that might have restricted treatment to the resolution of recurrent crises and attainment of stabilization rather than recovery of function.
We conducted two 3-year trials to test the effects of personal therapy specifically designed to forestall schizophrenic relapse, particularly in the second and third years after discharge. Part I of this report describes the study and the effects of personal therapy on relapse rates; part II (in this issue of the Journal) describes the effects of personal therapy on the personal and social adjustment of patients.
METHOD
Design
The studies were initiated in late 1986 and completed in 1995. During hospitalization for an index episode, 186 patients who had just been admitted to the inpatient schizophrenia unit of Western Psychiatric Institute and Clinic met eligibility criteria for the outpatient maintenance studies and gave informed, signed consent to participate in the studies after the benefits and risks had been fully explained. Eligibility for the studies included a Research Diagnostic Criteria (RDC) (35) diagnosis of schizophrenia or schizoaffective disorder; age 16 to 55 years; IQ above 75; the absence of organic brain syndrome and serious alcohol or drug abuse or dependence in the previous 6 months that significantly impaired adjustment; and no medical contraindications that precluded taking maintenance antipsychotic medication. We estimate that, as is common with such criteria, only 25% of all patients with schizophrenia admitted to the inpatient unit were eligible for study; the majority (perhaps 60%) were excluded for reasons of serious drug or alcohol abuse and/or diagnostic uncertainty. (The reasons for ineligibility were not archived.)
Following hospital discharge, 35 of the 186 patients either never returned to the research clinic or returned briefly but refused further treatment (N=25); were administratively terminated from the study for reasons of relocation, disposition to a state hospital, or accidental death (N=6); or had a change of diagnosis from schizophrenia to organic brain syndrome (N=4).
The remaining 151 patients qualified for one of two distinct, concurrent trials and were treated as outpatients under controlled conditions for 36 months. In trial 1, 97 patients who resided with family were randomly assigned to one of four conditions: personal therapy, family psychoeducation/management (family therapy), a combination of personal therapy and family psychoeducation/management (combination personal and family therapy), or supportive therapy. In trial 2, 54 patients who lived either alone or in shared quarters with nonrelatives were randomly assigned to personal therapy or supportive therapy. (One patient who had been living alone before the study returned to her mother's home during the study and withdrew from personal therapy at 18 months when she relapsed. Since this patient did not positively bias the findings regarding the effects of personal therapy and satisfied the criterion of “intent to treat,” she was included in all appropriate analyses.)
All patients in both trials were prescribed antipsychotic medication, adjusted in the initial months of treatment to the minimum effective neuroleptic dose, i.e., the dose below which prodromes of a new episode were likely to emerge but above which more than mild hypokinetic rigidity was observed (36). Medication was prescribed by two part-time, experienced psychiatrists, and medication management was supervised by four master's-level psychiatric nurse clinical specialists.
Since the adequacy or control of antipsychotic medication might have compromised the understanding of previous psychotherapy effects, medication records were analyzed in detail regarding antipsychotic drug compliance as well as type, dose, and route of administration by year, trial, and treatment condition in a search for systematic differences that might influence outcome independent of psychosocial treatment. No such differences were found.
A majority of the patients received intramuscular fluphenazine or haloperidol decanoate throughout the study: 109 (72%) of 151 patients in year 1, 84 (62%) of 135 patients in year 2, and 74 (59%) of 126 patients in year 3. Approximately half of the recipients of intramuscular medications in year 1 and one-fourth in years 2 and 3 also received a supplemental oral neuroleptic as needed. The remaining patients—42 (28%), 51 (38%), and 52 (41%) in year 1, 2, and 3, respectively—received oral antipsychotics exclusively, and the number increased as more patients were maintained on a regimen of clozapine over time (e.g., 11 of 151 patients in the first year and 23 of 126 patients during year 3). There were no trial or treatment condition differences in route of administration.
Medication noncompliance was infrequent. For example, 76% of scheduled intramuscular injections were received as prescribed, and only 21% were late by 1–6 weeks. Similarly, 89% of oral doses were judged by the medication nurse to have been taken as prescribed, and only 9% were believed to have been missed for 1–6 weeks. (Plasma or urine assays designed to validate these judgments were not made.)
Total neuroleptic doses prescribed, expressed in weekly mean dose equivalents of fluphenazine decanoate, were 7.16 mg (SD=6.23) in year 1, 6.88 mg (SD=6.25) in year 2, and 6.93 mg (SD=6.49) in year 3. No differences were observed by year or within a trial; however, somewhat higher neuroleptic doses were prescribed for the patients who were not living with family. The mean dose of clozapine was 330 mg/day (SD=150) across years; there were no trial or treatment condition differences in dose. However, by year 3, 27% (N=12) of the 45 patients who were not living with family, compared with only 14% (N=11) of the 81 patients who were living with family, were being maintained on a regimen of clozapine. There were no important antipsychotic medication differences within trials that would confound psychosocial treatment effects, but the facts that patients living independent of family received higher neuroleptic doses and that a higher percentage of these patients were maintained on a regimen of clozapine are indications of their more extensive psychiatric histories.
Most patients received supplemental thymoleptics as needed, and half were prescribed an antiparkinsonian medication at some time during the study; no significant differences were observed in these medications between or within trials.
The needs of all study patients that related to stable housing, health care, and entitlements were addressed by the patients' primary clinician, independent of treatment condition. Relapsed patients were returned to their original treatment condition on symptom remission, typically to a phase of intervention (in personal and family therapy) below that previously attained.
Personal therapy was provided by two of four full-time, master's-level psychiatric nurse clinical specialists and three part-time doctoral-level clinical psychologists. Family therapy was provided by the other two full-time master's-level psychiatric nurse clinical specialists and by one part-time master's-level psychologist. Supportive therapy was provided by the same project nurses who served as personal or family therapists. Patients assigned to the combined personal and family therapy condition had both a personal therapist and a family therapist. Seven of eight therapists were female, and all were white. All but two part-time psychologists had 15 to 21 years of experience working with schizophrenic patients, most in the context of this long-standing research program. Fidelity to personal, family, and supportive therapy was facilitated by explicit treatment manuals as well as by weekly individual and peer-group supervision provided by two senior (doctoral level) clinical supervisors and/or the principal investigator and by treatment process ratings that identified the practice principles used and the goals achieved. Therapist continuity was consistent: one part-time personal therapist left the study at mid-point and one full-time family therapist left 1 year before study termination. Only four personal therapy, three family therapy, and four supportive therapy patients experienced a change of clinician during the study.
All but eight personal therapy and/or family therapy patients met a priori criteria for treatment exposure that required a predetermined number of sessions as well as the acquisition of skills and their application (personal and family therapy) and/or receipt of medication. Since all eight patients were approximately distributed across personal therapy and family therapy cells and attended the clinic with regularity to the time of study completion or termination, they were included in all appropriate analyses, having at least satisfied the criterion of “intent to treat.” The small number precluded the separate analysis of “partial treatment takes” attempted in a previous study (12).
Definitions of Treatment
Personal therapy. A detailed description of personal therapy is available elsewhere (34). Briefly, personal therapy sought to forestall the late (second-year) relapse common among modern psychosocial approaches (12). Personal therapy also sought to enhance personal and social adjustment through the identification and effective management of affect dysregulation that was believed to either precede a psychotic relapse or provoke inappropriate behavior that was possibly generated by underlying neuropsychological deficits. Personal therapy was applied in a graduated, three-stage, systemic approach in recognition of the sensitivity to therapeutic intensity of many schizophrenic patients (34). Through a process called “internal coping,” personal therapy encouraged the patient to identify the affective, cognitive, and physiological experience of stress. The appraisal of stress and the effect of its subsequent expression on the behavior of others was also facilitated. Personal therapy focused on the patient's characteristic response to stress in general rather than on the idiosyncratic response to a specific stressor. It avoided symbolic interpretation and clarification of unconscious motives and drives. Whereas our earlier studies of family and behavioral approaches (12) sought to gain direct or indirect control over the external sources of stress that appeared to precipitate relapse, personal therapy focused on the patient's internal sources of dysregulation. Analyses of the relapse process (37, 38), whether in stage or continuum models, had indicated that “prodromes” of a new episode most often included aspects of impaired affect.
The basic phase of personal therapy was typically applied in the early months after discharge. Following principles that were useful for establishing a therapeutic alliance and achieving clinical stabilization, therapists offered formation of a treatment contract, provision of minimum effective dosing, basic psychoeducation regarding the nature and treatment of schizophrenia, and techniques of supportive therapy to personal therapy recipients as well as to supportive therapy patients. (Principles of supportive therapy included active listening, correct empathy, appropriate reassurance, reinforcement of patient health-promoting initiatives, and reliance on the therapist for advocacy and problem solving in times of crisis.)
Additional strategies were reserved exclusively for personal therapy recipients in the basic phase. These included a step-by-step plan for the resumption of expected roles and the provision of social and avoidance techniques from social skills training that had earlier been associated with positive 1-year outcomes (39). Internal coping was introduced to personal therapy recipients initially to determine the relationship between stressors as possible triggers and symptom exacerbation. Patients needed to meet certain criteria to advance to the next phase; these criteria included symptom stability, achievement of a stable dose of maintenance medication, and evidence that they had applied selected social skills strategies.
The intermediate phase most often occurred during the first 18 months after discharge. Patients were provided advanced psychoeducation that included a didactic on the adaptive strategies to be taught, the requirements for a successful rehabilitation, and a more formal focus on the prodromes of psychosis. Internal coping strategies progressed to the identification of individual cognitive, affective, and somatic indicators of distress and the appropriate application of basic relaxation (diaphragmatic breathing) and cognitive reframing techniques. In addition, skills training designed to ameliorate social behavior deficits (if needed) and to enhance social perception abilities was introduced. Patients who were able to meet additional clinical criteria moved to the advanced phase of treatment. These criteria included an understanding of the personal effects of stress, acquisition of social perception skills, continued stabilization, and application of basic relaxation techniques.
In the advanced phase, which usually occurred in the last 18 months of treatment, the therapist encouraged the timing of social and vocational initiatives in the community, awareness of one's individual prodromes, progressive relaxation principles, and a growing awareness of one's affect, together with its expression and perceived effect on the behavior of others. This latter phase also included instruction in principles of criticism management and conflict resolution. A simulated vocational setting was provided so that the patient could be observed applying acquired skills in “real-life” situations and any need for continuing remediation could be identified.
As described elsewhere (34), the many strategies embodied in personal therapy were not applied in equal “doses” to every patient. Rather, selected principles of personal therapy were tailored to patients' individual needs. For example, not all patients required or preferred systematic muscle relaxation, but nearly all used deep breathing exercises.
Family therapy. In trial 1, family therapy followed the graduated stages and process that we have described in detail elsewhere (40). These included the three broad phases of joining, survival skills training and reintegration within the home, and reintegration into the community. The principal modification to the family therapy approach was a change in didactic content that reflected issues of importance to the families of first-episode patients (41), such as diagnostic uncertainty and variable prognosis. (Twenty-seven percent [N=26] of patients who lived with family in trial 1 were first-episode patients.) Unlike our past study (12), which excluded households with low ratings for expressed emotion, families with both high and low ratings for expressed emotion were included in trial 1.
Eight percent of the patients (and families) in the personal and family therapy conditions failed to move beyond the basic phase of their respective treatments in trial 1. Approximately 38% of personal therapy patients entered but did not advance beyond the intermediate phase, and 40% of the families entered but did not advance beyond the middle phase of family therapy. Fifty-four percent of personal therapy patients and 52% of family therapy patients and families completed the intermediate phases and entered and/or completed the advanced phases of treatment. Constraints against advancement in personal and family therapy were found in the patient's clinical state and/or family resistance, as well as from limitations imposed by the length of research support. Process analyses of variables that facilitated or impeded advancement in treatment will be the subject of a future report.
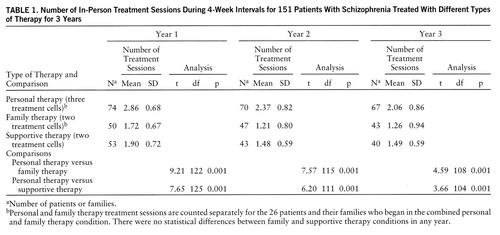
Table 1 shows the average number of monthly in-person treatment sessions and the significant differences between treatment conditions for trials 1 and 2 combined. Treatment sessions were 30–45 minutes long. There were no significant differences in frequency of contact among the three personal therapy cells, the two family therapy cells, and the two supportive therapy cells; therefore, the trials were pooled by treatment condition. Personal therapy sessions were, as designed, significantly more frequent than family therapy and supportive therapy sessions in each treatment year. Personal and family therapy patients also received 1.9 additional monthly medication management sessions in years 1 and 2, and an additional 1.3 sessions each month in year 3. These were brief (15-minute) contacts that usually followed a scheduled personal or family therapy session and were provided to assure that each study patient received the medication management services of a nurse clinical specialist. (Medication management was an integral part of each supportive therapy session provided by the nurses.) Although supportive therapy sessions were less frequent than personal therapy sessions, the 21 annual visits of supportive therapy recipients exceeded the 16 annual visits that are customary in outpatient mental health facilities (42). Actual session frequency approximated the intended frequency: weekly sessions for personal therapy recipients over 3 years, with less contact in year 3 for those who completed treatment objectives; biweekly family sessions for family therapy recipients in year 1, with biweekly to monthly sessions thereafter; and biweekly sessions for supportive therapy recipients in all years. It was not logistically feasible to insist that families and patients in the no-personal-therapy conditions attend more often in order to equalize session frequency. Rather, frequency was dictated by the therapeutic requirements of the respective treatment. However, if necessary, patients in all treatment conditions were seen more often at times of crisis or symptom exacerbation either by their primary therapist or by the Western Psychiatric Institute and Clinic emergency room staff during evenings or weekends.
RESULTS
Study Group Descriptions
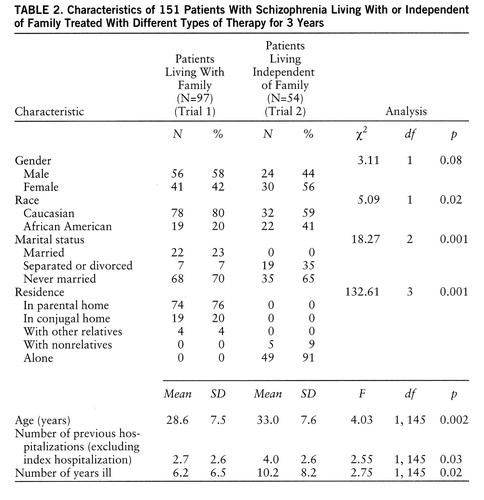
Table 2 shows important demographic and historical variables that differed significantly between patients in the two trials. Patients who were not living with family were older, had been ill for longer periods of time, and had had more previous hospitalizations. This group of patients also included higher percentages of women, African Americans, and individuals who were separated or divorced than did the group of patients residing with family.
Ninety-five (63%) of all study patients met RDC for definite schizophrenia, 11 (7%) for probable schizophrenia, and 45 (30%) for schizoaffective disorder, mostly of the depressed type. (Among the patients with schizoaffective disorder, 39 [87%] were judged to be “mainly schizophrenic,” three [7%] could not be classified, and three were judged to be “mainly affective.") RDC diagnoses were made by reliably trained project (doctoral level) psychologists who have had continuing experience with this method since 1978. All but 25 patients also met a DSM-III-R hospital diagnosis for schizophrenia during the index hospitalization (N=126), and 68 (54%) of these had the paranoid type. (DSM-III-R diagnoses were made by Western Psychiatric Institute and Clinic inpatient academic psychiatrists.) Eleven patients with “schizophreniform” disorders at hospital admission eventually satisfied DSM-III-R criteria for duration following discharge, and 14 patients given “nonschizophrenic” hospital diagnoses all met study RDC study criteria and subsequently had a distinct schizophrenic episode or were clearly paranoid and delusional at various times during the project.
The mean length of the index hospitalization was only 3.9 weeks (SD=1.5), much reduced from our previous studies (18, 39, 43), and 45 (30%) of the patients had a hospitalization in the year before the index hospitalization. Thus, the study group was less stable following index hospitalization discharge than previously studied groups. Regarding education, 36 (24%) had completed college, 59 (39%) had attended college, and 56 (37%) had completed high school or less. Thus, this group of patients had more education than groups we have studied previously. Forty-eight (32%) of the patients had worked at unskilled or semiskilled jobs in the past, 30 (20%) at clerical or sales positions, and 30 (20%) had functioned as homemakers or students in their highest occupational role.
On a 4-point repeated measure of therapeutic alliance called “treatment connectedness,” 639 (90%) of the 710 patient assessments collected over 3 years indicated moderate or high connectedness, as did 108 (87%) of 124 family assessments in the two family therapy treatment cells. However, in trial 1—among patients who were living with family—patients in the combined personal and family therapy condition were significantly less connected over all 3 years, and families were less connected in the family therapy condition than were families in the combined personal and family therapy condition during years 2 and 3.
Over the 3 years of study, only 27 patients (18%) terminated prematurely: 24 because of treatment noncompliance and refusal to continue the study and three for administrative reasons. Eighteen of 24 treatment-related terminations occurred in the no-personal-therapy conditions.
Relapse
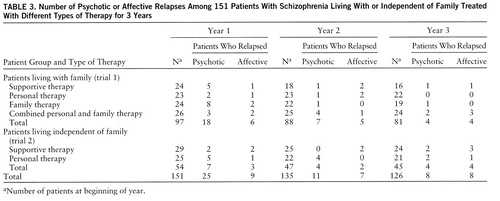
Relapse was analyzed by life table survivorship methods, not only for time to first psychotic episode but also for time to first affective episode as well as treatment-related termination. Multiple episodes were relatively few, and survivorship analyses of these were less revealing than the simple calculations presented in tables 3 and 4. The two trials were first analyzed separately and then combined as three personal therapy cells and three no-personal-therapy cells.
Over 3 years, 44 (29%) of 151 patients experienced a combined total of 66 recurrent episodes of schizophrenia, and 24 (16%) patients experienced 28 nonpsychotic affective relapses. These relapse rates are very low, given the serious psychiatric history and morbidity of the patients studied. The rates of schizophrenic relapse were lower than those observed in our former studies (12, 16, 18, 36). Schizophrenic relapse was defined as either a clinical change from the remission of positive symptoms to symptom exacerbation or a significant increase in persistent symptoms. The relapse criteria comprised both the clinical consensus of the research team and significant rating scale changes. The latter represented changes from mild or less to greater than mild on two or more of the four psychotic symptoms on the Brief Psychiatric Rating Scale (BPRS) (44) (change from the remission of positive symptoms to symptom exacerbation) or a 2-point increase on one or more moderately severe, persistent symptoms (significant increase in persistent symptoms), plus a decrease of 10 points or more on the Global Assessment Scale (GAS) (45). For example, among the patients who had psychotic relapses, the mean score on the four-item BPRS psychotic factor changed from 1.75 (SD=0.82) before relapse to 3.26 (SD=1.3) at the time of relapse (paired t=9.14, df=53, p=0.001). The mean GAS score changed from 60.5 (SD=10) before relapse to 39.6 (SD=11) at relapse (paired t=9.13, df=53, p=0.001). Type of relapse did not differ by treatment condition.
All but two of the 66 recurrent psychotic episodes required rehospitalization. All 24 patients with affective episodes were rehospitalized, and their 28 episodes were most often characterized by major depression. Thirteen episodes presented with suicidal ideation or attempts, four with depression alone, eight with concurrent alcohol or drug abuse, and three episodes with assaultive or hypomanic behavior. Multiple affective episodes were rare and noncontributing events for the patients who were living with family, but they were of importance for patients living independent of family. Twelve of the 22 multiple psychotic episodes appeared to be a continuation of the same episode that had required rehospitalization in the previous month. Table 4 provides a summary of the psychotic and affective relapses, together with treatment terminations, for all trials and conditions over the 3-year study period.
Relapse Among Patients Living With Family (Trial 1)
From life table analyses of the data provided in tables 3 and 4 (based upon the Wilcoxon [Gehan] statistic) that accounted for both the number and speed of relapse, there was a nonsignificant indication (χ2=2.87, df=1, p=0.09) that personal therapy forestalled psychotic relapse. Specifically, the personal therapy alone condition had a lower psychotic relapse rate than either the supportive therapy condition (χ2=2.74, df=1, p=0.10) or the family therapy condition (χ2=5.33, df=1, p=0.02). There were no significant differences regarding affective episodes. As can be seen in table 4, however, 13 of 15 treatment-related terminations among the patients living with family occurred in the no-personal-therapy conditions, particularly in the supportive therapy condition, thus limiting survivorship to less representative and possibly less vulnerable patients in these no-personal-therapy conditions.
When all adverse outcomes were tested by survivorship analyses (time to first psychotic or affective episode or treatment-related early termination), there was a significant overall effect of personal therapy on delaying adverse outcome (χ2=3.64, df=1, p=0.06). This most illustrative effect of personal therapy is shown in figure 1 and suggests that the greatest protection offered by personal therapy against poor outcome occurs in the first year after discharge. Among the four treatment conditions, the largest difference was between personal therapy alone and supportive therapy (χ2=6.62, df=1, p=0.01).
Relapse Among Patients Living Independent of Family (Trial 2)
Whether in terms of time to first psychotic episode or multiple psychotic episodes, among patients living independent of family, personal therapy recipients experienced significantly more relapse than supportive therapy recipients (χ2=5.63, df=1, p=0.02). As indicated in table 4, over 3 years, 11 patients who received personal therapy had 27 recurrent psychotic episodes, compared with four supportive therapy patients, each of whom experienced one episode. Conversely, there was a nonsignificant indication of fewer affective episodes among personal therapy recipients (χ2=2.87, df=1, p=0.09). Only two individual affective episodes occurred among personal therapy recipients, compared with 10 episodes among seven supportive therapy patients. However, when all adverse outcomes were analyzed (psychotic and affective episodes and treatment-related terminations), there was no significant difference between the two treatment conditions. When trials were combined, rates of relapse and treatment termination for patients given or not given personal therapy did not differ because of the psychotic relapse rate of patients living independent of family who received personal therapy.
DISCUSSION
For patients living with family (trial 1), the circumscribed but positive effects of personal therapy in forestalling psychotic relapse and the absence of a family therapy main or interactive effect are not so much indications of ineffectiveness of the psychosocial treatments as results of the extraordinary survivorship of the patients given supportive therapy. One-third of supportive therapy patients had premature, treatment-related terminations (most with subsequent poor outcomes), but the patients who continued to receive supportive therapy had a 76% survivorship at 1 year and 72% at 2 years. By comparison, the survivorship without psychotic relapse for the control patients in our previous trial (12) was only 31.5% after 2 years. (In other studies comparing supportive therapy with family therapy or social skills training, survivorship among the patients who received supportive therapy averaged only 50% at 1 year [46–49] and was often less than 20% at 2 years [13–15].)
There is some evidence that we achieved our goal of forestalling late schizophrenic relapse by applying a more disorder-relevant, individual approach in that 87% of the patients living with family who received personal therapy alone survived 2 years without relapse or early termination and experienced no further relapse or termination in year 3, compared with a 50% survivorship rate at 2 years for patients given social skills training alone in another study (12). We are also encouraged by the unexpected treatment adherence to personal therapy over the 3-year study period, compared with a high dropout rate (66%) at 2 years associated with insight-oriented psychotherapy in another outpatient study (11). The effects of the combined personal plus family therapy condition are very similar to the effects we found in an earlier study of social skills training plus family therapy (12). However, family therapy alone, with a 62% rate of survivorship at 2 years, appears somewhat less effective, though not statistically different from the previous family therapy alone condition (71% survivorship at 2 years) (12).
We can only speculate about the reasons for the low rate of relapse across treatment conditions in the current study. Patients did not differ from earlier study groups on important demographic and psychiatric history variables except that the patients in the current study were better educated than previous groups. A possible explanation might be traced to the considerable clinical experience gained by study clinicians during our numerous treatment studies at Western Psychiatric Institute and Clinic, including a recent investigation of supplemental thymoleptics in the management of affectively impaired outpatients with schizophrenia (50). Further, the supportive therapy condition in the current study was the most comprehensive of any previously tested by us. It included not only an explicit treatment contract but also the principles of supportive therapy, minimum effective dosing, patient psychoeducation, and case management addressed to needed services. This change in supportive therapy was made to enhance treatment compliance, and it apparently maintained the clinical remission of most patients who remained in treatment.
Finally, not to be ignored is the fact that the study provided reimbursement of transportation costs for the more financially impoverished patients, independent of treatment condition, to facilitate clinic attendance (approximately $6,000 to $7,000 annually for the program). Although this seems extravagant, the savings from one prevented rehospitalization would likely exceed the annual reimbursement of travel costs for all study subjects.
For patients living independent of family (trial 2), the unequivocal failure of personal therapy to forestall psychotic relapse (in fact, it significantly increased relapse rates) is difficult to explain in the absence of more definitive predictor analysis. In retrospect, we think that the severe practical problems associated with community maintenance might have represented such a full agenda for some of the patients living independent of family and receiving personal therapy that attempts to develop adaptive techniques useful for relapse prevention might have either seemed a low priority or constituted a detrimental cognitive overload. Patients had to meet clinical criteria for entry into the intermediate and advanced phases of personal therapy (34), but, in retrospect, we think that criteria assuring residential and symptom stability should be applied before basic phase principles are introduced.
Evidence suggesting that some patients living independent of family experienced cognitive overload could be found. We examined a schedule of 10 life stressors assessed among patients who lived independent of family. (Part II of our report in this issue of the Journal describes the nature and frequency of adjustment assessments.) Although patients living independent of family who received supportive therapy generally experienced more difficulty with these stressors at clinic intake than did those who received personal therapy, a comparison of the 11 relapsed and 14 nonrelapsed personal therapy patients revealed that those who eventually relapsed one or more times experienced more difficulty securing food and clothing at clinic intake than did those who did not relapse (t=2.21, df=23, p=0.04). However, it was during the next 30 months that relapsed patients were persistently involved in significantly more arguments and conflicts with landlords and/or community residential rehabilitation and transitional living staff than were patients who did not relapse. Case debriefings also indicated that most personal therapy patients who relapsed had initially lived in more unstable and/or minimally structured settings than did personal therapy patients who did not relapse. Clinical stability was ultimately achieved when appropriate supported housing was secured. It is unclear from this post hoc analysis, of course, whether conflicts and/or unstable residences were the cause or the effect of repeated psychotic episodes. Nonetheless, the phenomenon of concurrent environmental demands that challenge cognitive capacity might explain, in part, the limited effects observed for the individual psychotherapy of schizophrenia in this and previous studies, including our own problem-solving approach (25).
A better-than-expected outcome for supportive therapy patients who were living with family and a poor outcome for personal therapy patients who were living independent of family might reflect a failure to achieve an equal distribution of important characteristics across treatment conditions before treatment, in spite of random assignment. However, an exhaustive analysis of initial differences among treatment conditions revealed very few distinguishing characteristics. These represented more first episodes (and thus younger patients) as well as more families with high ratings for expressed emotion (51) in the family therapy conditions in trial 1, and more divorced or separated patients in the trial 2 personal therapy condition. Randomization appeared successful regarding the primary variables of clinical state and psychiatric history for which it was intended. Only when many secondary characteristics were explored could initial differences among treatment groups occasionally be detected, a likely occurrence that only very large study groups might correct.
Our findings reveal evidence that personal therapy provides greater prophylaxis against overall adverse outcome than family therapy or supportive therapy among patients with schizophrenia who live with family but provides less prophylaxis against psychotic relapse among those who live independent of family. The relative importance of this variable effect is better understood in terms of the unconfounded effects of personal therapy on personal and social adjustment, a consideration that is addressed in part II of our report in this issue of the Journal.
 |
 |
 |
 |
Received Jan. 31, 1996; revisions received Dec. 18, 1996, and Feb. 26 and May 30, 1997; accepted June 2, 1997. From the Department of Psychiatry, University of Pittsburgh School of Medicine. Address reprint requests to Professor Hogarty, Western Psychiatric Institute and Clinic, 3811 O'Hara St., Pittsburgh, PA 15213. Supported by a MERIT extension of NIMH grant MH-30750. The authors thank G. Alexander, M.D., P. Bartone, M.S.N., A. Garrett, Ph.D., K. Hammill, M.S.N., H. Levin, M.D., D. Reiss, Ph.D., and E. Venditti, Ph.D., for their assistance in conducting the studies.
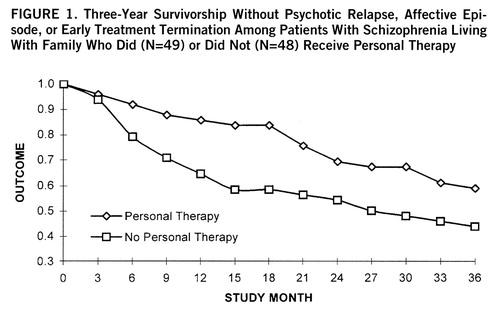
FIGURE 1. Three-Year Survivorship Without Psychotic Relapse, Affective Episode, or Early Treatment Termination Among Patients With Schizophrenia Living With Family Who Did (N=49) or Did Not (N=48) Receive Personal Therapy
1. Gunderson JG, Mosher LR (eds): Psychotherapy of Schizophrenia. New York, Jason Aronson, 1975Google Scholar
2. May PRA: Schizophrenia: evaluation of treatment methods, in Comprehensive Textbook of Psychiatry. Edited by Freedman AM, Kaplan HI, Sadock BJ. Baltimore, Williams & Wilkins, 1975, pp 955–981Google Scholar
3. Schooler NR: Antipsychotic drugs and psychosocial treatment in schizophrenia, in Psychopharmacology: A Generation of Progress. Edited by Lipton MA, DiMascio A, Killam KF. New York, Raven Press, 1978, pp 1155–1168Google Scholar
4. Drake RE, Sederer LI: The adverse effects of intensive treatment of chronic schizophrenia. Compr Psychiatry 1986; 27:313–326Crossref, Medline, Google Scholar
5. Schooler NR, Hogarty GE: Medication and psychosocial strategies in the treatment of schizophrenia, in Psychopharmacology: The Third Generation of Progress. Edited by Meltzer HY. New York, Raven Press, 1987, pp 1111–1119Google Scholar
6. Katz HM, Gunderson JG: Individual psychodynamically oriented psychotherapy for schizophrenic patients, in Handbook of Schizophrenia: Psychosocial Treatment of Schizophrenia. Edited by Herz MI, Keith SJ, Docherty JP. Amsterdam, Elsevier, 1990, pp 69–90Google Scholar
7. Mueser KT, Berenbaum H: Psychodynamic treatment of schizophrenia: is there a future? Psychol Med 1990; 20:253–262Google Scholar
8. Scott JE, Dixon LB: Psychological interventions for schizophrenia. Schizophr Bull 1995; 21:621–630Crossref, Medline, Google Scholar
9. Kates J, Rockland LH: Supportive psychotherapy of the schizophrenic patient. Am J Psychother 1994; 48:543–561Crossref, Medline, Google Scholar
10. Conte HR, Plutchik R: Controlled research in supportive psychotherapy. Psychiatr Annals 1986; 16:530–533Crossref, Google Scholar
11. Gunderson JG, Frank AF, Katz HM, Vannicelli ML, Frosch JP, Knapp PH: Effects of psychotherapy in schizophrenia, II: comparative outcome of two forms of treatment. Schizophr Bull 1984; 10:564–598Crossref, Medline, Google Scholar
12. Hogarty GE, Anderson CM, Reiss DJ, Kornblith SJ, Greenwald DP, Ulrich RF, Carter M: Family psychoeducation, social skills training, and maintenance chemotherapy in the aftercare treatment of schizophrenia, II: two-year effects of a controlled study on relapse and adjustment. Arch Gen Psychiatry 1991; 48:340–347Crossref, Medline, Google Scholar
13. Leff J, Kuipers L, Berkowitz R, Sturgeon D: A controlled trial of social intervention in the families of schizophrenic patients: two-year follow-up. Br J Psychiatry 1985; 146:594–600Crossref, Medline, Google Scholar
14. Falloon IRH, Boyd JL, McGill CW, Williamson W, Razoni J, Moss HB, Gilderman AM, Simpson GM: Family management in the prevention of morbidity of schizophrenia. Arch Gen Psychiatry 1985; 42:887–896Crossref, Medline, Google Scholar
15. Tarrier N, Barrowclough C, Vaughn C, Bamrak JS, Porceddu K, Watts S, Freeman H: Community management of schizophrenia: a two-year follow-up of a behavioural intervention with families. Br J Psychiatry 1989; 154:625–628Crossref, Medline, Google Scholar
16. Hogarty GE, Goldberg SC, Schooler NR, Ulrich RF: Drug and sociotherapy in the aftercare of schizophrenic patients, II: two-year relapse rates. Arch Gen Psychiatry 1974; 31:603–608Crossref, Medline, Google Scholar
17. Hogarty GE, Goldberg SC, Schooler NR, Collaborative Study Group: Drug and sociotherapy in the aftercare of schizophrenic patients, III: adjustment of nonrelapsed patients. Arch Gen Psychiatry 1974; 31:609–618Crossref, Medline, Google Scholar
18. Hogarty GE, Schooler NR, Ulrich RF, Mussare F, Herron E, Ferro P: Fluphenazine and social therapy in the aftercare of schizophrenic patients: relapse analyses of a two-year controlled study of fluphenazine decanoate and fluphenazine hydrochloride. Arch Gen Psychiatry 1979; 36:1283–1294Google Scholar
19. Ruben A: Is care management effective for people with serious mental illness? a research review. Health and Soc Work 1992; 17:138–150Crossref, Medline, Google Scholar
20. Hornstra RK, Bruce-Wolfe V, Sagduyu K, Riffle DW: The effect of intensive case management on hospitalization of patients with schizophrenia. Hosp Community Psychiatry 1993; 44:844–847Abstract, Google Scholar
21. Bond GR, McGrew JH, Fekete DM: Assertive outreach for frequent users of psychiatric hospitals: a meta-analysis. J Ment Health Administration 1995; 22:4–16Crossref, Medline, Google Scholar
22. Benton MK, Schroeder HE: Social skills training with schizophrenics: a meta-analytic evaluation. J Consult Clin Psychol 1990; 58:741–747Crossref, Medline, Google Scholar
23. Corrigan PW: Social skills training in adult psychotic populations: a meta-analysis. Behav Ther Exp Psychol 1991; 22:203–210Crossref, Medline, Google Scholar
24. Bellack AS, Mueser KT: Psychosocial treatment for schizophrenia. Schizophr Bull 1993; 19:317–336Crossref, Medline, Google Scholar
25. Goldberg SC, Schooler NR, Hogarty GE, Roper M: Prediction of relapse in schizophrenic patients treated by drug and social therapy. Arch Gen Psychiatry 1977; 34:171–184Crossref, Medline, Google Scholar
26. Brenner HD, Hodel B, Roder V, Corrigan P: Treatment of cognitive dysfunctions and behavioral deficits in schizophrenia. Schizophr Bull 1992; 18:21–26Crossref, Medline, Google Scholar
27. Hodel B, Brenner HD: Cognitive therapy with schizophrenic patients: conceptual basis, present state, future direction. Acta Psychiatr Scand 1994; 90:108–115Crossref, Google Scholar
28. Kraemer S, Suly KHD, Schmidt R, Lassle R: Cognitive therapy of schizophrenic patients under standard care. Nervenarzt 1987; 58:84–90Medline, Google Scholar
29. Spaulding WD, Sullivan M, Weller M, Reed D, Richardson C, Storzbach D: Changing cognitive functioning in rehabilitation of schizophrenia. Acta Psychiatr Scand 1994; 90:116–124Crossref, Google Scholar
30. Kingdon DG, Turkington D, John C: Cognitive behavioral therapy of schizophrenia. Br J Psychiatry 1994; 164:581–587Crossref, Medline, Google Scholar
31. Perris C: Cognitive Therapy With Schizophrenic Patients. New York, Guilford Press, 1988Google Scholar
32. Fowler D, Garet P, Kuipers E: Cognitive Behavior Therapy for Psychosis. Chichester, England, John Wiley & Sons, 1995Google Scholar
33. Tessler RC, Bernstein AG, Rosen BM, Goldman HH: The chronic mentally ill in community support systems. Hosp Community Psychiatry 1982; 33:208–211Abstract, Google Scholar
34. Hogarty GE, Kornblith SF, Greenwald D, DiBarry AL, Cooley S, Flesher S, Reiss D, Carter M, Ulrich R: Personal therapy: a disorder-relevant psychotherapy for schizophrenia. Schizophr Bull 1995; 21:379–393Crossref, Medline, Google Scholar
35. Spitzer RL, Endicott J, Robins E: Research Diagnostic Criteria (RDC) for a Selected Group of Functional Disorders, 3rd ed. New York, New York State Psychiatric Institute, Biometrics Research, 1978Google Scholar
36. Hogarty GE, McEvoy JP, Munetz M, DiBarry AL, Bartone P, Cather R, Cooley SF, Ulrich RF, Carter M, Madonia MJ, EPICS Research Group: Dose of fluphenazine, familial expressed emotion, and outcome in schizophrenia: results of a two-year controlled study. Arch Gen Psychiatry 1988; 45:797–805Crossref, Medline, Google Scholar
37. Carr VJ: Recovery from schizophrenia: a review of patterns of psychosis. Schizophr Bull 1983; 9:95–121Crossref, Medline, Google Scholar
38. Herz MI, Glazer W, Mirza M, Mostert M, Hafez H: Treating prodromal episodes to prevent relapse in schizophrenia. Br J Psychiatry 1989; 155:123–127Medline, Google Scholar
39. Hogarty GE, Anderson CM, Reiss DJ, Kornblith SJ, Greenwald DP, Javna CD, Madonia MJ: Family psychoeducation, social skills training, and maintenance chemotherapy in the aftercare treatment of schizophrenia, I: one-year effects of a controlled study on relapse and expressed emotion. Arch Gen Psychiatry 1986; 43:633–642Crossref, Medline, Google Scholar
40. Anderson CM, Reiss DJ, Hogarty GE: Schizophrenia and the Family: A Practitioner's Guide to Psychoeducation and Management. New York, Guilford Press, 1986Google Scholar
41. Wynne LC: Working with families of acute psychotics: problems for research and reconsideration, in Treatment of Schizophrenia: Family Assessment and Intervention. Edited by Goldstein MJ, Hand I, Hahlweg K. Heidelberg, Springer-Verlag, 1986, pp 109–115Google Scholar
42. Narrow WE, Regier DA, Rae DS, Manderscheid RW, Locke BZ: Use of services by persons with mental and addictive disorders. Arch Gen Psychiatry 1993; 50:95–107Crossref, Medline, Google Scholar
43. Hogarty GE, Goldberg SC, Collaborative Study Group: Drug and sociotherapy in the aftercare of schizophrenic patients: one-year relapse rates. Arch Gen Psychiatry 1973; 28:54–64Crossref, Medline, Google Scholar
44. Overall JE, Gorham DR: The Brief Psychiatric Rating Scale. Psychol Rep 1962; 10:799–812Crossref, Google Scholar
45. Endicott J, Spitzer RL, Fleiss JL, Cohen J: The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry 1976; 33:766–771Crossref, Medline, Google Scholar
46. Wallace CJ, Liberman RP: Social skills training for patients with schizophrenia: a controlled clinical trial. Psychiatry Res 1985; 15:239–247Crossref, Medline, Google Scholar
47. Leff J, Kuipers L, Berkowitz R, Eberlein-Vries R, Sturgeon D: A controlled trial of social intervention in the families of schizophrenic patients. Br J Psychiatry 1982; 141:121–134Crossref, Medline, Google Scholar
48. Falloon IRH, Boyd JL, McGill CW, Razoni J, Moss HB, Gilderman HA: Family management in the prevention of exacerbations of schizophrenia. N Engl J Med 1982; 306:1437–1444Google Scholar
49. Tarrier N, Barrowclough C, Vaughn C, Bamrak JS, Porceddu K, Watts S, Freeman H: The community management of schizophrenia: a controlled trial of a behavioural intervention with families to reduce relapse. Br J Psychiatry 1988; 153:532–542Crossref, Medline, Google Scholar
50. Hogarty GE, McEvoy JP, Ulrich RF, DiBarry AL, Bartone P, Cooley S, Hammel K, Carter M, Munetz MR, Perel J: Pharmacotherapy of impaired affect in recovering schizophrenic patients. Arch Gen Psychiatry 1995; 52:29–41Crossref, Medline, Google Scholar
51. Leff J, Vaughn CE: Expressed Emotion in Families. New York, Guilford Press, 1985Google Scholar



