Partial Compliance and Risk of Rehospitalization Among California Medicaid Patients With Schizophrenia
Abstract
OBJECTIVE: The objective of this study was to evaluate the relationship between compliance with an antipsychotic medication regimen and risk of hospitalization in a cohort of California Medicaid patients with schizophrenia. METHODS: Compliance behavior was estimated by using a retrospective review of California Medicaid pharmacy refill and medical claims for 4,325 outpatients for whom antipsychotics were prescribed for treatment of schizophrenia from 1999 to 2001. Compliance behavior was estimated by using four different definitions: gaps in medication therapy, medication consistency and persistence, and a medication possession ratio. Patients were followed for one year and had an average of 19.1 dispensing events. Logistic regression models using each compliance estimate were used to determine the odds of hospitalization. RESULTS: Risk of hospitalization was significantly correlated with compliance. With all definitions, lower compliance was associated with a greater risk of hospitalization over and above any other risk factors for hospitalization. For example, the presence of any gap in medication coverage was associated with increased risk of hospitalization, including gaps as small as one to ten days (odds ratio [OR]=1.98). A gap of 11 to 30 days was associated with an OR of 2.81, and a gap of more than 30 days was associated with an OR of 3.96. CONCLUSIONS: This study showed a direct correlation between estimated partial compliance and hospitalization risk among patients with schizophrenia across a continuum of compliance behavior.
Medication compliance, or adherence, among patients with schizophrenia has often been reported as an all-or-nothing behavior: the patient either is compliant or is not. This notion of noncompliance as complete, willful cessation of all antipsychotic medications is not an accurate representation of actual medication-taking behavior among outpatient populations with schizophrenia. Recent studies using more sophisticated assessments have found that a majority of patients with schizophrenia who are considered to be compliant with their antipsychotic medication regimens actually show a range of compliance behaviors, probably for many diverse reasons. The full range of compliance-spectrum behavior becomes apparent when patient self-report is contrasted with other, more quantitative, measures, such as the Medication Event Monitoring System (MEMS) (1), or when compliance is determined by blood samples taken during unscheduled home visits (2).
Thus the term "partial compliance" seems preferable to "noncompliance" in that the former explicitly acknowledges the common situation in which a person takes some, but not all, of his or her prescribed medication. Partial compliance may take several forms, including taking an amount that is consistently less than recommended, irregular ("on-and-off") dosing behavior, and having discrete gaps in antipsychotic therapy—for example, in the case of patients who are unwilling or unable to refill a prescription.
It is important to note that partial compliance refers only to compliance behavior and does not reflect either the efficacy of the treatment or the person's attitude toward taking medication. For example, partial compliance can be due to efficacy problems (such as cognitive dysfunction that leads to forgetting to pick up a refill), systems barriers (for example, a prescription is not refilled because insurance coverage has run out), or an intentional decision to stop taking medication.
A number of studies have shown that most patients with schizophrenia are partially compliant (3,4). Docherty and colleagues (3) found that 90 percent of patients with schizophrenia had some degree of partial compliance. In this overall sample of 675 patients, medications were not available for 36 percent of patient-days of medication exposure. McCombs and colleagues (4) found that 92 percent of a sample of 2,010 patients with schizophrenia had at least one disruption in antipsychotic medication coverage during the course of a year and that the mean duration of therapy was only 142 days per year (4). Another study reported that among patients with early-episode schizophrenia, 63 percent of a sample of 182 had at least one gap in therapy over a one-year period, with most of these gaps extending over a month (5). However, comparison of partial compliance rates between studies is difficult, because the techniques used to measure compliance, as well as the definitions of compliance, vary from study to study.
It is well known that medication noncompliance is one of the most important modifiable risk factors for relapse among patients with schizophrenia (6,7). Estimates suggest that noncompliance causes about 40 percent of relapse (8). A review of seven studies demonstrated that noncompliant patients had a six-month to two-year relapse risk that was about 3.7 times that of compliant patients (9). First-episode patients, who potentially have the most to lose from repeated relapse, are similarly likely to experience relapse when their treatment is interrupted (10). However, these studies used the traditional definition of noncompliance—that is, complete discontinuation of antipsychotic medication. Thus the relationship between partial compliance and relapse risk is not known. An understanding of the role of partial compliance in relapse will help define the threshold between the extent of partial compliance and risk of relapse.
One approach for examining the effect of partial compliance on outcome is to use pharmacy claims data as a conservative proxy measure for compliance behavior. Analysis of pharmacy claims has been used successfully for other chronic diseases—for example, hypertension and epilepsy—to show relationships between partial compliance and hospitalization (11,12,13,14). Claims records in administrative databases can be used to assess whether patients discontinue their medication therapy (stop taking their medication) or refill medications inconsistently (skip doses) (15,16,17,18,19,20).
The primary objectives of the analysis reported here were to determine the association between estimates of partial compliance and outcome, with the hypothesis that the lower the compliance, the greater the risk of hospitalization, and to evaluate the quantitative characteristics that define any potential relationship between partial compliance and hospitalization.
Methods
Study design and population
A 20 percent random sample of 1999-2001 California Medicaid data was used to evaluate the association between partial compliance and hospitalization. To be included, patients with schizophrenia—that is, patients with an ICD-9-CM code of 295.xx—had to have at least two dispensing events for antipsychotic medications during a six-month enrollment period (July 1 to December 31, 1999). Qualifying prescription claims included claims for all approved oral antipsychotic medications, including newer antipsychotics available before January 1, 2000.
Each patient was assigned an index date, defined as the date of the patient's first prescription during the enrollment period. Because it is possible that patients with new diagnoses would have significantly different compliance issues while being stabilized with medication therapy, the goal was to study patients who were already receiving antipsychotics. Therefore, patients were also required to have at least one prescription in the six months before their index date. The study was not examined by an institutional review board, because all personal identifiers were removed and the investigators were not aware of the patients' identities at any time.
Data were obtained for 12 months after each patient's index date (the observation period). Because compliance patterns might be affected when patients are about to lose eligibility, patients included in the study were those who remained eligible for California Medicaid for an additional three months after the observation period. Patients were excluded if they were younger than 18 years at the start of the study period, if they had long-term-care visits (because of the possibility of incomplete records), or if their calculated medication use (number of units dispensed divided by days' supply was ten or more. The reason for the units-per-day restriction was that a use of ten or more times per day suggests data entry errors.
Patients who had a claim coded with an ICD-9-CM code for bipolar disorder (296.0x, 296.1x, or 296.4-296.8) at any point within the available data set were dropped from the analysis on the grounds that these patients might use drugs other than antipsychotics (for example, lithium) as a primary therapy (thus violating necessary assumptions for calculation of compliance variables). Patients who were receiving long-acting antipsychotics (haloperidol decanoate or fluphenazine decanoate) were excluded because of inconsistencies in the number of days' supply recorded.
Measures of partial compliance
Four measures of compliance were evaluated: gaps in medication therapy, medication consistency, medication persistence, and a medication possession ratio (MPR). Because the results from all measures were similar, the primary focus in this article is on gaps in medication, a measure that is conceptually straightforward and easiest to use in clinical practice. For this study, medication gap was defined as the longest period during which no medication appeared to be available. Contiguous periods in which no medication appeared to be available were based on dispensing date and recorded days' supply for each antipsychotic prescription. Four categories based on each patient's maximum gap in therapy were defined: zero days, one to ten days, 11 to 30 days, and more than 30 days. The mean number of gaps per patient and the mean gap duration (across all therapy gaps) were also calculated.
Medication consistency is a measure of whether patients skipped doses when medication should have been available—that is, between the dates of the first and last prescriptions a patient had filled. Consistency was calculated, using a modified definition from the literature (21), as the percentage of time a patient appears to have medication available divided by the period during which the patient should have theoretically used all the available medication. A weighted average was taken across antipsychotic therapies. Medication persistence captures whether a patient discontinued all therapies. This calculation represents the number of days between the first and last prescription, divided by the fixed number of days in the study period.
The MPR was calculated in a manner similar to that used for therapy gaps and is a modification of the literature-based formula (15,16). The number of days a patient was not hospitalized and showed evidence of use of any antipsychotic medication (based on dispensing date and days' supply recorded on the prescription claim) were summed. The MPR was calculated by dividing this sum by the number of ambulatory days in the study period. By evaluating the percentage of days over a fixed period, the MPR combines assessments of skipping doses (consistency) and discontinuation (persistence) into a single composite measure.
Measure of hospitalization
A marker was created to indicate whether a patient had at least one "mental health hospitalization" during the one-year, postindex observation period. Mental health hospitalizations were identified by using "mental health" ICD-9-CM diagnosis codes in the first (primary) diagnosis field. The following diagnosis codes were used: schizophrenia (295.xx), depression (296.2x, 296.3x, 296.9x, 300.4x, 309.0x, or 311.xx), anxiety (300.0x, 300.2x, 300.3x, 306.9x, 308.xx, 309.2x, 309.4x, or 309.9x), other psychoses (297.xx, 298.xx, 299.xx, 300.1x, 302.8x, or 307.9x), and dementia (290.xx, 291.2x, 310.9x, or 331.0). Use of a broad definition of psychiatric hospitalization ensured that no relevant psychiatric hospitalizations related to the index diagnosis of schizophrenia were missed.
Statistical analysis
The primary analysis evaluated the relationship between compliance and the presence of at least one mental health hospitalization during the one-year follow-up period. Logistic regression models predicting presence of at least one hospitalization in the postindex year were developed for each of the compliance measures. Medication gap models predicted hospitalization by using four gap categories: zero days, one to ten days, 11 to 30 days, and more than 30 days. Logistic models for consistency, persistence, and the MPR predicted hospitalization by using continuous measures. Interactions were included only if they added significantly to the explanatory power of the model; variables were dropped from the models if they were insignificant and had a negative impact on model fit. Compliance was also categorized and evaluated by using chi square tests.
For descriptive analyses, consistency, persistence, and MPR mean scores as well as categorical frequencies are presented. For consistency and the MPR, the compliance categories defined less than 70 percent compliance as noncompliant and at least 70 percent compliance as compliant. Although no standard is available for identifying compliance categories, the literature suggests that a 70 percent cutoff is reasonable (3,22,23). The MPR was calculated in a manner such that no values exceeded 100 percent. The categories for persistence were less than 90 percent compliance and at least 90 percent compliance.
Results
Patient disposition and demographic characteristics
A total of 4,325 patients met the selection criteria. Patient characteristics are summarized in Table 1. The patients' mean age was 44.2 years; 58.5 percent were men, and 55.6 percent were white. Approximately half were also Medicare eligible (48.9 percent). A total of 654 patients (15.1 percent) had at least one psychiatric hospitalization. Analysis of the crude data also showed that age, ethnicity, and insurance status were associated with likelihood of hospitalization. Hospitalization was less likely with increasing age but more likely among patients who were African American and among patients who were eligible for Medicare (Table 2).
Partial compliance and hospitalization
The patients in the study were on the more compliant end of the compliance continuum, as indicated by the mean compliance variables, shown in Table 3. Only 267 patients (6.2 percent) had a persistence level of less than 90 percent, yielding an average persistence of 97 percent. During the one-year observation period patients had a mean±SD number of dispensing events of 19.1±15.9 for 1.65±.87 different drug entities.
Figure 1 shows the percentage of patients hospitalized as categorized by medication gap within a one-year period. All pairwise comparisons with the reference group were significant (p<.005). As the maximum gap increased, the percentage of patients hospitalized increased. For consistency and the MPR, significant differences (p<.001) in the percentages of patients with at least one hospitalization were found. Partially compliant patients had significantly higher rates of hospitalization. Patients who were less than 70 percent compliant by the MPR had higher rates of hospitalization than those who were at least 70 percent compliant (22.3 percent and 13.8 percent, respectively, p<.001). Similar results were observed for consistency (24.5 percent compared with 12.8 percent, p<.001). In addition, patients who were identified as being less than 90 percent compliant by the persistence measure had higher rates of hospitalization than those who were identified as being at least 90 percent persistent (25.1 percent and 14.5 percent, respectively, p<.001) (Table 3).
Compliance as a predictor of hospitalization
Having a maximum gap in use of medication that was as small as one to ten days in a one-year period was associated with a significantly increased risk of hospitalization (odds ratio [OR]=1.98) (Table 2). Compared with patients who did not have gaps in medication therapy, patients who had a one- to ten-day maximum gap had almost twice the odds of hospitalization. As the gap increased to 11 to 30 days and more than 30 days, ORs increased to 2.81 and 3.96, respectively.
Logistic regression results for the other three compliance measures were similar to the results for medication gaps. With a 10 percent improvement in consistency, persistence, or the MPR, the odds of hospitalization were lowered by factors of 16 percent, 9 percent, and 23 percent, respectively (p<.01). These models are consistent with the results observed for the maximum medication gap models. Odds of hospitalization were also significantly affected by Medicare eligibility, depending on the compliance variable (Table 4). Medicare eligibility and an increase in age of ten years were significant factors in the models for the MPR, consistence, and persistence.
Discussion
The major finding of this study was the direct relationship between measures of partial compliance and risk of hospitalization: the lower the level of compliance, the greater the risk of hospitalization. We emphasize that this finding is not as intuitive as it might appear. Most published studies showing the link between noncompliance and relapse define noncompliance as persistent and complete discontinuation of antipsychotic medication. From that perspective, the cohort in our analysis was mostly compliant, and even then a relationship was observed between partial compliance and hospitalization risk. This association behaves more like a continuous function than a categorical function—that is, once any degree of partial compliance was indicated by the data, there did not seem to be any low-end cutoff below which hospitalization risk reverted to that of the reference cohort (no indication of partial compliance). This observation held for all four compliance measures. These results suggest that relatively small changes in overall compliance are meaningfully associated with changes in the risk of hospitalization.
Partial compliance seems to be associated with increasing risk of relapse in the long-term treatment of schizophrenia. We found that medication gaps as small as one to ten continuous days in a one-year period were associated with a twofold increase in hospitalization risk. These results are consistent with those of other studies that have demonstrated the negative consequences of partial compliance. Valenstein and colleagues (23) found that patients who had poor compliance were 2.4 times as likely to have inpatient admissions compared with patients who had good compliance. In addition, patients who had poor compliance had a greater total number of psychiatric inpatient days (a mean of 33 days per year) compared with patients who had good compliance (a mean of 24 days per year).
Another study found that partially compliant patients were 49 percent as likely as compliant patients to have an inpatient hospitalization (24). Most recently, Gilmer and coworkers (25), in an analysis of a California Medicaid database, also found that rates of psychiatric hospitalization were lowest among patients who were compliant with their antipsychotic medication regimens (25). These data suggest that patients who do not achieve satisfactory responses to treatment may be experiencing partial compliance problems rather than medication efficacy problems. Steps taken to improve compliance offer an important treatment option that should be considered along with other options, such as combining or switching antipsychotic medications.
Several limitations of this study should be noted. One of the most important limitations is that pharmacy claims data do not provide insights into the reasons for partial compliance. Partial compliance is a behavioral finding with no attributable underlying cause. For example, there is no way to know whether partial compliance in our study sample reflected an intentional decision to stop taking medication or was unintentional, perhaps due to service barriers such as discontinuity of care (26).
Furthermore, the causality of the association between partial compliance and hospitalization has not been established. For example, it is possible that patients who do not fully respond to their medication would be more likely to have medication gaps and that the common shared risk is incomplete medication efficacy (27). We did not attempt a test of temporal contiguity between noncompliance and hospitalization, but such a test could be considered for a future analysis.
The database we used had technical limitations. The use of Medicaid claims data as a proxy for partial compliance relies on minimal coding errors (28,29). Patients' discontinuation of use of Medicaid services may not be reflected in a timely fashion (28); Medicaid patients may not be representative of the population as a whole; and claims data may not include potential confounders, such as medical history and lifestyle factors (28). Calculations for compliance variables are dependent on accurate claims information pertaining to dates, days' supply of medication, the patient's being discharged on the same medication as at admission, and the assumption that there are no other sources of medication supply—for example, medication samples. These latter problems could lead to an overestimation of the association between medication gaps and hospitalization. Although the use of pharmacy claims methodology has the potential advantage of assessment of large cohorts of patients over longer periods, potential sources of error lie in the assumption that claims data are a proxy for partial compliance. Although these factors may have introduced bias into our analysis, the analysis plan minimized sources of differential error between the reference group and the partial compliance group.
Given these factors, however, it should be noted that medical claims data almost certainly overestimate compliance, because claims data can report only whether the prescription was filled, not whether the medication was taken correctly or at all (28). Furthermore, the reference group likely included some patients who could be more accurately described as partially compliant. Thus the actual relationship between partial compliance and hospitalization is likely to be stronger than could be identified from our data. Factors other than partial compliance, many of which would not be captured in a claims database, including social support—or lack thereof—and substance abuse, can affect hospitalization rates.
Conclusions
The results of this study suggest that enhancing compliance across the range of partial compliance behaviors can reduce the risk of hospitalization among patients with schizophrenia. Future studies will explore the impact of partial compliance on other aspects of schizophrenia, such as the duration and severity of illness. Ultimately, enhanced compliance, through improved pharmacologic drug delivery interventions or behavioral interventions, could reduce the toll of relapse and rehospitalization associated with the long-term treatment of schizophrenia.
Acknowledgment
This study was supported by Janssen Pharmaceutica Products, L.P.
Dr. Weiden is affiliated with the neurobiologic disorder service of the State University of New York in Brooklyn. Dr. Kozma is affiliated with the College of Pharmacy of the University of South Carolina in Columbia. Dr. Grogg and Dr. Locklear are with the outcomes research division of Janssen Medical Affairs in Titusville, New Jersey. Send correspondence to Dr. Locklear at Janssen Medical Affairs, L.L.C., 1125 Trenton Harbourton Road, Titusville, New Jersey 08560 (e-mail, [email protected]). A version of this paper was presented at the annual meeting of the College of Psychiatric and Neurologic Pharmacists, held May 1 to 4, 2003, in Charleston, South Carolina.
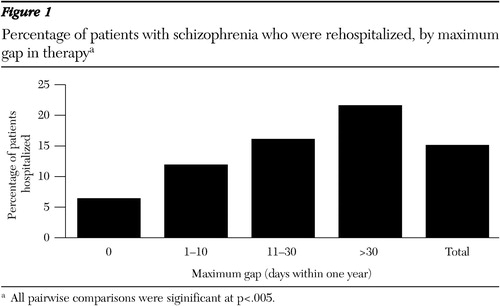
Figure 1. Percentage of patients with schizophrenia who were rehospitalized, by maximum gap in therapya
a All pairwise comparisons were siginificant at p<.005.
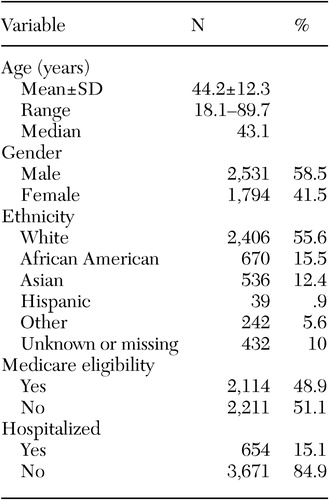 |
Table 1. Characteristics of a sample of 4,325 outpatients for whom antipsychotics were prescribed for treatment of schizophrenia
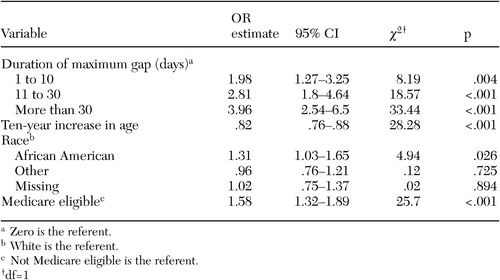 |
Table 2. Odds of hospitalization for a sample of 4,325 outpatients for whom antipsychotics were prescribed for treatment of schizophrenia, based on the maximum gap model
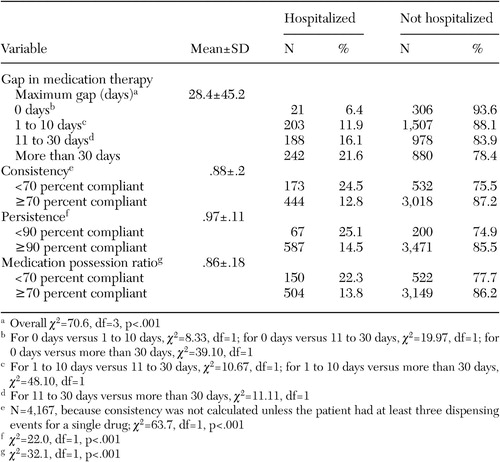 |
Table 3. Compliance and use of prescription medications in a sample of 4,325 outpatients for whom antipsychotics were prescribed for treatment of schizophrenia
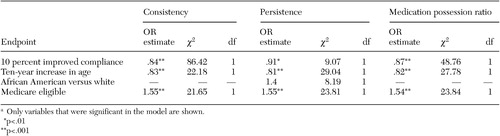 |
Table 4. Odds of hospitalization for a sample of 4,325 outpatients for whom antipsychotics were prescribed for treatment of schizophrenia, based on compliance modelsa
a Only variables that were significant in the model are shown.
1. Olivieri NF, Matsui D, Hermann C, et al: Compliance assessed by the Medication Event Monitoring System. Archives of Disease in Childhood 66:1399–1402, 1991Crossref, Medline, Google Scholar
2. Javaid JI, Janicak PG, Holland D: Blood level monitoring of antipsychotics and antidepressants. Psychiatric Medicine 9:163–187, 1991Medline, Google Scholar
3. Docherty JP, Grogg AL, Kozma C, et al: Antipsychotic maintenance in schizophrenia: partial compliance and clinical outcome. Presented at the annual meeting of the American College of Neuropsychopharmacology, San Juan, Puerto Rico, Dec 8–12, 2002Google Scholar
4. McCombs JS, Nichol MB, Stimmel GL, et al: Use patterns for antipsychotic medications in Medicaid patients with schizophrenia. Journal of Clinical Psychiatry 60(suppl 19):5–11, 1999Medline, Google Scholar
5. Mojtabai R, Lavelle J, Gibson PJ, et al: Gaps in use of antipsychotics after discharge by first-admission patients with schizophrenia, 1989 to 1996. Psychiatric Services 53:337–339, 2002Link, Google Scholar
6. Ayuso-Gutierrez JL, del Rio Vega JM: Factors influencing relapse in the long-term course of schizophrenia. Schizophrenia Research 28:199–206, 1997Crossref, Medline, Google Scholar
7. Marder SR: Facilitating compliance with antipsychotic medication. Journal of Clinical Psychiatry 59(suppl 3):21–25, 1998Medline, Google Scholar
8. Weiden PJ, Zygmunt A: The road back: working with the severely mentally ill. Medication noncompliance in schizophrenia: I. assessment. Journal of Practical Psychiatry and Behavioral Health March:106–110, 1997Google Scholar
9. Fenton WS, Blyler CR, Heinssen RK: Determinants of medication compliance in schizophrenia: empirical and clinical findings. Schizophrenia Bulletin 23:637–651, 1997Crossref, Medline, Google Scholar
10. Robinson D, Woerner MG, Alvir JMJ, et al: Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Archives of General Psychiatry 56:241–247, 1999Crossref, Medline, Google Scholar
11. Choo PW, Rand CS, Inui TS, et al: Validation of patient reports, automated pharmacy records, and pill counts with electronic monitoring of adherence to antihypertensive therapy. Medical Care 37:846–857, 1999Crossref, Medline, Google Scholar
12. Farmer KC: Methods for measuring and monitoring medication regimen adherence in clinical trials and clinical practice. Clinical Therapeutics 21:1074–1090, 1999Crossref, Medline, Google Scholar
13. Maronde RF, Chan LS, Larsen FJ, et al: Underutilization of antihypertensive drugs and associated hospitalization. Medical Care 27:1159–1166, 1989Crossref, Medline, Google Scholar
14. Steiner JF, Koepsell TD, Fihn SD, et al: A general method of compliance assessment using centralized pharmacy records: description and validation. Medical Care 26:814–823, 1988Crossref, Medline, Google Scholar
15. Sclar DA, Skaer TL, Chin A, et al: Utility of a transdermal delivery system for antihypertensive therapy: I. American Journal of Medicine 91(suppl 1A):50S-56S, 1991Google Scholar
16. Sclar DA, Skaer TL, Chin A, et al: Utility of a transdermal delivery system for antihypertensive therapy: II. American Journal of Medicine 91(suppl 1A):57S-60S, 1991Google Scholar
17. Gurwitz JH, Glynn RJ, Monane M, et al: Treatment for glaucoma: adherence by the elderly. American Journal of Public Health 83:711–716, 1993Crossref, Medline, Google Scholar
18. Skaer TL, Sclar DA, Markowski DJ, et al: Effect of value-added utilities on prescription refill compliance and Medicaid health care expenditures: a study of patients with non-insulin-dependent diabetes mellitus. Journal of Clinical Pharmacy and Therapeutics 18:295–299, 1993Crossref, Medline, Google Scholar
19. Monane M, Bohn RL, Gurwitz JH, et al: Non-compliance with congestive heart failure therapy in the elderly. Archives of Internal Medicine 154:433–437, 1994Crossref, Medline, Google Scholar
20. McCombs JS, Nichol MB, Newman CM, et al: The costs of interrupting antihypertensive drug therapy in a Medicaid population. Medical Care 32:214–226, 1994Crossref, Medline, Google Scholar
21. Steiner JF, Prochazka AV: The assessment of refill compliance using pharmacy records: methods, validity, and applications. Journal of Clinical Epidemiology 50:105–116, 1997Crossref, Medline, Google Scholar
22. Hogarty GE: Prevention of relapse in chronic schizophrenic patients. Journal of Clinical Psychiatry 54(3 suppl):18–23, 1993Google Scholar
23. Valenstein M, Copeland LA, Blow FC, et al: Pharmacy data identify poorly adherent patients with schizophrenia at increased risk for admission. Medical Care 40:630–639, 2002Crossref, Medline, Google Scholar
24. Grogg A, Eaddy M, Mauch R, et al: The effects of antipsychotic partial compliance on resource utilization in a schizophrenic and bipolar population. Poster presented at the annual meeting of the New Clinical Drug Evaluation Unit, Boca Raton, Fla, June 12, 2002Google Scholar
25. Gilmer TP, Dolder CR, Lacro JP, et al: Adherence to treatment with antipsychotic medication and health care costs among Medicaid beneficiaries with schizophrenia. American Journal of Psychiatry 161:692–699, 2004Link, Google Scholar
26. Weiden P, Olfson M, Essock S: Medication noncompliance and mental health policy, in Compliance and the Treatment Alliance. Edited by Blackwell B. Amsterdam, Harwood, 1996Google Scholar
27. Weiden P, Olfson M: Cost of relapse in schizophrenia. Schizophrenia Bulletin 21:419–428, 1995Crossref, Medline, Google Scholar
28. Bright RA, Avorn J, Everitt DE: Medicaid data as a resource for epidemiologic studies: strengths and limitations. Journal of Clinical Epidemiology 42:937–945, 1989Crossref, Medline, Google Scholar
29. Iezzoni LI: Assessing quality using administrative data. Annals of Internal Medicine 127(8 pt 2):666–674, 1997Google Scholar



