The Effects of Treatment-Resistant Depression and First-Ever Depression on Mortality Following Acute Coronary Syndrome: Interactive or Independent?
To the Editor: Drs. Carney and Freedland (1) presented a fascinating review on treatment-resistant depression and mortality following acute coronary syndrome. As a possible mechanism explaining the association between treatment-resistant depression and mortality in acute coronary syndrome patients, the authors suggested the presence of first-ever depressive episodes, which are associated with both treatment resistance and increased risk of cardiac events.
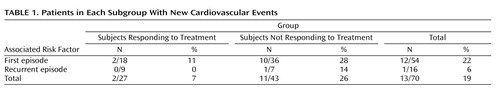
We therefore explored the association between treatment-resistant depression, first-ever depression, and cardiovascular prognosis using data from the Myocardial INfarction and Depression Intervention Trial (MIND-IT), a multi-center randomized controlled trial on the treatment of post-acute coronary syndrome depression. We previously reported (2) , using Cox regression analysis, that patients who did not respond to treatment had an unadjusted hazard ratio of 4.89 (95% confidence interval [CI]=1.08–22.10) for new cardiovascular events relative to patients who responded to treatment. Testing the hypothesis of Drs. Carney and Freedland, we adjusted for the presence of first episodes. However, adjusting hardly affected the association (hazard ratio=4.42; 95% CI=0.97–20.10), which is indicative of no support for the hypothesis. An explanation may be that in our sample first episodes were not associated with new cardiovascular events or treatment resistance. However, they are associated with both new cardiovascular events (hazard ratio=4.12 [95% CI=0.53–31.77]) and with treatment resistance (odds ratio=2.57 [95% CI=0.82–8.03]). The number of patients in each subgroup and their associated risk of cardiac events are shown in Table 1 .
Our tentative conclusion is that first depressive episodes and treatment resistance are two independent risk factors for worse outcomes that do not interact but add up independently. Our results do not support the hypothesis that first depressive episodes would underlie the association between treatment-resistant depression and negative cardiac outcomes. Since cell numbers in our study were very low, however, we feel that caution is warranted and no firm conclusions can yet be determined.
We agree with Drs. Carney and Freedland that treatment-resistant depression is likely a marker of an underlying cardiac risk factor associated with treatment resistance in patients with coronary heart disease and that researchers should investigate this factor. One possible risk factor that is often overlooked is treatment nonadherence, which is associated with both depression and cardiac prognosis. Treatment nonadherence is one of the reasons for treatment resistance in depressed patients, and it is likely that a patient who is nonadherent to antidepressant treatment is also nonadherent to cardiac aftercare.
1. Carney RM, Freedland KE: Treatment-resistant depression and mortality after acute coronary syndrome. Am J Psychiatry 2009; 166:410–417Google Scholar
2. de Jonge P, Honig A, van Melle JP, Schene AH, Kuyper AM, Tulner D, Schins A, Ormel J: Nonresponse to treatment for depression following myocardial infarction: association with subsequent cardiac events. Am J Psychiatry 2007; 164:1371–1378Google Scholar