Service Use and Outcomes of First-Admission Patients With Psychotic Disorders in the Suffolk County Mental Health Project
Abstract
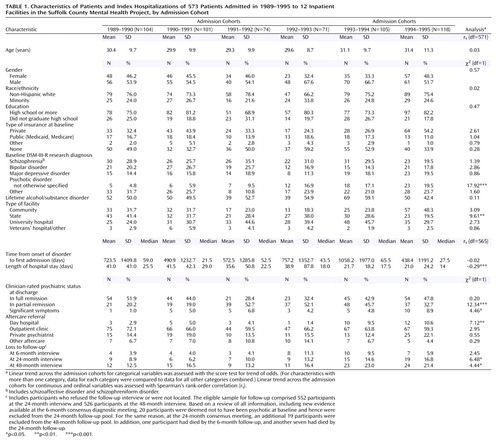
OBJECTIVE: The purpose of the study was to examine the inpatient and outpatient service use and 4-year outcomes of newly admitted psychotic patients during a period of rapid change in the provision of psychiatric services in a well-defined catchment area in New York State in the 1990s. METHOD: Subjects were 573 participants of the Suffolk County Mental Health Project. This group comprised patients with psychotic disorders first admitted between September 1989 and August 1995 to 12 inpatient facilities across Suffolk County, N.Y., and followed for up to 48 months. The subjects’ service use, course of illness, symptomatic outcomes, suicide risk, homelessness risk, and satisfaction with care were compared across admission years. RESULTS: The length of inpatient stays decreased significantly across the years. However, the number of outpatient visits and therapy sessions did not vary. Although the patients admitted in later years were more symptomatic at admission to their first hospitalization, their course and outcomes over the follow-up period were not worse and they were not less satisfied with their care, compared with the patients admitted in earlier years. CONCLUSIONS: The clinical characteristics of patients and the role of inpatient care in the management of patients with psychotic disorders gradually changed during the 1990s. These changes, however, were not associated with changes in the use of outpatient services or outcomes. Nevertheless, shorter hospital stays and the presence of more severely ill patients highlight the need for more attention to linkage to aftercare and enhancement of support networks in the community.
The 1990s witnessed many changes in mental health services for patients with severe mental disorders (1). Perhaps the most visible of these changes was the reduced reliance on inpatient treatment. Although this trend began in the early 1960s with the first major wave of deinstitutionalization, it continued well through the 1990s. Between 1988 and 1994, for example, the total number of days of care in mental hospitals declined by 12.5 million days per year (2), a decrease that was only partly offset by an increase of 1.2 million days of psychiatric care in general hospitals. This decline was due mostly to shorter lengths of hospital stays, as the number of psychiatric discharges did not decrease during this period (2).
Policies intended to reduce the length of hospital stays were partly motivated by cost concerns. Many policy makers and clinicians also believed that partial hospitalization and outpatient services would be as effective as inpatient care but would be less restrictive and more conducive to patients’ integration into the community.
Whether and to what extent this shift in locus of care occurred and its effects on clinical and social outcomes of patients with severe mental illness have yet to be fully examined. A study of privately insured patients treated between 1993 and 1995 revealed a paradoxical decrease in the use of outpatient services that accompanied a reduction in inpatient days (3). Such overall reduction in services is a cause for concern, particularly for patients with severe mental disorders. Many of these patients require long-term aftercare, and some require rehospitalization for stabilization or medication adjustment. Thus, reduced use of services may adversely affect the course and outcome of these conditions.
We used data from a longitudinal epidemiological study of first-admission patients with psychotic disorders in the early to mid-1990s in a well-defined catchment area in New York State to examine changes in the mix and volume of services provided to this patient population during this period. We also examined changes in the patients’ clinical and social outcomes and in their satisfaction with care. Recruitment that extended over a period of 6 years provided a natural experiment in which systematic variations in usual services and outcomes in this setting could be studied. We focused on first admissions in order to minimize the effect of past treatment history and better reflect the treatment careers of new entrants into the care system.
We addressed three specific questions: 1) How did the use of inpatient and outpatient services change among consecutive cohorts of patients admitted in 1989–1995? 2) How did the 48-month course and outcome of these consecutive cohorts of patients change? 3) How did their global functioning and satisfaction with care change?
Method
Subjects
The data were drawn from the Suffolk County Mental Health Project, a longitudinal epidemiological study of consecutive first admissions to 12 psychiatric facilities in Suffolk County, N.Y., between 1989 and 1995 (4). Briefly, inclusion criteria for the study were age 15–60 years, residence in the county, clinical evidence of psychosis, and both capacity and willingness to provide written informed consent. Exclusion criteria were a psychiatric hospitalization more than 6 months before the current admission, moderate or severe mental retardation, and inability to speak English. Overall, 674 individuals met the inclusion criteria and agreed to participate in the study. We further limited the sample for this study to patients who had no previous hospitalizations (N=600) and who had their first admission between September 1, 1989, and August 31, 1995 (N=573). Although a few patients were admitted to the participating facilities before September 1, 1989, the recruitment sites became fully operational only after this date. Similarly, although the study continued through the early 1996, the recruitment rate in the later months dropped to below 50%, partly because of the extremely short stays of some of the patients.
Data Collection
Written informed consent was obtained from the subjects for participation in the study, and their written permission to gather information from medical records and from significant others was obtained. After the baseline interview, the subjects were interviewed by telephone every 3 months and in person at months 6, 24, and 48. Interviews were conducted by trained research interviewers, all of whom were mental health professionals.
Nonparticipation and Loss to Follow-Up
The proportion of subjects who agreed to participate and were located for interview at baseline did not vary systematically across the years of the study included in this report (score test for trend=0.10, df=1, p=0.75). Overall, 72.0% (N=674) of the patients referred to the study completed the baseline interview. Patients who were referred to the study but did not agree to participate or were not located were more likely to be older and female and more likely to have their first admission in state or university facilities rather than in community facilities or other types of facilities. We adjusted for these factors in the main analyses.
At the 6-month consensus diagnostic meeting, which included a review of all information available to the project psychiatrists, 20 participants were deemed not to have had a psychotic disorder at baseline and hence were excluded from the 24-month follow-up pool. For the same reason, at the 24-month consensus meeting, an additional 19 participants were excluded from the pool of eligible subjects for the 48-month follow-up. These exclusions had no effect on the results of the study. In addition, one participant had died by the 6-month follow-up, and another seven had died by the 24-month follow-up. Thirty-six (6.3%) of the 573 participants in the follow-up pool at 6 months, 67 (12.1%) of the 552 participants at 24 months, and 94 (17.9%) of the 526 participants at 48 months either could not be located or refused participation and were thus classified as lost to follow-up. The prevalence of loss to follow-up at 24 and 48 months increased across successive cohorts (Table 1). However, loss to follow-up was not associated with baseline diagnosis, severity of symptoms, course, or satisfaction with care at earlier assessment points. Furthermore, when analyses were repeated by limiting the sample to participants who were not lost to follow-up by 48 months, the results were mainly similar to those reported here.
Patient and Index Treatment Characteristics
Data on patient characteristics were obtained from the Structured Clinical Interview for DSM-III-R (SCID) (5). Length of stay, characteristics of the index treatment facility, patient disposition, and status at discharge (categorized as “full remission,” “partial remission,” and “having significant symptoms”) were extracted from admission hospital records by using a standardized form. Preadmission duration of illness and treatment history were assessed as part of the SCID and were codedb by using a modified version of the Strauss-Carpenter Prognostic Rating Scale (6). The type of insurance was determined at baseline and at the 6- and 24-month assessments (7). The DSM-III-R baseline research diagnosis was a consensus decision of two or more psychiatrists on the basis of the SCID interviews and hospital records (4).
Course of Treatment
The number and length of rehospitalizations were assessed every 6 months. Medical records were obtained for the index admission in Suffolk County and for subsequent self-reported hospitalizations and outpatient treatments, irrespective of location. On the basis of these records, the course of outpatient treatment was rated globally every 6 months on a scale adopted from the Schedule for Affective Disorders and Schizophrenia—Lifetime Version (SADS-L) (8). Categories of response for the rating of outpatient treatment course included “continuous treatment,” “several brief periods of treatment,” “consultation/brief periods,” and “none.” The type and frequency of outpatient treatment contacts were assessed by using a standardized instrument that was also completed every 6 months.
Course of Illness, Clinical Outcomes, Suicide, and Homelessness
The course of illness was rated every 6 months by the interviewers on a modified scale adopted from the Strauss-Carpenter Prognostic Rating Scale (6); the period covered by the rating was the preceding 6 months. Ratings on this scale included “full remission for 3 months or longer,” “full remission for less than 3 months,” “partial remission,” “new episodes during interval,” and “original disorder continued.” For the analyses reported here, these categories were collapsed into the following three categories: full remission (the first two ratings), partial remission, and continuous illness or new episodes (the last two ratings). Full remission was defined as an 8-week period in which the subject was asymptomatic, regardless of treatment status. Partial remission was defined as having some symptoms of the index episode.
Symptoms were rated at baseline and at 6, 24, and 48 months. Ratings were done with the Brief Psychiatric Rating Scale (BPRS) (9), Scale for the Assessment of Positive Symptoms (SAPS) (10), and Scale for the Assessment of Negative Symptoms (SANS) (11).
After each follow-up wave, a search of the National Death Index database was conducted to assess the vital status of participants who were lost to follow-up. On the basis of these data and further information from family members of the deceased participant, suicidal deaths were identified.
Homelessness ratings were conducted at the 24- and 48-month interviews. Ratings were based on self-reports of any homeless nights during the past 2 years.
Global Functioning
Global functioning at 24 and 48 months was assessed by using a scale adopted from the SADS-L (8). Ratings included “return to highest level of functioning,” “residual impairment,” “considerable residual impairment,” and “chronic condition or marked deterioration.” Project psychiatrists made these ratings with information from interviews, medical records, interviews with significant others, and rating scales.
Satisfaction With Care
The patients’ satisfaction with care was measured at 6 and 24 months by using two questions: 1) How satisfied were you with the quality of services you received? (rated on a scale from 1, quite dissatisfied, to 4, very satisfied) and 2) Did you get the kind of treatment you wanted? (rated on a scale from 1, no, not at all, to 3, yes). Because some patients participated in more than one outpatient program, these questions were asked for as many as three programs. The ratings used here reflect the average across programs. There was no association between the number of programs and the average rating.
Data Analysis
Baseline patient characteristics were compared across six cohorts identified on the basis of the date of admission (patients admitted between September 1, 1989, and August 31, 1990, formed the 1989–1990 cohort, those admitted between September 1, 1990, and August 31, 1991, formed the 1990–1991 cohort, and so on). To assess trends across admission cohorts, the score test for trend was used for categorical variables and Spearman’s rank-order correlation was used for ordinal variables.
Patterns of treatment, illness course, and symptomatic outcomes over the 48 months were compared across admission cohorts by using generalized estimating equations (12). All generalized estimating equation analyses were adjusted for age, gender, race, education, baseline research diagnosis, and facility type at first admission. Interaction terms for admission cohort with follow-up time were also entered into the models. In addition, analyses of service use were adjusted for updated insurance type (insurance type was assessed at baseline and at 6 and 24 months). In models that showed a statistically significant linear relationship between admission cohort and outcome, we further searched for a possible nonlinear relationship by testing for a quadratic term for admission cohort. Generalized estimating equation analyses were conducted with the Stata 7 xtgee routine (13).
Results
Patient and Index Treatment Characteristics
The patients recruited in the six admission cohorts were similar on most sociodemographic and clinical characteristics (Table 1). The proportion of patients recruited from state facilities declined across the admission cohorts, mainly because of downsizing of the major adult state hospital in the county. The length of first hospital stays declined across admission cohorts. Although the reduction in length of stay occurred in all facility types, it was particularly dramatic for state facilities (Figure 1).
Score test for trend showed a statistically significant trend in the proportion of patients discharged “in partial remission” or “having significant symptoms” across successive cohorts (Table 1). The trend for patients discharged “in partial remission” was largely due to a dramatic increase in such ratings between 1991–1992 and 1992–1993. In subsequent cohorts, however, the proportion of such ratings gradually declined. There was also a systematic increase in the proportion of patients discharged to day hospitals (Table 1).
Course of Treatment
Overall, 43% of the patients were rehospitalized at least once during the 48 months of follow-up (the median number of rehospitalizations among those rehospitalized was two, with a range from one to 12). In the generalized estimating equation analyses, the number of inpatient days over the 48 months declined across admission cohorts (B=–1.84, SE=0.49, z=3.78, p<0.001). However, the generalized estimating equation analyses for the number of rehospitalizations assessed every 6 months revealed no significant variations across cohorts. Thus, the decline in the number of inpatient days was likely due to reduced lengths of stay, not reduced frequency of hospitalizations.
The reduction in inpatient days was not associated with increased use of outpatient services. In the generalized estimating equation analyses, the number of day treatment, individual therapy, medication, and overall outpatient visits did not systematically vary across admission cohorts. Furthermore, generalized estimating equation analyses of the global ratings of course of outpatient treatment (conducted every 6 months) suggested a decline across admission cohorts in the proportion of patients in treatment who received “continuous treatment” (adjusted odds ratio=0.90, 95% confidence interval [CI]=0.82–0.99, z=2.23, p<0.03) and an increase in the proportion of patients who received “several brief periods of treatment” (adjusted odds ratio=1.25, 95% CI=1.05–1.49, z=2.50, p<0.02). The proportion of patients with “consultation/brief periods” of outpatient treatment did not change systematically across admission cohorts nor did the proportion of those who received any outpatient treatment versus none.
Course of Illness, Clinical Outcomes, Suicide, and Homelessness
Illness course and clinical outcomes for the most part did not vary systematically across admission cohorts. The generalized estimating equation analyses revealed an increase in the proportion of patients rated as being in “full remission” across admission cohorts (adjusted odds ratio=1.11, 95% CI=1.01–1.21, z=2.17, p=0.03). Further logistic regression analyses revealed that the difference across cohorts was limited to the 6-month assessment (adjusted odds ratio=1.13, 95% CI=1.02–1.26, z=2.28, p<0.03), and there were no significant differences across cohorts at the later assessment points. There were also no systematic variations in the proportion of patients with ratings of “partial remission” or “new episodes during interval/original disorder continued.”
The comparison of symptom severity in the generalized estimating equation analyses revealed no significant differences in the BPRS and SANS scores. However, analysis of the SAPS scores revealed a nonsignificant trend for higher levels of positive symptoms in later cohorts (B=0.03, SE=0.02, z=1.89, p=0.06). Further analyses using linear regressions revealed that the difference in SAPS scores across admission cohorts was limited to the baseline assessment (B=0.06, SE=0.02, z=3.36, p=0.001), and there were no systematic variations at follow-up assessments.
Five (0.9%) of the 573 participants committed suicide over the 48 months of the study (two in the 1990–1991 cohort and one each in the 1989–1990, 1991–1992, and 1993–1994 cohorts). There was no systematic trend in this variable across admission cohorts (score test for trend=1.44, df=1, p=0.23).
At 48 months, 77 (17.1%) of the 450 participants with follow-up data on housing status reported episodes of homelessness since the first discharge. There was no systematic trend in self-reported homelessness across admission cohorts (score test for trend=0.61, df=1, p=0.44).
Global Functioning
Many patients were rated as having “returned to highest level of functioning” at follow-up (44.8% at 24 months and 44.1% at 48 months). In the generalized estimating equation analyses, a significantly higher proportion of patients in the later admission cohorts had this rating (adjusted odds ratio=1.35, 95% CI=1.13–1.63, z=3.20, p=0.001) and a smaller proportion of patients had a rating of “residual impairment” or “considerable residual impairment” (adjusted odds ratio=0.79, 95% CI=0.65–0.96, z=2.33, p=0.02). The proportion of patients with a rating of “chronic condition or marked deterioration” did not vary systematically across cohorts.
Satisfaction With Care
No differences across admission cohorts were found for satisfaction with care. Overall, 22.6% of the patients at 6 months and 43.7% at 24 months stated that they were “very satisfied” with their services. Also, 40.5% of the patients at 6 months and 64.8% at 24 months stated that they had received the kind of treatment that they wanted. The increase in the proportion of satisfied patients with time may be an artifact of treatment dropout of unsatisfied patients, as only the patients who received treatment during the interval were asked about satisfaction with care. Further analyses showed that a low level of satisfaction at 6 months was associated with a higher likelihood of dropping out of treatment during the next 6 months (satisfaction with services: odds ratio=1.65, 95% CI=1.21–2.24, z=3.18, p=0.001; receiving the kind of treatment that was wanted: odds ratio=2.66, 95% CI=1.78–3.98, z=4.76, p<0.001). Similarly, a low level of satisfaction at 24 months was associated with dropping out of treatment during the next 6 months (satisfaction with services: odds ratio=2.24, 95% CI=1.36–3.68, z=3.16, p=0.002; receiving the kind of treatment that was wanted: odds ratio=3.60, 95% CI=1.95–6.65, z=4.09, p<0.001).
Discussion
During the years of study, the mental health care system in Suffolk County, N.Y., and across the United States underwent drastic changes. One major element of these changes was the reduction in the length of inpatient stays. In New York State, these changes were expedited by a new policy initiative—the Community Reinvestment Act of 1993—that was intended to divert funds from inpatient care to outpatient and community-based services (14).
Changes in the use of inpatient services are reflected in our data. The average length of inpatient stays declined drastically across admission cohorts spanning the 1989–1995 period. We also observed a systematic change in the characteristics of first-admission patients hospitalized in Suffolk County across the 6 admission years. Patients in later cohorts had more severe positive symptoms at admission. This difference was probably due to changes in admission policies over this period, as patients who were less severely ill were increasingly less likely to be admitted into hospitals (2).
Both the reduction in the length of hospital stays and the change in the characteristics of patients suggest a shift in the role of inpatient care in the management of severely mentally ill patients. Inpatient services were increasingly used for short-term emergency management of more severely ill patients, and patients with less severe illness were shifted to less intensive settings. Probably as a result of these changes, patients discharged in later years may have been more symptomatic. This pattern was not very clear in our data, as the trend for patients discharged “in partial remission” was largely due to a dramatic increase in such ratings between 1991–1992 and 1992–1993, and, in subsequent cohorts, the proportion of such ratings gradually declined. However, this trend was clearly shown in another study of three cohorts of depressed inpatients discharged between years 1988 and 1996, in which patients who were admitted in later years and who had shorter stays had more symptoms and a lower level of functioning after discharge (15).
Despite the reduced length of inpatient stays over the period of the study, no corresponding increase in the use of outpatient services was found. Although more patients in later admission cohorts were referred to day treatment, this pattern did not translate into increased use of day treatment services. Moreover, continuity of outpatient care, rated globally, did not improve in later admission cohorts. If anything, fewer patients in later cohorts received continuous outpatient treatment. These findings are consistent with the results of a study of a national cohort of privately insured patients that also found no increase in utilization of outpatient services after reduction in inpatient service use (3).
It is noteworthy, however, that the patients admitted during later years experienced a speedy symptomatic recovery after discharge from their first admission and by the 6-month follow-up had symptom measures that were virtually indistinguishable from those of the patients admitted in earlier years. There was also no evidence that the course of illness in later admission cohorts was poorer than that in earlier cohorts. In fact, global measures showed a puzzling trend for patients admitted in later years to function better than those admitted in earlier years.
Although we do not have a ready explanation for these findings, it seems plausible that changes in the structure and content of services in the early to mid-1990s and, most importantly, the drastic reduction in the length of inpatient stays in this period did not adversely affect patient outcomes in the short run. We also did not observe any meaningful trends in rates of suicide and homelessness across admission cohorts. Finally, among patients who remained in care, satisfaction with services did not vary systematically across cohorts.
During the course of the study, admissions to state facilities and, as a result, the proportion of state facility patients in this sample declined dramatically. Because patients admitted to state facilities traditionally have fewer resources and experience poorer course and outcomes, the smaller numbers of such patients in later cohorts could potentially confound the results. However, when the analyses were conducted separately for participants recruited from state facilities and from other facilities, the results were essentially similar to the main results reported here.
As the total number of inpatient psychiatric admissions in Suffolk County declined during the years of the study (16), the proportion of patients with early psychotic disorders who were admitted also likely declined in later years. Many of these patients may have received care in less intensive settings or in criminal justice settings. However, it is unlikely that sample selection could explain the findings of the study because the patients admitted in later years, if anything, appeared to be more severely ill than those admitted in earlier years.
Another possible explanation for the findings of similar course and outcome at follow-up across admission cohorts despite the more severe presentation at baseline and shorter stays in later cohorts is that the potentially negative effects of these factors were offset by the possible improvements in the content of outpatient services in later years, including the introduction of atypical antipsychotic medications. In our sample, only 19.6% of the patients ever received such medications over the 48 months. Repeating the analyses after excluding these participants produced results similar to those reported here; thus the findings cannot be attributed to the use of these medications. Nevertheless, changes in other aspects of outpatient care remain a possible explanation to be explored in future research. For instance, some evidence suggests a shift toward more time-limited and behavioral psychosocial interventions during this period at least in community mental health centers (17).
It is also plausible that the reduced length of inpatient stays had a positive effect on the course and outcome of psychotic disorders. Past research on the relationship between length of inpatient stays and clinical and social outcomes produced conflicting results (15, 18–22). Perhaps most relevant to the present study are the results of the McLean First-Episode Psychosis Project, which recruited patients in a time frame similar to the Suffolk County Mental Health Project. That study also recorded a dramatic reduction in average length of stay during the study period (22). But neither time to syndromal recovery nor the proportion of patients attaining syndromal recovery by 2 years varied systematically across the admission cohorts.
In interpreting the results of our study, some limitations should be considered. First, although the Suffolk County Mental Health Project obtained consensus longitudinal diagnoses, we used only the baseline diagnoses in this report to limit the potential effect of course of illness on diagnostic decisions. It is noteworthy, however, that adjustment of the analyses for the 24-month consensus diagnoses did not substantially change the results of the study. Furthermore, the results of analyses after stratification of the data based on the 24-month diagnoses (schizophrenia versus other) were mainly consistent with the results reported here. One notable difference in the subgroup of participants with a 24-month diagnosis of schizophrenia was higher SANS scores in later cohorts. However, this variation was limited to the baseline assessment and did not persist at later assessment points, which suggests that the participants with schizophrenia admitted in later years were more symptomatic at baseline. Second, the scope of measures of service use in this study was limited. Future studies need to examine other domains, including the process and the quality of care (17), use of informal care providers, and use of other services in the community. Finally, future studies also need to examine any possible shift of the burden of care to the criminal justice system in this time frame.
In conclusion, the results of this study contain a mixed message for clinicians and policy makers. On the one hand, the shorter hospital stays and higher likelihood of partial remission or nonremission at the time of discharge call for more attention to provision of community-based support services, including reliable linkage mechanisms that enhance continuation of aftercare in outpatient settings. Simple linking interventions (23) and focused case management programs (24) have shown promising results. The prominent role of families in the care of patients with severe mental disorders also calls for greater attention to supportive and educational family interventions.
On the other hand, it is reassuring to know that shorter hospital stays did not negatively affect the short-term course and outcome of psychotic disorders and that for most patients in the early course of illness, resources available in the community provided adequate substitutes for hospital care.
 |
Received April 29, 2003; revisions received Dec. 10, 2003, and March 31, 2004; accepted Aug. 9, 2004. From the Department of Psychiatry, Beth Israel Medical Center; the Departments of Psychiatry and Epidemiology, Mailman School of Public Health, Columbia University, New York; Montefiore Medical Center and Albert Einstein College of Medicine, Bronx, N.Y.; Department of Veterans Affairs, Office of Quality and Performance, Washington, D.C.; Hillside Hospital, Glen Oaks, N.Y.; and the Department of Psychiatry and Behavioral Science, State University of New York at Stony Brook, Stony Brook, N.Y. Address correspondence and reprint requests to Dr. Mojtabai, Department of Psychiatry, Beth Israel Medical Center, First Ave. at 16th St., New York, NY 10010; [email protected] (e-mail). Supported in part by NIMH grants MH-01754 and MH-44801.
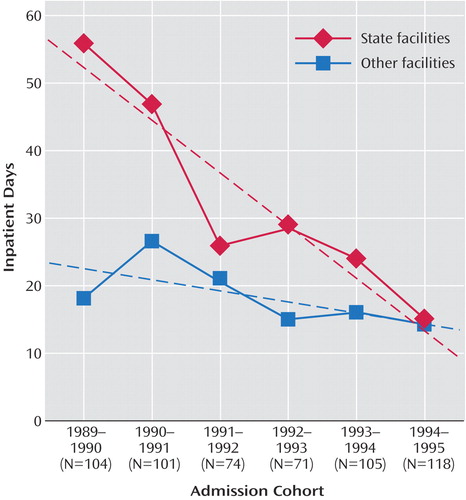
Figure 1. Median Lengths of First-Admission Stays for Patients Hospitalized in State and Other Facilities in the Suffolk County Mental Health Project, 1989–1995a
aDotted lines represent time trends based on fitted regression models.
1. Mechanic D: Mental Health and Social Policy: The Emergence of Managed Care. Needham Heights, Mass, Allyn & Bacon, 1999Google Scholar
2. Mechanic D, McAlpine DD, Olfson M: Changing patterns of psychiatric inpatient care in the United States, 1988–1994. Arch Gen Psychiatry 1998; 55:785–791Crossref, Medline, Google Scholar
3. Leslie DL, Rosenheck R: Shifting to outpatient care? mental health care use and cost under private insurance. Am J Psychiatry 1999; 156:1250–1257Abstract, Google Scholar
4. Bromet E, Schwartz J, Fennig S, Geller L, Jandorf L, Kovasznay B, Lavelle J, Miller A, Pato C, Ram R, Rich C: The epidemiology of psychosis: the Suffolk County Mental Health Project. Schizophr Bull 1992; 18:243–255Crossref, Medline, Google Scholar
5. Spitzer RL, Williams JBW, Gibbon M, First MB: The Structured Clinical Interview for DSM-III-R (SCID), I: history, rationale, and description. Arch Gen Psychiatry 1992; 49:624–629Crossref, Medline, Google Scholar
6. Strauss JS, Carpenter WT: Predictors of outcome in schizophrenia, II: relationship between predictor and outcome variables. Arch Gen Psychiatry 1974; 31:37–42Crossref, Medline, Google Scholar
7. Rabinowitz J, Bromet EJ, Lavelle J, Severance KJ, Zariello SL, Rosen B: Relationship between type of insurance and care during the early course of psychosis. Am J Psychiatry 1998; 155:1392–1397Link, Google Scholar
8. Endicott J, Spitzer RL: A diagnostic interview: the Schedule for Affective Disorders and Schizophrenia. Arch Gen Psychiatry 1978; 35:837–844Crossref, Medline, Google Scholar
9. Woerner MG, Mennuzza S, Kane JM: Anchoring the BPRS: an aid to improved reliability. Psychopharmacol Bull 1988; 24:112–117Medline, Google Scholar
10. Andreasen NC: Scale for the Assessment of Positive Symptoms (SAPS). Iowa City, University of Iowa, 1984Google Scholar
11. Andreasen NC: Scale for the Assessment of Negative Symptoms (SANS). Iowa City, University of Iowa, 1983Google Scholar
12. Carr GJ, Chi EM: Analysis of variance for repeated measures: data: a generalized estimating equations approach. Stat Med 1992; 11:1033–1040Crossref, Medline, Google Scholar
13. Stata Reference Manual: Release 7.0. College Station, Tex, Stata Corp, 2001Google Scholar
14. New York State Office of Mental Health: Reinvestment’s First Five Years, 2000. http://www.omh.state.ny.us/omhweb/omhq/q1299/reinvestment%5Freview.htmGoogle Scholar
15. Lieberman PB, Wiitala SA, Elliott B, McCormick S, Goyette SB: Decreasing length of stay: are there effects on outcomes of psychiatric hospitalization? Am J Psychiatry 1998; 155:905–909Link, Google Scholar
16. Mental Health Statistics Unit, New York State Office of Mental Health: 2000 New York State Chartbook of Mental Health Information. http://www.omh.state.ny.us/omhweb/chartbook/text.htmGoogle Scholar
17. Cypres A, Landsberg G, Spellman M: The impact of managed care on community mental health outpatient services in New York State. Adm Policy Ment Health 1997; 24:509–521Crossref, Medline, Google Scholar
18. Riessman CK, Rabkin JG, Struening EL: Brief versus standard psychiatric hospitalization: a critical review of the literature. Community Ment Health Rev 1977; 2:1–10Crossref, Google Scholar
19. Heeren O, Dixon L, Gavirneni S, Regenold WT: The association between decreasing length of stay and readmission rate on a psychogeriatric unit. Psychiatr Serv 2002; 53:76–79Link, Google Scholar
20. Craig TJ, Fennig S, Tanenberg-Karant M, Bromet EJ: Rapid versus delayed readmission in first-admission psychosis: quality indicators for managed care? Ann Clin Psychiatry 2000; 12:233–238Crossref, Medline, Google Scholar
21. Mojtabai R, Nicholson RA, Neesmith DH: Factors affecting relapse in patients discharged from a public hospital: results from survival analysis. Psychiatr Q 1997; 68:117–129Crossref, Medline, Google Scholar
22. Tohen M, Hennen J, Zarate CM Jr, Baldessarini RJ, Strakowski SM, Stoll AL, Faedda GL, Suppes T, Gebre-Medhin P, Cohen BM: Two-year syndromal and functional recovery in 219 cases of first-episode major affective disorder with psychotic features. Am J Psychiatry 2000; 157:220–228Link, Google Scholar
23. Olfson M, Mechanic D, Boyer CA, Hansell S: Linking inpatients with schizophrenia to outpatient care. Psychiatr Serv 1998; 49:911–917Link, Google Scholar
24. Susser E, Valencia E, Conover S, Felix A, Tsai WY, Wyatt RJ: Preventing recurrent homelessness among mentally ill men: a “critical time” intervention after discharge from a shelter. Am J Public Health 1997; 87:256–262Crossref, Medline, Google Scholar



