Randomized Controlled Trial of Outpatient Mentalization-Based Treatment Versus Structured Clinical Management for Borderline Personality Disorder
Abstract
Objective: This randomized controlled trial tested the effectiveness of an 18-month mentalization-based treatment (MBT) approach in an outpatient context against a structured clinical management (SCM) outpatient approach for treatment of borderline personality disorder. Method: Patients (N=134) consecutively referred to a specialist personality disorder treatment center and meeting selection criteria were randomly allocated to MBT or SCM. Eleven mental health professionals equal in years of experience and training served as therapists. Independent evaluators blind to treatment allocation conducted assessments every 6 months. The primary outcome was the occurrence of crisis events, a composite of suicidal and severe self-injurious behaviors and hospitalization. Secondary outcomes included social and interpersonal functioning and self-reported symptoms. Outcome measures, assessed at 6-month intervals, were analyzed using mixed effects logistic regressions for binary data, Poisson regression models for count data, and mixed effects linear growth curve models for self-report variables. Results: Substantial improvements were observed in both conditions across all outcome variables. Patients randomly assigned to MBT showed a steeper decline of both self-reported and clinically significant problems, including suicide attempts and hospitalization. Conclusions: Structured treatments improve outcomes for individuals with borderline personality disorder. A focus on specific psychological processes brings additional benefits to structured clinical support. Mentalization-based treatment is relatively undemanding in terms of training so it may be useful for implementation into general mental health services. Further evaluations by independent research groups are now required.
Borderline personality disorder is characterized by affective instability, impulsivity, interpersonal problems, cognitive distortions, and suicidality (1) . Suicide risk is estimated at up to 10% (2) . Randomized controlled trials have shown psychological treatments to be effective relative to routine care or other therapies (3 – 8) . However, specialist treatment may show superiority to routine care primarily because it is delivered in a structured, protocol-driven manner by better-trained and better-supervised practitioners. Moreover, the requirement of extensive training and stringent monitoring of adherence to standards for most evidence-based therapies are obstacles to comprehensive implementation across mental health services.
For broad dissemination, treatment for borderline personality disorder should be manualized, with minimal training and supervision demands. A randomized design for assessing such a treatment must meet the following minimal criteria: 1) a comparison group also receiving a manualized, structured treatment with equivalent supervision; 2) delivery of both by professionals trained to similar levels; 3) statistical power to detect relatively small differences; and 4) a representative sample of clinically referred patients with a confirmed diagnosis of borderline personality disorder at high risk of suicide. The present trial of mentalization-based treatment (MBT) was initiated to meet these criteria and reports outcomes after 18 months of treatment.
MBT (9 , 10) is a psychodynamic treatment rooted in attachment and cognitive theory. It requires limited training with moderate levels of supervision for implementation by generic mental health professionals. It aims to strengthen patients’ capacity to understand their own and others’ mental states in attachment contexts in order to address their difficulties with affect, impulse regulation, and interpersonal functioning, which act as triggers for acts of suicide and self-harm (11) .
MBT delivered by generic mental health professionals in the context of a partial hospital program was cost-effective and superior to treatment as usual over a period of 36 months (12 – 14) . Treatment effects remained 5 years after all index treatment had ceased (14) . The present pragmatic randomized superiority trial investigated MBT as a treatment for suicidal and self-harming patients with borderline personality disorder when delivered in an outpatient context by nonspecialist mental health practitioners at a publicly funded clinical service. To control for the nonspecific benefits of a structured treatment, the comparison group also received a protocol-driven treatment, structured clinical management (SCM), in an outpatient context representing best current clinical practice. Practitioners received equivalent supervision.
Method
The study was designed to test the hypothesis that patients receiving outpatient MBT would be more likely to desist from parasuicidal behavior (self-harm and suicide attempts) and require less hospitalization than those offered an outpatient structured protocol of similar intensity but excluding MBT components.
Protocol and Design
Patients referred to St Ann’s Hospital’s specialist personality disorder service were randomly assigned to one of two active treatment arms and assessed at entry and over the course of an 18-month treatment at 6, 12, and 18 months. The study was approved by Barnet Enfield and Haringey Local Research and Ethics Committee and conducted at the Halliwick personality disorder service and in a community outpatient facility. Patients were provided with written information and consented only after complete description of the study. All treatments were funded under the NHS. Participants were not paid.
Participants
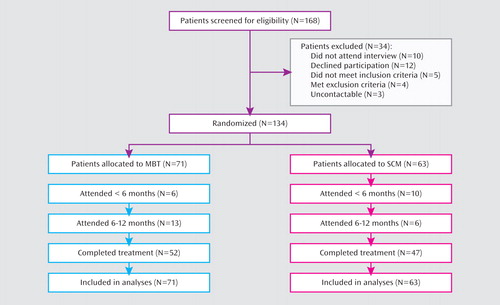
Patients (N=168) were recruited from consecutive referrals for personality disorder treatment from clinical services between January 2003 and February 2006. All participants were assessed using the Structured Clinical Interview for DSM-IV (SCID-I and SCID-II). Inclusion criteria were 1) diagnosis of borderline personality disorder, 2) suicide attempt or episode of life-threatening self-harm within last 6 months, and 3) age 18–65. Exclusion criteria were kept to a minimum. Patients were excluded if they currently 1) were in long-term psychotherapeutic treatment, 2) met DSM-IV criteria for psychotic disorder or bipolar I disorder, 3) had opiate dependence requiring specialist treatment, or 4) had mental impairment or evidence of organic brain disorder. Current psychiatric inpatient treatment, temporary residence, drug/alcohol misuse, and comorbid personality disorder were not exclusion criteria. One hundred fifty-eight patients attended for interview. Of these, five did not have borderline personality disorder, two had opiate dependence, one had bipolar I disorder, one a psychotic disorder, and three were uncontactable after the diagnostic interview. Of the 146 patients enrolled, 12 refused randomization leaving 134 entering the two outpatient treatment programs (MBT=71, SCM=63). Figure 1 shows the flow of participants through the trial. All patients were offered 18 months of therapy, approximately 140 sessions, and about 75% of the subjects across the two groups met our criteria for completion (at least 70 sessions attended over the first year). There was no difference in the distribution of completer categories across the groups (χ 2 =1.87, df=2, p=0.18).
a Early (before 6 months) “dropouts” attended less than a quarter of sessions and late dropouts attended less than half available session over approximately a year of treatment, the remainder are considered completers.
Randomization
Randomization followed consent, enrollment, and baseline assessment by a research assistant at St Ann’s Hospital. Treatment allocation was made offsite via telephone randomization using a stochastic minimization program (MINIM) balancing for age (blocked as 18–25, 26–30, >30 years), gender, and presence of antisocial personality disorder. A study psychiatrist informed patients of their assignment.
Interventions
Both treatments were conducted within a structured framework following principles outlined elsewhere (9) and recently summarized in NICE Guidance (15) . This included crisis contact and crisis plans, pharmacotherapy, general psychiatric review, and written information about treatment. Crisis plans were developed collaboratively within each treatment team for all patients. MBT therapists focused on helping patients reinstate mentalizing during a crisis via telephone contact. SCM therapists focused on support and problem solving. Efforts were made to keep all patients in treatment if they missed appointments.
MBT is manualized, consisting of 18 months of weekly combined individual and group psychotherapy provided by two different therapists (10) . An outpatient SCM protocol was developed through the Barnet Enfield and Haringey Mental Health NHS Trust (“Structured Clinical Management of Borderline Personality Disorder: Best Clinical Practice,” available from A. Bateman upon request) to reflect best generic practice for borderline personality disorder offered by nonspecialist practitioners within U.K. psychiatric services. Regular individual and group sessions were offered with appointments every 3 months for psychiatric review. Therapy was based on a counseling model closest to a supportive approach with case management, advocacy support, and problem-oriented psychotherapeutic interventions. Information about treatment integrity, therapists, and power calculations is available in supplementary data accompanying the online version of this article.
Medication
Patients were prescribed medication by a member of the treatment team (MBT condition) or their consultant psychiatrist (SCM condition). All patients were offered medication reviews every 3 months. All prescribers were asked to adhere to APA guidelines (16) . Prescribing patterns and dosage were monitored by review of medical records every 6 months. We report on antidepressant, antipsychotic, mood stabilizer, and minor tranquillizer use.
Outcomes
Primary outcome declared prior to the study was the proportion of each group without severe parasuicidal behavior as indicated by 1) suicide attempt, 2) life-threatening self-harm, or 3) hospital admission. Hospital admission was included because patients are primarily offered inpatient care in anticipation of suicide attempts and severe self-harm. Incidence of suicidal and severe self-injurious behaviors and episodes of hospitalization, assessed in 6-month periods both in terms of counts and as dichotomous data (present or absent in each period) was used to indicate the severity of life-threatening parasuicidal behavior taken at baseline for the 6 months prior to treatment and for each 6-month period until the end of treatment at 18 months. Count data were analyzed using a mixed effects Poisson regression model; for binary data a mixed effects logistic regression model was used. Secondary outcomes were independently rated Global Assessment of Functioning (GAF) scores at the beginning and end of treatment and self-reported psychiatric symptoms, social and interpersonal functioning, and medication use assessed at baseline and at 6-month intervals until the end of treatment at 18 months.
The criteria for suicidal acts are described in a previous report (7) . Hospital admission statistics were based on local computerized medical records. Patients’ subjective experience of symptoms was measured using the SCL-90-R (17) , and depression was assessed by using the Beck Depression Inventory (18) . Social adjustment and interpersonal functioning were measured using the modified Social Adjustment Scale–self-report (19) and the Inventory of Interpersonal Problems–circumflex version (20 , 21) . The instruments provide an assessment of an individual’s work, spare time activities, and family life as well as difficulties with interpersonal functioning.
Global functioning was rated at the beginning and end of treatment using the Global Assessment of Functioning (GAF), which has been found to show less improvement in naturalistic follow-along studies than diagnostic symptoms (22) . Assessors were blind to treatment group, and their assessment was compared with clinician ratings to indicate reliability.
Statistical Analysis
All results were analyzed using an intention-to-treat analysis based on treatment assignment. The mean number of scheduled clinical meetings attended was 92 (SD=38) for MBT and 84 (SD=40) for SCM, a nonsignificant difference. A total of 99 patients (74%) attended at least 50% of treatment sessions offered (MBT=52 [73%]; SCM=47 [75%]).
Adequacy of randomization was assessed by conducting between-group comparisons of baseline characteristics on all measures using chi-square statistics for dichotomous variables and Kruskal-Wallis statistics and t tests for count and interval data, respectively. Most of the clinical outcome measures were not normally distributed and were relatively low-frequency events. The primary and secondary outcome measures assessed at 6-month intervals were analyzed using mixed effects logistic regressions for binary data, Poisson regression models for count data, and mixed effects linear growth curve models for normally distributed variables (23) . The coefficients are odds ratios (OR) for binary data, incidence rate ratios (IRR) for count data (predicted values are natural logarithms of relative risk), and slopes for continuous variables using robust standard errors to provide conservative estimates of statistical significance. Mixed effects models and general estimating equations use all available data. Missing values were not a significant problem in the analysis of the data set (<5%). Covariates that could moderate or account for some of the group differences on the basis of past literature (e.g., Cluster A, antisocial personality, gender, age) were included in the models, and the results were compared with models without the covariates. None of the covariates we tested yielded a significant improvement on any of the models. SPSS version 16 and Stata version 10 were used throughout.
Results
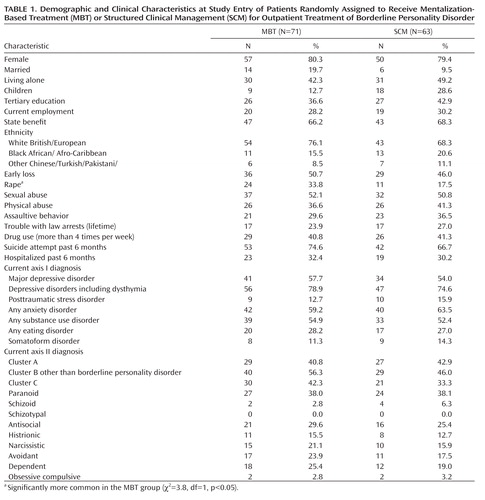
Analyses of the primary and secondary outcomes were based on the intent-to-treat sample of 134 patients. No significant differences on any diagnostic or clinical variable were found in the 12 patients who declined participation, except that those electing to join the trial were more likely to have been diagnosed with a serious alcohol use problem (p<0.005). Patients assigned to MBT and SCM were similar in terms of age (mean=31.3 [SD=7.6] and 30.9 [SD=7.9] years, respectively), number of serious self-harm episodes (mean=4.1 [SD=4.9] and 3.8 [SD=3.7]), days of hospitalization in the prior 6 months (mean=5.5 [SD=11.6] and 6.0 [SD=12.4]), or number of axis I diagnoses (mean=2.8 [SD=1.3] and 2.8 [SD=1.3]) or axis II diagnoses (mean=2.4 [SD=1.1] and 2.3 [SD=1.0]). Other pretreatment demographic characteristics are summarized in Table 1 . The two treatment groups did not differ significantly on any pretreatment characteristic or clinical or self-report measure except reported rape, which was more common in the MBT group ( Table 1 ).
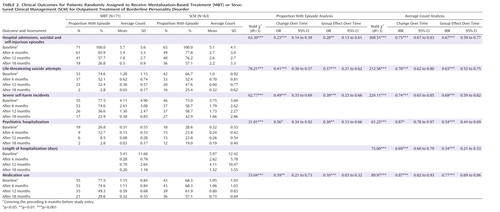
All primary and secondary outcome variables are shown in Table 2 and Table 3 . Although patients in both groups made statistically significant improvements, MBT was associated with greater improvements than SCM for most outcomes.
Primary Outcomes
Six-month periods free of suicidal behaviors, severe self-injurious behaviors, and hospitalization improved from 0% to 43% in the SCM group and to 73% in the MBT group (χ 2 =11.5, df=1, p<0.0007; relative risk=1.7, 95% CI=1.23–2.35). The mixed effects logistic regressions including all four time-points indicated that the number of 6-month periods free of risk behavior increased in patients assigned to MBT more than for patients in the SCM group (odds ratio=0.28; 95% CI=0.13–0.61; p<0.002). However, differences only became statistically significant after 12 months of treatment (χ 2 =4.3, df=1, p<0.04; relative risk=1.8, 95% CI=1.05–3.0). Analysis of the count variable (number of episodes of hospital admissions, suicide attempts, and severe self-injuries) also indicated substantial declines in both groups but a substantially greater reduction in the MBT than the SCM group (d=0.73, 95% CI=0.34–1.13 and see Table 2 ). Figure 2 displays the primary outcome variable estimates derived from the generalized estimating equation models used to assess the treatment effect and illustrates the rate of reduction of parasuicidal behaviors in the two groups.
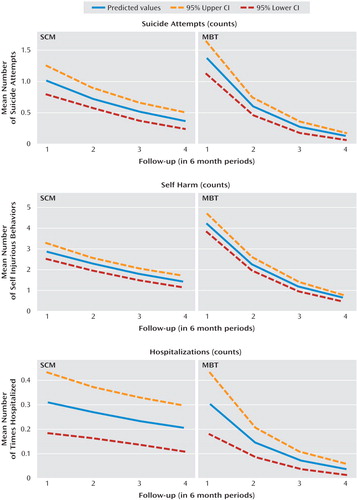
a Follow-up assessment 1 covered the 6 months before the intervention. Assessments 2, 3, and 4 occurred at 6, 12, and 18 months, respectively, and covered the preceding 6-month period. Estimates were derived from the generalized estimating equation models used to assess the treatment effect.
Suicidal behavior
The count and dichotomous data were relatively consistent, showing reduced suicidal behavior in both groups. The rate of improvement was significantly greater in the MBT group both in terms of any suicide attempt and the count data associated with it ( Table 2 ). In the last 6 months of treatment only two patients in the MBT group compared with 16 in the SCM group made a suicide attempt (χ 2 =12.8, p<0.0004; relative risk=0.11, 95% CI=0.02–0.46). However, differences between groups only became marked in the last 6 months of treatment; at 12 months, groups were not significantly different (χ 2 =2.6, p<0.10; relative risk=0.68, 95% CI=0.44–1.04). The end-of-treatment difference between the groups suggested a medium effect size (d=0.65, 95% CI=0.58–0.73).
Self-harm behavior
Analyses of the frequency of self-harm behaviors showed a significantly steeper reduction in the MBT group compared with SCM ( Table 2 ). During the 6 months before end of treatment fewer patients in the MBT group severely self-harmed (24% versus 43%, χ 2 =4.6, p<0.05; relative risk=0.55, 95% CI=0.33–0.92). However, during the first 6 months of treatment, comparison of the proportion of individuals manifesting self-injurious behavior favored the SCM group (75% versus 59%, χ 2 =3.1, p<0.08; relative risk=1.27, 95% CI=0.99–1.63). From 6 to 18 months the proportion of these patients in the MBT group who self-harmed showed a steeper decline when compared with the SCM group. Figure 2 shows that the more consistent reduction in the counts of self-injurious behavior and the difference in incidence rate ratios favoring MBT was highly statistically significant ( Table 2 ) as well as yielding a moderate effect size (d=0.62, 95% CI=0.28–0.97).
Hospitalizations
Table 2 also displays information about hospitalization in the two groups. Before treatment about 25% of each group had had at least one hospital admission. During the first 6 months of treatment patients in the MBT group had significantly fewer days in hospital (Kruskal-Wallis χ 2 =4.25, p<0.04), and the difference increased by 12 months (Kruskal-Wallis χ 2 =6.54, p<0.02) and 18 months (Kruskal-Wallis χ 2 =9.01, p<0.003). The decline in number of admissions over the whole period of treatment was significantly steeper in the MBT group ( Table 2 ). The number of patients hospitalized was dramatically reduced in the MBT group relative to the SCM group ( Table 2 ) and was markedly lower in the MBT group in the last 6 months of treatment (χ 2 =7.7, p<0.005; relative risk=0.14, 95% CI=0.3–0.64).
Secondary Outcomes
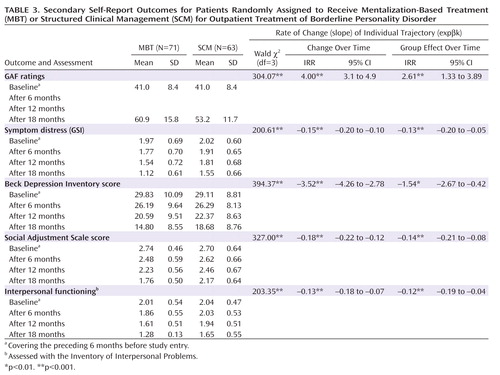
Secondary outcomes included GAF ratings and self-ratings of symptom severity, depression, interpersonal functioning, and social adjustment. All were measured by scales producing continuous data and analyzed using mixed effects linear regression models. Table 3 includes the mean ratings on GAF scale. These increased substantially for both groups over the 18-month period from 41 (95% CI=39.7–42.7) to 57 (95% CI=54.9–60.0) (t=15.5, df=125, p<0.0001) but the increase was rated as greater in the MBT group ( Table 3 ). Table 3 also shows marked improvement on all self-rated measures for both groups. This was particularly notable for symptoms of depression and social adjustment. The slope of decline in self-reported symptoms and relationship and social adjustment problems was significantly greater in the MBT group across all four measures. The size of difference between the two groups at the end of treatment was substantial for reduction in interpersonal distress (d=0.95, 95% CI=0.59–1.3), moderate for social adjustment problems (d=0.72, 95% CI=0.37–1.06) and symptom distress (d=0.67, 95% CI=0.33–1.02), and more modest for depression (d=0.45, 95% CI=0.10–0.79).
In line with the improvements in symptoms, use of medication reduced significantly in both groups. The proportion of patients not receiving medication increased from 27% to 57%. The mixed effects logistic regression confirmed that this increase was greater for the MBT group ( Table 2 ). Counting the number of classes of psychotropic medication also showed a decline across both groups with the incidence rate ratio suggesting a significant difference in favor of the MBT group ( Table 2 ). The number of individuals receiving two or more different classes of medication substantially reduced in both groups from 30% at the beginning of treatment to 8% at the end of treatment.
Discussion
This study suggests that structured, integrated psychological and psychiatric treatment offering coordinated clinical management recommended by NICE (15) significantly benefits patients with borderline personality disorder. Both conditions were associated with substantially reduced suicidality, self-harm, and hospitalization and improvement on measures of symptoms and social and interpersonal functioning by the end of treatment. The rate of improvement in both groups was higher than spontaneous remission of symptoms of borderline personality disorder (24 , 25) .
Like Giesen-Bloo (4) , we found a difference between two active treatments but over a shorter period and unrelated to amount of therapist contact. The same pattern of group differences holds for intent-to-treat analyses reported here and completers, restricted to those who attended at least 70 sessions in the first 12 months of treatment. Outpatient MBT was superior to outpatient SCM in terms of effects on suicide attempts, severe incidents of self-harm, and on self-reported measures, suggesting that psychotherapy focusing on psychological functions relevant to symptoms of borderline personality disorder (e.g., ability to reflect on mental states of oneself and others) can enhance a structured, integrated treatment program providing generic psychological support. This concurs with earlier findings that specific treatment was more effective than supportive psychotherapy (5) or treatment by expert (3) .
The different time courses of change between treatments may be due to their contrasting focus—SCM on problem behaviors and MBT on states of mind and understanding causes and consequences of emotional states and social and interpersonal interactions. Thus, self-harm improved more slowly with MBT than with SCM—albeit with an ultimately more impressive reduction—but mood, interpersonal measures, and social adjustment improved more rapidly. We attribute the early reduction of hospitalization in the MBT group to more effective crisis management further indicated by better attendance figures.
The study has a number of strengths in relation to previous investigations of psychosocial treatment for borderline personality disorder. First, the sample is a relatively unselected group of clinically referred patients with a confirmed diagnosis of borderline personality disorder at high risk, and included comorbid antisocial personality disorder which did not reduce treatment response. Second, the superiority of MBT indicates that sustained emphasis on a patient’s way of thinking or behaving in a consistent manner is more helpful than generic psychotherapy. Perhaps therapists are supported by a primary theoretical model onto which they consistently map clinical and interactional data. Without this, therapy may become incoherent and therapists responsive rather than proactive. Since we do not report measures of mentalization as a mediator variable, we make no claim for this demonstration but affirm that a specific focus using a coherent theoretical model is likely to improve outcomes. Third, the superiority of the specific approach cannot be attributed to differences in therapists’ experience and sophistication. Both treatments were delivered by professionals trained to the same level and with similar experience as in Linehan’s trial of dialectical behavior therapy (3) . In this respect MBT may have advantages. MBT has minimal training and supervision demands because it uses a commonsense view of the mind and incorporates generic ideas from different models of psychotherapy, blending them into a healthy ecumenism relevant to borderline personality disorder (26) . Therapists therefore have to modify their practice rather than learn new techniques. Current results suggest that reasonable outcomes may be achievable within the framework of mental health services without lengthy specialist training. This supports the general utility of MBT and contraindicates the adoption of generic approaches or premature exclusive adoption of any one therapeutic model. The outcomes literature indicates a choice of evidence-based approaches; selection is perhaps best guided by pragmatic considerations such as skill-set and competencies of available personnel and accessibility of appropriate training.
This investigation has some limitations. Longer-term follow-up is needed to determine whether differential effects are maintained and to establish whether patients no longer meet criteria for formal diagnosis at least 36 months posttreatment. Change in diagnosis after 18 months is not a compelling indicator of continued dysfunction. We are collecting diagnostic data at long-term follow-up. In the current study we were interested in the rate of improvement on robust clinically significant indicators that are currently more central in the planning of services than diagnostic status. There is a risk of bias when the developers of a method are central in designing and delivering its evaluation (27) ; replication by independent groups is urgently required. The failure to monitor the predicted mechanism of change is a serious flaw in the design (28) although this may be remedied in subsequent studies of the process material collected as part of this evaluation.
Future studies should explore not only the relative efficacy of different evidence-based approaches to psychotherapy for borderline personality disorder and potential differences in patient-based moderators of outcome but also the training necessary to deliver the intervention effectively along with economic considerations related to dissemination and maintenance of competencies within the workforce.
1. Lieb K, Zanarini MC, Schmahl C, Linehan MM, Bohus M: Borderline personality disorder. Lancet 2004; 364:453–461Google Scholar
2. Schneider B, Schnabel A, Wetterling T, Bartusch B, Weber B, Georgi K: How do personality disorders modify suicide risk? J Pers Disord 2008; 22:233–245Google Scholar
3. Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, Korslund KE, Tutek DA, Reynolds SK, Lindenboim N: Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry 2006; 63:757–766Google Scholar
4. Giesen-Bloo J, van Dyck R, Spinhoven P, van Tilburg W, Dirksen C, van Asselt T, Kremers I, Nadort M, Arntz A: Outpatient psychotherapy for borderline personality disorder; randomized trial of schema-focused therapy vs transference focused therapy. Arch Gen Psychiatry 2006; 63:649–658Google Scholar
5. Clarkin JF, Levy KN, Lenzenweger MF, Kernberg O: Evaluating three treatments for borderline personality disorder. Am J Psychiatry 2007; 164:922–928Google Scholar
6. Davidson K, Norrie J, Tyrer P, Gumley A, Tata P, Murray H, Palmer S: The effectiveness of cognitive behavior therapy for borderline personality disorder: results from the borderline personality disorder study of cognitive therapy (BOSCOT) trial. J Pers Disord 2006; 20:450–465Google Scholar
7. Bateman A, Fonagy P: Effectiveness of partial hospitalization in the treatment of borderline personality disorder: a randomized controlled trial. Am J Psychiatry 1999; 156:1563–1569Google Scholar
8. Blum N, St John D, Pfohl B, Stuart S, McCormick B, Allen J, Arndt S, Black DW: Systems Training for Emotional Predictability and Problem Solving (STEPPS) for outpatients with borderline personality disorder: a randomized controlled trial and 1-year follow-up. Am J Psychiatry 2008; 165:468–478Google Scholar
9. Bateman A, Fonagy P: Psychotherapy for Borderline Personality Disorder: Mentalisation Based Treatment. Oxford, Oxford University Press, 2004Google Scholar
10. Bateman A, Fonagy P: Mentalization Based Treatment: A Practical Guide. Oxford, Oxford University Press, 2006Google Scholar
11. Linehan MM: Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York, Guilford, 1993Google Scholar
12. Bateman A, Fonagy P: Treatment of borderline personality disorder with psychoanalytically oriented partial hospitalization: an 18-month follow-up. Am J Psychiatry 2001; 158:36–42Google Scholar
13. Bateman A, Fonagy P: Health service utilization costs for borderline personality disorder patients treated with psychoanalytically oriented partial hospitalization versus general psychiatric care. Am J Psychiatry 2003; 160:169–171Google Scholar
14. Bateman A, Fonagy P: 8-year follow-up of patients treated for borderline personality disorder: mentalization-based treatment versus treatment as usual. Am J Psychiatry 2008; 165:631–638Google Scholar
15. NICE: Borderline Personality Disorder: treatment and management. http://www.nice.org.uk/Guidance/CG78/NiceGuidance/pdf/English 2009Google Scholar
16. American Psychiatric Association: Practice Guideline for the Treatment of Patients With Borderline Personality Disorder. Am J Psychiatry 2001; 158(Oct suppl)Google Scholar
17. Derogatis LR: SCL-90-R: Administration, Scoring, and Procedures Manual, II. Towson, Md, Clinical Psychometric Research, 1983Google Scholar
18. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J: An inventory for measuring depression. Arch Gen Psychiatry 1961; 4:561–571Google Scholar
19. Weissman MM, Bothwell S: Assessment of social adjustment by patient self-report. Arch Gen Psychiatry 1976; 33:1111–1115Google Scholar
20. Horowitz LM, Rosenberg SE, Baer BA, Ureno G, Villasenor VS: Inventory of Interpersonal Problems: psychometric properties and clinical applications. J Consult Clin Psychol 1988; 56:885–892Google Scholar
21. Alden LE, Wiggins JS, Pincus AL: Construction of circumflex scales for the Inventory of Interpersonal Problems. J Personality Assessment 1990; 55:521–536Google Scholar
22. Gunderson JG, Daversa MT, Grilo CM, McGlashan TH, Zanarini MC, Shea MT, Skodol AE, Yen S, Sanislow CA, Bender DS, Dyck IR, Morey LC, Stout RL: Predictors of 2-year outcome for patients with borderline personality disorder. Am J Psychiatry 2006; 163:822–826Google Scholar
23. Rabe-Hesketh S, Skrondal A: Multilevel and longitudinal modeling using STATA. College Station, Tex, Stata Press, 2008Google Scholar
24. Zanarini MC, Frankenburg FR, Hennen J, Silk KR: The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder. Am J Psychiatry 2003; 160:274–283Google Scholar
25. Skodol AE, Pagano ME, Bender DS, Shea MT, Gunderson JG, Yen S, Stout RL, Morey LC, Sanislow CA, Grilo CM, Zanarini MC, McGlashan TH: Stability of functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder over two years. Psychol Med 2005; 35:443–451Google Scholar
26. Stone M: Perspective: pitfalls in the psychotherapy of borderline personality or the triumph of faith over fact. J Pers Disord 2009; 23:3–5Google Scholar
27. Luborsky L, Diguer L, Seligman DA, Rosenthal R, Krause ED, Johnson S, Halperin G, Bishop M, Berman JS, Schweizer E: The researcher’s own therapy allegiances: a ‘wild card’ in comparisons of treatment efficacy. Clin Psychol Science and Practice 1999; 6:95–106Google Scholar
28. Kazdin AE: Mediators and mechanisms of change in psychotherapy research. Annu Rev Clin Psychol 2007; 3:1–27Google Scholar