Individual Differences in a Husband and Wife Who Developed PTSD After a Motor Vehicle Accident: A Functional MRI Case Study
This report describes a husband and wife with acute posttraumatic stress disorder (PTSD) who exhibited different subjective, psychophysiological, and neurobiological responses to traumatic script-driven imagery that caused them to reexperience their traumas. The couple, who had been trapped in their car during a serious motor vehicle accident, was assessed for responses to script-driven traumatic imagery with a heart rate monitor and functional magnetic resonance imaging (fMRI). The accident involved more than 100 vehicles, multiple deaths, and serious injuries. After they crashed into a car in front of them, both subjects were trapped in their car for several minutes, during which they witnessed a child burn to death and feared that they too would die. Neither sustained physical injuries. Both reported reliving their peritraumatic responses. The man experienced intense anxiety, arousal, and escape-focused cognitions; his heart rate increased 13 bpm from baseline. Blood-oxygenation-level-dependent (BOLD) signal increases were found in his anterior frontal, anterior cingulate, superior and medial temporal, thalamic, parietal, and occipital brain regions. In contrast, the woman reported being extremely “numb” and “frozen,” had no heart rate change, and had BOLD signal increases only in occipital regions. This report highlights the importance of individual differences in subjective and biological characteristics of posttraumatic remembrances, particularly those related to peritraumatic dissociation and numbing.
Initial Assessment
Both subjects were assessed 4 weeks after the accident with the Structured Clinical Interview for DSM-IV (1), the Clinician-Administered PTSD Scale (2), the Peritraumatic Dissociative Experiences Scale (3), and the Dissociative Experiences Scale (4). Both met criteria for acute stress disorder, with score on the Clinician-Administered PTSD Scale of 74 and 86 for the husband and wife, respectively. The wife experienced much greater peritraumatic dissociation and had a score on the Peritraumatic Dissociative Experiences Scale of 22 versus her husband’s score of 1; however, both had low trait dissociation, with scores on the Dissociative Experiences Scale of less than 3. Responses to script-driven traumatic imagery were measured with 4-T fMRI, a heart rate monitor, and self-report measures (for detailed methods, see references 5–8).
Case Presentations
Mr. A, the husband, was a 48-year-old professional who was completely healthy until the accident. He reported feeling extremely aroused during the accident and was actively involved, both cognitively and behaviorally, in rescuing himself and his wife, ultimately breaking the windshield to allow their escape. The next day, he began experiencing flashbacks and nightmares, and his reexperiencing symptoms often included feeling as if the accident were recurring. He also became very psychologically and physiologically aroused when thinking or talking about the accident. He avoided driving on the highway where the accident occurred, as well as thoughts and conversations about it. His sleep was very poor and his concentration severely impaired, rendering him unable to function at work. Other hyperarousal symptoms were irritability and startle reactions. He reported no past or present substance abuse, past psychiatric history, or current medical problems and was not taking any medications. He reported no family psychiatric history, described his childhood as uneventful, stated he had a good relationship with his parents, and reported no history of neglect or emotional, physical, or sexual abuse. He was sociable as a child and adolescent, completed an undergraduate accounting degree, and had since worked as an accountant.
Ms. A, the wife, was a 55-year-old professional who was healthy until the accident. She described being “in shock” during the accident and, although trapped but not pinned in the car, reported, “I could hardly move because I was completely frozen.” Like her husband, she began experiencing flashbacks and nightmares the next day and often felt as if it were recurring, although for her, this involved feeling “numb” and “frozen.” She avoided driving and reading newspaper stories about the accident. Her sleep was extremely poor, her concentration was significantly impaired, and she was highly irritable and easily angered. Her work functioning was completely impaired (she sold her business several months after the accident). She reported no past or present substance abuse but reported a postpartum depression after the birth of her first child and a past history of mild panic disorder. She had no medical problems and was not taking any medications. She reported no family psychiatric history but described her childhood as quite “traumatic.” That is, although she reported no history of physical or sexual abuse, her father died when she was 9 years old, and she described her mother as a very “cold” and “distant” woman with whom she did not feel safe. She was sociable while growing up, and her school performance was above average. She graduated from business school and ran a business for several years before the accident.
In response to script-driven imagery of the accident, the husband reported a vivid memory that included thinking about how to escape, breaking the windshield, and feeling very anxious and “jumpy.” His heart rate increased 13 bpm from baseline. His experience corresponded to higher BOLD signals from the prescript baseline in anterior frontal, anterior cingulate, superior and medial temporal (including left amygdala), left thalamic, and parietal and occipital regions (Figure 1 and Table 1). Six months later, after a course of exposure-based treatment, he no longer had PTSD.
In marked contrast—but consistent with reliving her original peritraumatic response—the wife reported feeling extremely “numb” and “frozen” while recalling the traumatic memory, and her heart rate did not change from baseline. Increases in BOLD signal intensity from baseline were only found in occipital regions (Brodmann’s areas 18 and 19) (Figure 1 and Table 1). Of importance, there were no differences in baseline brain activation between her and her husband, and her neural responses to script-driven imagery of sad and anxious memories were similar to his (data not shown). After 6 months of treatment, including prolonged exposure, she still had clinically significant PTSD. It is interesting to note that Foa (8) suggested emotional numbness to be one of the factors contributing to a lack of successful processing of trauma.
Discussion
In terms of subjective experiences, heart rate responses, and patterns of neural activation, these two survivors of the same traumatic event exhibited two distinct yet internally coherent peritraumatic and subsequent pathological responses to traumatic reminders. The husband’s reports of cognitive and behavioral activation along with physiological arousal are consistent with observed increases in anterior frontal, thalamic, and amygdala activations and heart rate. His response also resembles the traditionally described hyperarousal response to script-driven imagery in PTSD (9). In contrast, the woman’s “numb” and “frozen” subjective experiences, lack of an increase in heart rate, and very different pattern of neural activations, despite having a severe case of acute and subsequent PTSD, add to an emerging literature on individual differences in posttraumatic pathophysiology (10–14).
In summary, our fMRI results demonstrate that PTSD patients can have very different responses, both subjectively and biologically, while reexperiencing traumatic events. They also indicate the need for more research on dissociative and numbing responses associated with an absence of increased cardiovascular arousal as distinct types of PTSD reexperiencing symptoms. Finally, our fMRI findings suggest that different neuronal mechanisms may generate these different reactions to traumatic reminders.
 |
Received July 31, 2002; revision received Dec. 17, 2002; accepted Dec. 19, 2002. From the Department of Psychiatry, Medical Biophysics, University of Western Ontario, London, Ontario, Canada; the Department of Psychiatry, Boston University School of Medicine, Boston; and the Robarts Research Institute, London, Ontario, Canada. Address reprint requests to Dr. Lanius, Department of Psychiatry, London Health Sciences Centre, 339 Windermere Rd., PO Box 5339, London, ON, Canada N6A 5A5; [email protected] (e-mail). Supported by a grant from the Canadian Institutes of Health Research and the Ontario Mental Health Foundation.
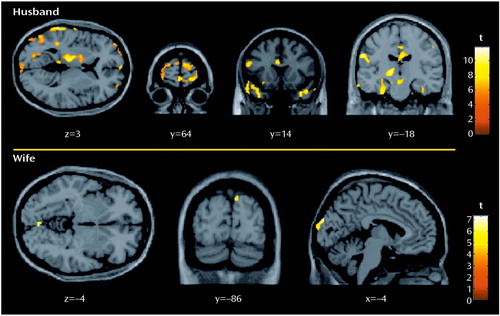
Figure 1. Images Showing Brain Regions With Significant Functional MRI Responsesa to Traumatic Imagery in a Husband and Wife Who Developed PTSD After a Motor Vehicle Accident
aBrain activation was determined with blood-oxygen-level-dependent functional MRI. Significant change from baseline was defined as p<0.05 (statistical parametric mapping [t], df=82.39; cluster size >10 voxels).
1. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview (SCID) for DSM-IV Axis I Disorders. Washington, DC, American Psychiatric Press, 1977Google Scholar
2. Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Charney DS, Keane TM: Clinical-Administered PTSD Scale for DSM-IV. Boston and West Haven, Conn, National Center for Posttraumatic Stress Disorder, 1995Google Scholar
3. Marmar CR, Weiss DS, Metzler TJ: The Peritraumatic Dissociative Experiences Questionnaire, in Assessing Psychological Trauma and PTSD. Edited by Wilson JP and Keane TM. New York, Guilford Press, 1997, pp 412-428Google Scholar
4. Bernstein EM, Putnam FW: Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis 1986; 174:727-735Crossref, Medline, Google Scholar
5. Lanius RA, Williamson PC, Densmore M, Boksman K, Gupta MA, Neufeld RW, Gati JS, Menon RS: Neural correlates of traumatic memories in posttraumatic stress disorder: a functional MRI investigation. Am J Psychiatry 2001; 158:1920-1922Link, Google Scholar
6. Bremner JD, Narayan M, Staib LH, Southwick SM, McGlashan T, Charney DS: Neural correlates of memories of childhood sexual abuse in women with and without posttraumatic stress disorder. Am J Psychiatry 1999; 156:1787-1795Abstract, Google Scholar
7. Shin LM, McNally RJ, Kosslyn SM, Thompson WL, Rauch SL, Alpert NM, Metzger LJ, Lasko NB, Orr SP, Pitman RK: Regional cerebral blood flow during script-driven imagery in childhood sexual abuse-related PTSD: a PET investigation. Am J Psychiatry 1999; 156:575-584Abstract, Google Scholar
8. Foa EB: Psychological processes related to recovery from a trauma and an effective treatment for PTSD. Ann NY Acad Sci 1997; 821:410-424Crossref, Medline, Google Scholar
9. Pitman RK, Shalev AY, Orr SP: Posttraumatic stress disorder: emotion, conditioning and memory, in The New Cognitive Neurosciences. Edited by Gazzaniga MS. Cambridge, Mass, MIT Press, 2000, pp 1133-1147Google Scholar
10. Griffin MG, Resick PA, Mechanic MB: Objective assessment of peritraumatic dissociation: psychophysiological indicators. Am J Psychiatry 1997; 154:1081-1088Link, Google Scholar
11. Lanius RA, Williamson PC, Boksman K, Densmore M, Gupta M, Neufeld RW, Gati JS, Menon RS: Brain activation during script-driven imagery induced dissociative responses in PTSD: a functional magnetic resonance imaging investigation. Biol Psychiatry 2002; 52:305-311Crossref, Medline, Google Scholar
12. Mason JW, Wang S, Yehuda R, Riney S, Charney DS, Southwick SM: Psychogenic lowering of urinary cortisol levels linked to increased emotional numbing and a shame-depressive syndrome in combat-related posttraumatic stress disorder. Psychosom Med 2001; 63:387-401Crossref, Medline, Google Scholar
13. Nishith P, Griffin MG, Poth TL: Stress-induced analgesia: predictions of posttraumatic symptoms in battered versus nonbattered women. Biol Psychiatry 2002; 51:867-874Crossref, Medline, Google Scholar
14. Osuch EA, Benson B, Geraci M, Podell D, Herscovitch P, McCann UD, Post RM: Regional cerebral blood flow correlated with flashback intensity in patients with posttraumatic stress disorder. Biol Psychiatry 2001; 50:246-253Crossref, Medline, Google Scholar



