Major Depression and Associated Impairment: Same or Different Genetic and Environmental Risk Factors?
Abstract
OBJECTIVE: Impairment was added as a diagnostic criterion for many psychiatric disorders in DSM-IV. Does the addition of impairment influence only prevalence rates, or does it also introduce new etiological factors into psychiatric diagnoses? METHOD: A lifetime history of major depression and associated functional impairment was assessed by personal interview with 3,669 female and 4,377 male twins from the population-based Virginia Twin Registry. Structural equation modeling was used to estimate the correlation between risk factors for major depression and associated functional impairment. RESULTS: While the risk factors for major depression and associated functional impairment are substantially correlated, they are not identical. The most parsimonious model suggests that over a quarter of the variance in associated functional impairment is due to factors unrelated to risk for major depression. Of the variance unique to associated functional impairment, approximately one-third is familial. The relationship between associated functional impairment and major depression did not differ significantly between men and women. CONCLUSIONS: Risk factors for major depression and associated functional impairment are substantially but imperfectly correlated. The addition of associated functional impairment as a criterion for the diagnosis of major depression not only lowers prevalence estimates but also introduces a small set of new etiological factors into the diagnosis of major depression.
DSM-IV added clinically significant distress or associated functional impairment to the criterion used to diagnose many psychiatric disorders. This change in nomenclature was partly prompted by the high estimated prevalence of psychiatric disorders in community surveys, the variation in prevalence estimates across surveys, and their limited usefulness for determining service needs (1). It has been argued that the application of criteria for associated functional impairment will yield more meaningful prevalence estimates because impairment is a better indicator of harmful dysfunction and need for treatment than the presence of a psychiatric syndrome alone (2). The implications of using associated functional impairment to define cases of illness remain unclear.
Associated functional impairment may be etiologically related to psychiatric syndromes in three ways. First, the risk factors for syndrome and associated functional impairment may be identical (Figure 1, top). Using associated functional impairment to define a case would alter the diagnostic threshold by excluding individuals who did not have associated functional impairment but would not change the associated risk factors. Second, the risk factors for syndrome and associated functional impairment may be correlated but not identical (Figure 1, middle). Using associated functional impairment to define a case would therefore alter the diagnostic threshold and introduce into the psychiatric diagnostic process a new set of risk factors specific to associated functional impairment. Third, the risk factors for syndrome and associated functional impairment could be entirely distinct (Figure 1, bottom). Associated functional impairment would solely measure risk factors for coping with mental illnes, but these factors would be unrelated to the risk factors for syndrome. Currently, we do not know which of these alternatives is true for any of the major psychiatric syndromes defined by DSM-IV.
In this report, we examine the relationship between major depression and associated functional impairment in an epidemiological twin study with the goal of discriminating between the three etiological schemas outlined in Figure 1. This paradigm offers several advantages over clinical studies or epidemiological studies of unrelated individuals. An epidemiological sample will yield an unbiased estimate of the relationship between major depression and associated functional impairment independent of help seeking. The pattern of twin resemblance in an epidemiological sample will allow us to extend our etiological schema to estimate the genetic and environmental risk factors for major depression, and their continuity with the genetic or environmental risk factors for associated functional impairment. The pattern of resemblance in male and female twins will also allow us to estimate if there are sex differences in the relationship between major depression and associated functional impairment.
Method
Subjects
The Caucasian twins who are the subject of this report are enrolled in two ongoing longitudinal studies of genetic and environmental risk factors for common psychiatric and substance use disorders. The first study comprised female-female twin pairs and the second study comprised male-male and male-female twin pairs. Both male and female twin subjects were initially ascertained by the Virginia Twin Registry by means of a systematic review of all birth certificates in the Commonwealth of Virginia.
Female-female pairs were eligible to participate in ongoing Virginia Twin Registry studies if they were born between 1934 and 1971, if both members of the pair completed a mailed questionnaire (3), and if either member of a pair completed a subsequent structured psychiatric interview in person or by telephone. The individual rate of response to the initial questionnaire was approximately 64%, but the cooperation rate was almost certainly higher than this, since an unknown number of twins did not receive their questionnaire because of faulty addresses, improper forwarding of mail, and the like. The individual response rate to the initial interview was 91.9% (N=2,164 of 2,354). Of the completed interviews, 89.3% were completed face to face, nearly all in the twin’s home, and 10.7% (mostly twins living outside Virginia) were interviewed by telephone. Interviews were conducted between 1988 and 1989. Male-male and male-female pairs were eligible to participate in ongoing Virginia Twin Registry studies if they were born between 1940 and 1974 and both members of the pair completed a structured psychiatric interview by telephone. Unlike the female-female pairs, this interview represented the first contact with the male-male and male-female pairs. The individual response rate to the interview was 72.4% (6,815 of 9,418) (4). Interviews were conducted between 1993 and 1996. After complete description of the current study to the subjects, written informed consent was obtained.
Twins were included in the current study if each member of a pair completed the major depression module of the first structured psychiatric interview administered to the female-female and male-male and male-female groups. The eligible total group comprised 8,046 individual twins (4,377 male and 3,669 female) from 851 male monozygotic, 641 male dizygotic, 671 female monozygotic, 467 female dizygotic, and 1,393 opposite-sex dizygotic pairs. Twin zygosity was determined by use of standard questions (5), photographs, restriction length polymorphism markers (6), and polymerase chain reaction zygosity tests. The mean age of the eligible female twins from female-female pairs, male twins from male-male and male-female pairs, and female twins from male-female pairs at interview was 28.96 years (SD=7.68, range=17–54), 34.73 (SD=9.09, range=19–56), and 34.68 (SD=8.89, range=19–56), respectively.
Assessment of Impairment
Lifetime history of major depression was assessed at interview by using an adapted version of the Structured Clinical Interview for DSM-III-R (7). Test-retest reliability (kappa) of lifetime major depression over a mean of 30 days (SD=9) among 375 twins was 0.66.
Associated functional impairment was assessed at the end of the major depression module by asking subjects, “During the worst period, did these feelings interfere with your daily tasks (keeping house for a housewife, school for a student, work for a worker, etc.)?” If a subject answered yes to this question, he or she was asked a series of secondary probes, which might include, “Could you still do (job/housework) the way you usually do? What could you still do? Would others at work (or your supervisor) notice that you weren’t your usual self?” Answers to these probes were used to rate impairment as absent, moderate, or severe. “No impairment” meant virtually no objective impact of symptoms on functioning. “Moderate impairment” meant functioning with some difficulty. “Severe impairment” meant nearly nonfunctional: couldn’t go to work, couldn’t do any housework, etc. Subjects were rated as having no or clinically insignificant (rating=0), moderate (rating=1), or severe (rating=2) impairment.
Statistics
A structural equation model known as a causal, contingent, or common pathway model (8) was used to model the correlation between the risk factors for major depression and associated functional impairment in twins (Figure 2). The model is causal because it assumes a direct path (b) from the risk factors for major depression to the risk factors for associated functional impairment. The model is contingent because associated functional impairment is assessed only in those with a history of major depression; it is “common pathway” because genetic and environmental effects on major depression can only affect associated functional impairment by flowing through the observed phenotype of major depression. This model assumes that risk for lifetime major depression (coded as 1 or 0) may be modeled as a normally distributed underlying continuum of risk and that an individual’s estimated position on this underlying continuum reflects the severity of his or her risk for developing major depression. Individuals with subthreshold major depression were not surveyed about associated functional impairment, and all individuals with no or subthreshold major depression are therefore coded as missing for associated functional impairment.
The estimated risk factors for major depression are divided into additive genetic (Ad), common environmental (Cd), and individual-specific environmental components (Ed), in which the subscript d indicates that they are specific for major depression. The risk factors for associated functional impairment may derive from two sources: risk factors shared with major depression (reflected in path b) and risk factors independent of major depression (subdivided into additive genetic [Ai], common environmental [Ci], and individual-specific environmental components [Ei], whereas the subscript i indicates that they are specific for associated functional impairment). If all risk factors for major depression similarly influenced risk for associated functional impairment, then b would approach 1, and ai, ci, and ei would approach zero. If risk factors for major depression and associated functional impairment were unrelated, b would approach zero and associated functional impairment would be entirely due to the effects of ai, ci and ei. If risk factors for major depression and associated functional impairment are related but not identical, then b would be between 0 and 1, and associated functional impairment would be caused by the genetic and environmental risk factors for major depression and by a set of unique genetic and/or environmental risk factors for associated functional impairment.
Sex Differences
The CCC model was fit within the framework of a sex-limitation model which has been described in detail elsewhere (9). In brief, this model evaluates sex differences by estimating the correlation between the genetic and familial environmental risk factors for major depression in men and women. If the correlation is zero, this indicates that the risk factors are entirely different in men and women. If the correlation is 1, this indicates that the risk factors are identical in men and women. If the correlation lies between 0 and 1, this indicates that there are risk factors that are partly shared by men and women and partly specific to each sex. These correlations therefore allow us to test if the same genes or familial environmental effects influence the risk factors for major depression in men and women. Moreover, to the extent that the risk factors for major depression and associated functional impairment are correlated, the genetic and familial environmental correlation for major depression in males and females will also mediate sex differences in associated functional impairment. There is no correlation estimated between the individual-specific environmental risk factors for major depression in men and women because these are, by definition, unshared by relatives, irrespective of sex.
To extend the CCC model to test for sex differences, the model in Figure 1 was therefore drawn twice, once for male twins and once for female twins. A correlation path was drawn between the genetic risk factors for major depression in males and females, and another was drawn between the common environmental risk factors for major depression in males and females. The information for estimating these correlations comes from the opposite-sex dizygotic twin pairs. Sex differences in the relative magnitude of the risk factors for major depression and associated functional impairment are evaluated by comparing the fit of a model in which the risk factors are estimated separately for each sex with one in which the risk factors are constrained to be equal in men and women. If there is no statistically significant change in the fit of the constrained model, we infer that the relative magnitude of the risk factors is similar in men and women. Sex differences in major depression (but not associated functional impairment) have been reported elsewhere (4, 10).
Evaluating Model Fit
The fit of our twin model is evaluated by maximum likelihood estimation. The relative fit of different submodels is estimated by subtracting twice the difference in the log likelihood of one model from another. This difference in log likelihood between models functions like a chi-square test. A change in model fit of 3.84 units for each degree of freedom difference between models constitutes a statistically significant change in model fit at p=0.05.
Results
Group Characteristics
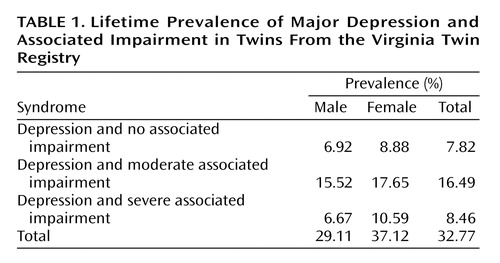
The lifetime prevalence of major depression with and without associated functional impairment among men and women from matched twin pairs is given in Table 1. The women had a significantly higher lifetime prevalence of any major depression and major depression with severe associated functional impairment than men (p=0.05). Twins from matched versus unmatched pairs did not have a significantly different prevalence of major depression (32.77% versus 32.61%) (χ2=0.01, df=1, p=0.92) or associated functional impairment (none or mild: 23.85% versus 24.03%; moderate: 50.32% versus 53.31%; severe: 25.82% versus 22.65%) (χ2=1.83, df=2, p=0.40).
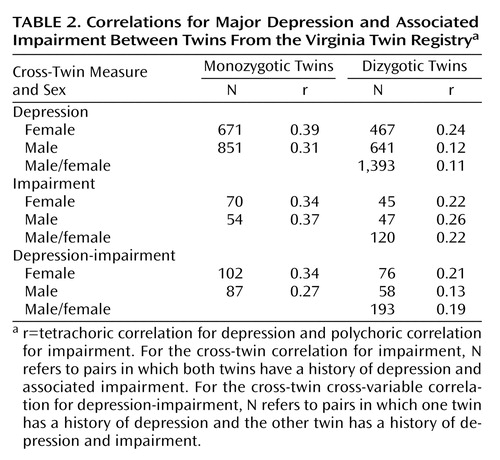
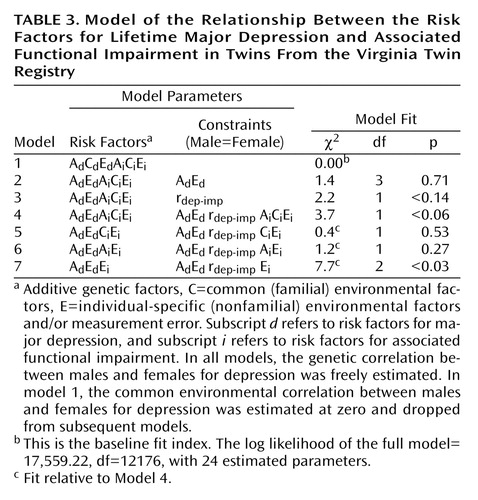
Model Fitting
Twin correlations for major depression and associated functional impairment by sex and zygosity are given in Table 2. The twin models that were fit to the male and female data are summarized in Table 3. In the full model (model 1), the correlation between the genetic risk factors for major depression in males and females is estimated to be 0.54 (confidence interval [CI]=0.20–0.65). The correlation between the risk factors for major depression and associated functional impairment is estimated to be 0.61 (CI=0.56–0.86) in females and 0.71 (CI=0.56–0.77) in males. Risk factors for associated functional impairment unrelated to those for major depression are estimated to account for 39% of the variance in associated functional impairment in females and 29% in males. Total risk for associated functional impairment is estimated to reflect genetic effects shared with major depression (in males, 22%, CI=3%–30%; in females, 19%, CI=0%–26%), genetic effects specific to associated functional impairment (in males, 0%, CI=0%–16%; in females, 8%, CI=0%–25%), familial environmental effects shared with major depression (in males, 0%, CI=0%–16%; in females, 5%, CI=0%–22%), familial environmental effects specific to associated functional impairment (in males, 14%, CI=1%–25%; in females, 0%, CI=0%–12%), individual-specific environmental effects and measurement error shared with major depression (in males, 49%, CI=40%–58%; in females, 38%, CI=32%–45%), and individual-specific environmental effects specific to associated functional impairment and/or errors in the measurement of associated functional impairment (in males, 14%, CI=4%–30%; in females, 30%, CI=9%–56%).
The results obtained by comparing the statistical fit of various submodels relative to the full model (Table 3) suggest that 1) there are no statistically significant sex differences in the magnitude of the genetic versus environmental effects on major depression (model 2), 2) there are no statistically significant sex differences are in the magnitude of the correlation between the risk factors for major depression and associated functional impairment (model 3), 3) there are no statistically significant sex differences in the magnitude of the genetic versus environmental effects on associated functional impairment that are unrelated to major depression (model 4), 4) there are familial risk factors for associated functional impairment that are unrelated to major depression (model 7), but these are small in magnitude, and 5) we cannot discriminate statistically between the importance of genetic versus familial environmental risk factors specific to associated functional impairment in our reduced models (model 5 and model 6).
We consider model 4 (in which both genetic and familial environmental effects on associated functional impairment that are unrelated to major depression are freely estimated) the most parsimonious summary of our data. In this model, the heritability of major depression is 35% in men and women. The correlation between the genetic risk factors for major depression in men and women is 0.54. The correlation between the risk factors for major depression and associated functional impairment is 0.78. Total risk for associated functional impairment in men and women is estimated to reflect genetic effects shared with major depression (25%), genetic effects specific to associated functional impairment (4%), familial environmental effects specific to associated functional impairment (5%), individual-specific environmental effects plus measurement error shared with major depression (47%), and individual-specific environmental effects specific to associated functional impairment and/or errors in the measurement of associated functional impairment (19%).
Discussion
In our epidemiological sample of adult twins, the risk factors for major depression and associated functional impairment were substantially correlated but clearly not identical. This finding is consistent with our second etiological schema (Figure 1, middle). Adding criteria for associated functional impairment to the diagnosis of major depression will have two effects. It will alter the diagnostic threshold, and it will index a new but relatively small set of risk factors unrelated to the syndrome of major depression.
The observed correlation between the risk factors for major depression and associated functional impairment is consistent with prior evidence for a strong association between the severity of major depression and level of associated functional impairment. Functional impairment in the workplace is generally reported to occur only at moderate to high levels of depression (11). Impairment is also positively associated with number of depressive symptoms, number of depressive episodes, and comorbidity with other psychiatric disorders (12). All three characteristics have been shown to index severity of familial risk for major depression (13, 14). The strong etiological relationship between major depression and associated functional impairment supports the increasing nosological focus on impairment. However, in our sample, 9% of the familial risk factors and 19% of the nonfamilial risk factors for associated functional impairment are estimated to be unrelated to the risk factors for major depression. Our estimate for nonfamilial risk factors incorporates errors of measurement; nevertheless, the presence of modest impairment-specific risk factors is consistent with other work that has shown that clinical severity is imperfectly correlated with functional impairment (12, 15, 16).
Conclusions
Introducing impairment as a criterion for the diagnosis of psychiatric disorders could have radically changed the epidemiology of psychiatric syndromes. However, in the case of lifetime major depression, associated functional impairment indexes both risk factors for major depression and, to a much lesser extent, risk factors specific to associated functional impairment. Our results therefore suggest that the addition of associated functional impairment as a criterion for the diagnosis of major depression will lower prevalence estimates and modestly change the pattern of risk factors associated with major depression. That is, major depression plus associated functional impairment is not entirely the same disorder as major depression without requirements for impairment.
Currently, we can only speculate about the source of risk factors specific for associated functional impairment, although we do know that they are in part familial. Work history, not depressive symptoms, was shown to be the best predictor of long-term occupational outcome among subjects with a history of depression (11). We predict that the risk factors specific to associated functional impairment will index personal characteristics (such as personality, coping skills, and perceived support) and contextual features (such as education, marital history, and socioeconomic status).
Limitations
The results of this study should be interpreted in light of four methodological considerations. First, our estimate of the prevalence of lifetime history of major depression is higher than the prevalence in the National Comorbidity Survey (17) but similar to or lower than the prevalence reported for other population-based studies (18). History of major depression in the Virginia Twin Study is assessed separately for the last year and the lifetime before the last year, and this protocol provides two “chances” for an individual to meet criteria for major depression. While the National Comorbidity Survey used lay interviewers and a highly structured psychiatric interview, an approach that may underestimate the population rates of illness (19), the Virginia Twin Study employed experienced clinicians and a semistructured interview. Like the National Comorbidity Survey, the Virginia Twin Study used methods to encourage “effortful responding.” Our subjects were somewhat younger than those assessed in the National Comorbidity Survey, which may also contribute to prevalence differences (20). Recent studies have suggested that lay interviewers using highly structured instruments may underestimate the rates of depressive illness in community samples compared to clinician assessments (21, 22). Second, lifetime history of major depression and associated functional impairment were assessed at one point in time, an approach that confounds effects of individual-specific environmental and measurement error. The correlation between the risk factors for major depression and associated functional impairment could therefore be underestimated because of errors in measuring major depression or associated functional impairment. Third, although we expect a continuous relationship between symptom profiles and symptom-related impairment, measurement of impairment is not feasible until some minimum symptom threshold has been reached. We overcame this coarsening of measurement by treating both the symptom and the impairment measures as categorical indicators of underlying continuous measures by using a threshold model (23). In this approach, the symptom-impairment relationship that is modeled is between the underlying continuous latent variables and is not directly between the observed categorical measures. One of the desirable consequences of this formulation is that refinement of the measures—for example, to assess the impairment associated with subdiagnostic symptoms—would be expected to increase the power of the study but would not be expected to lead to systematic changes in the parameters that describe the relationship between the latent trait dimensions. Fourth, our findings may not be replicated in clinical samples because of the biases associated with treatment seeking and variation in the impairment profile associated with depression in primary versus tertiary medical settings (24).
 |
 |
 |
Received Dec. 8, 2002; revision received April 8, 2003; accepted April 11, 2003. From the Virginia Institute for Psychiatric and Behavioral Genetics, Departments of Human Genetics and Psychiatry, Virginia Commonwealth University; and the School of Epidemiology and Health Science and the Centre for Census and Survey Research, University of Manchester, Manchester, U.K. Address reprint requests to Dr. Kendler, Department of Psychiatry, 800 East Leigh St., P.O. Box 980126, Richmond, VA 23298; [email protected] (e-mail). Supported by NIH grants MH-60324, MH-57761, MH-01458, MH-40828, MH-65322, MH/AA/DA-49492, and AA-09095. The authors thank Dr. Carol Prescott for her assistance with the data-collection phase of this project and the contribution of the Virginia Twin Registry, now part of the Mid-Atlantic Twin Registry, for the ascertainment of subjects for this study. The Twin Registry, directed by Dr. Linda Corey, receives support from NIH, the Carman Trust, and the W.M. Keck, John Templeton, and Robert Wood Johnson Foundations.
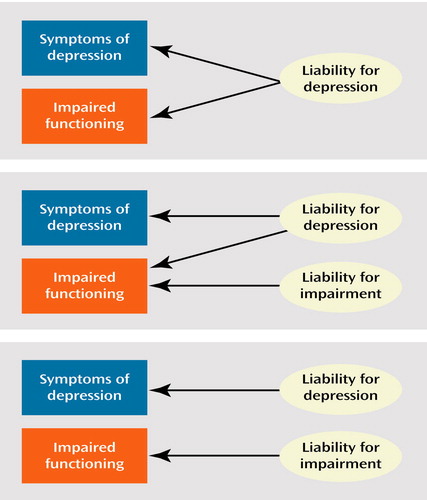
Figure 1. Etiological Schema of the Relationships Between Major Depression and Associated Impairmenta
aRisk factors pictured at the top are identical. Risk factors shown in the middle are partly the same and partly different. Risk factors at the bottom are different.
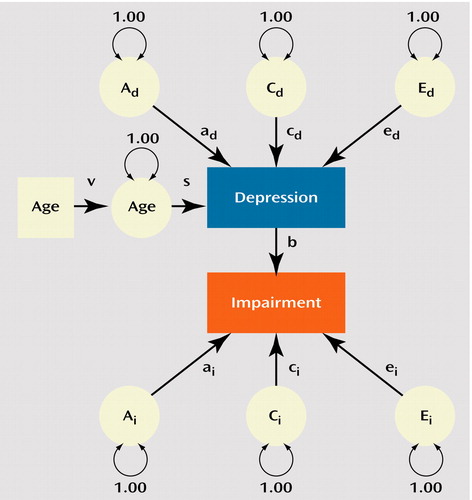
Figure 2. A Bivariate Twin Model for Depression and Associated Functional Impairment With Age in Twins From the Virginia Twin Registrya
aThe model begins with the risk factors for depression (subscript d), which are divided into additive genetic (Ad), common environmental (Cd), and individual-specific environmental (Ed) components. Individuals scoring above the threshold on this dimension are susceptible to the development of associated functional impairment. The vulnerability to impairment derives from two sources: 1) risk factors shared between depression and impairment, reflected in path b, and 2) risk factors for impairment that are unrelated to risk factors for depression. These are also subdivided into additive genetic (Ai), common environmental (Ci), and individual-specific environmental components (Ei), in which the subscript i indicates that they are specific for impairment. Path coefficients, indicated by lowercase letters (a, c, and e), reflect standardized partial regression coefficients. The proportion of variance in the dependent variables accounted for by the independent variable is equal to the square of the connecting path. Heritability of depression, for example, equals ad2. Observed variables are depicted in boxes and latent variables in circles. The model is constrained so that ad2+cd2+ed2=1.0 and b2+ai2+ci2+ei2=1.0. Furthermore, the total heritable influences on impairment can be subdivided into those that are shared with depression, which equal ad2×b2 and those that are specific to impairment ai2.
1. Wakefield JC, Spitzer RL: Lowered estimates—but of what? Arch Gen Psychiatry 2002; 59:129–130Crossref, Medline, Google Scholar
2. Narrow WE, Rae DS, Robins LN, Regier DA: Revised prevalence estimates of mental disorders in the United States: using a clinical significance criterion to reconcile 2 surveys’ estimates. Arch Gen Psychiatry 2002; 59:115–123Crossref, Medline, Google Scholar
3. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ: A population-based twin study of major depression in women: the impact of varying definitions of illness. Arch Gen Psychiatry 1992; 49:257–266Crossref, Medline, Google Scholar
4. Kendler KS, Gardner CO, Neale MC, Prescott CA: Genetic risk factors for major depression in men and women: similar or distinct heritabilities and same or partly distinct genes. Psychol Med 2001; 31:605–616Crossref, Medline, Google Scholar
5. Eaves LJ, Eysenck HJ, Martin NG: Genes, Culture and Personality: An Empirical Approach. London, Oxford University Press, 1989Google Scholar
6. Spence JE, Corey LA, Nance WE, Marazita ML, Kendler KS, Schieken RM: Molecular analysis of twin zygosity using VNTR DNA probes (abstract). Am J Hum Genet 1988; 43:A159Google Scholar
7. Spitzer RL, Williams JBW, Gibbon M: Structured Clinical Interview for DSM-III-R (SCID). New York, New York State Psychiatric Institute, Biometrics Research, 1987Google Scholar
8. Kendler KS, Neale MC, Sullivan P, Corey LA, Gardner CO, Prescott CA: A population-based twin study in women of smoking initiation and nicotine dependence. Psychol Med 1999; 29:299–308Crossref, Medline, Google Scholar
9. Neale MC, Cardon LR: Methodology for Genetic Studies of Twins and Families. Dordrecht, the Netherlands, Kluwer Academic, 1992, pp 211–223Google Scholar
10. Kendler KS, Gardner CO, Prescott CA: Corrections to 2 prior published articles. Arch Gen Psychiatry 2000; 57:94–95Crossref, Medline, Google Scholar
11. Mintz J, Mintz LI, Arruda MJ, Hwang SS: Treatments of depression and the functional capacity to work. Arch Gen Psychiatry 1992; 49:761–768Crossref, Medline, Google Scholar
12. Mojtabai R: Impairment in major depression: implications for diagnosis. Compr Psychiatry 2001; 42:206–212Crossref, Medline, Google Scholar
13. Kendler KS, Gardner CO, Prescott CA: Clinical characteristics of major depression that predict risk of depression in relatives. Arch Gen Psychiatry 1999; 56:322–327Crossref, Medline, Google Scholar
14. Foley DL, Neale MC, Kendler KS: Reliability of a lifetime history of major depression over 4 to 8 years: implications for heritability and comorbidity. Psychol Med 1998; 28:857–870Crossref, Medline, Google Scholar
15. Solomon A, Haaga DA, Arnow BA: Is clinical depression distinct from subthreshold depressive symptoms? a review of the continuity issue in depression research. J Nerv Ment Dis 2001; 189:498–506Crossref, Medline, Google Scholar
16. Pincus HA, Davis WW, McQueen LE: “Subthreshold” mental disorders: a review and synthesis of studies on minor depression and other “brand names.” Br J Psychiatry 1999; 174:288–296Crossref, Medline, Google Scholar
17. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8–19Crossref, Medline, Google Scholar
18. Rorsman B, Grasbeck A, Hagnell O, Lanke J, Ohman R, Ojesjo L, Otterbeck L: A prospective study of first-incidence depression: the Lundby study, 1957–1972. Br J Psychiatry 1990; 156:336–342Crossref, Medline, Google Scholar
19. Helzer JE, Robins LN, McEvoy LT, Spitznagel E: A comparison of clinical and Diagnostic Interview Schedule diagnoses. Arch Gen Psychiatry 1985; 42:657–666Crossref, Medline, Google Scholar
20. Klerman GL, Lavori PW, Rice J, Reich T, Endicott J, Andreasen NC, Keller MB, Hirschfeld RM: Birth cohort trends in rates of major depressive disorder among relatives of patients with affective disorder. Arch Gen Psychiatry 1985; 42:689–693Crossref, Medline, Google Scholar
21. Eaton WW, Neufeld K, Chen L-S, Cai G: A comparison of self-report and clinical diagnostic interviews for depression: Diagnostic Interview Schedule and Schedules for Clinical Assessment in Neuropsychiatry in the Baltimore Epidemiologic Catchment Area follow-up. Arch Gen Psychiatry 2000; 57:217–222Crossref, Medline, Google Scholar
22. Murphy JM, Monson RR, Laird NM, Sobol AM, Leighton AH: A comparison of diagnostic interviews for depression in the Stirling County Study. Arch Gen Psychiatry 2000; 57:230–236Crossref, Medline, Google Scholar
23. Falconer DS: Introduction to Quantitative Genetics, 3rd ed. New York, John Wiley & Sons, 1989Google Scholar
24. Wells KB, Burnam MA, Rogers W, Hays R, Camp P: The course of depression in adult outpatients: results from the Medical Outcomes Study. Arch Gen Psychiatry 1992; 49:788–794Crossref, Medline, Google Scholar



