Neurocognitive Dysfunction in First-Episode Psychosis: Correlates With Symptoms, Premorbid Adjustment, and Duration of Untreated Psychosis
Abstract
OBJECTIVE: The authors examined the relationship of neurocognitive function with duration of untreated psychosis, premorbid illness factors, and clinical symptoms to determine whether long duration of untreated psychosis independently compromises cognitive function. METHOD: Patients recruited to a study of the effect of an early detection program on the duration of untreated first-episode psychosis in two catchment areas were compared to patients in a similar treatment program in two other catchment areas without an early detection program. The median duration of untreated psychosis was 10.5 weeks for all patients. A total of 301 patients entered the study, and 207 completed a comprehensive neuropsychological test battery that assessed working memory/fluency, executive function, verbal learning, impulsivity, and motor speed. The median time from start of treatment to neuropsychological testing was 108 days; all patients were tested within 9 months. RESULTS: No significant association was found between duration of untreated psychosis and any of the cognitive measures. Strong associations were demonstrated between poorer premorbid school functioning and neurocognitive deficits, especially in verbal learning and working memory. No relationship was found between neurocognitive functions and clinical measures, except for an inverse correlation of Positive and Negative Syndrome Scale negative symptoms and working memory and a positive correlation between positive symptoms and motor speed. CONCLUSIONS: The data contribute to a disconfirmation of the hypothesis of an association between duration of untreated psychosis and neurocognitive performance at baseline.
Patients with schizophrenia exhibit wide-ranging impairments on neuropsychological tasks, compared to healthy subjects, including tasks measuring memory, attention, and executive function (1). However, lack of methodological rigor prevents firm conclusions about selective deficits in schizophrenia (2, 3). A further delineation of dysfunctional cognitive processes would provide information about the neurobiology of the disorder (4) as well as contribute to its rehabilitation (1). Abnormalities detected earlier in development are more likely to be etiological (5). First-episode psychosis is an optimal disorder for examining the neurobiology of the illness, since confounds such as hospitalizations, long-term medication, and chronicity can be avoided. Study groups that include patients with chronic illness may also be selectively biased toward poorer treatment response and outcome (6).
Most studies of cognition in the early course of psychosis show that deficits are already present (6–13). However, conclusions are limited by the small number of subjects in these studies and because the duration of untreated psychosis was not reported.
It has been suggested that long duration of untreated psychosis has a neurotoxic effect (14). If such an effect exists, it is likely to affect cognitive function (15). A few studies have examined the association between duration of untreated psychosis and cognitive functions, and the results of these studies are inconsistent. Two studies found associations between longer duration of untreated psychosis and more severe and enduring cognitive deficits (16, 17). Amminger et al. (18) reported that longer duration of untreated psychosis predicted cognitive deterioration. Barnes et al. (19) reported an association approaching significance between attentional shifting and duration of untreated psychosis. However, two other studies found no significant relationship between duration of untreated psychosis and cognitive variables (15, 20).
The relationship between neurocognitive deficits and premorbid adjustment in schizophrenia has been studied to a limited degree. Binder et al. (21) reported no difference in neuropsychological performance between patients with short and long prodromal periods, suggesting that neuropsychological deficits in first-episode schizophrenia are independent of the early course of the illness. DeQuardo et al. (22) associated premorbid asociality with adult neuropsychological dysfunction, and Levitt et al. (23) reported an association of poor premorbid adjustment with perseverative errors on the Wisconsin Card Sorting Test and poor visual memory span performance. Bilder et al. (6) found that neuropsychological measures correlated with childhood adjustment. Silverstein et al. (24) reported greater cognitive deficits when premorbid adjustment was unfavorable, particularly for measures of attention and executive functions. Collectively, these studies indicate a relationship between premorbid social adjustment and neurocognitive deficits after onset of the disorder, but methodological shortcomings, especially the small numbers of subjects, make the results inconclusive.
The relationship between neurocognitive deficits and symptoms of schizophrenia is also an area with inconsistent findings. Some have found an association of neurocognitive deficits with negative symptoms (6, 25–27), others have not (9, 21).
The primary aim of this study was to examine the relationship between pretreatment factors and neurocognitive function in a large group of clinically stabilized patients with first-episode psychosis, for whom age at onset and length of illness could be accurately determined. The study addressed two main questions: 1) Are there indications that patients with longer duration of untreated psychosis have poorer neurocognitive function at first treatment? 2) Is neurocognitive function related to premorbid adjustment and to presenting clinical symptoms?
Method
TIPS (a Norwegian acronym standing for early intervention in psychosis) is a multisite investigation of the relationship between duration of untreated psychosis and outcome in first-episode psychoses (28). The study was approved by the Regional Committee for Medical Research Ethics. All patients gave written informed consent.
Patients were recruited from consecutive referrals to psychiatric services in four catchment-area-based health care sectors between 1997 and 2000. Inclusion criteria were residence in the catchment areas (670,000 inhabitants); meeting the DSM-IV criteria for schizophrenia (N=56), schizophreniform disorder (N=50), schizoaffective disorder (N=26), brief psychotic episode (N=14), delusional disorder (N=13), affective psychosis with mood incongruent delusions (N=28), or psychotic disorder not otherwise specified (N=20); being actively psychotic (having a Positive and Negative Syndrome Scale [29] score of 4 or more on positive scale items 1, 3, 5, or 6, or general scale item 9); never having received adequate treatment for psychosis (defined as treatment with antipsychotic medication [more than 3.5 mg/day of haloperidol equivalents] for more than 12 weeks or until remission of the psychotic symptoms [30]); having no neurological or endocrine disorders related to the psychosis; speaking one of the Scandinavian languages; and having an IQ higher than 70. The Structured Clinical Interview for DSM-IV Axis I Disorders (31) was used for diagnostic purposes. Diagnostic assessments were conducted by trained clinical research personnel and discussed by the assessment team until diagnostic consensus was reached. A total of 301 patients was included. Symptom ratings were conducted at first treatment and at 3 months. A standardized side effects scale (the St. Hans Rating Scale for Extrapyramidal Syndromes [32]) was used to assess extrapyramidal side effects at 3 months.
To maximize cooperation and to avoid state effects of the acute psychosis, patients received neuropsychological testing at remission of psychotic symptoms or at 3 months, whichever came first. Sixty-five patients did not participate in neuropsychological testing, and 29 patients who were tested later than 9 months after intake were excluded from baseline analyses, since their results were judged not to represent baseline functioning. There were no differences between the participants and the nonparticipants on any major demographic (age, gender, cultural background, marital status, educational status, employment status), clinical (duration of untreated psychosis, diagnosis, Positive and Negative Syndrome Scale scores), or premorbid functioning (Premorbid Adjustment Scale [33] score) variables, except that the nonparticipant group included more patients with substance abuse (42%, compared with 29% in the participant group) (p<0.05, Fisher’s exact test). Of the 207 patients who were included, 125 were tested as scheduled and 82 were tested between 4 and 9 months after study entry. Patients who were tested later than scheduled had less education (11.3 years versus 12.6 years) (p<0.001, Student’s t test) and poorer overall school functioning (Premorbid Adjustment Scale school functioning score: 2.3 versus 1.9) (p<0.05, Student’s t test).
At neuropsychological testing, 8.5% of the patients were not receiving antipsychotic medication, 23.5% were receiving first-generation antipsychotics (14% were receiving perphenazine; 7% were receiving zuclopenthixol; and the rest were receiving haloperidol, pimozide, chlorpromazine, or chlorprothixene), and 68% were receiving second-generation antipsychotics (53% were receiving olanzapine; 12%, risperidone; and 3%, sertindole). The mean dose was 7.2 mg/day of haloperidol equivalents (SD=0.4). Only nine patients used anticholinergic antiparkinsonian medication. Table 1 outlines the patients’ demographic and clinical characteristics.
Neurocognitive Tests
Eight neuropsychological tests, described in detail elsewhere (34), were used for assessing neurocognitive function. The tests were administered by test technicians or clinical psychologists trained in standardized assessment and experienced in working with psychotic patients; the test administrators were supervised by a doctoral-level psychologist. The test battery took 3–4 hours to complete and was administered in the following order:
| 1. | California Verbal Learning Test (35). Scores were obtained for total immediate recall (mean sum of trials 1–5), errors (mean sum of trials 1–5), delayed free recall, and recognition. | ||||
| 2. | Backward Masking Test (36). The mean for the two mask conditions (33 msec and 49.5 msec interstimulus intervals) was used to improve the reliability of the measure. | ||||
| 3. | Finger Tapping Test (37). We expected no lateralized motor deficits, and the mean score for the two hands was used in data analyses. | ||||
| 4. | Wisconsin Card Sorting Test (38). Measures were number of categories completed, perseverative errors, perseverative responses, number of trials to first category, and failure to maintain set. | ||||
| 5. | Controlled Oral Word Association Task (39). The total number of words generated in 1 minute for the three letters were summed. | ||||
| 6. | Trail Making Test (A and B) (37). The scores used were the total time for the completion of part A and part B, respectively. | ||||
| 7. | Digit Span Distractibility Test (40). The total number of digits recalled in the correct order on each test was summed and divided by number of possible correct answers; neutral and distractor strings were scored separately. | ||||
| 8. | Continuous Performance Test, Identical Pairs Version (41). Four major performance indices were included: 1) hits, which is the proportion of correct responses to target trials; 2) mean false alarms for digits and shapes, which is the proportion of responses to catch trials; 3) reaction time; and 4) d′, an index of discriminability. The scores were the mean ratio for six trials. | ||||
In addition, three subscales of the WAIS-R (42) (similarities, block design, and digit span) were administered to estimate IQ.
Handedness was assessed by asking the patients to identify their preferred hand.
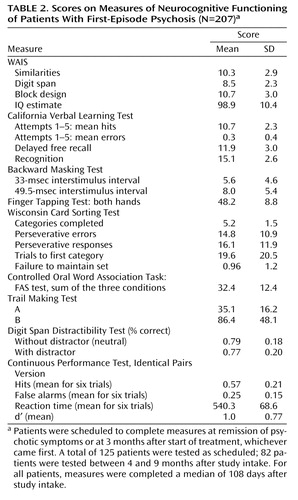
Patients varied considerably across all cognitive measurements (Table 2). In general, the patients in this study had scores that were one-half to one standard deviation below those of healthy comparison samples and one-half to one standard deviation higher than those for samples of patients with chronic schizophrenia (10, 36–38, 40).
A subset of measures from each test was entered as input variables in a principal component analysis. The selection of measures from each test was based on a combination of the theoretical foundation of the essential quality of the test, clinical experience, and a previous principal component analysis. In previous work (34), we identified five dimensions that explained 72% of the variance: 1) working memory/fluency (four items: Controlled Oral Word Association Task score, Digit Span Distractibility Test scores with and without distractor, and Continuous Performance Test hits), 2) executive function (three items, all from the Wisconsin Card Sorting Test: categories completed, perseverative responses [reversed], and number of attempts to the first category completed [reversed]), 3) verbal learning (three items, all from the California Verbal Learning Test: immediate recall score, delayed free recall score, and errors [reversed]), 4) impulsivity (two items, both from the Continuous Performance Test: false alarms and reaction time [reversed]), and 5) motor speed (one item only: Finger Tapping Test score). These five dimensions were used in the data analyses in the present report.
Clinical Measures
Duration of untreated psychosis was measured as the time from the first onset of psychotic symptoms (defined as the first week with psychotic symptoms corresponding to a Positive and Negative Syndrome Scale score of 4 or more on one of the positive scale items [items 1, 3, 5, or 6] or the general scale item 9) to the start of first adequate treatment of psychosis (defined as start of adequate antipsychotic medication or hospital admission for treatment of acute psychosis). The duration of untreated psychosis was calculated as the sum of periods with active untreated psychosis. Multiple sources, including personal interviews with both patients and relatives, were used to ascertain the duration of untreated psychosis.
Symptoms were measured with the Positive and Negative Syndrome Scale. Global functioning was measured by the Global Assessment of Functioning Scale (43). The scores were split into symptom scores and function scores to improve reliability (44).
Premorbid functioning was measured by the Premorbid Adjustment Scale, which assesses levels of functioning until 6 months before the onset of psychosis on a scale from 0 (best) to 6 (poorest). The premorbid period was subdivided into four periods: childhood (<11 years), early adolescence (12–15 years), late adolescence (16–18 years), and adulthood (≥19 years). The Premorbid Adjustment Scale covers two discrete areas of functioning: school functioning (school performance and school adaptation) and socialization (social accessibility-isolation, peer relationships, and capacity to establish sociosexual relationships [the latter was not assessed for childhood]). Recent reports have indicated different predictive powers across the domains of school functioning and socialization. We report the mean scores for the two domains across the childhood, early adolescence, and late adolescence periods.
The reliability of the clinical measurements ranged from fair to very good (44).
Statistical Analysis
Analyses were made with the statistical package SPSS for Windows (version 11) (SPSS Inc., Chicago). All tests were two-tailed. The applied method for group comparison was the Student’s t test if not indicated otherwise. Nonparametric tests were mainly used for data without normal distribution, such as the duration of untreated psychosis. When parametric tests were appropriate, the duration of untreated psychosis was transformed to its natural logarithm. Given the considerable number of cognitive and clinical measures in the analyses, only p values <0.01 are reported as significant.
The bivariate relationships between the significant demographic, clinical, and premorbid variables and the cognitive indices were studied before examining the bivariate relationship between duration of untreated psychosis and the cognitive indices. To rule out confounding factors, the associations between the five cognitive indices (as the dependent variables), the duration of untreated psychosis, and the demographic, clinical, and premorbid variables were studied in five separate multiple linear regression analyses. The variables were entered hierarchically and stepwise in blocks. For each block, the variables with the strongest association with the dependent variable were kept in the model. The final model was examined for nonlinear relationships between the dependent and independent variables, interaction effects, and effects of outliers and influential observations. Only the final models are presented.
Results
Demographic and Clinical Factors
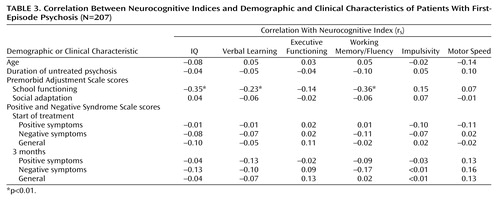
Women showed better performance than men on the verbal learning index (t=–3.88, df=201, p<0.001), while men did better than women on the motor speed index (t=6.44, df=201, p<0.001). The 26 left-handed patients (13% of all patients) performed slightly better than right-handed subjects on the verbal learning index (t=–2.63, df=201, p<0.01). There were no significant associations between actual ages, in this case the same as age at onset, and any of the cognitive indices (Table 3).
Patients with affective psychosis had a significantly higher score on the impulsivity index than those without affective psychosis (t=–3.58, df=191, p<0.001). There were no significant associations between the other diagnostic groups and the cognitive indices, and no significant differences between the patients with narrowly defined schizophrenia spectrum disorders and the patients with other disorders. There were no significant associations between drug or alcohol abuse and any cognitive indices, with the exception of the motor speed measure, on which patients with concomitant abuse did significantly better than those without concomitant substance abuse (t=–2.42, df=199, p<0.05). No significant correlations were found between Positive and Negative Syndrome Scale symptoms at 3 months on any cognitive indices.
Eighty-eight patients (42.5%) did not have symptom remission by the start of neuropsychological testing. There were no significant differences on the cognitive indices between the groups with and without remission, and no significant differences between the patients tested as scheduled and the patients tested later than scheduled. There were no significant associations between the neurocognitive indices and the type of medication received (first- or second-generation antipsychotics) or between the neurocognitive indices and medication dose.
Premorbid Functioning
Premorbid school functioning, as measured by the Premorbid Adjustment Scale, was strongly associated with IQ, the verbal learning measure, and the working memory/fluency index (Table 3). There were no strong associations between any of the neurocognitive indices and measures of premorbid social functioning.
Duration of Untreated Psychosis
No significant associations were found between the duration of untreated psychosis and any of the cognitive indices in bivariate analyses (Table 3). The same held for all specific tests referred to in Table 2. In some studies of duration of untreated psychosis and clinical outcome, duration of untreated psychosis has been dichotomized at 1 week, 6 months, or 1 year (45–47). In our study, dichotomizing duration of untreated psychosis at these cutoff points did not influence the results.
A relationship between cognitive indices and duration of untreated psychosis could theoretically be masked by other variables. Multiple linear regression analyses for each of the indices were conducted to rule out this possibility. Significant demographic and clinical variables were entered in blocks, with duration of untreated psychosis in the final analysis (first block: age, gender, and handedness; second block: diagnosis; third block: school functioning, as measured by the Premorbid Adjustment Scale, and length of education; fourth block: duration of untreated psychosis). Premorbid school functioning retained its significant influence on verbal learning and working memory/fluency in the multivariate regression analyses. Duration of untreated psychosis had no significant relationship to any of the cognitive indices.
Discussion
This study confirmed, in a sufficiently large group of subjects, the finding of two previous studies (15, 20): that there is no consistent association between duration of untreated psychosis and any cognitive dimension in first-episode psychosis at start of treatment. Our study’s findings also reflect a recent study by Ho et al. (48) showing no association between duration of untreated psychosis and possible toxic neural effects as assessed by brain volumetric measurements. The median duration of untreated psychosis in the present study was considerably shorter than duration of untreated psychosis in older studies (49). Since both duration of untreated psychosis and neurocognitive functioning vary widely between patients, the observed lack of association cannot be explained through truncated variance in the key measures.
As expected, school functioning, as measured by the Premorbid Adjustment Scale, was associated with the cognitive dimensions of working memory/fluency and verbal learning. Poor school performers continue to perform poorly after onset of illness. The fact that the association also included elements of adaptation indicates that these functions are linked to a broader domain of disturbances. The finding that working memory deficit is an essential factor in the development of schizophrenia is also consistent with the high-risk study by Erlenmeyer-Kimling et al. (50). In that study, this deficit occurred in all children who were followed into adulthood and received a diagnosis of schizophrenia. Silverstein et al. (24) observed that the primary areas of association between premorbid adjustment and cognitive dysfunction involved attention and executive functions. In the present study, working memory/fluency and verbal learning represented the strongest connection to premorbid adjustment. This difference may be due to the broader array of cognitive functions used in this study.
Few relationships were found between clinical and neurocognitive indices, suggesting that the two domains are relatively independent when the psychosis is treated. In our study design, first testing was done when the patients’ acute psychosis had remitted or when the patients were clinically stable, and the lack of an association between symptoms as measured by the Positive and Negative Syndrome Scale and the neurocognitive indices was expected. Our study procedure introduced the possibility of a methodologically based difference between patients who had or had not experienced clinical remission at first testing. As no differences in scores were found between patients with remission and the smaller group of patients with continuing psychosis, the effects of this difference appear to be minimal. Testing treated patients also introduces the possibility of medication effects on neurocognition, although we found no relationship between medication types or dose and neuropsychological test results.
Neurocognitive functioning varied widely between patients, but group means for most tests were clearly below the levels found for normative healthy comparison samples. Since the study did not include a healthy comparison group, the exact difference cannot be calculated. The decision to wait for remission or clinical stability makes it impossible to pinpoint when in the course of early psychosis these deficits emerged. As there were no differences in the neurocognitive indices between patients tested as scheduled and the smaller group of patients tested later, the deficits appear to be stable early on. There is no reason to believe that our choice to delay testing until patients were clinically stable had any effect on the study’s main finding, the lack of association between duration of untreated psychosis and neurocognitive functioning. Hypothetical differences in cognitive functioning that disappear after few weeks of treatment are not likely to have any significant long-term effects.
The number of eligible patients who do not consent to study participation or who do not cooperate with testing is infrequently described in studies of neurocognition in schizophrenia. The present study group was drawn from patients participating in a large study of consecutive first-episode patients from catchment-area-based psychiatric services. Even if the degree of nonparticipation of eligible patients was higher than originally anticipated, and thus represented a methodological limitation, the study design offered the unique possibility to compare the study patients to the original intake sample. The main difference was the higher likelihood for nonparticipants to be drug or alcohol abusers. There were few differences in neurocognitive functioning between patients with substance abuse and those without substance abuse who completed the neuropsychological tests, and none of these differences were related to the study’s main finding.
The study’s main strength is the large size of the study group. The number of patient participants was larger than in previous studies of the relationship between cognitive functioning and clinical status in first-episode psychosis. The neuropsychological test battery used in the present study also included tests of a wider range of cognitive functions, compared with previous studies, and the duration of untreated psychosis and the clinical variables were assessed reliably.
 |
 |
 |
Received March 7, 2003; revision received July 9, 2003; accepted July 15, 2003. From the Department of Psychiatry, Ullevål University Hospital, Oslo; Rogaland Psychiatric Hospital, Stavanger, Norway; and Roskilde Psychiatric University Hospital, Fjorden, Denmark. Address correspondence to Dr. Rund, Department of Psychology, University of Oslo, P.O. Box 1094 Blindern, N-0317 Oslo, Norway; [email protected] (e-mail). This work is part of the TIPS project (TIPS is a Norwegian acronym standing for early intervention in psychosis). The project includes the following research group: Thomas H. McGlashan, M.D. (principal investigator), Per Vaglum, M.D. (principal investigator), Svein Friis, M.D., Ulrik Haahr, M.D., Jan Olav Johannessen, M.D., Tor K. Larsen, M.D., Ingrid Melle, M.D., Stein Opjordsmoen, M.D., Bjørn Rishovd Rund, Ph.D., and Erik Simonsen, M.D. The TIPS project is supported by grant 133897/320 from the Norwegian Research Council, grant 1997/41 from the National Council for Mental Health/Health and Rehabilitation, NIMH grant K05 01654, and grants from the Norwegian Health Ministry, Rogaland and Oslo County, and the Theodore and Vada Stanley Foundation.
1. Rund BR, Borg NE: Cognitive deficits and cognitive training in schizophrenic patients. Acta Psychiatr Scand 1999; 100:85–95Crossref, Medline, Google Scholar
2. Chapman LJ, Chapman JP: The measurement of differential deficits. J Psychiatry Res 1978; 14:303–311Crossref, Medline, Google Scholar
3. Rund BR: A review of longitudinal studies of cognitive functions in schizophrenia patients. Schizophr Bull 1998; 24:425–435Crossref, Medline, Google Scholar
4. Hutton SB, Puri BK, Duncan L-J, Robbins TW, Barnes TRE, Joyce EM: Executive function in first-episode schizophrenia. Psychol Med 1998; 28:463–473Crossref, Medline, Google Scholar
5. Cornblatt B, Obuchowski M, Schnur D, O’Brien JD: Hillside study of risk and early detection in schizophrenia. Br J Psychiatry 1998; 172(suppl 33):26–32Google Scholar
6. Bilder RM, Goldman RS, Robinson D, Reiter G, Bell L, Bates JA, Pappadopulos E, Willson DF, Alvir JMJ, Woerner MG, Geisler S, Kane JM, Lieberman JA: Neuropsychology of first-episode schizophrenia: initial characterization and clinical correlates. Am J Psychiatry 2000; 157:549–559Link, Google Scholar
7. Saykin AJ, Shtasel DL, Gur RE, Kester DB, Mozley LH, Stafiniak P, Gur RC: Neuropsychological deficits in neuroleptic naive patients with first-episode schizophrenia. Arch Gen Psychiatry 1994; 51:124–131Crossref, Medline, Google Scholar
8. Nuechterlein K, Gittlin MJ, Subotnok KL: The early course of schizophrenia and long-term maintenance neuroleptic therapy. Arch Gen Psychiatry 1995; 52:203–205Crossref, Medline, Google Scholar
9. Hoff AL, Harris D, Faustman WO, Beal M, DeVilliers D, Mone RD, Moses JA, Csernansky JG: A neuropsychological study of early onset schizophrenia. Schizophr Res 1996; 20:21–28Crossref, Medline, Google Scholar
10. Øie M, Rund BR: Neuropsychological deficits in adolescent-onset schizophrenia compared with attention deficit hyperactivity disorder. Am J Psychiatry 1999; 156:1216–1222Abstract, Google Scholar
11. Mohamed S, Paulsen JS, O’Leary D, Arndt S, Andreasen N: Generalized cognitive deficits in schizophrenia: a study of first-episode patients. Arch Gen Psychiatry 1999; 56:749–754Crossref, Medline, Google Scholar
12. Addington J, Brooks BL, Addington D: Cognitive functioning in first episode psychosis: initial presentation. Schizophr Res 2002; 62:59–64Crossref, Google Scholar
13. Kravariti E, Morris RG, Rabe-Hesketh S, Murray RM, Frangou S: The Maudsley early onset schizophrenia study: cognitive function in adolescents with recent onset schizophrenia. Schizophr Res 2003; 61:137–148Crossref, Medline, Google Scholar
14. Wyatt RJ, Heuter I: Rationale for the study of early intervention. Schizophr Res 2001; 51:69–76Crossref, Medline, Google Scholar
15. Norman RMG, Townsend L, Malla AK: Duration of untreated psychosis and cognitive functioning in first-episode patients. Br J Psychiatry 2001; 179:340–345Crossref, Medline, Google Scholar
16. Scully PJ, Coakley G, Kinsella A, Waddington JL: Psychopathology, executive function and general cognitive impairment in relation to duration of initially untreated versus subsequent treated psychosis in chronic schizophrenia. Psychol Med 1997; 27:1303–1310Crossref, Medline, Google Scholar
17. Wyatt RJ, Damiani LM, Henter ID: First-episode schizophrenia: early intervention and medication discontinuation in the context of course and treatment. Br J Psychiatry Suppl 1998; 33:77–83Google Scholar
18. Amminger GP, Edwards J, Brewer WJ, Harrigan S, McGorry PD: Duration of untreated psychosis and cognitive deterioration in first-episode schizophrenia. Schizophr Res 2002; 54:223–230Crossref, Medline, Google Scholar
19. Barnes TR, Hutton SB, Chapman MJ, Mutsatsa S, Puri BK, Joyce EM: West London first-episode study of schizophrenia: clinical correlates of duration of untreated psychosis. Br J Psychiatry 2000; 177:207–211Crossref, Medline, Google Scholar
20. Hoff AL, Sakuma M, Razi K, Heydebrand G, Csernansky JG, DeLisi LE: Lack of association between duration of untreated illness and severity of cognitive and structural brain deficits at the first episode of schizophrenia. Am J Psychiatry 2000; 157:1824–1828Link, Google Scholar
21. Binder J, Albus M, Hubmann W, Scherer J, Sobizack N, Franz U, Mohr F, Hecht S: Neuropsychological impairment and psychopathology in first-episode schizophrenic patients related to the early course of illness. Eur Arch Psychiatry Clin Neurosci 1998; 248:70–77Crossref, Medline, Google Scholar
22. DeQuardo JR, Tandon R, Goldman R, Meador-Woodruff JH, McGrath-Giroux M, Brunberg JA, Kim L: Ventricular enlargement, neuropsychological status, and premorbid function in schizophrenia. Biol Psychiatry 1994; 35:517–524Crossref, Medline, Google Scholar
23. Levitt JJ, O’Donnell BF, McCarley RW, Nestor PG, Shenton ME: Correlations of premorbid adjustment in schizophrenia with auditory event-related potential and neuropsychological abnormalities. Am J Psychiatry 1996; 153:1347–1349Link, Google Scholar
24. Silverstein ML, Mavrolefteros G, Close D: Premorbid adjustment and neuropsychological performance in schizophrenia. Schizophr Bull 2002; 28:157–165Crossref, Medline, Google Scholar
25. Johnstone EC, Crow TJ, Frith CD, Husband J, Kreel L: Cerebral ventricular size and cognitive impairment in chronic schizophrenia. Lancet 1976; 11:924–926Crossref, Google Scholar
26. Andreasen NC, Olsen SA, Dennert JW, Smith MR: Ventricular enlargement in schizophrenia: relationship to positive and negative symptoms. Am J Psychiatry 1982; 139:297–302Link, Google Scholar
27. Perlick D, Mattis S, Stastny P, Silverstein B: Negative symptoms are related to both frontal and nonfrontal neuropsychological measures in chronic schizophrenia. Arch Gen Psychiatry 1992; 49:245–246Crossref, Medline, Google Scholar
28. Johannessen JO, McGlashan TH, Larsen TK, Horneland M, Joa I, Mardal S, Kvebæk R, Friis S, Melle I, Opjordsmoen S, Simonsen E, Haahr E, Vaglum P: Early detection strategies for untreated first-episode psychosis. Schizophr Res 2001; 51:39–46Crossref, Medline, Google Scholar
29. Kay SR, Fiszbein A, Opler LA: The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull 1987; 13:261–276Crossref, Medline, Google Scholar
30. Remington G, Kapur S, Zipursky RB: Pharmacotherapy of first-episode schizophrenia. Br J Psychiatry Suppl 1998; 33:66–70Google Scholar
31. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P), version 2. New York, New York State Psychiatric Institute, Biometrics Research, 1995Google Scholar
32. Gerlach J, Korsgaard S, Clemmesen P, Lauresen AM, Magelund G, Noring U, Povlsen UJ, Bech P, Casey DE: The St Hans Rating Scale for Extrapyramidal Syndromes: reliability and validity. Acta Psychiatr Scand 1993; 87:244–252Crossref, Medline, Google Scholar
33. Cannon-Spoor HE, Potkin SG, Wyatt RJ: Measurement of premorbid adjustment in chronic schizophrenia. Schizophr Bull 1982; 8:470–484Crossref, Medline, Google Scholar
34. Friis S, Sundet K, Rund BR, Vaglum P, McGlashan TH: Neurocognitive dimensions characterizing first-time psychotic patients. Br J Psychiatry Suppl 2002; 43:85–90Crossref, Google Scholar
35. Delis DC, Kramer JH, Kaplan E, Ober BA: The California Verbal Learning Test Manual. New York, Psychological Corp, 1987Google Scholar
36. Rund BR: Backward-masking performance in chronic and nonchronic schizophrenics, affectively disturbed patients, and normal control subjects. J Abnorm Psychol 1993; 102:74–81Crossref, Medline, Google Scholar
37. Lezak MD: Neuropsychological Assessment, 3rd ed. New York, Oxford University Press, 1995Google Scholar
38. Heaton RK, Chelune GJ, Talley JL, Kay GG, Curtiss G: Wisconsin Card Sorting Test Manual. Odessa, Fla, Psychological Assessment Resources, 1993Google Scholar
39. Spreen O, Strauss E: A Compendium of Neuropsychological Tests: Administration, Norms, and Commentary, 2nd ed. New York, Oxford University Press, 1998Google Scholar
40. Oltmanns TF, Neale JN: Schizophrenic performance when distractors are present: attention deficit or differential task difficulty? J Abnorm Psychol 1975; 84:205–209Crossref, Medline, Google Scholar
41. Cornblatt BA, Risch M, Faris G, Friedman D, Erlenmeyer-Kimling L: The Continuous Performance Test, Identical Pairs Version (CPT-IP), I: new findings about sustained attention in normal families. Psychiatry Res 1988; 26:223–238Crossref, Medline, Google Scholar
42. Wechsler D: Wechsler Adult Intelligence Scale—Revised. New York, Psychological Corp, 1981Google Scholar
43. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 3rd ed, revised (DSM-III-R). Washington, DC, APA, 1987, p 12Google Scholar
44. Friis S, Larsen TK, Melle I, Opjordsmoen S, Johannessen JO, Haahr U, Simonsen E, Rund BR, Vaglum P, McGlashan TH: Methodological pitfalls in early detection studies. Acta Psychiatr Scand 2003; 107:3–9Crossref, Medline, Google Scholar
45. Haas GL, Sweeney JA: Premorbid and onset features of first-episode schizophrenia. Schizophr Bull 1992; 18:373–386Crossref, Medline, Google Scholar
46. McGorry PD, Edwards J, Mihalopoulos C, Harrigan SM, Jackson HJ: EPPIC: an evolving system of early detection and optimal management. Schizophr Bull 1996; 22:305–326Crossref, Medline, Google Scholar
47. Harrigan SM, McGorry PD, Kirstev H: Treatment delay and outcome in first-episode psychosis: is there a critical point of decline? Schizophr Res 2002; 53(suppl 3):44–45Google Scholar
48. Ho B-C, Alicata D, Ward J, Moser DJ, O’Leary DS, Arndt S, Andreasen NC: Untreated initial psychosis: relation to cognitive deficits and brain morphology in first-episode schizophrenia. Am J Psychiatry 2003; 160:142–148Link, Google Scholar
49. Norman RM, Malla AK: Duration of untreated psychosis: a critical examination of the concept and its importance. Psychol Med 2001; 31:381–400Crossref, Medline, Google Scholar
50. Erlenmeyer-Kimling L, Roberts SA, Rock D, Adamo UH, Shapiro BM, Pape S: Prediction from longitudinal assessment of high-risk children, in Origins and Development of Schizophrenia: Advances in Experimental Psychopathology. Edited by Lenzenweger MF, Dworkin RH. Washington, DC, American Psychiatric Press, 1998, pp 427–445Google Scholar



