Improving Treatment Outcomes Includes Increasing the Diversity of the Psychiatric Workforce
As practitioners, we are well aware of the need for new and better treatments for our patients, but we must not overlook others in the population who would benefit from existing treatments and yet, for various reasons, are neglected. New treatment development must be based on the understanding of underlying pathophysiology, which directly depends on new empirical insights into genetic, molecular, cellular, and neurocircuit alterations as they relate to individuals’ symptoms and phenotypic presentations. Ultimately, rigorous clinical trials must be performed in diverse populations to translate more basic discoveries to patients and to determine the efficacy and potential risks of new treatments. At a societal level, the key issues are related to increasing access to psychiatric treatment for populations who are underresourced and to decreasing barriers to mental health care for Black, Indigenous, and people of color (BIPOC) individuals. To make headway, focus needs to be on the effects of structural racism as they play out in relation to mental health care for BIPOC individuals. This issue of the Journal presents articles that address new treatment development, that aim to improve the applicability of current treatments, and that provide recommendations for developing a more diverse psychiatric workforce as part of an effort to overcome barriers to psychiatric care for BIPOC communities.
In relation to new treatment development, articles in this issue explore the use of a progesterone receptor modulator strategy for treating premenstrual dysphoric disorder (PMDD) and the use of a neurosteroid progesterone metabolite for treating postpartum and major depression. Other work focuses on understanding and improving the applicability of current treatments, including the use of electroconvulsive therapy (ECT) for the treatment of mania, the use of antipsychotics for reducing violent behavior in patients with schizophrenia, the general use of contraceptives in female psychiatric patients, and the use of virtual modalities to enable “long distance” psychotherapy treatment. From a health care delivery perspective, we include two pieces that emphasize the imperative of creating greater diversity in the psychiatric workforce and in academic psychiatry departments. This foundational component addresses barriers to treatment for underserved populations and is a necessary step in enhancing mental health care for BIPOC individuals.
Pragmatic Issues Important to Clinical Practice
Drs. Alby Elias and Naveen Thomas from the University of Melbourne and Dr. Harold Sackeim from Columbia University focus on the use of ECT for treatment-resistant mania by comprehensively reviewing the literature and discussing the optimal ECT parameters for treating mania (1). In another article, Dr. Leanne McCloskey from Northwestern University and her colleagues present a primer on the use of contraceptives in women with psychiatric disorders (2). Along with an accompanying editorial (3) by Dr. Kim Yonkers from the University of Massachusetts Medical School, emphasis is placed on the fact that psychiatric illnesses disproportionately affect women, on the negative consequences of unintended pregnancies, on the effects of oral contraceptives on mood, and on the potential drug interactions with oral contraceptives. In relation to the COVID-19 pandemic, we include a very timely review by Dr. John Markowitz from Columbia University and his colleagues that assesses the limited evidence base addressing the efficacy of psychotherapeutic interventions delivered by teletherapy and video therapy. The authors discuss practical issues of direct clinical value related to improving the remote therapy experience for both patients and providers (4).
New Treatment Development
Comasco et al. (5) present data from a clinical trial using ulipristal acetate (UPA), a progesterone receptor modulator acting as an antagonist, to treat women with PMDD. PMDD, thought to be mediated by fluctuations in progesterone and estrogen, is associated with mood and somatic symptoms occurring during the late luteal phase of the menstrual cycle. In general, these symptoms should be consistently present over a number of cycles and also should improve after the onset of menses. In this double-blind study, 95 women with PMDD were randomly assigned to receive either 5 mg/day of UPA or placebo over the course of three 28-day treatment cycles. Of note, UPA is approved for use in the treatment of uterine fibroids. Findings demonstrated that compared with placebo, UPA resulted in significantly greater reductions in mood and psychological symptoms but not in the physical symptoms associated with PMDD. It is noteworthy that UPA was generally well tolerated and that 27.5% of women taking UPA developed amenorrhea. In an editorial (6), Dr. David Rubinow from the University of North Carolina discusses the specifics of this study and also provides an overview focused on PMDD in which he argues that studying PMDD can provide broader insights into other depressive disorders and predict the psychopharmacological utility of hormone receptor modulation.
Along the lines of using hormone-related treatment strategies, and also involving progesterone physiology, the neurosteroid allopregnanolone is a metabolite of progesterone that has received considerable attention for its potential antidepressant and anxiolytic effects. Allopregnanolone, also known as brexanolone, is a GABAA receptor modulator that was recently approved by the U.S. Food and Drug Administration for intravenous use in the treatment of postpartum depression. As extensive work is ongoing in an attempt to develop orally administered neurosteroids for the treatment of depression, Drs. Robert Kleinman from Massachusetts General Hospital and Alan Schatzberg from Stanford University contribute a commentary in this issue on the clinical effects of neurosteroids (7). They provide an update on the development of these compounds and also speculate about the similarities between the effects of neurosteroids and other GABA-ergic agents, such as benzodiazepines. A previously published comprehensive review by Zorumski et al. (8) elaborates on putative mechanisms of action of neurosteroid compounds, including how some of their pharmacological effects differ from those of traditional benzodiazepines.
Conduct Disorder and Treating Violent Behavior in Patients With Schizophrenia
Krakowski et al. (9) focus on the question as to whether a history of conduct disorder is important in understanding violent behavior and its treatment in patients with schizophrenia. To this end, the authors used data from a previously published study (10) that were collected from a double-blind clinical trial that studied 99 predominantly chronically ill, assaultive patients with schizophrenia. This study compared the efficacy of 12 weeks of administration of clozapine, olanzapine, and haloperidol on reducing violent behavior. Results from the original study demonstrated that clozapine was most effective in reducing assaults and that olanzapine was significantly better than haloperidol. In the present article in this issue of the Journal, the authors report that individuals with a history of conduct disorder were approximately two to three times more likely to engage in violent behavior than those without this history. In relation to treatment, the authors found an interaction between having a history of conduct disorder and medication response. While clozapine was more effective than olanzapine and haloperidol in reducing violent behavior in patients with schizophrenia and no history of conduct disorder, having such a history conferred an even greater advantage of clozapine. It is noteworthy that these differential effects of the antipsychotics and their interaction with a history of conduct disorder appeared to be unrelated to the overall efficacy of the drugs in treating the core symptoms of schizophrenia. In their editorial (11), Dr. Margo Faay from University Medical Center Utrecht and Dr. Iris Sommer from University Medical Center Groningen discuss general factors that lead to the risk of violence in patients with psychotic disorders, such as early life trauma, substance abuse, impulsivity, and medication nonadherence. In addition, they discuss the findings from the present study in relation to other studies focused on the prevention of aggressive behavior in patients with psychotic disorders.
The Imperative to Create Greater Diversity in the Psychiatric Workforce and in Academic Psychiatry
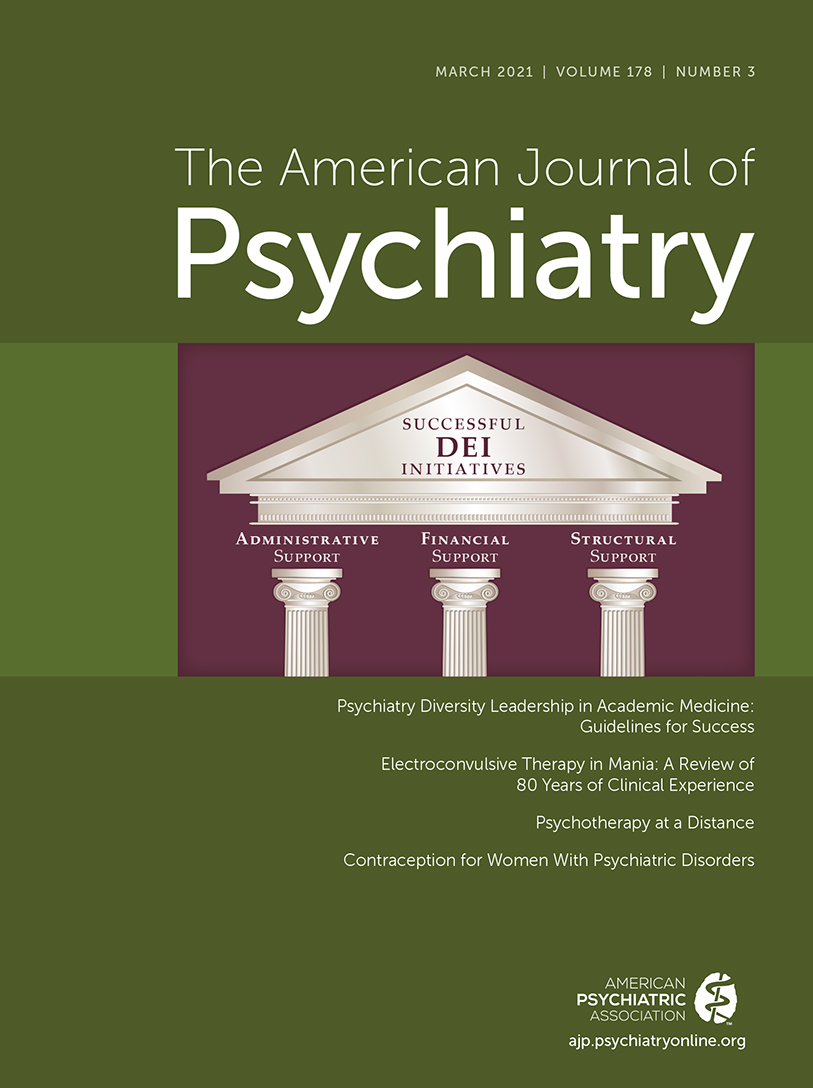
It is essential that we increase the diversity of our psychiatric workforce, and by so doing, we will be moving in the direction of breaking down barriers for BIPOC individuals to seek and receive mental health treatment. To do so, we need to address issues of structural racism within and outside of medicine and psychiatry. Academic settings are critical because they provide the necessary training and research opportunities for future generations of psychiatrists. An important step in increasing diversity in academic settings is to formalize the commitment to change by establishing funded leadership positions with the mandate and resources to enact and prioritize the diversity, equity, and inclusion (DEI) agenda. In this issue of the Journal, we are privileged to have a Clinical Case Conference that presents the dilemma of a Black female faculty member who is asked by her chair to lead the department’s DEI committee—a request that is made without adequate resources and with mixed messages from the chair (12). The authors of this salient article are women involved in leading DEI efforts at their respective universities: Drs. Ayana Jordan, Ruth Shim, Carolyn Rodriguez, Eraka Bath, Jean-Marie Alves-Bradford, Lisa Eyler, Nhi-Ha Trinh, Helena Hansen, and Christina Mangurian. They draw upon their own experiences in surveying the range of salary support that has been provided for their work in this role. Notably, only 56% of these individuals received any support. The authors also discuss the hurdles and barriers that must be overcome to effectively accomplish the departmental goals of attracting, retaining, and promoting women and BIPOC faculty. In an accompanying editorial, Dr. Altha Stewart from the University of Tennessee Health Science Center, and a past president of APA, further elaborates on the historical underpinnings of structural racism in academic medicine (13). She strongly emphasizes the necessity that senior leaders must recognize and address elements of structural racism at their own institutions in conjunction with providing an environment in which BIPOC faculty can flourish.
Summary
To conclude, this issue of the Journal presents papers that address broad issues relevant to improving treatment outcomes, including the development of new therapeutics (ulipristal acetate for PMDD, and neurosteroids for the treatment of depression), updates on and modifications to the use of current treatments (ECT for treatment-resistant mania, the use of contraceptives in women with psychiatric disorders, methods for performing remote psychotherapy, and the superior efficacy of clozapine treatment for violent behavior in patients with schizophrenia), and the need to support the development of a more diverse psychiatric workforce, which will result in greater opportunities to care for BIPOC patients. We are grateful to all of the contributing authors. This is especially the case for the authors who provided the DEI-focused work, as the issues raised in these papers are critical for advancing antiracism efforts in psychiatry—an important publication priority for the Journal (14).
1 : Electroconvulsive therapy in mania: a review of 80 years of clinical experience. Am J Psychiatry 2021; 178:229–239Abstract, Google Scholar
2 : Contraception for women with psychiatric disorders. Am J Psychiatry 2021; 178:247–255Link, Google Scholar
3 : Treatment of psychiatric conditions in pregnancy starts with planning (editorial). Am J Psychiatry 2021; 178:213–214Abstract, Google Scholar
4 : Psychotherapy at a distance. Am J Psychiatry 2021; 178:240–246Link, Google Scholar
5 : Ulipristal acetate for treatment of premenstrual dysphoric disorder: a proof-of-concept randomized controlled trial. Am J Psychiatry 2021; 178:256–265Abstract, Google Scholar
6 : One small step for PMDD, one large step for affective disorders (editorial). Am J Psychiatry 2021; 178:215–217Abstract, Google Scholar
7 : Understanding the clinical effects and mechanisms of action of neurosteroids. Am J Psychiatry 2021; 178:221–223Link, Google Scholar
8 : Neurosteroids as novel antidepressants and anxiolytics: GABA-A receptors and beyond. Neurobiol Stress 2019; 11:
9 : The importance of conduct disorder in the treatment of violence in schizophrenia: efficacy of clozapine compared with olanzapine and haloperidol. Am J Psychiatry 2021; 178:266–274Link, Google Scholar
10 : Atypical antipsychotic agents in the treatment of violent patients with schizophrenia and schizoaffective disorder. Arch Gen Psychiatry 2006; 63:622–629Crossref, Medline, Google Scholar
11 : Risk and prevention of aggression in patients with psychotic disorders (editorial). Am J Psychiatry 2021; 178:218–220Abstract, Google Scholar
12 : Psychiatry diversity leadership in academic medicine: guidelines for success. Am J Psychiatry 2021; 178:224–228Link, Google Scholar
13 : Dismantling structural racism in academic psychiatry to achieve workforce diversity (editorial). Am J Psychiatry 2021; 178:210–212Link, Google Scholar
14 : The American Journal of Psychiatry’s commitment to combat racism, social injustice, and health care inequities (editorial). Am J Psychiatry 2020; 177:791Link, Google Scholar