Depressive Disorder and Incident Diabetes Mellitus: The Effect of Characteristics of Depression
Abstract
Objective
The purpose of this study was to test the hypothesis that clinically significant depression detected in a population sample increases the risk of diabetes mellitus. The authors examined the effect of characteristics of depression frequently found in the community on the risk of incident diabetes mellitus.
Method
A large community sample of adults aged ≥55 years (N=4,803) was assessed at baseline in a longitudinal three-wave epidemiological enquiry using a psychiatric interview and the Geriatric Mental State Schedule. Cases of depression were diagnosed according to standardized criteria, and diabetes was assessed using a risk factors questionnaire. Follow-up evaluations, conducted 2.5 and 5 years later, were completed to determine the incidence of diabetes.
Results
At baseline, 379 case subjects with depression were identified. The risk of incident diabetes mellitus was higher among subjects with depression when compared with nondepressed subjects, and the association remained significant after controlling for potential confounders, including diabetes risk factors. The estimated rate of diabetes mellitus attributable to depression was 6.87%. An increased risk of diabetes mellitus was also associated with the following characteristics of depression: nonsevere depression, persistent depression, and untreated depression. Treatment with antidepressants was not associated with an increased risk of diabetes mellitus.
Conclusions
Clinically significant depression is associated with a 65% increased risk of diabetes mellitus. Characteristics of depression frequently found in the community, namely nonsevere depression, persistent depression, and untreated depression, may play a role in the development of diabetes in a predominantly elderly adult population.
Predictions about the epidemic nature of both diabetes mellitus and depression during the first quarter of the 21st century are a matter of concern (1, 2), and negative effects in cases of comorbidity of these two conditions have been reported (3). In this context, hypotheses regarding the possibility that depression may eventually produce diabetes mellitus have recently been tested in longitudinal studies. In a meta-analysis, Mezuk et al. (4) identified 13 such studies and concluded that depressed individuals have a 60% increased risk of developing diabetes mellitus (4). However, most of these studies used rather weak methods to document depression (5), such as self-reports or general physicians' diagnoses, and therefore do not provide enough information on subjects with clinically significant depression (6). Of interest, in a previous meta-analysis, Knol et al. (7) found that only the study conducted by Eaton et al. (8) used formal diagnostic criteria for depression, and the reported hazard ratio was nonsignificant in that study. A more recent study conducted by Mezuk et al. (9) reported an association with new-onset diabetes mellitus in individuals with major depression that was detected in the community using the National Institute of Mental Health Diagnostic Interview Schedule. However, most cases of depression in the general population, particularly in older age groups, may not be major (10–13).
In this study, we tested the hypothesis that clinically significant depression, not limited to major depressive disorder, increases the risk of diabetes mellitus in the general population. In addition, we examined the effect of the following characteristics of depression frequently observed in previous community studies: nonsevere depression, first-ever depression, persistent depression, and untreated depression.
Method
General Design and Study Population
The sample for the present study was drawn from the Zaragoza Dementia and Depression (ZARADEMP) Project (14), a longitudinal three-wave epidemiological enquiry conducted in Zaragoza, Spain, documenting the incidence and risk factors of dementia and depression, as well as the association with somatic morbidity, in the adult population aged ≥55 years. The Helsinki convention principles of written informed consent, privacy, and confidentiality have been maintained throughout the project. A random sample of community dwelling people, stratified with proportional allocation by age and sex, was drawn from the most recent available census (in 1991). The sample size was calculated for the project's main objective, which was the study of cases of incident dementia, taking into account information on expected losses (i.e., deceased subjects, subjects who moved away, subjects who no longer agreed to participate) from the previous Zaragoza Study (10). Figure 1 illustrates the flow diagram of the ZARADEMP Project. The refusal rate was 20.5%, and 4,803 individuals were ultimately interviewed at baseline (wave I, 1994). Subjects with dementia and subtypes of dementia were excluded from the two follow-up evaluations (wave II, 1997; wave III, 1999). Additional details about the project's design and objectives have been published previously (14). In the present study, case subjects with diabetes mellitus at baseline and individuals with missing data were removed from the follow-up interviews, and thus 3,521 subjects were included.
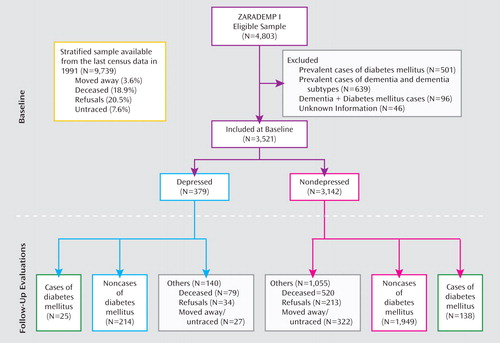
aThe ZARADEMP Project consisted of two follow-up interviews after baseline: wave II (mean duration: 2.18 years [SD=0.23]) and wave III (mean duration: 4.72 years [SD=0.38]).
Procedure
An epidemiological case finding design was implemented in each assessment wave. In wave I (baseline interview), well-trained and regularly supervised lay interviewers conducted the 25- to 90-minute ZARADEMP interview at the subjects' homes. Institutionalized subjects were assessed in their place of residence. The interview incorporates standardized Spanish versions of the following instruments, as relevant to the present report: the Geriatric Mental State Schedule–History and Etiology AGECAT (Automated Geriatric Examination for Computer Assisted Taxonomy) package (10, 15), Katz Index (16, 17), Instrumental Activities of Daily Living scale (18, 19), and a series of questions regarding medical and psychiatric history in the EURODEM (European Community Concerted Action on the Epidemiology and Prevention of Dementia) Study Risk Factors Questionnaire (20). Medical reports, which are frequently available at individuals' homes in Spain and usually include laboratory data, were used in the diagnostic process. Utilizing the same interview as the lay interviewers, the trained supervising research psychiatrists reassessed those participants whose cases were considered to be questionable according to predetermined criteria. These interviews were also conducted in the participants' homes. Our previous studies support the validity of this case finding/diagnostic process in the community (10). A similar procedure was implemented in follow-up assessment waves II and III, with the interviewers unaware of the results of the baseline interview.
Assessment of Depression
Diagnosis of depression was based on the Geriatric Mental State Schedule, and AGECAT criteria (confidence level ≥3) were applied. This method has been proven valid to detect cases of depression in community samples that require clinical attention (21). AGECAT criteria were also used to classify "severe cases" (which include melancholic symptoms) and "nonsevere cases" of depression. Information from the history and etiological schedule was used to define history of depression and use of antidepressant treatment (classified according to the Anatomical Therapeutic Chemical Classification system [22]; codes: N06A* and/or N06C1A). We defined persistence of depression as the presence of depression at baseline and the first follow-up evaluation.
Assessment of Diabetes Mellitus
The presence of diabetes mellitus was scored by assessment of each subject's medical history using the EURODEM questionnaire (20). Scores were calculated based on responses primarily to the following three questions: "Do you have diabetes?" "Who diagnosed that you have diabetes?" "What kind of treatment did you receive for the diabetes?" Only subjects responding positively to the first question and for whom the diagnosis was established by a medical doctor and who were also receiving treatment (insulin, oral hypoglycemic agent, or diet) were regarded as having diabetes.
Covariates
Potentially confounding factors assessed at baseline included demographic variables, diabetes mellitus risk factors (hypertension, smoking, statin use, body mass index, alcohol intake, family history of diabetes), functional disability, and use of both antidepressants and antipsychotics. Educational level was dichotomized as low (completed only primary school or less) or not low. Smoking was based on World Health Organization criteria (23) for lifetime tobacco exposure, and subjects were classified as smokers or nonsmokers. Statin and psychotropic use were defined according to the Anatomical Therapeutic Chemical Classification system (22). Body mass index was calculated as weight in kilograms divided by height in square meters. Alcohol intake was categorized according to World Health Organization criteria as moderate- or high-risk consumption (≥40 grams per day for men and ≥20 grams per day for women). Family history of diabetes mellitus was based on self-reports in the EURODEM questionnaire and categorized as "no close relative," "one close relative" (parent or sibling), or "two or more close relatives" with a history of diabetes. Disability was based on the Katz Index and Instrumental Activities of Daily Living scale. For this study, the scores were dichotomized, distinguishing between disability (positive scores on both instruments) and no disability.
Statistical Analysis
Differences between baseline characteristics for depressed and nondepressed subjects were assessed using two-tailed chi-square tests on categorical data, and differences on variables with approximately normal distributions were assessed using two-tailed t tests. Crude incidence rates of diabetes mellitus were calculated by dividing the number of diabetes cases by person-years. For individuals with diabetes mellitus, person-years were estimated as the sum of the known disease-free period plus one-half the interval between the date of the individual's last clinical visit without the disease and the date in which the individual was regarded as diabetic. For individuals without diabetes mellitus, person-years were calculated from baseline to the date of the individual's last clinical visit or to the date of death or moving away or refusal to participate in the interview (information on deaths and moving away were obtained from census data). Confidence intervals (CIs) for incidence rates were based on Poisson distribution.
Cox proportional hazards regression models were used to calculate the hazard ratio of developing diabetes mellitus in participants with depression relative to those without. In order to explore mechanisms explaining the association, we used a series of models in which we gradually controlled for potential confounders/mediators. Model 1 included terms for age and sex. Model 2 included the terms in model 1 plus terms for living situation and educational level. Model 3 included the terms in model 2 plus the following additional terms: family history of diabetes mellitus, hypertension, statin use, functional disability, current smoking, alcohol risk consumption, and antidepressant and antipsychotic use. Unexpected results in calculating model 3 led to a closer investigation. We observed that there had been differential losses in body mass index that occurred during follow-up evaluations (8.4% among depressed subjects and 5% among nondepressed subjects). Therefore, to improve the accuracy of the statistical analysis, we performed imputation of a single variable (i.e., body mass index) by a linear regression model based on a set of predictors (the covariates used) (24). The regression model represented ordinary least squares regression because the imputed variable (body mass index) was continuous.
To estimate the population attributable risk proportion to depression, the following calculation was performed: p×[(HRexposed–HRunexposed)/HRexposed] ×100 ("p" represents the proportion of subjects who were exposed and "HR" represents the hazard ratio adjusted in model 3) (25).
We also used model 3 to study the effect of the different characteristics of depression on the risk of diabetes mellitus, adjusted by the same variables. Differences in hazard ratios among these specific characteristics were assessed by comparing the hazard ratios in one group with each counterpart within depression (e.g., severe versus nonsevere, previous versus first-ever), using chi-square analysis comparing logarithms of the hazard ratios.
Results
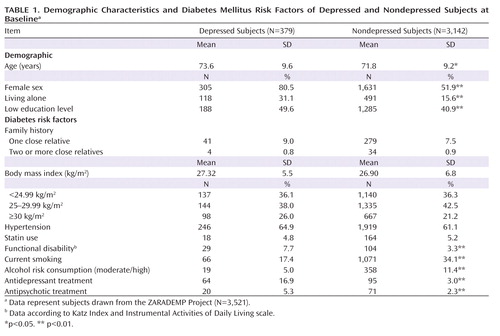
Of the total sample in the analysis for this study (N=3,521), 379 participants (10.8%) were diagnosed with depression. Baseline characteristics of depressed and nondepressed participants are shown in Table 1. Compared with participants without depression, depressed subjects were 1.7 years older and were more likely to be female, to be less educated, to live alone, and to have a functional disability. No significant differences were observed between groups in mean body mass index, statin use, family history of diabetes, or hypertension. Depressed subjects were less likely to be smokers and/or moderate to high alcohol consumers. In contrast, they were more frequently taking antidepressant and/or antipsychotic medication.
 |
As seen in Table 2, 163 incident cases of diabetes mellitus were found in the follow-up assessment waves (25 depressed subjects [6.6%] and 138 nondepressed subjects [4.4%]). The incidence rate was higher among depressed subjects (19.70 per 1,000 person-years) relative to nondepressed subjects (12.36 per 1,000 person-years).
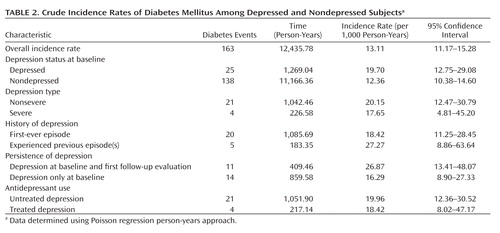 |
In relation to characteristics of depression, most individuals who were depressed at baseline (N=315 [83.1%]) were considered to have nonsevere depression; 51 [13.5%] had a history of depression; and 64 [16.9%] were taking antidepressant medication. At the follow-up assessments, 109 individuals (28.8%) continued to be depressed (persistent depression). The incidence rate of diabetes mellitus was higher in individuals who had nonsevere depression, a history of depression, and untreated depression. It was also higher for those who had persistent depression, when compared with each depression counterpart (e.g., severe versus nonsevere, previous versus first-ever).
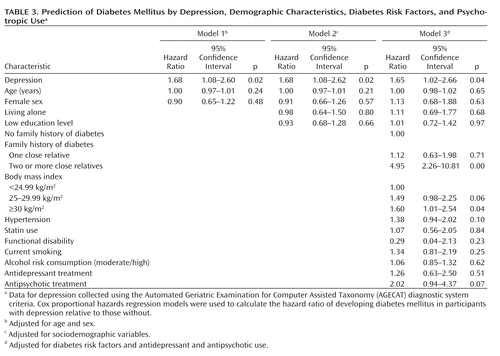
In the multivariate analysis (Table 3), a significant association was observed between depression at baseline and incident diabetes mellitus, adjusted for age and sex (model 1). Other factors at baseline were also associated with incident diabetes mellitus, adjusted for age and sex. The risk estimates (hazard ratios) were 4.67 (95% CI=2.18–10.00) for family history of diabetes (two or more close relatives); 1.61 (95% CI=1.10–2.40) for body mass index 25–29.99 kg/m2; 1.92 (95% CI=1.25–2.96) for body mass index ≥30 kg/m2; and 1.57 (95% CI=1.08–2.27) for hypertension. The association between depression and incident diabetes mellitus persisted after adjustment for other sociodemographic variables (model 2) and after additional adjustment in model 3 for diabetes risk factors and antidepressant and antipsychotic use (hazard ratio=1.65; 95% CI=1.02–2.66). In this final model (model 3), incident diabetes mellitus was also associated with family history of diabetes (two or more close relatives) and with a body mass index ≥30 kg/m2, but the association with both antidepressant and antipsychotic use was nonsignificant. By removing both antidepressant and antipsychotic use from the model, the increased risk of diabetes mellitus in depressed subjects persisted (hazard ratio=1.75 [95% CI=1.11–2.77, p=0.02]). In contrast, when depression was removed from model 3, the association of each psychotropic drug with diabetes mellitus increased but remained nonsignificant.
 |
The population attributable risk percentage for diabetes mellitus, comparing depressed and nondepressed subjects and based on hazard ratios obtained after adjustment in model 3, was 6.87% (95% CI=1.04%–11.64%).
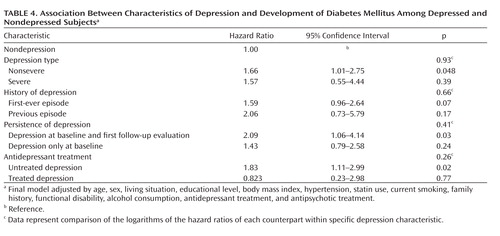
Table 4 shows hazard ratios for the development of diabetes mellitus in relation to depression characteristics. Compared with nondepressed individuals, participants considered to have nonsevere depression at baseline had a significantly increased risk of diabetes mellitus (hazard ratio=1.66 [95% CI=1.01–2.75, p=0.048]). Similarly, the risk was statistically significant for individuals with persistent depression (hazard ratio=2.09 [95% CI=1.06–4.14, p=0.03]) and for individuals with untreated depression (hazard ratio=1.83 [95% CI=1.11–2.99, p=0.02]). Furthermore, a nearly significant difference for developing diabetes mellitus was observed in individuals both with and without a history of depression. Directly comparing the hazard ratios associated with specific depression characteristics with each counterpart within depression (e.g., severe versus nonsevere, previous versus first-ever) did not result in any significant difference in hazard ratio.
 |
Discussion
This 5-year longitudinal study of community dwelling adults aged ≥55 years supports the hypothesis that clinically significant depression increases the risk of diabetes mellitus. As expected, body mass index and, particularly, family history of diabetes (two or more close relatives) were associated with new-onset diabetes mellitus, and the association with other related factors, such as hypertension and antipsychotic use, was close to statistical significance. However, when we controlled for all of these potential confounders, the association of depression with diabetes mellitus remained statistically significant (hazard ratio=1.65 [95% CI=1.02–2.66, p=0.04]).
Two recent meta-analyses (4, 7) previously reported an increased risk of developing diabetes in depressed individuals. However, most studies reviewed used self-reports or general physicians' diagnoses to document depression and therefore did not provide enough information on clinically significant depression. To our knowledge, only Epidemiologic Catchment Area studies have previously used a standardized psychiatric interview in this type of assessment. Eaton et al. (8) did not find a significantly increased risk of diabetes mellitus, and Mezuk et al. (9) reported an increased risk only in cases of major depressive disorder. In contrast, the association with new-onset diabetes mellitus in our study was not limited to major depressive disorder. Furthermore, the fact that we used standardized AGECAT diagnostic criteria (15, 21) provided us with an advantage over many previous studies (5). AGECAT "caseness" (confidence level ≥3) implies the "desirability of intervention" (21, 26). A previous 4.5-year follow-up study conducted in Zaragoza, Spain (13), supports the clinical implications in cases of depression detected using this system in the assessment of community elderly (42.0% of subjects died, and 22.7% remained depressed at the follow-up interview). The public health perspective in our study also seems relevant, since the estimated rate of diabetes mellitus attributable to depression was 6.87% (prevalence of depression: 10.8%). The population attributable risk is a function of the strength of the association and the prevalence of the risk factor. The estimated attributable risk was 9% in the Mezuk et al. meta-analysis (4), with a reported prevalence of depression of 16%.
Our study suggests that the association with diabetes mellitus may vary according to some characteristics of depression. The increased risk of this endocrine disease in individuals with severe depression that was detected using AGECAT criteria was not statistically significant, but it is unclear whether the nonsignificant findings are the result of the relatively small number of severe cases or the magnitude of the association. However, we found a statistically significant increment in the risk of diabetes mellitus in individuals with nonsevere depression. This is remarkable, since most cases of depression with clinical repercussion in our study (83.1%), and similarly in other studies of community dwelling adults aged ≥55 years, were nonsevere (10–12, 21, 27). Cases of depression considered to be nonsevere using AGECAT criteria may be similar to those considered "minor" or "subthreshold" by some investigators (28). In relation to DSM criteria, agreement with AGECAT criteria is considered "moderate" (26). Data reported by Schaub et al. (26) are fairly coincident with our previous data (10, 12) and suggest that close to 50% of AGECAT "severe" cases of depression correspond to DSM-IV-TR criteria for "major" depression and approximately two-thirds of "nonsevere" cases correspond to DSM-IV-TR criteria for "minor" depression.
Contrary to van den Akker et al. (29), we did not find an increased risk of new-onset diabetes in subjects with first-ever depression. However, van den Akker et al. limited their study to the population <50 years of age. Conversely, we found support for our conjectures about the increased risk for diabetes mellitus associated with both persistent and untreated depression. Carnethon et al. (30) suggested the association with persistent depression, but their assessment was based on self-reports. We cannot claim that the hazard ratios associated with these specific characteristics explored are significantly higher when compared with each counterpart within depression. Nevertheless, the associations found are still noticeable because both persistent and untreated depression are commonly reported in population studies of the elderly (12, 13).
In relation to treating depression in community studies of the elderly, there is conflicting evidence about the potential association of antidepressant use with new-onset diabetes mellitus (31, 32). Andersohn et al. (32) recently reported an increased risk in a large cohort of depressed patients in a clinical network. Their finding may lead to arguments about the possibility that antidepressant treatment and not depression itself increases the risk of diabetes mellitus. However, we did not find support for this argument, since we observed that depression increased the risk of new-onset diabetes after controlling for antidepressant use. Moreover, if we remove antidepressant treatment from the model, the increased risk of diabetes mellitus among the depressed patients persists, and if we remove depression from the model, the risk of diabetes mellitus does not increase significantly as the result of antidepressant treatment at baseline.
Some limitations to this study must be addressed. There was significant attrition from sampling to enrollment, which was higher than that of studies such as the Cache County Study (33). However, the investigators in the Cache County Study considered their sample to be unusual and their response rate to be high. Moreover, the attrition rate in our sample was expected in the study design (10, 14), and we previously argued that our investigation competes favorably with several two-stage epidemiological studies in this field (14). It might also be argued that the exclusion of subjects with dementia at baseline from the two follow-up interviews might have affected the main findings related to incident diabetes mellitus. However, secondary analysis has shown no significant differences in the prevalence of diabetes mellitus between individuals with and without dementia. Since we have not found evidence that dementia modifies the risk of new-onset diabetes mellitus, we trust that this has not biased our study in any important way.
In view of previous reports (34), we were surprised to find less frequent smoking among depressed subjects relative to nondepressed subjects and no differences in the frequency of body mass index categories. Cultural factors should be considered in relation to smoking, since women predominate in this sample and tobacco use is rare among women in this age group in Spain (35), which is reflected in this study (tobacco use in women: 6.1%). The absence of differences between depressed and nondepressed subjects in relation to body mass index categories might be partially explained by differential loss between both groups for this particular variable. Since we used imputation techniques to address these losses, we also trust that our results have not been severely biased.
The main limitation in this and similar studies of self-reported diabetes relates to the diagnosis of diabetes mellitus in the absence of laboratory measures. We believe the information was acceptable in cases previously diagnosed by primary care physicians or specialists, but previous reports suggest that a considerable proportion of patients are not aware that they have diabetes mellitus (36, 37). Undercounting cases of diabetes might be more important among depressed individuals, since they are less likely to see a doctor (38). However, the resulting systematic misclassification would not modify the main conclusion derived from this study. False negative cases of diabetes among depressed subjects at baseline would be erroneously included in the denominator (person-years) for calculation of the incidence rate of diabetes. Moreover, undercounting diabetes among depressed subjects in the two follow-up waves would result in a decrement of the numerator (incident cases of diabetes) and the underestimation of the incidence rate of diabetes among this group. In this way, the rates for depressed subjects would come nearer to the rates for nondepressed subjects, and the risk ratio (hazard ratio) would be nonsignificant. However this is contrary to our findings.
In summary, previous reports have suggested that there is a robust association between depression and incidence of diabetes mellitus (4). The results of this study, showing a 65% increased risk of diabetes mellitus associated with clinically significant depression, reinforce that conclusion. Furthermore, depression with characteristics frequently observed in the community, namely nonsevere, persistent, and untreated depression, is associated with an increment of risk of diabetes mellitus. In view of the epidemic nature of both diabetes and depression, we believe our results have important public health as well as clinical implications. However, whether interventions in depression lower the increased risk of diabetes has yet to be examined.
1 : Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. Lancet 1997; 349:1498–1504 Crossref, Medline, Google Scholar
2 : Global burden of diabetes, 1995–2025: prevalence, numerical estimates, and projections. Diabetes Care 1998; 21:1414–1431 Crossref, Medline, Google Scholar
3 : The impact of depressive symptoms and chronic diseases on active life expectancy in older Americans. Am J Geriatr Psychiatry 2008; 16:425–432 Crossref, Medline, Google Scholar
4 : Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care 2008; 31:2383–2390 Crossref, Medline, Google Scholar
5 : Comment on: Knol MJ, Twisk JWR, Beekman ATF, Heine RJ, Snoek FJ, Pouwer F (2006) depression as a risk factor for the onset of type 2 diabetes mellitus: a meta-analysis. Diabetologia 2006; 49:2797–2798 Crossref, Medline, Google Scholar
6 : Depression in diabetes: The chicken or the egg? Psychosom Med 2007; 69:297–299 Crossref, Medline, Google Scholar
7 : Depression as a risk factor for the onset of type 2 diabetes mellitus: a meta-analysis. Diabetologia 2006; 49:837–845 Crossref, Medline, Google Scholar
8 : Depression and risk for onset of type II diabetes: a prospective population-based study. Diabetes Care 1996; 19:1097–1102 Crossref, Medline, Google Scholar
9 : The influence of educational attainment on depression and risk of type 2 diabetes. Am J Public Health 2008; 98:1480–1485 Crossref, Medline, Google Scholar
10 : The prevalence of dementia and depression in the elderly community in a southern European population: the Zaragoza Study. Arch Gen Psychiatry 1995; 52:497–506 Crossref, Medline, Google Scholar
11 : Minor depression and health status among US adults with diabetes mellitus. Am J Manag Care 2007; 13:65–72 Medline, Google Scholar
12 : Depression in the elderly community, I: prevalence by different diagnostic criteria and clinical profile. Eur J Psychiatry 2008; 22:131–140 Google Scholar
13 : Depression in the elderly community, II: outcome in a 4.5 years follow-up. Eur J Psychiatry 2008; 22:141–150 Google Scholar
14 : The ZARADEMP project on the incidence, prevalence and risk factors of dementia (and depression) in the elderly community, II: methods and first results. Eur J Psychiatry 2005; 19:40–54 Google Scholar
15 : A computerized psychiatric diagnostic system and case nomenclature for elderly subjects: GMS and agecat. Psychol Med 1986; 16:89–99 Crossref, Medline, Google Scholar
16 : Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. JAMA 1963; 185:914–919 Crossref, Medline, Google Scholar
17 : Capacidad funcional de pacientes mayores de 65 años, según el Índice de katz. Fiabilidad del método Atención Primaria 1992; 10:812–816 Medline, Google Scholar
18 : Assessment of older people: self-maintaining and Instrumental Activities of Daily Living. Gerontologist 1969; 9:179–186 Crossref, Medline, Google Scholar
19 : Evaluación del deterioro cognitivo y funcional de la demencia. Escalas de mayor interés en la Atención Primaria, in El Médico Ante la Demencia y su Entorno, Módulo 1. Edited by Boada MTárraga L.. Barcelona, Spain, Bayer SA, 1995, pp 37–50 Google Scholar
20 : European studies on the incidence of dementing diseases: a report of the EURODEM research group. Neuroepidemiology 1992; 11(suppl 1):1–22 Crossref, Google Scholar
21 : Depression among older people in Europe: the EURODEP studies. World Psychiatry 2004; 3:45–49 Medline, Google Scholar
22 World Health Organization: Anatomical Chemical Classification Index With Defined Daily Doses (DDDs). Oslo, Norway, World Health Organization Collaborating Centre for Drug Statistics Methodology, 2001 Google Scholar
23 : Effect of smoking on global cognitive function in nondemented elderly. Neurology 2004; 62:920–924 Crossref, Medline, Google Scholar
24 : Statistical Analysis With Missing Data, 2nd ed. New York, Wiley InterScience, 2002 Crossref, Google Scholar
25 : Use and misuse of population attributable fractions. Am J Public Health 1998; 88:15–19 Crossref, Medline, Google Scholar
26 : A comparison of GMS-A/AGECAT, DSM-III-R for dementia and depression, including subthreshold depression (SD): results from the Berlin Aging Study (BASE). Int J Geriatr Psychiatry 2003; 18:109–117 Crossref, Medline, Google Scholar
27 : The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care 2005; 28:2668–2672 Crossref, Medline, Google Scholar
28 : Minor and major depression and the risk of death in older persons. Arch Gen Psychiatry 1999; 56:889–895 Crossref, Medline, Google Scholar
29 : Is depression related to subsequent diabetes mellitus? Acta Psychiatr Scand 2004; 110:178–183 Crossref, Medline, Google Scholar
30 : Longitudinal association between depressive symptoms and incident type 2 diabetes mellitus in older adults: the Cardiovascular Health Study. Arch Intern Med 2007; 167:802–807 Crossref, Medline, Google Scholar
31 : No increased incidence of diabetes in antidepressant users. Int Clin Psychopharmacol 2007; 22:382–386 Crossref, Medline, Google Scholar
32 : Long-term use of antidepressants for depressive disorders and the risk of diabetes mellitus. Am J Psychiatry 2009; 166:591–598 Link, Google Scholar
33 : Prevalence of depression and its treatment in an elderly population: the Cache County Study. Arch Gen Psychiatry 2000; 57:601–607 Crossref, Medline, Google Scholar
34 : Examining a bidirectional association between depressive symptoms and diabetes. JAMA 2008; 299:2751–2759 Crossref, Medline, Google Scholar
35 : Smoking after age 65 years and mortality in Barcelona, Spain. Am J Epidemiol 1998; 148:575–580 Crossref, Medline, Google Scholar
36 : Full accounting of diabetes and pre-diabetes in the US population in 1988–1994 and 2005–2006. Diabetes Care 2009; 32:287–294 Crossref, Medline, Google Scholar
37 : Primary care diabetes in Spain. Prim Care Diabetes 2008; 2:101–103 Crossref, Google Scholar
38 : Predictors of self-neglect in community-dwelling elders. Am J Psychiatry 2002; 159:1724–1730 Link, Google Scholar



