The Predictive Power of Peritraumatic Dissociation and Acute Stress Symptoms for Posttraumatic Stress Symptoms: A Three-Month Prospective Study
Abstract
OBJECTIVE: The authors prospectively examined the power of peritraumatic dissociation and acute stress symptoms in predicting posttraumatic stress disorder (PTSD) symptoms. METHOD: Thirty-five assault victims were assessed with the Peritraumatic Dissociative Experiences Questionnaire within 24 hours of the assault. Participants were reassessed 2 weeks after the trauma with the Stanford Acute Stress Reaction Questionnaire and 3 months after the trauma with the Clinician-Administered PTSD Scale and the Impact of Event Scale. Correlational analyses and a hierarchical multiple regression were conducted. RESULTS: Peritraumatic dissociation and acute stress symptoms were correlated with later PTSD symptoms and diagnosis. Together, peritraumatic dissociation and acute stress symptoms accounted for 33% of the variance in PTSD symptoms. CONCLUSIONS: These results support earlier findings that peritraumatic dissociative experiences and acute stress are robust predictors of PTSD. Such symptoms may be of use for identifying at an early stage individuals at highest risk of remaining symptomatic. Future studies should investigate the predictive power of specific peritraumatic and acute stress disorder symptom clusters.
The relationship between peritraumatic dissociation and posttraumatic stress disorder (PTSD) has been studied in war veterans, disaster victims, and traffic accident victims (1–4). Peritraumatic dissociation involves alterations in the experience of time, place, and person during and immediately after trauma exposure. Participants reporting more peritraumatic dissociation are at greater risk for developing PTSD (1–4). Studies also show that acute stress disorder after traffic accidents and crimes is a predictor of PTSD (5, 6). The DSM-IV diagnosis of acute stress disorder includes a set of symptoms experienced within the first month following exposure and includes symptoms of dissociation, intrusion, avoidance, and hyperarousal. We sought to extend the work of Shalev et al. (4) and Brewin et al. (5) by examining the power of both peritraumatic dissociation and acute stress in predicting PTSD symptoms and diagnosis 3 months after a traumatic event.
Method
Victims of violent assaults were consecutively recruited in a university hospital emergency department. The exclusion criteria were 1) a lasting unconsciousness, 2) misuse of alcohol or drugs, 3) a psychotic illness, or 4) a current life-threatening injury. Eighty-seven victims gave written informed consent and were assessed for peritraumatic dissociation within 24 hours of the assault. They were reinterviewed by a psychiatrist (P.B.) for acute stress disorder and PTSD symptoms and diagnosis 2 weeks and 3 months after the assault. Fifty-two participants dropped out between the first and last assessment, yielding a study group of 35 subjects. Twenty (57%) were women, 19 (54%) were married, and 18 (51%) were employed. The dropouts were younger (mean age=30.4 years, SD=11.5) than the participants (mean age=39.7, SD=16) (t=3.17, df=85, p=0.002) and had higher levels of unemployment (p=0.002, Fisher’s exact test). More of the dropouts had been assaulted with a weapon (χ2=7.44, df=4, p=0.006), but the dropouts and participants did not differ in terms of hospitalization in surgical units (χ2=0.10, df=4, p=0.75) or in terms of peritraumatic dissociation (t=0.6, df=84, p=0.55).
Peritraumatic dissociation was assessed by using the 10-item Peritraumatic Dissociative Experiences Questionnaire—Self-Report Version (2). The score on this questionnaire was the mean response across all items. Internal consistency of the 10-item Peritraumatic Dissociative Experiences Questionnaire was good (alpha=0.79). Previous studies reported alphas of 0.79–0.80 for the eight-item version of this questionnaire (2, 4). Acute stress disorder symptoms were assessed with the Stanford Acute Stress Reaction Questionnaire, a 30-item self-report instrument that includes subscales of dissociation, reexperiencing, avoidance, and hyperarousal (7). The Stanford Acute Stress Reaction Questionnaire was scored by summing all of the relevant items for each subscale. The reliability of the Stanford Acute Stress Reaction Questionnaire ranges from 0.80 to 0.95 with a test-retest reliability of 0.69 (7).
For the assessment of PTSD symptoms and diagnosis, we used the Impact of Event Scale (8) and the Clinician-Administered PTSD Scale (9). The Impact of Event Scale is a valid 15-item self-report measure that assesses symptoms of intrusion and avoidance (8). This scale provided a dimensional assessment of PTSD and was scored as the raw sum of all items. The Clinician-Administered PTSD Scale is a structured interview yielding a DSM-IV diagnosis of PTSD with test-retest reliability ranging from 0.90 to 0.98 (9).
The statistical significance level was set at 5% for two-sided tests. Mean scores were reported plus or minus one standard deviation. Analyses used t tests, Fisher’s exact tests, and chi-square tests to examine differences between participants who did or did not develop PTSD. To analyze the relationship between peritraumatic dissociation, acute stress symptoms, and PTSD symptoms, we computed Pearson’s correlations and a hierarchical multiple linear regression. There were no missing data.
Results
Of the 35 participants, 18 had been shot, stabbed, mugged, or threatened with a weapon and 17 had been badly beaten. Seven victims were hospitalized in surgical units. At 3 months, 12 participants had PTSD. There was no relation between PTSD status and age (mean age=44.1, SD=15.5, for PTSD subjects versus mean=37.5, SD=16.1, for subjects without PTSD) (t=1.17, df=33, p=0.25), marital status (p=0.27, Fisher’s exact test), level of employment (p=0.11, Fisher’s exact test), or type of trauma (χ2=0.35, df=4, N=35, p=0.55). As expected, the Peritraumatic Dissociative Experiences Questionnaire scores of the 12 participants with PTSD (mean=3.1, SD=0.9) were higher than the scores of the 23 participants without PTSD (mean=2.3, SD=0.6) (t=3.2, df=33, p<0.01). Also as expected, Stanford Acute Stress Reaction Questionnaire scores of the participants with PTSD (mean=88.2, SD=30) were higher than those of participants without PTSD (mean=59.5, SD=27.6) (t=2.8, df=33, p<0.01).
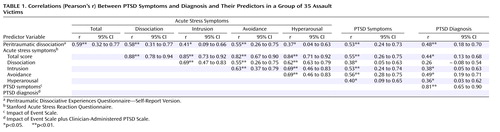
We examined Pearson’s intercorrelation coefficients between peritraumatic dissociation and acute stress symptoms and PTSD symptoms and diagnosis. As shown in Table 1, peritraumatic dissociation and acute stress symptoms were related to PTSD symptoms and diagnosis. The overlapping confidence intervals around the correlations, particularly the subscales of the Stanford Acute Stress Reaction Questionnaire, suggest that no early predictor is significantly stronger than any other.
We next compared the predictive power of peritraumatic dissociation and total acute stress symptoms in explaining the occurrence of PTSD symptoms 3 months after the trauma. After ruling out collinearity between our two predictors (variance inflation factor=1.53, tolerance=0.65), we computed a hierarchical multiple linear regression (10). Peritraumatic dissociation, which occurs first and is of short duration, was entered first and accounted for adjusted R2=25.8% of the PTSD symptoms (F=12.80, df=1, 33, p=0.001). Entered in the second step, the acute stress symptoms accounted for an additional 7% of the variance (t=2.10, p=0.044), for a total of 32.8% (F=9.25, df=1, 32, p=0.001). Reversing the order of entry of the variables led to acute stress symptoms explaining 28.1% of the PTSD symptoms and the peritraumatic dissociation explaining an additional 4.6% of the variance (t=1.80, p=0.08).
Discussion
To our knowledge, our study is the first to contrast prospectively and concurrently the power of peritraumatic dissociation and acute stress symptoms in predicting PTSD symptoms using well-established measures. The results of the multiple regression indicate that both variables are good predictors of subsequent PTSD symptoms. This replicates and extends the finding of others (1, 3–6). There were methodological limitations, however, such as a greater dropout rate among unemployed and younger participants. The small number of subjects also prevented us from making more fine-grained analyses, such as looking at acute stress symptom clusters in predicting PTSD. Although replication of these results is needed to draw firm conclusions, quantification of immediate dissociative experiences and acute stress symptoms may eventually help the clinician identify at an early stage traumatized victims at highest risk for developing PTSD.
 |
Received Jan. 31, 2001; revisions received March 15, Aug. 8, and Nov. 15, 2002; accepted Nov. 26, 2002. From the Service Universitaire de Psychiatrie et Psychologie Médicale, Hôpital Casselardit-La Grave, the Département des Urgences, and the Département d’Epidémiologie, Hôtel-Dieu, Centre Hospitalier Universitaire de Toulouse, France; the Department of Psychiatry, McGill University, Douglas Hospital Research Center, Montreal; and the UFR de Psychologie, Centre d’Etudes et de Recherches en Psychopathologie, Université de Toulouse-II, France. Address reprint requests to Dr. Birmes, Service Universitaire de Psychiatrie et Psychologie Médicale, Hôpital Casselardit-La Grave, Centre Hospitalier Universitaire de Toulouse, 170, Avenue de Casselardit, TSA 40031, 31059 Toulouse, Cedex 9, France; [email protected] (e-mail).
1. Fullerton CS, Ursano RJ, Epstein RS, Crowley B, Vance KL, Kao TC, Baum A: Peritraumatic dissociation following motor vehicle accidents: relationship to prior trauma and prior major depression. J Nerv Ment Dis 2000; 188:267-272Crossref, Medline, Google Scholar
2. Marmar CR, Weiss DS, Metzler T: Peritraumatic dissociation and posttraumatic stress disorder, in Trauma, Memory, and Dissociation. Edited by Bremner JD, Marmar CR. Washington, DC, American Psychiatric Press, 1998, pp 229-252Google Scholar
3. Koopman C, Classen C, Spiegel D: Predictors of posttraumatic stress symptoms among survivors of the Oakland/Berkeley, Calif, firestorm. Am J Psychiatry 1994; 151:888-894Link, Google Scholar
4. Shalev AY, Peri T, Canetti L, Schreiber S: Predictors of PTSD in injured trauma survivors: a prospective study. Am J Psychiatry 1996; 153:219-225Link, Google Scholar
5. Brewin CR, Andrews B, Rose S, Kirk M: Acute stress disorder and posttraumatic stress disorder in victims of violent crime. Am J Psychiatry 1999; 156:360-366Abstract, Google Scholar
6. Harvey AG, Bryant RA: Two-year prospective evaluation of the relationship between acute stress disorder and posttraumatic stress disorder following mild traumatic brain injury. Am J Psychiatry 2000; 157:626-628Link, Google Scholar
7. Cardena E, Koopman C, Classen C, Waelde LC, Spiegel D: Psychometric properties of the Stanford Acute Stress Reaction Questionnaire (SASRQ): a valid and reliable measure of acute stress. J Trauma Stress 2000; 13:719-734Crossref, Medline, Google Scholar
8. Horowitz MJ, Wilner N, Alvarez W: Impact of Event Scale: a measure of subjective stress. Psychosom Med 1979; 41:209-218Crossref, Medline, Google Scholar
9. Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM: The development of a Clinician-Administered PTSD Scale. J Trauma Stress 1995; 8:75-90Crossref, Medline, Google Scholar
10. Tabachnick BG, Fidell LS: Multiple regression, in Using Multivariate Statistics, 2nd ed. Edited by Tabachnick BG, Fidell LS. New York, HarperCollins, 1989, pp 123-191Google Scholar



