Unexplained Fatigue Syndromes in a Multinational Primary Care Sample: Specificity of Definition and Prevalence and Distinctiveness From Depression and Generalized Anxiety
Abstract
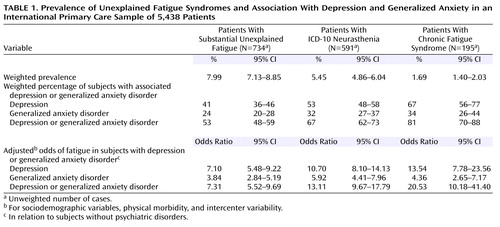
OBJECTIVE: The authors investigated whether narrow definitions of unexplained fatigue syndromes that require additional minor somatic symptoms are more strongly associated with psychiatric morbidity than wider ones. METHOD: This was a secondary analysis of the World Health Organization Collaborative Project on Psychological Problems in General Health Care. A total of 5,438 primary care patients from 14 countries were assessed with the Composite International Diagnostic Interview. RESULTS: The prevalence of fatigue syndromes fell from 7.99 to 1.69 as somatic criteria were added. Patients with depression or anxiety were more likely to report unexplained fatigue, but this association was stronger for definitions of unexplained fatigue with more somatic criteria. CONCLUSIONS: Definitions of unexplained fatigue syndromes that require more somatic criteria selected more patients with psychiatric disorders in this culturally diverse sample. These findings might have implications for the revision of existing international diagnostic criteria for neurasthenia or chronic fatigue syndrome.
There is considerable overlap between unexplained fatigue syndromes and psychiatric morbidity in both the community and primary health care (1). It has been argued that this strong association results from the use of broad case definitions and that stricter, narrower criteria for fatigue syndromes with lower prevalence would have less overlap with psychiatric morbidity (2). These narrower definitions require the presence of other unexplained physical symptoms in addition to fatigue. However, the little empirical evidence that exists does not support the notion that narrowing this definition reduces the association with psychiatric morbidity (3). Furthermore, those with more somatic symptoms tend to have more psychiatric morbidity (4). The current study aimed to provide a stringent test of the hypothesis that narrow definitions of fatigue syndromes have less overlap with psychiatric morbidity and was carried out in a culturally diverse sample of primary health care patients in 14 countries.
Method
This study was a secondary analysis of the World Health Organization Collaborative Project on Psychological Problems in General Health Care (5). A total of 25,916 consecutive primary care patients in 15 centers from 14 countries were screened with the 12-item General Health Questionnaire. There was a 96.1% rate of response (range=91%–100%). Patients were selected for a baseline assessment by using a stratified random sampling according to site-specific General Health Questionnaire thresholds. The baseline assessment included the Composite International Diagnostic Interview modified for use in primary care and involved 5,438 patients (62% rate of response, range=43%–99%). The intercenter reliability in the form of an interviewer-observer reliability coefficient for the primary care version of the Composite International Diagnostic Interview was found to be 0.92 overall, ranging from 0.81 to 1.00 for individual sections. More details on the methods of the original study are given elsewhere (5).
The symptom of fatigue was evaluated with questions from the Composite International Diagnostic Interview (6). Three screening questions were asked of all subjects (“In the past month have you felt tired all the time?” “Do you get easily tired while performing everyday tasks?” “Does even minimal physical effort cause exhaustion?”). Then the interviewer asked a specific sequence of questions to determine the clinical importance and possible cause of the symptom. Medical causes were excluded by local physicians using predefined rules. Three case definitions of unexplained fatigue were used in the present study: 1) substantial unexplained fatigue: unexplained fatigue during the past month and inability to recover from it by means of rest or relaxation, 2) ICD-10 neurasthenia: substantial unexplained fatigue plus one or more of the following: muscular aches and pains, dizziness, headaches, sleep disturbance, and inability to relax, and 3) chronic fatigue syndrome: an approximation of the Centers for Disease Control’s 1994 definition (2), defined as substantial unexplained fatigue plus three or more of the following: pain, headache, unrefreshing sleep, impaired concentration, and impaired memory. It should be noted that we could not apply the usual time criteria (3 months for neurasthenia and 6 for chronic fatigue syndrome) because these were not measured consistently in the data set.
Data analysis was carried out by using the survey commands of Stata 6.0 (7). All the analyses were carried out by using probability weights to account for the two-phase design of the study. The prevalence of fatigue syndromes and 95% confidence intervals (CIs) were calculated by using the “svyprop” command in Stata. The association of psychiatric disorders with fatigue syndromes was estimated with a series of weighted logistic regression models by using the “svylogit” command in Stata. We used the presence of fatigue syndrome (yes or no) as the dependent variable and the psychiatric disorders of interest as independent variables and adjusted for various sociodemographic variables, intercenter variability, and the presence of physical morbidity. The latter was a binary variable derived by asking patients whether they were suffering from a list of common chronic medical conditions. Adjusted odds ratios and 95% CIs for fatigue were calculated for subjects with a psychiatric disorder in relation to comparison subjects.
Results
As expected, the prevalence of unexplained fatigue syndromes fell from about 7.99 to 1.69 (Table 1) as criteria were added. Overlap with depression and generalized anxiety disorder was greater for the narrower definitions (which require additional physical symptoms), with over 80% of the patients with chronic fatigue syndrome also having either depression or generalized anxiety disorder. Although the prevalence of fatigue varied considerably between centers, this pattern was consistently seen in all centers. The pattern persisted after adjustment for a number of potentially confounding variables (Table 1).
Discussion
It is repeatedly argued by those committed to a certain, largely organic, view of fatigue syndromes that broadening the definition of fatigue syndromes has led to a spurious association with psychiatric disorders. The current report shows this to be erroneous: a wider definition of unexplained fatigue syndromes results in more prevalence and has less overlap with psychiatric disorders than definitions that require additional minor symptoms. This can be explained by the positive association between psychiatric morbidity and somatic symptoms (4) since the narrower definitions of fatigue require the presence of additional unexplained somatic symptoms.
This study has some limitations. First, it was carried out among primary care patients, and the possibility of a Berksonian bias cannot be excluded: if subjects with both unexplained fatigue and psychiatric morbidity were more likely to consult a primary care physician, then the association would be overestimated. However, the association of fatigue with psychiatric morbidity has been found in community studies as well (1), and the odds ratios reported here are generally comparable with previous research. Second, this was a secondary analysis of a data set collected for other purposes. Our approximation of fatigue syndromes was limited from the data available. We could not apply the 3- or 6-months duration criteria, and the odds ratios reported might have been underestimated if psychiatric disorders are associated with the chronicity of fatigue. However, this study was carried out in several countries around the world, both developed and developing, and used a large sample size. Our findings extend the findings of a hospital-based study in America (3) and a primary care study in the United Kingdom (8) that observed that the somatic symptoms included in the definition of chronic fatigue syndrome were positively correlated with measures of psychiatric morbidity.
The ICD-11 is currently under development, and diagnosis is an important aspect of medical care that should help doctors and their patients. Diagnostic criteria for fatigue syndromes will need to acknowledge the overlap with psychiatric morbidity. Creating narrow definitions will not help identify a “pure” form of chronic fatigue and may hinder rather than help us understand more about fatigue and its effective treatment.
 |
Received May 6, 2002; revision received Aug. 6. 2002; accepted Oct. 8, 2002. From the Department of Psychiatry, University of Bristol; and the Department of Psychiatry, University of Ioannina School of Medicine, Ioannina, Greece. Address reprint requests to Dr. Petros Skapinakis, Department of Psychiatry, University of Bristol, Cotham House, Cotham Hill, Bristol BS6 6JL, U.K.; [email protected] (e-mail). This study was begun while Dr. Skapinakis was studying for a Ph.D. at the University of Wales College of Medicine and was funded by the Alexander S. Onassis Public Benefit Foundation. The authors thank Professor Simon Wessely and Dr. Gregory Simon for their comments on a draft of the article. Data reported in this article were collected as part of the World Health Organization Collaborative Project on Psychological Problems in General Health Care. Participating investigators include O. Ozturk and M. Rezaki, Ankara, Turkey; C. Stefanis, Athens, Greece; S.M. Channabasavana and T.G. Sriram, Bangalore, India; H. Helmchen and M. Linden, Berlin; W. van der Brink and B. Tiemens, Groningen, the Netherlands; M. Olatawura and O. Gureye, Ibadan, Nigeria; O. Benkert and W. Maier, Mainz, Germany; R. Gater and S. Kisely, Manchester, U.K.; Y. Nakane and S. Michitsuji, Nagasaki, Japan; Y. Lecrubier and P. Boyer, Paris; J. Costa e Silva and L. Villano, Rio de Janeiro; R. Florenzano and J. Acuna, Santiago, Chile; G.E. Simon and M. von Korff, Seattle; Y. He-Quin and X. Shi Fu, Shanghai; and M. Tansella and C. Bellantuono, Verona, Italy. The study advisory group includes J. Costa e Silva, D.P. Goldberg, Y. Lecrubier, M. vonKorff, and H-U Wittchen. Coordinating staff at World Health Organization headquarters includes N. Sartorius and T.B. Ustun.
1. Skapinakis P, Lewis G, Meltzer H: Clarifying the relationship between unexplained chronic fatigue and psychiatric morbidity: results from a community survey in Great Britain. Am J Psychiatry 2000; 157:1492-1498Link, Google Scholar
2. Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A (International Chronic Fatigue Syndrome Study Group): The chronic fatigue syndrome: a comprehensive approach to its definition and study. Ann Intern Med 1994; 121:953-959Crossref, Medline, Google Scholar
3. Katon W, Russo J: Chronic fatigue syndrome criteria: a critique of the requirement for multiple physical complaints. Arch Intern Med 1992; 152:1604-1609Crossref, Medline, Google Scholar
4. Simon GE, VonKorff M: Somatization and psychiatric disorder in the NIMH Epidemiologic Catchment Area study. Am J Psychiatry 1991; 148:1494-1500Link, Google Scholar
5. Sartorius N, Ustun TB, Costa e Silva JA, Goldberg D, Lecrubier Y, Ormel J, VonKorff M, Wittchen HU: An international study of psychological problems in primary care: preliminary report from the World Health Organization Collaborative Project on “Psychological Problems in General Health Care.” Arch Gen Psychiatry 1993; 50:819-824Crossref, Medline, Google Scholar
6. Robins LN, Wing J, Wittchen HU, Helzer JE, Babor TF, Burke J, Farmer A, Jablenski A, Pickens R, Regier DA, et al: The Composite International Diagnostic Interview: an epidemiological instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch Gen Psychiatry 1988; 45:1069-1077Crossref, Medline, Google Scholar
7. Stata Reference Manual: Release 6.0. College Station, Tex, Stata Corp, 1999Google Scholar
8. Wessely S, Chalder T, Hirsch S, Wallace P, Wright D: Psychological symptoms, somatic symptoms, and psychiatric disorder in chronic fatigue and chronic fatigue syndrome: a prospective study in the primary care setting. Am J Psychiatry 1996; 153:1050-1059Link, Google Scholar



