Overgeneralization of Conditioned Fear as a Pathogenic Marker of Panic Disorder
Abstract
Objective
Classical conditioning features prominently in many etiological accounts of panic disorder. According to such accounts, neutral conditioned stimuli present during panic attacks acquire panicogenic properties. Conditioned stimuli triggering panic symptoms are not limited to the original conditioned stimuli but are thought to generalize to stimuli resembling those co-occurring with panic, resulting in the proliferation of panic cues. The authors conducted a laboratory-based assessment of this potential correlate of panic disorder by testing the degree to which panic patients and healthy subjects manifest generalization of conditioned fear.
Method
Nineteen patients with a DSM-IV-TR diagnosis of panic disorder and 19 healthy comparison subjects were recruited for the study. The fear-generalization paradigm consisted of 10 rings of graded size presented on a computer monitor; one extreme size was a conditioned danger cue, the other extreme a conditioned safety cue, and the eight rings of intermediary size created a continuum of similarity from one extreme to the other. Generalization was assessed by conditioned fear potentiating of the startle blink reflex as measured with electromyography (EMG).
Results
Panic patients displayed stronger conditioned generalization than comparison subjects, as reflected by startle EMG. Conditioned fear in panic patients generalized to rings with up to three units of dissimilarity to the conditioned danger cue, whereas generalization in comparison subjects was restricted to rings with only one unit of dissimilarity.
Conclusions
The findings demonstrate a marked proclivity toward fear overgeneralization in panic disorder and provide a methodology for laboratory-based investigations of this central, yet understudied, conditioning correlate of panic. Given the putative molecular basis of fear conditioning, these results may have implications for novel treatments and prevention in panic disorder.
Many etiological accounts of panic disorder implicate classical conditioning as a central pathogen (1–4). According to these accounts, neutral conditioned stimuli that are present during an aversive panic attack acquire the capacity to trigger anticipatory anxiety for, or an actual occurrence of, panic attacks through classical conditioning (1, 2, 5). Conditioned stimuli contributing to the onset and maintenance of panic disorder are thought to extend to exteroceptive and interoceptive stimulus events resembling those co-occurring with panic (1, 2, 6) via stimulus generalization—a learning mechanism whereby fear responses extend to a range of stimuli resembling the original conditioned stimuli (7). For example, conditioned fear to the environment where a panic attack occurs (e.g., a specific shopping mall) might transfer, or generalize, to similar environments (e.g., all shopping malls). Similarly, fear associated with the autonomic constituents of panic may generalize to everyday activities that elicit similar changes in physiology (e.g., exercise or climbing stairs). Whether exteroceptive or interoceptive, generalization is thought to allow an initial panic attack to evolve into panic disorder through the proliferation of cues that trigger anticipatory anxiety. From this perspective, panic disorder involves a proclivity toward overgeneralization (8).
Despite the intuitive appeal of these ideas, few studies have systematically examined conditioned fear generalization in humans (9), and none has examined such processes in panic disorder. Systematic tests of generalization involve examination of conditioned fear responses to both a conditioned danger cue and generalization stimuli parametrically varying in similarity to the conditioned danger cue. Such tests generate generalization gradients—or slopes—in which the strongest fear response is to the conditioned danger cue and decreasing levels of fear occur in response to generalization stimuli of decreasing similarity to the danger cue (see reference 10, for example). Notably, generalization gradients in both intact animals and healthy humans are characterized by steep quadratic slopes reflecting precipitous declines in conditioned responding to the closest two or three approximations of the conditioned danger cue, followed by a leveling off in response to the remaining generalization stimuli (9–12).
This study was initiated to assess the degree to which generalization gradients in panic disorder deviate from the pattern found in healthy subjects, with the prediction of less quadratic and more gradual declines in conditioned fear in patients with panic disorder as the presented generalization stimulus differentiates from the conditioned danger cue. We tested this prediction using a novel paradigm (9) that generates both self-report and physiological measures of generalization. The paradigm relies on fear-potentiated startle—the amygdala-dependent, fear-related, cross-species enhancement of the startle reflex (13–15).
Method
Participants
Nineteen patients with a current DSM-IV-TR diagnosis of panic disorder and 19 healthy comparison subjects were recruited for the study. The demographic and clinical characteristics of the two groups are provided in Table 1. There were no between-group differences in gender or age.
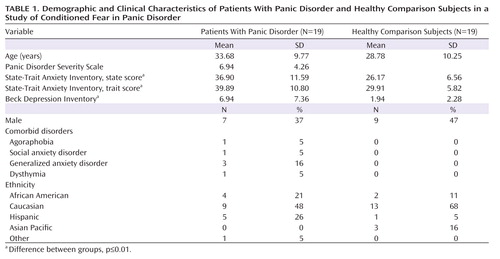 |
Diagnostic exclusion criteria for patients with panic disorder included current major depressive disorder; history of alcohol or substance abuse or dependence (other than nicotine) within 6 months of study start; and current or past history of bipolar depression, psychosis, or delusional disorders. Comparison subjects had to be free of any current or past axis I psychopathology as assessed by the Structured Clinical Interview for DSM-IV-TR, Patient Edition (SCID; 16). Additionally, exclusion criteria that applied to all participants were use of psychopharmacological medication or other drugs that alter CNS function within 2 weeks of testing or use of fluoxetine within 6 weeks of testing; current use of illicit drugs, as determined by the SCID and confirmed with a urine test; pregnancy; or medical conditions or treatment for conditions that would interfere with the objectives of the study as determined by a staff physician.
anic diagnoses were determined by the SCID, administered by one of four staff psychologists (interrater reliability, kappa=0.76). All patients were also independently assessed by a senior psychiatrist (D.S.P.) to confirm the SCID diagnosis. Finally, the Panic Disorder Severity Scale (17) was completed for patients with panic disorder to provide a continuous measure of symptom severity. At study outset, participants received a description of the experimental procedures and gave written informed consent, as approved by the National Institute of Mental Health institutional review board.
Physiological Apparatus
Stimulation and recording were controlled by a commercial system (Contact Precision Instruments, Boston). Startle blink was measured electromyographically through two 6-mm tin-cup electrodes placed under the left eye (sampling rate=1000 Hz; bandwidth=30–500 Hz). Startle was probed with a burst of white noise (40 msec, 102 dBA) with a near instantaneous rise time presented binaurally through headphones.
Conditioned Generalization Paradigm
The paradigm used in this study was identical to the one we described in detail elsewhere (9), in which 10 rings of gradually increasing size (Figure 1) presented on a computer monitor serve as conditioned stimuli and generalization stimuli. The largest and smallest rings serve as the conditioned danger cue (CS+) and conditioned safety cue (CS–), the former paired and the latter unpaired with an aversive unconditioned stimulus; the eight intermediately sized rings serve as generalization stimuli that form a continuum of similarity between the conditioned danger and conditioned safety cues. All conditioned and generalization stimuli are presented for 8 seconds on a computer monitor. The unconditioned stimulus is a 100-msec electric shock delivered to the left wrist (3–5 mA) that was rated by participants as being "highly uncomfortable but not painful."
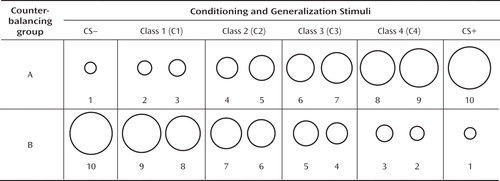
aParticipants were counterbalanced into two groups. For half of participants (group A), the largest ring was the conditioned danger cue (conditioned stimulus paired with shock, CS+) and the smallest was the conditioned safety cue (conditioned stimulus unpaired with shock, CS–), and for the other half (group B) this was reversed. The numerals below the rings label the stimuli from smallest to largest. As was done previously by Lissek et al. (9) to avoid an unduly large number of trials while maintaining a gradual continuum of size across rings, each of two intermediaries were collapsed into a single class of stimulus, leaving four classes of generalization stimuli. For both counterbalancing groups A and B, these classes of generalization stimuli are numbered such that class 4 consists of the two rings closest in size to the conditioned danger cue (rings 8 and 9 for counterbalancing group A, rings 3 and 2 for group B), and classes 3, 2, and 1 consist of rings progressively increasing in similarity to the conditioned safety cue. The diameter for the smallest ring (ring 1) was 2.00 inches, and diameters of subsequent rings increased progressively by 15%, such that ring 2 was 15% larger than ring 1 (diameter=2.30 inches), ring 3 was 30% larger than ring 1 (diameter=2.60 inches), ring 4 was 45% larger than ring 1 (diameter=2.90 inches), and so on (through 4.70 inches).
The paradigm consists of three phases: preacquisition, acquisition, and generalization test. Table 2 lists the trial types and frequencies included in each phase, including the number of conditioned danger cues coterminating with the unconditioned stimulus. Half of the trials for each phase were followed by startle probes 4 or 5 seconds after onset of the conditioned or generalization stimulus and were intermixed with a balanced number of startle probes presented during intertrial intervals. Nine startle probes were presented prior to study start, and time intervals between startle probes ranged from 18 to 25 seconds throughout the study.
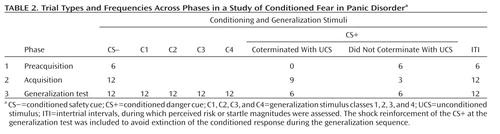 |
During the remaining unprobed stimulus trials and intertrial intervals, behavioral ratings of perceived risk for shock, as well as the associated response times, were assessed. Specifically, the question "Level of risk?" appeared on the computer monitor above the presented stimulus 1 or 2 seconds after trial onset and cued participants to enter a risk rating on a 3-point scale (1=no risk, 2=moderate risk, and 3=high risk). Participants were instructed to answer according to their "gut feeling" of risk and to respond as quickly as possible using a computer keyboard. Finally, after the acquisition and generalization phases, participants reported levels of anxiety evoked by conditioned danger and conditioned safety cues using 10-point Likert scales (1=none, 5=some, 10=a lot).
Data Analysis
Startle electromyography (EMG) was rectified and smoothed (20-msec moving window average). The onset latency window for the blink reflex was 20–100 msec, and the peak magnitude was determined within 120 msec of response onset. The average baseline EMG level for the 50 msec preceding the startle stimulus was subtracted from peak levels. EMG magnitudes across all phases were standardized using within-subject T score conversions. The size of the conditioned danger cue was not found to interact with the effects of stimulus type across groups for any dependent measure, so this factor was not entered in the final analyses. Acquisition of conditioning was analyzed with a 2×2 (group [patients and comparison subjects] by stimulus [danger cue and safety cue]) analysis of variance (ANOVA) with repeated measures. Additionally, generalization effects were analyzed using a 2×6 (group by stimulus type [safety cue, class 1, class 2, class 3, class 4, danger cue]) ANOVA with repeated measures. ANOVAs were computed using Wilks's lambda and were followed, when necessary, by either trend analyses or paired-samples t tests. Quadratic trend analyses were particularly important for testing the shape of generalization gradients, with the a priori hypothesis that patient but not comparison subject gradients would depart from the quadratic function found in healthy humans and intact animals (9–12). Alpha was set at 0.05 and was corrected using Hochberg's adjustment for multiple tests where appropriate (18). Finally, effect sizes were estimated using the unbiased estimator d (19).
Results
Pre-Acquisition
Analyses of startle EMG and online risk ratings revealed neither main effects of stimulus type nor stimulus type-by-group interactions.
Acquisition
Startle EMG.
Descriptive statistics are displayed in Table 3. Conditioned potentiation to the danger versus safety cue was acquired by both the patient group (F=15.11, df=1, 18, p=0.001; d=0.85) and the comparison group (F=22.75, df=1, 18, p<0.0002; d=1.05), and the strength of potentiation did not differ across groups.
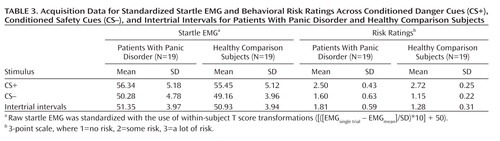 |
Strong perceptions of shock risk to the conditioned danger cue (versus conditioned safety cue) were acquired by both patients (F=32.36, df=1, 18, p<0.0001; d=1.25) and comparison subjects (F=373.22, df=1, 18, p<0.0001; d=4.24), and a significant stimulus type-by-group interaction emerged (F=13.53, df=1, 36, p=0.001; d=0.58). Follow-up tests of this interaction revealed that panic patients, relative to healthy comparison subjects, reported greater risk to the conditioned safety cue (p=0.009, d=1.21) but less risk to the conditioned danger cue (p=0.05, d=0.82) as well as less overall difference between conditioned danger and safety cues (p=0.001, d=1.57). Finally, conditioned danger and safety cues did not differ in terms of reaction times for risk ratings, and no stimulus type-by-group interaction for reaction times was found.
Retrospective anxiety.
Both groups reported higher levels of anxiety to the conditioned danger cue (mean=6.89, SD=2.54) relative to the conditioned safety cue (mean=2.47, SD=1.81) with p values <0.0006 (d=1.71). Additionally, such increases from safety to danger cue differed by group (F=13.99, df=1, 36, p=0.001; d=0.59), with weaker anxiety to the danger cue (p=0.009, d=0.86) and stronger anxiety to the safety cue (p=0.05, d=0.67) among panic patients (CS+: mean=6.11, SD=2.47; CS–: mean=3.11, SD=2.02) relative to comparison subjects (CS+: mean=8.06, SD=1.86; CS–: mean=1.89, SD=1.37) and stronger overall increases to the danger versus safety cue among comparison subjects (p=0.001, d=1.18). Notably, the stronger reported anxiety and risk ratings to the safety cue among patients are consistent with findings of heightened fear to learned signals of safety among anxiety patients generally (20) and panic patients specifically (21).
Generalization Test
Startle EMG.
Robust enhancement of startle during conditioned danger versus conditioned safety cues persisted during generalization for both patients and the comparison group (p values <0.0001, d values >1.13) and no stimulus type-by-group interaction was observed. Additionally, generalization of fear conditioning was evidenced by main effects of stimulus type in both patients (F=5.87, df=5, 14, p=0.004; d=0.55) and comparison subjects (F=8.16, df=5, 14, p=0.001; d=0.64), which were driven by downward gradients in startle magnitude as the presented stimulus differentiated from the conditioned danger cue (Figure 2). The pattern of this downward gradient differed across groups, as reflected by a significant stimulus type-by-group interaction (F=2.54, df=5, 32, p<0.05; d=0.51) that was attributable to between-group differences in the quadratic component of their respective slopes (stimulus type-by-group quadratic trend: F=4.94, df=1, 36, p=0.03; d=0.71). Follow-up tests on the stimulus type-by-group quadratic interaction were assessed using a Hochberg-adjusted p value of 0.025 and revealed a significant quadratic component in the generalization gradient of comparison subjects (F=13.95, df=1, 18, p=0.002; d=0.82) but not panic patients.
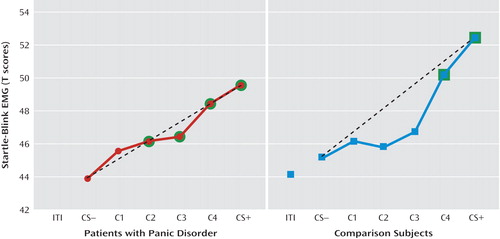
aThe dotted lines reflect linear decreases in startle from CS+ to CS– with which to visualize the deviation of gradients from linearity. Such deviations reflect a significant quadratic component in the generalization gradient of healthy comparison subjects (p=0.001) but not patients with panic disorder (p=0.62). The data points outlined in green mark stimulus classes for which startle is potentiated relative to the CS– (at the Hochberg-adjusted p value) for each group. Startle EMG was standardized using within-subject T score transformations ([([EMGsingle trial – EMGmean]/SD)*10]+50).
Figure 2 illustrates this group difference in quadratic components by displaying generalization gradients across groups separately. The dotted lines denote hypothetical linear decreases in startle potentiation from conditioned danger to conditioned safety cues, with which to visualize the presence and absence of a quadratic departure from linearity among comparison subjects and patients, respectively. Comparison subjects displayed a marked deviation from linearity, characterized by a steep curvilinear (quadratic) decline in conditioned fear as the presented stimulus differentiates from the conditioned danger cue. By contrast, the absence of a quadratic function in panic patients is evidenced by little deviation from linearity, indicating a more gradual decline in conditioned fear as stimuli move down the continuum of similarity. This less steep decline among patients demonstrates stronger generalization of fear from the learned danger cue to resembling stimuli as a conditioning marker of panic disorder.
To identify the point on the continuum of similarity at which startle potentiation ceased to generalize for patients and comparison subjects, planned comparisons were conducted whereby the conditioned safety cue was the reference condition compared against the conditioned danger cue as well as intermediary classes of generalization stimuli (classes 1–4). Hochberg's adjustment for multiple comparisons was applied to each of these five contrasts in patients and comparison subjects separately. Results in patients (criterion p=0.02) indicate startle potentiation to the conditioned danger cue (p<0.0001, d=1.14) that generalized to class 4 (p=0.002, d=0.80), class 3 (p=0.01, d=0.66), and class 2 (p=0.02, d=0.56) but not class 1 (p=0.11, d=0.37). By contrast, results in comparison subjects (criterion p=0.008) indicate startle potentiation to the conditioned danger cue (p<0.0001, d=1.27) that generalized to class 4 (p=0.001, d=0.78) but not class 3 (p=0.12, d=0.37), class 2 (p=0.54, d=0.14), or class 1 (p=0.37, d=0.20). As denoted by data points outlined in green in Figure 2, generalization of fear-potentiated startle in panic patients can be described as extending as far as the third approximation of the conditioned danger cue (i.e., class 2), whereas that of comparison subjects extended only to the closest approximation (i.e., class 4). This group difference demonstrates that panic patients require less danger cue similarity to trigger the conditioned fear response, and it provides further evidence for stronger fear generalization among patients with panic disorder.
Online risk ratings.
Conditioned elevations in perceived risk to the conditioned danger cue (versus conditioned safety cue) were displayed by both patients and comparison subjects (p values <0.0001, d values >1.55), and such elevations did not differ by group. Additionally, both groups displayed conditioned generalization as indexed by main effects of stimulus type in both patient and comparison groups (both p values <0.0001, d values >1.63) that were driven by graded decreases in perceived risk as the presented stimulus diverged from the conditioned danger cue (see Figure 3, left panel). Furthermore, a main effect of group was observed (F=4.88, df=1, 36, p=0.004; d=0.70), indicating higher risk ratings among panic patients regardless of stimulus type, and a significant stimulus type-by-group quadratic trend emerged (F=4.89, df=1, 36, p=0.03; d=0.70). This stimulus type-by-group interaction was driven by a group-by-class 4 (versus danger cue) interaction (F=8.45, df=1, 36, p=0.006; d=0.92) whereby panic patients, relative to comparison subjects, displayed less reduction in perceived risk from the conditioned danger cue to its closest approximation, class 4.
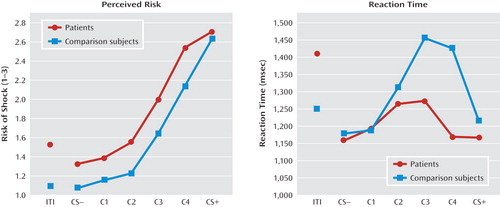
aParticipants were instructed to rate their perceived risk of shock, answering according to their "gut feeling" of risk (1=no risk, 2=some risk, 3=high risk), and to respond as quickly as possible using a computer keyboard. CS+=conditioned stimulus paired with shock; CS–=conditioned stimulus unpaired with shock; C1, C2, C3, and C4=generalization stimulus classes 1, 2, 3, and 4; ITI=intertrial interval.
Reaction times.
A main effect of stimulus type (F=4.46, df=5, 32, p=0.003; d=0.34) was observed and consisted of quadratic (F=18.19, df=1, 36, p=0.0001; d=0.68) and cubic components (F=5.62, df=1, 36, p=0.02; d=0.38). Reaction time data in both groups form inverted U's (see Figure 3, right panel), suggesting slower risk ratings for stimuli with less certain threat information (classes 1–4) and faster risk ratings for stimuli communicating more certain threat or safety information (i.e., threat and safety signals). Consistent with this visual assessment, overall analyses of data revealed the quickest reaction times to the safety cue, with responses to class 2, class 3, and class 4 each significantly slower than the safety cue (p values <0.009, d values >0.45); significantly slower responses to class 4 and class 3 versus the danger cue (p values <0.02, d values >0.41); and equally fast responses to the conditioned danger relative to the conditioned safety cue (p=0.41, d=0.13). This pattern of results implicates reaction times as an index of threat uncertainty, with longer reaction times reflecting more uncertainty.
Although both groups displayed the inverted-U pattern, a stimulus type-by-group cubic trend was observed (F=7.345, df=1, 36, p=0.01; d=0.86). This interaction was driven by significantly faster responses to class 4 in patients relative to comparison subjects (p<0.05, d=0.45), as group differences between all other stimulus classes were nonsignificant, and reaction times to class 4 versus the danger cue were significantly longer for healthy comparison subjects (p=0.004, d=0.40) but not patients (p=0.94, d=0.06). That response times for class 4 and the danger cue were not significantly different among panic patients suggests that patients were equally certain of risk for shock whether presented with the closest approximation of the danger cue or the danger cue itself. Conversely, among comparison subjects, the significant increase in threat uncertainty from the danger cue to class 4 suggests a decrease in perceived risk from the danger cue to its first approximation. This group difference in reaction time mirrors group differences in risk ratings from the danger cue to class 4 (see Figure 3, left panel). Specifically, as confirmed above by the significant interaction between group status and risk ratings to the danger cue versus class 4, decreases in perceived risk among patients from the danger cue to class 4 were smaller than those among comparison subjects.
Retrospective anxiety.
Conditioned danger relative to conditioned safety cues were rated as more anxiety provoking (mean=7.54, [SD=1.92] compared with mean=1.68, [SD=1.41]; p<0.0001, d=2.51), demonstrating the persistence of conditioning during the generalization test. Additionally, ratings for conditioned danger and safety cues did not differ across patients (CS+: mean=7.68, SD=2.08; CS–: mean=2.05, SD=1.87) and comparison subjects (CS+: mean=7.39, SD=1.79; CS–: mean=1.28, SD=0.46), as indicated by a nonsignificant group-by-stimulus type interaction (p=0.52, d=0.21).
Subjective Measures Across Acquisition and Generalization
Whereas patients displayed weaker differentiation of conditioned danger and conditioned safety cues as indicated by online risk ratings and reported anxiety during the first half of the study (acquisition phase; p values ≤0.01), levels of differentiation were comparable across groups during the latter half of the study (generalization phase). This observation was confirmed by a time (acquisition versus generalization)-by-group-by-stimulus type interaction for both risk ratings (F=4.24, df=1, 36, p<0.05; d=0.65) and reported anxiety (F=10.95, df=1, 36, p=0.002; d=1.05) and suggests retarded acquisition of conditioning among panic patients.
Group Differences at Intertrial Intervals
Notably, patients relative to comparison subjects displayed higher risk ratings (p=0.001) as well as a nonsignificant trend for stronger startle reactions (p=0.09) during intertrial intervals, suggesting stronger perceived threat among patients during intervals separating ring presentations when the computer monitor was blank.
Discussion
This study represents the first psychobiological demonstration of perturbed conditioned fear generalization in any anxiety disorder and in panic disorder specifically. The results suggest that panic disorder involves overgeneralization of conditioned fear, manifest in both potentiated-startle and self-report data. Replicating our previous study (9), generalization gradients in healthy comparison subjects resembled gradients in animal models of conditioning, as they were characterized by precipitous quadratic declines in conditioned responding as the presented stimulus diverged in similarity from the learned danger cue. Gradients among patients with panic disorder, however, fell along less steep and less quadratic slopes of responding, indicating stronger transfer of fear to stimuli resembling the conditioned danger cue. Consistent with these group differences in gradient shape, fear-potentiated startle in comparison subjects generalized to stimuli within one degree of dissimilarity to the danger cue (i.e., class 4) but not two or more degrees, whereas such potentiation in patients generalized to stimuli with up to three degrees of danger cue dissimilarity (i.e., class 4, class 3, class 2). This latter result demonstrates that the fear system of panic patients, relative to healthy individuals, is triggered by less robust threat information—indicative of lower thresholds of threat reactivity following conditioning among those with panic. Complementing startle EMG results, online risk ratings and associated response times indicated greater generalization of perceived risk from the conditioned danger cue to its closest approximation (class 4) among those with relative to those without panic disorder.
Overgeneralization as a Phenomenological Constituent of Panic Disorder
The overgeneralization in panic patients observed in this study may contribute importantly to the psychopathology of the disorder. Although conditioned stimuli themselves are restricted to actual stimuli present at the time of panic, fear generalization may result in proliferation of environmental cues capable of eliciting panic-related apprehension. Thus, a proclivity toward overgeneralization may result in an increased likelihood of encountering "panic reminders" in the weeks and months following the attack—conferring greater risk for additional attacks and eventual panic disorder. That said, because this study did not use prospective methods but rather tested individuals with existing panic disorder, longitudinal work is needed to determine whether abnormalities in generalization predate the onset of panic disorder and contribute toward its development or reflect ongoing disease processes of the disorder.
Putative Mechanism for Overgeneralization in Panic Patients
Fear of fear, referring to the tendency to respond fearfully to somatic arousal associated with fear, is an emotional process centrally implicated in explanatory models of panic disorder (1, 3, 22). Through this process, minor increases in anxious arousal occurring in the everyday context are escalated by secondary fear of such arousal. Whereas healthy individuals may be more able to regulate these minor increases in anxiety by way of top-down cognitive control, those with panic disorder may be unable to regulate because of the secondary fear of this arousal that escalates minor anxious reactivity to a more major form. In the current context, the danger information contained in the danger cue approximation (i.e., generalization stimulus) likely evokes a degree of initial fear reactivity. Subsequently, higher-level sensory processing of the approximation, revealing more subtle sensory distinctions between the actual danger cue and its approximation, is likely to result in a nonthreatening appraisal of the approximation—leading to a dampening of the initial fear response. According to this perspective, the fear-of-fear process associated with panic disorder escalates the initial fear response to the approximation that in turn overwhelms the panic patient's capacity to down-regulate this reactivity by way of higher-order sensory discrimination, resulting in the expression of fear in the presence of the approximation. Additionally, our finding of retarded acquisition of discriminative conditioning (as indicated in risk ratings and reported anxiety) suggests that discrimination abnormalities in panic disorder may be reversed given a sufficient number of learning trials—an observation consistent with past conditioning findings in the disorder (21). That is, with enough training, the unreinforced generalization stimulus may come to elicit little initial fear with which to form secondary fear of fear, resulting in the relative absence of a fear response to the generalization stimulus among panic patients.
Treatment Implications
The results of this study suggest hypotheses on novel treatments for panic disorder. Our data suggest that panic disorder involves perturbed discrimination of risk for aversive outcomes, as opposed to another form of pathology: oversensitivity to overt danger, as modeled by the conditioned danger cue. Data in animal models demonstrate that administration of d-cycloserine, a partial agonist of the N-methyl-d-aspartate receptor, enhances an organism's ability to discriminate conditioned danger cues from conditioned safety cues (22, 23). Given animal findings that d-cycloserine strengthens acquisition of aversive conditioning (see references 24 and 25, for example), d-cycloserine may enhance conditioned discrimination by strengthening the accuracy of learning—with a resulting decrease in generalization errors.
Another pharmacological prediction may be drawn from work in gerbils implicating conditioning-dependent retuning of sensory representations of the conditioned danger cue toward resembling stimuli (see reference 26, for example) that may lead to overgeneralization by rendering perceptual discrimination of the danger cue from its approximations more difficult. This perceptual blurring of the conditioned danger cue and its approximations has been tightly linked to the cholinergic system, with increased acetylcholine activity (in primary sensory cortex) associated with increases in this type of conditioning-dependent plasticity (27). Consequently, medications with anticholinergic properties (e.g., scopolamine) may facilitate improved sensory discrimination of the conditioned danger cue and its approximations and may thereby treat overgeneralization of the kind associated with panic disorder.
One final treatment implication stems from retarded acquisition of discriminative conditioning in panic disorder evidenced by deficient levels of learning in panic patients during the first but not the second half of the study. This conditioning deficit is related to the speed of—rather than the capacity for—discriminative conditioning. That is, after a sufficiently large number of learning trials, panic patients are able to discriminate the hedonic value of danger signals from those of safety at a level comparable to healthy comparison subjects. This finding suggests that overgeneralization in panic disorder might be reduced through psychotherapeutic interventions with a sufficient number of sessions aimed at imparting discriminative learning between genuine panic cues and resembling cues that may trigger false alarms but are themselves associated with no negative outcome. The pharmacological interventions described above, in tandem with this type of psychotherapy, may facilitate the strength and speed of discriminative learning in panic patients, with a resulting decrease in fear generalization.
Conclusions
Generalization of conditioned fear represents a promising but largely unstudied pathogenic marker of panic disorder. In this study, we sought to fill this gap using a novel fear-potentiated startle paradigm. Consistent with predictions, patients with panic disorder displayed marked elevations in conditioned fear generalization, as indicated by less steep decreases in conditioned responding as the presented stimulus differentiated from the danger cue. Additionally, conditioned fear in panic patients transferred to stimuli with up to three units of differentiation, whereas generalization in healthy comparison subjects was restricted to stimuli with only one unit of differentiation. Such results point to fear overgeneralization as a robust conditioning correlate of panic disorder.
1 : A modern learning theory perspective on the etiology of panic disorder. Psychol Rev 2001; 108:4–32 Crossref, Medline, Google Scholar
2 : A reanalysis of agoraphobia. Behav Ther 1978; 9:47–59 Crossref, Google Scholar
3 : Panic disorder: a product of classical conditioning. Behav Res Ther 1988; 26:441–450 Crossref, Medline, Google Scholar
4 : The Causes and Cures of Neurosis. London, Routledge and Kegan Paul, 1965 Google Scholar
5 : The observable unconscious and the inferable conscious in current Soviet psychophysiology: interoceptive conditioning, semantic conditioning, and the orienting reflex. Psychol Rev 1961; 68:81–147 Crossref, Google Scholar
6 : A contemporary learning theory perspective on the etiology of anxiety disorders: it's not what you thought it was. Am Psychol 2006; 61:10–26 Crossref, Medline, Google Scholar
7 : Conditioned Reflexes. New York, Oxford University Press, 1927 Google Scholar
8 American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed, Text Revision (DSM-IV-TR). Washington, DC, American Psychiatric Press, 2000 Google Scholar
9 : Generalization of conditioned fear-potentiated startle in humans: experimental validation and clinical relevance. Behav Res Ther 2008; 46:678–687 Crossref, Medline, Google Scholar
10 : Stimulus generalization of fear responses: effects of auditory cortex lesions in a computational model and in rats. Cereb Cortex 1997; 7:157–165 Crossref, Medline, Google Scholar
11 : Steady state data and a quantitative model of operant generalization and discrimination. J Exp Psychol Anim B 1975; 104:3–21 Crossref, Google Scholar
12 : Effects of discrimination training on stimulus generalization. J Exp Psychol 1959; 58:321–334 Crossref, Medline, Google Scholar
13 : Conditioned fear and startle magnitude: effects of different footshock or backshock intensities used in training. J Exp Psychol Anim Behav Process 1978; 4:95–103 Crossref, Medline, Google Scholar
14 : Fear-potentiated startle in humans: effects of anticipatory anxiety on the acoustic blink reflex. Psychophysiology 1991; 28:588–595 Crossref, Medline, Google Scholar
15 : Amygdala and anterior cingulate cortex activation during affective startle modulation: a PET study of fear. Eur J Neurosci 2003; 18:1325–1331 Crossref, Medline, Google Scholar
16 : Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P). New York, Biometrics Research, New York State Psychiatric Institute, 2002 Google Scholar
17 : Multicenter collaborative Panic Disorder Severity Scale. Am J Psychiatry 1997; 154:1571–1575 Link, Google Scholar
18 : A sharper Bonferroni procedure for multiple tests of significance. Biometrika 1988; 75:800–802 Crossref, Google Scholar
19 : Statistical Methods for Meta-Analysis. San Diego, Calif, Academic Press, 1985 Google Scholar
20 : Classical fear-conditioning in the anxiety disorders: a meta-analysis. Behav Res Ther 2005; 43:1391–1424 Crossref, Medline, Google Scholar
21 : Impaired discriminative fear-conditioning resulting from elevated fear responding to learned safety cues among individuals with panic disorder. Behav Res Ther 2009; 47:111–118 Crossref, Medline, Google Scholar
22 : D-Cycloserine: effects on long-term retention of a conditioned response and on memory for contextual attributes. Neurobiol Learn Mem 1999; 72:158–168 Crossref, Medline, Google Scholar
23 : Age- and dose-dependent facilitation of associative eyeblink conditioning by D-cycloserine in rabbits. Behav Neurosci 1997; 111:1303–1312 Crossref, Medline, Google Scholar
24 : D-Cycloserine causes transient enhancement of memory for a weak aversive stimulus in day-old chicks (Gallus domesticus). Neurobiol Learn Mem 1996; 66:236–240 Crossref, Medline, Google Scholar
25 : D-Cycloserine, a positive modulator of the N-methyl-D-aspartate receptor, enhances performance of learning tasks in rats. Pharmacol Biochem Behav 1989; 34:649–653 Crossref, Medline, Google Scholar
26 : Learning related plasticity of gerbil auditory cortex: feature maps versus meaning maps, in Advances in Metabolic Mapping Techniques for Brain Imaging of Behavioral and Learning Functions. Edited by \ Gonzalez-Lima FFinkestadt TScheich H. London, Kluwer Academic, 1992, pp 447–474 Crossref, Google Scholar
27 : Associative representational plasticity in the auditory cortex: a synthesis of two disciplines. Learn Mem 2007; 14:1–16 Crossref, Medline, Google Scholar



