The Longitudinal Course of Thought Disorder in Geriatric Patients With Chronic Schizophrenia
Abstract
OBJECTIVE: This study longitudinally assessed previously validated dimensions of thought disorder—verbal underproductivity and disconnection—in geriatric schizophrenia and replicated previous cross-sectional differences in communication disorders. METHOD: Two hundred twenty patients with chronic schizophrenia were assessed with the Thought, Language, and Communication Scale over a mean follow-up period of 2.3 years. RESULTS: Patients had increases in verbal underproductivity but stable scores on disconnection over the follow-up period. Worsening in verbal underproductivity was associated with concurrent worsening in Mini-Mental State Examination scores and older age at baseline. CONCLUSIONS: Verbal underproductivity worsens with aging and is associated with cognitive worsening, although disconnected speech is relatively stable. Some geriatric patients with schizophrenia may lose the skills necessary to report symptoms, leading to the impression that their clinical status is improving.
Communication in schizophrenia is commonly characterized by several types of abnormalities, referred to as “formal thought disorder.” Positive thought disorder (also referred to as “disconnection” or “disorganization syndrome”) involves abnormalities in the production of language, such as derailment and tangentiality, whereas negative thought disorder denotes a reduction in the amount of overall output or information in speech, which includes poverty of content of speech and poverty of speech. Empirical studies of the structure of communication disorders have indicated that poverty of content of speech is actually associated with disconnection and not verbal productivity (1).
The longitudinal course of thought disorder is not well understood. Thought disorder was found to be stable during the early stages of an acute psychotic episode (2), and the severity of both poverty of speech and disconnected speech remain stable across an acute episode (3) and a subsequent 8-month follow-up (4). Addressing the long-term course of communication disorders, Harvey et al. (5) examined age-related differences in formal thought disorder in a cross-sectional study of schizophrenia patients who ranged in age from 19 to 96. Poverty of speech was found to be more common and severe in geriatric patients. However, the disconnection component was less severe in geriatric patients. Further analyses indicated that this lower severity of disconnection was not due to differences in verbal output. Cognitive impairment was found to predict poverty of speech. These findings tentatively suggest that disconnection and poverty of speech in schizophrenia, despite being generally stable over time, may change with age and possibly with level of cognitive functioning.
The present study is a longitudinal examination of the course of these two dimensions of thought disorder in older patients with schizophrenia. Based on previous findings, we hypothesized that
| 1. | Poverty of speech will worsen over time. | ||||
| 2. | Disconnection will remain stable or improve over time. | ||||
| 3. | Age and cognitive impairment will predict the baseline severity and subsequent course of poverty of speech. | ||||
Method
As part of a longitudinal study of chronic schizophrenia described elsewhere (5, 6), we selected schizophrenia patients who had follow-up assessments on the measures described.
We identified 799 schizophrenia patients at baseline and 220 with follow-up assessments. Patients were lost to follow-up because of uncooperativeness of the patient (N=87), death of the patient (N=290), or discharge to a noncooperative treatment site (N=202). The mean follow-up interval was 842 days (SD=489, range=362–2,264). Among the patients with follow-up data, 127 (57.7%) were women; the group had a mean age of 74.9 (SD=9.4, range=49–97) at baseline, a mean of 10.2 years (SD=2.7) of education, and a mean age at first hospitalization of 27.6 (SD=10.9). One hundred forty-three were residents of a psychiatric hospital for chronic illness, and 57 were residents of a nursing home who had been discharged from a psychiatric hospital for chronic illness. Exactly 77.7% of the patients were Caucasian, 16.4% were African American, and 5.9% were Hispanic. All were English speaking, without sensory deficits, and cooperative with the assessment procedures.
In this study, we report on the results of the patients’ performance on the Mini-Mental State Examination (MMSE) (7) and the interviewers’ ratings of thought disorder on the Thought, Language, and Communication Scale (8, 9). The Thought, Language, and Communication Scale ratings were based on a symptom interview and unscripted conversation with the patients at the time of the assessments. The Thought, Language, and Communication Scale provides definitions and criteria for 18 subtypes of abnormal language. For the present report, we were interested in two previously confirmed (1) subtypes of thought disorder, disconnection and verbal underproductivity. The disconnection subscale is the sum of the following Thought, Language, and Communication Scale items: poverty of content of speech, derailment, tangentiality, loss of goal, circumstantiality, and incoherence (1). Verbal productivity was examined with the poverty of speech item. The aspects of speech performance reported here were found in a previous study to have suitable interrater reliability (all intraclass correlation coefficients >0.56, range=0.56–0.91) in older patients with schizophrenia with our raters, who were blind to the present hypotheses (5).
We used repeated-measures analyses of variance (ANOVAS) to examine changes in the language and cognitive variables over time. To examine changes in disconnection, we selected only patients who were verbally productive (severity of poverty of speech <3) and entered changes in poverty of speech as a covariate to determine if changes in disconnection were independent of changes in verbal underproductivity. We examined the association between verbal underproductivity, disconnected speech, MMSE scores, and gender and compared changes in verbal productivity, disconnection, and MMSE scores in younger and older patients. For this final analysis, we used a median split at age 74 as the between-subject factor. These two groups were equivalent in time between assessments (t=–1.23, df=180, p=0.22).
Results
A multivariate ANOVA to examine baseline differences in cognition, poverty of speech, disconnection, age, and age at first hospitalization between those who were reevaluated and those who were lost to follow-up was not significant (Pillai’s trace F=1.75, df=5, 550, p=0.12).
The patients displayed worsening in verbal underproductivity over time, with mean poverty of speech ratings of 1.9 (SD=1.4) at baseline and 2.3 (SD=1.4) at follow-up (Pillai’s trace F=13.3, df=1, 219, p<0.001, Wilks’s lambda=0.94). Only 5% of the patients displayed improvements in poverty of speech; the majority (74%) who improved did so by 1 point. Verbally productive patients demonstrated improved disconnection from baseline (mean=4.8, SD=4.7) to follow-up (mean=3.7, SD=4.4) (Pillai’s trace F=4.9, df=1, 124, p<0.03, Wilks’s lambda=0.96). However, when entering change in poverty of speech as a covariate, this finding was no longer significant (Pillai’s trace F=0.64, df=1, 124, p=0.43, Wilks’s lambda=0.99). MMSE scores were stable for the group as a whole from baseline (mean=11.4, SD=9.8) to follow-up (mean=12.1, SD=10.2) (Pillai’s trace F=1.3, df=1, 188, p=0.26, Wilks’s lambda=0.99).
Poverty of speech was associated with MMSE scores at baseline (r=–0.60, p<0.001) and follow-up (r=–0.58, p<0.001) and severity scores on disconnection at baseline (r=–0.45, p<0.001) and follow-up (r=–0.35, p<0.001). Worsening in poverty of speech was correlated with decreases in MMSE scores (r=–0.30, p<0.03) and greater age at baseline (r=–0.15, p<0.03) but not years of education, medication status (none, typical or atypical antipsychotic), or age at first hospitalization. Disconnection was not significantly associated with MMSE scores at baseline (r=0.03, p=0.71) or follow-up (r=0.04, p=0.60). Gender was not significantly associated with disconnection at baseline (rpoint biserial=0.03, p=0.40) or endpoint (rpoint biserial=0.05, p=0.51).
In the repeated-measures ANOVA examining changes in poverty of speech by age, the main effect of change in poverty of speech was significant (Pillai’s trace F=22.1, df=1, 180, p<0.001, Wilks’s lambda=0.89). The interaction between poverty of speech and age was significant (Pillai’s trace F=4.04, df=1, 180, p=0.04, Wilks’s lambda=0.97). As demonstrated in Figure 1, this interaction effect suggests that the older group had a greater worsening in verbal underproductivity over time. The repeated-measures ANOVA examining changes in disconnection by age was not significant (Pillai’s trace F=2.9, df=1, 180, p=0.09, Wilks’s lambda=0.98). The repeated-measures ANOVA examining changes in MMSE by age was also not significant (Pillai’s trace F=1.4, df=1, 180, p=0.25, Wilks’s lambda=0.99).
Discussion
Older schizophrenia patients with a chronic course of illness show decreases in verbal productivity over time, with this change predicted by worsening in MMSE scores. Improvement in verbal productivity over time was rare and minimal. Scores on the disconnection scale indicated an improvement over time; however, this change is an artifact of decreases in output. It may be more accurate to refer to this “improvement” as a shift in the behavioral topography of communication disorders, from disconnected to unproductive speech, as patients age. Viewed this way, thought disorder does not appear to “burn out” in chronic schizophrenia.
Age-related differences in thought disorder were noted in the cross-sectional study (5), and the present longitudinal study confirms a worsening in poverty of speech over time in the truly geriatric patients. The reduction in verbal output over time complements previous work that has suggested a decline in cognitive and functional skills during this age range (10), particularly in frontal “executive” functions (11), as poverty of speech is associated with dorsolateral prefrontal cortex dysfunction (12). Reduced verbal output also suggests that findings of improvement in positive and disorganized symptoms with aging in schizophrenia should be carefully considered in the context of possible reductions in verbal productivity. Decreased verbal output may affect one’s ability to report hallucinations and delusions, as well as reducing the tendency to produce aberrant language. Future studies may address some of the limitations of this study, such as the influence of physical illnesses on thought disorder in late life.
Received March 1, 2004; revision received May 31, 2004; accepted June 10, 2004. From the Department of Psychiatry, Mount Sinai School of Medicine. Address correspondence and reprint requests to Dr. Bowie, Department of Psychiatry, Mount Sinai School of Medicine, 1425 Madison Ave, 4th Floor, Box 1230, New York, NY 10029; [email protected] (e-mail). Funded by the Mount Sinai Mental Health Clinical Research Center on Late-Life Schizophrenia (K.L. Davis, principal investigator), the Silvio Conte Neuroscience Center (NIMH grant MH-36692; K.L. Davis, principal investigator), NIMH grant 63116 (Dr. Harvey, principal investigator), and the VA Veterans Integrated Service Network 3 Mental Illness Research, Education, and Clinical Center.
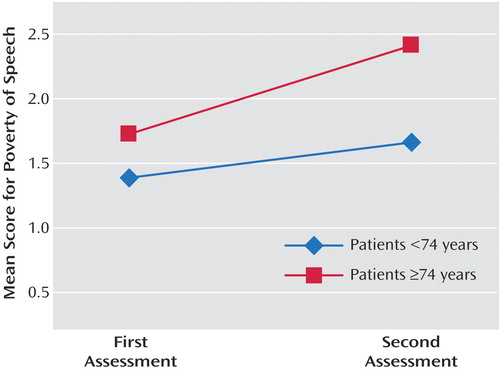
Figure 1. Change in Poverty of Speech by Age in Geriatric Patients With Chronic Schizophrenia
1. Harvey PD, Lenzenweger MF, Keefe RS, Pogge DL, Serper MR, Mohs RC: Empirical assessment of the factorial structure of clinical symptoms in schizophrenic patients: formal thought disorder. Psychiatry Res 1992; 44:141–151Crossref, Medline, Google Scholar
2. Harvey PD, Earle-Boyer EA, Wieglus MS: The consistency of thought disorder in mania and schizophrenia: an assessment of acute psychotics. J Nerv Ment Dis 1984; 172:458–463Crossref, Medline, Google Scholar
3. Earle-Boyer EA, Levinson JC, Grant R, Harvey PD: The consistence of thought disorder in mania and schizophrenia, II: an assessment of consecutive admissions. J Nerv Ment Dis 1986; 174:443–447Crossref, Medline, Google Scholar
4. Harvey PD, Docherty NM, Serper MR, Rasmussen M: Cognitive deficits and thought disorder, II: an 8-month followup study. Schizophr Bull 1990; 16:147–156Crossref, Medline, Google Scholar
5. Harvey PD, Lombardi J, Leibman M, Parrella M, White L, Powchick P, Mohs RC, Davidson M, Davis KL: Age-related differences in formal thought disorder in chronically hospitalized schizophrenic patients: a cross-sectional study across nine decades. Am J Psychiatry 1997; 154:205–210Link, Google Scholar
6. Davidson M, Harvey PD, Powchick P, Parrella M, White L, Knobler HY, Losonczy MF, Keefe RS, Katz S, Frecska E: Severity of symptoms in chronically institutionalized geriatric schizophrenic patients. Am J Psychiatry 1995; 152:197–207Link, Google Scholar
7. Folstein MF, Folstein SE, McHugh PR: “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12:189–198Crossref, Medline, Google Scholar
8. Andreasen NC: Thought, language, and communication disorders, I: clinical assessment, definition of terms and evaluation of their reliability. Arch Gen Psychiatry 1979; 36:1315–1321Crossref, Medline, Google Scholar
9. Andreasen NC: Thought, language, and communication disorders, II: diagnostic significance. Arch Gen Psychiatry 1979; 36:1325–1330Crossref, Medline, Google Scholar
10. Friedman JI, Harvey PD, Coleman T, Moriarty PJ, Bowie C, Parrella M, White L, Adler D, Davis KL: Six-year follow-up study of cognitive and functional status across the lifespan in schizophrenia: a comparison with Alzheimer’s disease and normal aging. Am J Psychiatry 2001; 158:1441–1448Link, Google Scholar
11. Fucetola R, Seidman LJ, Kremen WS, Faraone SV, Goldstein JM, Tsuang MT: Age and neuropsychologic function in schizophrenia: a decline in executive abilities beyond that observed in healthy volunteers. Biol Psychiatry 2000; 48:137–146Crossref, Medline, Google Scholar
12. Dolan RJ, Bench CJ, Liddle PF, Friston KJ, Frith CD, Grasby PM, Frackowiak RS: Dorsolateral prefrontal cortex dysfunction in the major psychoses; symptom or disease specificity? J Neurol Neurosurg Psychiatry 1993; 56:1290–1294Crossref, Medline, Google Scholar



