Sex Differences in Functional Connectivity in First-Episode and Chronic Schizophrenia Patients
Abstract
OBJECTIVE: There has been consistent evidence for a lower incidence and milder course of schizophrenia in women, yet there have been very few investigations of sex differences in brain function in this disorder. This study used a new high-temporal-resolution measure of functional brain connectivity to test the prediction that female patients would show relatively greater inter- and intrahemispheric connectivity than male patients, particularly in the early stage of schizophrenia. METHOD: Forty patients with chronic schizophrenia (20 women and 20 men) and 24 patients with first-episode schizophrenia (12 women and 12 men) and their respective matched comparison groups completed a conventional auditory oddball task. Phase synchronous gamma (40 Hz) activity was extracted from EEG recording during the task and time-locked to the oddball (target) stimuli. RESULTS: Chronic schizophrenia subjects showed a reduction in global functional connectivity (lower gamma phase synchrony) relative to their matched healthy subjects. Unexpectedly, this reduction was most apparent in female patients. By contrast, while first-episode patients showed a general reduction in the speed of frontal connectivity, the speed of global connectivity was relatively faster in female patients. CONCLUSIONS: This is the first study to investigate sex differences in schizophrenia that used the functional connectivity measure of gamma phase synchrony. The results suggest that in female patients with schizophrenia, additional breakdowns in brain network connectivity may develop with illness chronicity.
Recently, there has been a resurgence in attention to sex differences in schizophrenia, reflecting the important contribution of these differences to the heterogeneity of schizophrenia phenomenology (for review, see references 1–4).
The majority of investigations have focused on sex differences in the epidemiology and clinical expression of schizophrenia. These studies have observed a consistent two- to three-fold increase in the incidence of schizophrenia in men versus women when the DSM-IV criterion of age at onset before 45 years is adopted (5). Indeed, as early as 1896, Kraepelin noted that “men appear to be three times more likely to suffer from the illness” (6). Men with schizophrenia also exhibit more negative symptoms than do women (7) and experience an earlier age at onset (of about 3–5 years) that is consistent across different cultures (8), definitions of psychosis onset (9), and diagnostic tools (10).
Another large set of studies has addressed sex differences in schizophrenia in relation to neuroanatomical deficits. The consensus from these studies, despite the use of different brain imaging methodologies, is that male subjects with schizophrenia exhibit greater structural brain abnormalities than do female schizophrenia subjects (11). Key neuroanatomical abnormalities include larger ventricle-brain ratios (12), reduced gray matter volume—particularly in temporolimbic structures (13), and a lack of the normal asymmetry shown by healthy male subjects (14). Male schizophrenia patients also display a greater rate of minor physical anomalies and neurological soft signs than do female patients (15).
By comparison, a smaller number of studies have examined sex differences in schizophrenia in relation to brain function. In general, men show a greater deviation than do women across neuropsychological tests of cognitive function (16) as well as a reduction in regional cerebral blood flow (17). To date, very few investigations of sex differences in schizophrenia have been published that have used high-temporal-resolution measures such as EEG (18, 19). In a previous investigation, Turetsky et al. (20) reported significant sex differences in the event-related potentials of patients with schizophrenia. Results revealed a dissociation by sex in the P300 event-related potential: while male subjects exhibited a reduced P300 in the right parietal region, female subjects showed a greater deficit in the anterior (frontal) region.
Given the dearth of neurophysiological investigation into sex differences in schizophrenia, we focused for the first time in this study on sex-related variation in functional brain connectivity. We employed a measure of high-frequency synchronous brain activity—40-Hz gamma phase synchrony (21)—extracted from the EEG recordings. Disturbances of functional integration have been recognized as a fundamental characteristic of schizophrenia since the earliest attempts to describe this disorder in terms of “loss of the inner unity” and a disturbance in the “intrapsychic coordination” of mental activities (22). Previous models of schizophrenia have postulated that the abnormal temporal integration of brain networks underlies the core failure of cognitive coordination (or “cognitive dysmetria”) in this disorder (23, 24).
Synchronous gamma activity has been observed in animal and human studies, and across microscopic and macroscopic scales of recording, using both depth-electrode and scalp-recorded EEG (for a review, see reference 25). It has been proposed that in-phase synchronous gamma activity may be a mechanism involved in the “binding problem.” This refers to the manner in which the brain is able to integrate or bind together the diverse neuronal activities relating to a single stimulus among the vast array of parallel processing occurring at any given time (26).
In-phase synchronous gamma oscillations in scalp-recorded EEG activity are distinct from the power (or amplitude) of this activity. Our preliminary investigation of sex differences in patients with chronic schizophrenia focused on gamma power (27). Schizophrenia patients as a group exhibited decreased gamma power frontally and in the left hemisphere, consistent with previous reports (28–30). However, no sex differences in gamma power were observed. It was postulated that the measure of power may fail to reveal more specific sex-related variation in functional connectivity or that the sample may have comprised a more severely ill spectrum of women with chronic schizophrenia. To address these issues, this study examined sex differences in gamma phase synchrony in patients with first-episode schizophrenia as well as those with chronic schizophrenia.
Studies of brain structure in healthy subjects may provide some basis from which to speculate about the normal pattern of sex differences in gamma phase synchrony. Of particular relevance are neuroanatomical and cytoarchitectural morphometry studies demonstrating greater inter- and intrahemispheric connectivity in healthy women compared with men (31, 32). Furthermore, healthy women have been shown to exhibit greater EEG power and coherence than do men (33). Therefore, we predicted that healthy women would show greater functional connectivity than men, reflected in greater intra- and interhemispheric gamma phase synchrony. While both chronic and first-episode schizophrenia patients would show an abnormal pattern of gamma phase synchrony, women with first-episode schizophrenia would exhibit relatively greater functional connectivity in terms of gamma phase synchrony.
Method
Subjects
Forty patients with chronic schizophrenia (20 men [mean age=33.9, SD=7.9] and 20 women [mean age=34.4, SD=8.5]) and 24 subjects in their first episode of schizophrenia (12 men [mean age=19.0, SD=2.5] and 12 women [mean age=19.7, SD=4.2]) took part. Diagnosis of schizophrenia was confirmed by using section G (schizophrenia and psychotic disorders) of the Composite International Diagnostic Interview and consensus of three psychiatrists (two independent from the study), according to DSM-IV and ICD-10 criteria. The additional criterion for the first-episode schizophrenia group was first presentation to health services with psychotic symptoms that warranted such a diagnosis. Confirmatory information for the first-episode schizophrenia diagnosis was provided by interviews with family and case managers (including case notes).
An equal number of healthy comparison subjects were matched in age (within 3 years) and sex to subjects in each of the schizophrenia groups. For the healthy subjects matched to the chronic schizophrenia group, the mean age was 34.1 years (SD=9.1) for the men and 34.1 years (SD=9.3) for the women. For the healthy subjects matched to the first-episode group, the mean age was 19.8 years (SD=3.6) for the men and 19.9 years (SD=3.2) for the women.
Exclusion criteria for all subjects were left-handedness (34), neurological disorder or head injury, mental retardation, and meeting DSM-IV criteria for drug dependence, assessed by using Composite International Diagnostic Interview section M and the Westmead Hospital Clinical Information Base (35). The healthy subjects were also screened for history of a psychiatric illness (in themselves or in a first-degree relative) or treatment with psychiatric medication. IQ equivalence for all subjects (patients and healthy subjects) was greater than 85 as assessed by the Wide Range Achievement Test (36) and was therefore within the normal range.
Table 1 summarizes the clinical data, including medication dosage, duration of illness, and symptom ratings for both the chronic and first-episode schizophrenia groups. Schizophrenia symptoms were rated with the Positive and Negative Syndrome Scale (37). Medication dosage was measured in terms of chlorpromazine equivalents (38). Because male subjects in the chronic schizophrenia group were receiving higher medication doses than were the female subjects (t=2.04, df=38, p<0.05), dosage was controlled in the focal analyses. Male subjects in the first-episode schizophrenia group exhibited more severe negative symptoms than did female subjects (t=5.88, df=22, p<0.03), which was also controlled in the focal analyses.
All subjects were asked to refrain from smoking or drinking caffeinated beverages for at least 3 hours before testing. After a complete description of the study to the subjects, written informed consent was obtained in accordance with National Health and Medical Research Council guidelines.
Experimental Task
EEG data were acquired using a standard auditory “oddball” paradigm. Stereo headphones conveyed regular tones at a constant interval of 1.3 seconds to both ears. Eighty-five percent were 1000-Hz “background” (task-irrelevant) and 15% were “target” (task-relevant) tones of 1500 Hz. All tones were presented at 80 dB above the subject’s auditory threshold (determined before recording). Target tones were randomly intermixed with backgrounds, with the only constraint being that two targets were never presented in succession. Subjects were instructed to respond to the target tones as quickly and as accurately as possible by pressing two reaction time buttons with the index finger of each hand (to counterbalance motor effects).
EEG Data Acquisition
All subjects were seated in a sound- and light-attenuated room. An electrode cap (39) was used to acquire data from Fp1, Fp2, F7, F3, Fz, F4, F8, T3, C3, Cz, C4, T4, T5, P3, Pz, P4, T6, O1, and O2 scalp sites. Linked earlobes served as the reference. Horizontal eye movement potentials were recorded by using two electrodes placed 1 cm lateral to the outer canthus of each eye. Vertical eye movement potentials were recorded by using two electrodes placed on the middle of the supraorbital and infraorbital regions of the left eye. Skin resistance at each site was <5 kΩ. A continuous acquisition system was employed, and data were electro-oculogram-corrected offline (40). The sampling rate was 250 Hz. A low-pass filter was applied to the signals before digitization. The cutoff for this filter was 50 Hz, with attenuation being 40 dB/decade above 50 Hz. In addition, a 50-Hz notch filter was applied to eliminate interference from the 50-Hz alternating current main power supply.
Each subject was instructed to keep their eyes open and to look at a colored dot in the center of the screen in order to minimize eye movements during presentation of tone stimuli. The recording session continued until 40 correctly identified target epochs were acquired.
Gamma Data Reduction
Only correctly identified target epochs for which a button press was obtained within 1 second of the target tone (total of 40) were scored. For each target epoch, from each recording site, a 64-sample Welch window was moved along sample by sample, starting with the center of the Welch window at 500 msec before the stimulus (–500 msec) and ending with the center of the Welch window at 750 msec after the stimulus. Linear trends were first removed by subtracting the line of best fit over all samples centered at stimulus presentation. At each sample position, gamma frequency was computed by means of fast Fourier transformation (41). Frequency bins of 3.91 Hz ranged within a narrow band of gamma activity from 37.1 to 41.0 Hz, which encompasses the focal frequency of 40 Hz and were centered at 39.1 Hz (42). Phase synchronicity was then estimated at each time point by taking the phase estimates across each site of interest at a given time and computing the circular variance of these phase estimates (43). This yielded a single-scale estimate of the extent of phase locking across these sites for each point in time. The result was a time series of gamma phase synchronicity across the sites in question. Five such time series were derived for each epoch, one for global (all sites) synchronicity and four regional synchronicity waveforms: frontal (Fp1, Fp2, Fz, F3, F4, F7, and F8), posterior (O1, O2, T5, T6, P3, P4, and PZ), left hemisphere (Fp1, F3, F7, C3, T3, T5, P3, and O1), and right hemisphere (Fp2, F4, F8, C4, T4, T6, P4, and O2). The time series of gamma phase synchrony was indexed at each time point in terms of magnitude (an inverted normalized measure that ranges between 0 and 1, with 1 reflecting greater synchrony) and the latency corresponding to each measure of magnitude (in milliseconds). Phase synchrony differs from coherence estimates in that it may be derived using multiple sites (rather than pairs), and it indexes the synchrony in the phase of activity across these sites rather than the simple correlation in activity.
Magnitude and latency of gamma phase synchrony were averaged across the 40 target epochs for each subject at each time point. This yielded an averaged target gamma phase synchrony waveform for each region of interest (global, frontal, posterior, left hemisphere, and right hemisphere). Averaged gamma phase synchrony waveforms were smoothed with a 15-sample running average, following the previously published procedure (42).
Previous studies have revealed two peaks in the averaged gamma phase synchrony time series in response to target stimuli, including an early response maximal (within the latency window –150 to 150 msec, or “early gamma”) and a late poststimulus response maximal (in the latency window 200 to 450 msec, or “late gamma”). In this study, we analyzed peak magnitude and latency of gamma phase synchrony in relation to sex differences in schizophrenia compared with healthy subjects.
Statistical Analysis
Prior to statistical analysis, all outliers were removed from the data and replaced with the group mean for the relevant electrode site. Values more than one and a half times the interquartile range above the upper or below the lower quartiles were considered to be outliers. The groups were not statistically different on percentage of missing data.
Mixed-design multivariate analyses of variance (MANOVAs) were undertaken to analyze between-group differences in peak magnitude and latency of both early and late gamma phase synchrony in response to target stimuli. To examine global gamma phase synchrony, group (schizophrenia versus healthy subjects) was the between-group factor, and sex was the within-subject factor. For regional gamma phase synchrony, region (frontal versus posterior or left versus right hemisphere) was included as a second within-subject, repeated-measures factor. Interactions with sex were explored further using within-group MANOVAs (within schizophrenia and healthy groups) with sex as the between-subject factor.
Multivariate analyses of covariance were also conducted to examine the possible confounding effects of medication and symptoms on significant effects.
While each analysis was undertaken in relation to explicit predictions, we nonetheless employed a strict alpha level of 0.01, given that analyses of gamma phase synchrony were conducted for five different regional groupings.
Results
Gamma Phase Synchrony in Chronic Schizophrenia
Figure 1 presents the averaged regional waveform (including peak magnitude and latency, marked by red lines) for both early and late gamma phase synchrony for male and female chronic schizophrenia patients and their matched healthy comparison subjects in response to target stimuli.
A significant group-by-sex interaction was revealed for the magnitude of global late gamma phase synchrony (F=17.51, df=1, 76, p<0.0001). This interaction primarily was due to the reduction of gamma phase synchrony in female relative to male subjects in the chronic schizophrenia group (F=29.74, df=1, 38, p<0.0001). There were no significant effects involving sex or group for early global gamma phase synchrony.
There were no significant interactions involving group or sex for the frontal or posterior gradient of early or late gamma phase synchrony.
Analyses revealed a significant group-by-laterality interaction for early gamma phase synchrony (F=9.14, df=1, 76, p<0.004) that was due to reduced left hemisphere gamma phase synchrony in chronic schizophrenia patients relative to healthy subjects (F=9.52, df=1, 76, p<0.004), but a lack of group differences for the right hemisphere. For late gamma phase synchrony, there was a significant sex-by-laterality interaction (F=7.09, df=1, 76, p<0.01) that was due to the generally greater reduction for women relative to men in left hemisphere gamma phase synchrony (F=14.27, df=1, 76, p<0.001) but not right hemisphere gamma phase synchrony.
There were no significant interactions between group and sex for the laterality of early or late gamma phase synchrony magnitude or latency.
Gamma Phase Synchrony in First-Episode Schizophrenia
Figure 2 presents the averaged regional waveform (including peak magnitude and latency, marked by red lines) for both early and late gamma phase synchrony for male and female first-episode schizophrenia patients and their matched comparison subjects in response to target stimuli.
A significant group-by-sex interaction effect was revealed for the peak latency of early global gamma phase synchrony (F=6.68, df=1, 44, p<0.01). This interaction was due to faster latency in female versus male first-episode schizophrenia patients (F=7.80, df=1, 22, p<0.01) not present in the healthy subjects.
There were no interactions with group and sex for late global gamma phase synchrony.
A significant group-by-region interaction was revealed for the early gamma phase synchrony latency across the frontal and posterior gradient (F=8.56, df=1, 44, p<0.006). Latency of frontal synchrony was delayed relative to posterior synchrony in first-episode schizophrenia patients (F=15.56, df=1, 46, p<0.001), whereas there was no difference in healthy subjects. This interaction may have accounted for the significant main effect for group (F=8.23, df=1, 44, p<0.007), which revealed the generally delayed early gamma phase synchrony in the frontal region of first-episode schizophrenia patients relative to healthy subjects (F=8.87, df=1, 46, p<0.006). There were no interactions with group and sex for late global gamma phase synchrony.
A significant group main effect was found for the magnitude of early gamma phase synchrony (F=16.73, df=1, 44, p<0.001) with first-episode schizophrenia patients displaying reduced magnitude within both the left (F=9.58, df=1, 46, p<0.004) and right (F=11.57, df=1, 46, p<0.002) hemispheres relative to the healthy group. There was also a significant main effect for group (F=16.72, df=1, 44, p<0.0001) that was due to delayed early gamma phase synchrony latency in first-episode schizophrenia patients relative to healthy subjects for both the right (F=7.34, df=1, 46, p<0.009) and left (F=14.43, df=1, 46, p<0.001) hemispheres. There were no interactions with group and sex for late global gamma phase synchrony.
Discussion
This was the first study to explore sex differences in patients with schizophrenia using a new high-temporal-resolution measure of functional connectivity, gamma phase synchrony. This study also sought to examine the effect of illness chronicity on sex differences in brain function by including both chronic and first-episode schizophrenia patients. Consistent with predictions, both patient groups showed marked deficits in functional connectivity relative to healthy subjects. With regard to sex, female first-episode schizophrenia subjects demonstrated relatively enhanced synchronization as predicted. However, female chronic schizophrenia subjects exhibited even more severe impairments than male chronic schizophrenia subjects. These findings may be considered in terms of both illness chronicity and the temporal course of gamma phase synchrony.
It has been previously reported that early gamma phase synchrony may play a role in feed-forward anticipation of stimulus processing and the integration of sensory features. Late gamma phase synchrony, on the other hand, may reflect aspects of poststimulus discrimination and context processing (44). As a group, both chronic schizophrenia and first-episode schizophrenia patients exhibited marked disturbances in both early and late gamma phase synchrony. Specifically, chronic schizophrenia patients displayed a global reduction in functional connectivity, with particularly pronounced deficits in the left hemisphere, while first-episode schizophrenia patients exhibited a similar disturbance in left hemisphere gamma phase synchrony in addition to deficits in frontal connectivity. This widespread pattern of disconnectivity is consistent with previous studies demonstrating deficits in cognitive coordination of both early stimulus integration and the later processes of selective attention and context (23, 45). Furthermore, the pattern of hypofrontality and left hemisphere disconnectivity also adds weight to structural and functional investigations that suggest these regions are central to the neurodevelopment of schizophrenia (46–48).
In the first-episode schizophrenia group, faster early synchronization was observed in female relative to male subjects, suggesting that they have a greater adaptive capacity. Given the role of early gamma phase synchrony (49), this capacity may reflect an attempt to broaden the span of apprehension for incoming stimuli in an attempt to regulate a fundamental deficit in information processing. This is similar to observations of an extended span of apprehension and enhanced perceptual grouping (50), previously attributed to overactivity, which seem to suggest pathophysiologic rather than structural abnormality (51). While these studies have not considered sex differences, we might speculate that the onset of schizophrenia in women is preferentially associated with a distinctive pathophysiologic process rather than neuroanatomical impairment. This suggestion is consistent with findings of greater anatomical abnormalities in male schizophrenia subjects (11).
By contrast, the relatively enhanced speed of integration was not seen in female chronic schizophrenia subjects. Indeed, female chronic schizophrenia subjects by comparison showed a greater deficit in global late gamma phase synchrony than their male counterparts. In view of the function of late gamma phase synchrony, we may speculate that the departure in the pattern of synchronization according to chronicity in women with schizophrenia reflects the developmental progression of a pathophysiologic process. Pronounced deficits in context-related integration may reflect a particularly virulent progression of the pathophysiologic course, and associated cognitive impairment, in those women with schizophrenia unable to compensate for or adapt effectively to their illness. Supporting this view are reports of a consistently earlier age at onset in men and the corresponding evidence that suggests that chronic schizophrenia in women represents a particularly severe spectrum of the illness (1).
The differences in early versus late gamma phase synchrony observed in women with first-episode relative to chronic schizophrenia accounted largely for the total difference between the first-episode and chronic schizophrenia groups. That is, as a whole, first-episode schizophrenia patients exhibited more pronounced deficits in early gamma phase synchrony, whereas deficits in the chronic schizophrenia patients were most apparent for late gamma phase synchrony. The development of more “entrenched” impairments in stimulus discrimination and context in chronic schizophrenia is consistent with reports of greater deficits in executive functioning in this group (52). The consistently greater contribution of the female patients to this pattern of chronicity highlights an important sex-specific finding that requires further exploration in a larger sample of male and female subjects. It is important to note that a reduction in the gamma phase synchrony of the older group of healthy women was also found, further emphasizing that the process underlying impaired synchrony in women may have a basis in otherwise healthy physiologic development.
In conclusion, our study provides the first preliminary evidence that suggests schizophrenia disturbances in functional brain integration are related to sex and to illness chronicity. Current literature is attributing an increasingly significant role to gonadal hormones, particularly estrogen, in brain function. Therefore in view of this evidence (53), future investigations of gamma phase synchrony might also seek to consider additional variables such as menstrual cycle fluctuations indexed by precise blood specimen measures.
 |
Received May 28, 2003; revision received Nov. 18, 2003; accepted Nov. 24, 2003. From The Brain Dynamics Centre, Westmead Hospital, University of Sydney; and the University of Alberta, Edmonton, Alta., Canada. Address reprint requests to Dr. Slewa-Younan, The Brain Dynamics Centre, Acacia House, Westmead Hospital, Westmead NSW, 2145, Australia; [email protected] (e-mail). Supported by a New South Wales Institute of Psychiatry Research Fellowship (Dr. Slewa-Younan).
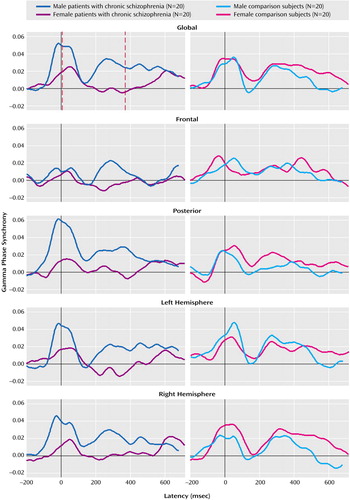
Figure 1. Gamma Phase Synchrony in Response to Target Stimuli for Subjects With Chronic Schizophrenia and Matched Healthy Comparison Subjects, by Gendera
aRed dashed lines mark the midpoint for early (0 msec) and late (325 msec) peak synchrony. This figure demonstrates the pattern of generally reduced gamma phase synchrony in chronic schizophrenia versus healthy comparison subjects, most prominent in female chronic schizophrenia patients.
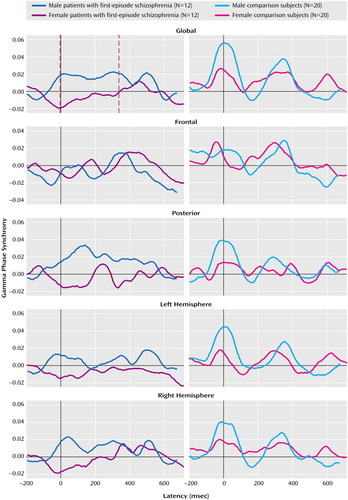
Figure 2. Gamma Phase Synchrony in Response to Target Stimuli for Subjects With First-Episode Schizophrenia and Matched Healthy Comparison Subjects, by Gendera
aRed dashed lines mark the midpoint for early (0 msec) and late (325 msec) peak synchrony. This figure demonstrates the pattern of generally reduced but faster early gamma phase synchrony in female patients with first-episode schizophrenia relative to male first-episode patients.
1. Leung A, Chue P: Sex differences in schizophrenia, a review of the literature. Acta Psychiatr Scand Suppl 2001; 401:3–38Google Scholar
2. Tamminga CA: Gender and schizophrenia. J Clin Psychiatry 1997; 58(suppl 15):33–37Medline, Google Scholar
3. Kulkarni J: Women and schizophrenia: a review. Aust NZ J Psychiatry 1997; 31:46–56Crossref, Medline, Google Scholar
4. Flor-Henry P: Schizophrenia: sex differences. Can J Psychiatry 1985; 30:319–322Crossref, Medline, Google Scholar
5. Duncan T: Gender, social mobility and psychiatric diagnoses. Soc Sci Med 1998; 46:1235–1247Crossref, Medline, Google Scholar
6. Kraepelin E: Dementia praecox (1896), in The Clinical Roots of the Schizophrenia Concept. Edited by Cutting J, Shepherd M. Cambridge, UK, Cambridge University Press, 1987, pp 13–24Google Scholar
7. Murray RM, Van Os J: Predictors of outcome in schizophrenia. J Clin Psychopharmacol 1998; 18 (2 suppl 1):2S-4SGoogle Scholar
8. Jablensky A, Sartorius N, Ernberg G, Anker M, Korten A, Cooper JE, Day R, Bertelsen A: Schizophrenia: manifestations, incidence and course in different cultures: a World Health Organization ten-country study. Psychol Med Suppl 1992; 20:1–97Crossref, Medline, Google Scholar
9. Hafner H, an der Heiden W, Behrens S, Gattaz WF, Hambrecht M, Loffler W, Maurer K, Munk-Jorgensen P, Nowotny B, Riecher-Rossler A, Stein A: Causes and consequences of the gender difference in age at onset of schizophrenia. Schizophr Bull 1998; 24:99–113Crossref, Medline, Google Scholar
10. Hafner H, Maurer K, Loffler W, an der Heiden W, Munk-Jorgensen P, Hambrecht M, Riecher-Rossler A: The ABC Schizophrenia Study: a preliminary overview of the results. Soc Psychiatry Psychiatr Epidemiol 1998; 33:380–386Crossref, Medline, Google Scholar
11. Zolese G: Women and schizophrenia, in Women and Mental Health. Edited by Kohen D. London, Routledge, 2000Google Scholar
12. Andreasen NC, Swayze VW II, Flaum M, Yates WR, Arndt S, McChesney C: Ventricular enlargement in schizophrenia evaluated with computed tomographic scanning: effects of gender, age, and stage of illness. Arch Gen Psychiatry 1990; 47:1008–1015Crossref, Medline, Google Scholar
13. Gur RE, Turetsky BI, Cowell PE, Finkelman C, Maany V, Grossman RI, Arnold SE, Bilker WB, Gur RC: Temporolimbic volume reductions in schizophrenia. Arch Gen Psychiatry 2000; 57:769–775Crossref, Medline, Google Scholar
14. Bullmore E, Brammer M, Harvey I, Murray R, Ron M: Cerebral hemispheric asymmetry revisited: effects of handedness, gender and schizophrenia measured by radius of gyration in magnetic resonance images. Psychol Med 1995; 25:349–363Crossref, Medline, Google Scholar
15. Alexander RC, Mukherjee S, Richter J, Kaufmann CA: Minor physical anomalies in schizophrenia. J Nerv Ment Dis 1994; 182:639–644Crossref, Medline, Google Scholar
16. Ragland JD, Gur RE, Klimas BC, McGrady N, Gur RC: Neuropsychological laterality indices of schizophrenia: interactions with gender. Schizophr Bull 1999; 25:79–89Crossref, Medline, Google Scholar
17. Gur RE, Gur RC: Gender differences in regional cerebral blood flow. Schizophr Bull 1990; 16:247–254Crossref, Medline, Google Scholar
18. Josiassen RC, Roemer RA, Johnson MM, Shagass C: Are gender differences in schizophrenia reflected in brain event-related potentials? Schizophr Bull 1990; 16:229–246Crossref, Medline, Google Scholar
19. Flor-Henry P, Koles ZJ: Statistical quantitative EEG studies of depression, mania, schizophrenia and normals. Biol Psychiatry 1984; 19(3-4):257–279Google Scholar
20. Turetsky BI, Colbath EA, Gur RE: P300 subcomponent abnormalities in schizophrenia, I: physiological evidence for gender and subtype specific differences in regional pathology. Biol Psychiatry 1998; 43:84–96Crossref, Medline, Google Scholar
21. Haig AR, Gordon E, Wright JJ, Meares RA, Bahramali H: Synchronous cortical gamma-band activity in task-relevant cognition. Neuroreport 2000; 11:669–675Crossref, Medline, Google Scholar
22. Kraepelin E: Dementia Praecox and Paraphrenia Together With Manic-Depressive Insanity and Paranoia. Birmingham, UK, Classics of Medicine Library, 1919Google Scholar
23. Andreasen NC, Nopoulos P, O’Leary DS, Miller DD, Wassink T, Flaum M: Defining the phenotype of schizophrenia: cognitive dysmetria and its neural mechanisms. Biol Psychiatry 1999; 46:908–920Crossref, Medline, Google Scholar
24. Friston KJ: Schizophrenia and the disconnection hypothesis. Acta Psychiatr Scand Suppl 1999; 395:68–79Crossref, Medline, Google Scholar
25. Lee KH, Williams LM, Breakspear M, Gordon E: Synchronous gamma activity: a review and contribution to an integrative neuroscience model of schizophrenia. Brain Res Brain Res Rev 2003; 41:57–78Crossref, Medline, Google Scholar
26. Singer W, Gray CM: Visual feature integration and the temporal correlation hypothesis. Ann Rev Neurosci 1995; 18:555–586Crossref, Medline, Google Scholar
27. Slewa-Younan S, Gordon E, Williams L, Haig AR, Goldberg E: Sex differences, gamma activity and schizophrenia. Int J Neurosci 2001; 107:131–144Crossref, Medline, Google Scholar
28. Haig AR, Gordon E, De Pascalis V, Meares RA, Bahramali H, Harris A: Gamma activity in schizophrenia: evidence of impaired network binding? Clin Neurophysiol 2000; 111:1461–1468Crossref, Medline, Google Scholar
29. Gordon E, Williams LM, Haig AR, Bahramali H, Wright J, Meares R: Symptom profile and “gamma” processing in schizophrenia. Cognitive Neuropsychiatry 2001; 6:7–20Crossref, Google Scholar
30. Lee K-H, Williams LM, Haig AR, Gordon E: Gamma (40 Hz) phase synchronicity and symptom dimensions in schizophrenia. Cognitive Neuropsychiatry 2003; 8:57–71Crossref, Medline, Google Scholar
31. Holloway RL, Anderson PJ, Defendini R, Harper C: Sexual dimorphism of the human corpus callosum from three independent samples: relative size of the corpus callosum. Am J Phys Anthropol 1993; 92:481–498Crossref, Medline, Google Scholar
32. Courten-Myers GM: The human cerebral cortex: gender differences in structure and function. J Neuropathol Exp Neurol 1999; 58:217–226Crossref, Medline, Google Scholar
33. Flor-Henry P, Koles ZJ: EEG characteristics in normal subjects: a comparison of men and women and of dextrals and sinistrals. Res Commun Psychol Psychiatr Behav 1982; 7:21–38Google Scholar
34. Briggs GG, Nebes RD: Patterns of hand preference in a student population. Cortex 1975; 11:230–238Crossref, Medline, Google Scholar
35. Williams LM, Gordon E, Bahramali H, Wright J, Meares RA: Late component ERPs are associated with distinct schizophrenia syndromes. Res Commun Psychol Psychiatr Behav 1982; 7:21–38Google Scholar
36. Snelbaker AJ, Wilkinson Gray S, Robertson GJ, Glutting JJ: Wide Range Achievement Test 3 (WRAT 3), in Understanding Psychological Assessments: Perspectives on Individual Differences. Edited by Dorfman WI, Hersen M. New York, Kluwer Academic/Plenum, 2001, pp 259–274Google Scholar
37. Kay SR, Opler LA, Fiszbein A: Positive and Negative Syndrome Scale (PANSS). North Tonawanda, NY, Multi-Health Systems, 1986Google Scholar
38. Lambert T: Lundbeck utility for neuroleptic dose conversion. Melbourne, University of Melbourne, Multimedia in Psychiatry Unit, 1998Google Scholar
39. Blom JL, Anneveldt M: An electrocap tested. Electroencephalogr Clin Neurophysiol 1982; 54:591–594Crossref, Medline, Google Scholar
40. Gratton G, Kramer AF, Coles MGH, Donchin E: A new method for off-line removal of ocular artifact. Electroencephalogr Clin Neurophysiol 1983; 55:468–484Crossref, Medline, Google Scholar
41. Press WH, Teukolsky SA, Vetterling WT, Flannery BP: Fourier and spectral applications, in Numerical Recipes in C: The Art of Scientific Computing. Cambridge, UK, Cambridge University Press, 1993, pp 537–608Google Scholar
42. Haig AR, De Pascalis V, Gordon E: Peak gamma latency correlated with reaction time in a conventional oddball paradigm. Electroencephalogr Clin Neurophysiol 1999; 110:158–165Google Scholar
43. Haig AR, Gordon E: Prestimulus EEG alpha phase synchronicity influences N100 amplitude and reaction time. Psychophysiology 1998; 35:591–595Crossref, Medline, Google Scholar
44. Duncan-Johnson CC, Donchin E: The P300 component of the event-related brain potential as an index of information processing. Biol Psychol 1982; 14:1–52Crossref, Medline, Google Scholar
45. Polich J, Kok A: Cognitive and biological determinants of P300: an integrative review. Biol Psychol 1995; 41:103–146Crossref, Medline, Google Scholar
46. Chua SE, McKenna PJ: Schizophrenia—a brain disease? a critical review of structural and functional cerebral abnormality in the disorder. Br J Psychiatry 1995; 166:563–582Crossref, Medline, Google Scholar
47. Flor-Henry P: Gender, hemispheric specialization and psychopathology. Soc Sci Med 1978; 12:155–162Medline, Google Scholar
48. Lieberman J, Chakos M, Wu H, Alvir J, Hoffman E, Robinson D, Bilder R: Longitudinal study of brain morphology in first episode schizophrenia. Biol Psychiatry 2001; 49:487–499Crossref, Medline, Google Scholar
49. Haig AR: Missing Links: The Role of Phase Synchronous Gamma Oscillations in Normal Cognition and Their Dysfunction in Schizophrenia. Sydney, Australia, University of Sydney, Department of Psychological Medicine, 2001Google Scholar
50. Williams LM: Cognitive inhibition and schizophrenic symptom subgroups. Schizophr Bull 1996; 22:139–151Crossref, Medline, Google Scholar
51. Seidman LJ, Goldstein JM, Goodman JM, Koren D, Turner WM, Faraone SV, Tsuang MT: Sex differences in olfactory identification and Wisconsin Card Sorting performance in schizophrenia: relationship to attention and verbal ability. Biol Psychiatry 1997; 42:104–115Crossref, Medline, Google Scholar
52. Bilder RM, Goldman RS, Robinson D, Reiter G, Bell L, Bates JA, Pappadopulos E, Willson DF, Alvir JMJ, Woerner MG, Geisler S, Kane JM, Lieberman JA: Neuropsychology of first-episode schizophrenia: initial characterization and clinical correlates. Am J Psychiatry 2000; 157:549–559Link, Google Scholar
53. Behl C: Sex hormones, neuroprotection and cognition. Prog Brain Res 2002; 138:135–142Crossref, Medline, Google Scholar



