Characteristics of Cocaine-Dependent Patients Who Attempt Suicide
Abstract
OBJECTIVE: Although suicidal behavior is frequent among cocaine-dependent patients, it has been little studied. Therefore, the author examined the characteristics of cocaine-dependent patients who had attempted suicide. METHOD: Cocaine-dependent patients who had attempted suicide (N=84) were compared with cocaine-dependent patients who had never attempted suicide (N=130) on clinical, personality, psychiatric, and physical variables. RESULTS: Significantly more of the patients who had attempted suicide were female and had a family history of suicidal behavior; they reported significantly more childhood trauma and were significantly more introverted, neurotic, and hostile. They had also had significantly more comorbidity with alcohol and/or opiate dependence, major depression, and physical disorders. CONCLUSIONS: The clinical implications are that family, childhood, personality, psychiatric, and physical risk factors contribute to suicidal behavior in cocaine-dependent patients. Comorbidity appears to be an important determinant of suicidal behavior.
Cocaine dependence is a major public health problem. Patients with cocaine dependence have a greater risk of suicidal behavior. For example, Marzuk et al. (1) found that 29% of suicide victims in New York aged 21–30 tested positive for cocaine. Data from 13,673 participants in the Epidemiologic Catchment Area survey in the United States showed that cocaine abusers had a significantly greater risk of attempting suicide (2). However, the characteristics of cocaine-dependent patients who attempt suicide have been little studied. Therefore, it was decided to compare cocaine-dependent patients who had attempted suicide with those who had never attempted suicide.
Increasingly, studies suggest that suicidal behavior is a multidetermined act involving psychosocial, family, genetic, personality, psychiatric, physical, and other risk factors that affect developmental processes across the lifespan (3, 4). Therefore, in the present study, it was decided to focus on four main areas across the lifespan: family history of suicide, childhood trauma, personality traits, and comorbidity.
Family history of suicide was examined, as this has been shown in other psychiatric diagnoses to predispose patients to a suicide attempt (5). Childhood trauma was examined, as recent studies have reported that abuse and neglect in childhood may predispose individuals to suicide attempts as adults (6–8). Personality was examined, as personality traits such as impulsivity, hostility, and introversion are associated with suicide attempts (4, 9). Comorbidity was examined, as other substance dependence, psychiatric, or physical disorder comorbidities have been shown to be important determinants of suicidal behavior (10–15). Whether there was comorbidity with major depression, opiate dependence, or physical disorders was examined, as these were significant comorbidities in a previous study of alcoholics who attempted suicide (16). In addition, whether there was comorbidity with alcohol dependence was examined.
The hypothesis that was tested was that cocaine-dependent patients who attempted suicide would have more family history of suicidal behavior, more childhood trauma, higher impulsivity, hostility, and introversion personality scores, and more comorbidity with opiate and/or alcohol dependence, major depression, and physical illness.
Method
A consecutive series of 214 cocaine-dependent patients who were admitted to the Substance Abuse Treatment Program at the Department of Veterans Affairs, New Jersey Healthcare System, East Orange Campus, was examined. Inclusion criteria were that the patients met DSM-IV criteria for cocaine dependence and identified cocaine as their illicit drug of first choice. Exclusion criteria were a lifetime history of schizophrenia or other psychosis or mental retardation.
A semistructured interview was conducted concerning the patient’s history of cocaine dependence, sociodemographic variables, any alcohol and/or opiate dependence, current treatment for a medical disorder, lifetime history of suicide attempts, and suicidal behavior in a first- or second-degree relative. A suicide attempt was defined as a self-destructive act with some intent to end one’s life that was not self-mutilatory in nature. The information from the patient was supplemented by collateral information from mental health program staff, medical records, and the program internist and physician’s assistant, and, where possible, from previous treating mental health professionals. The age at each attempt, the method used, and whether the attempt led to medical attention were also recorded. Excessive abuse of cocaine was not considered a suicide attempt.
The patients were also interviewed by a psychiatrist (A.R.) with the depression section of the Structured Clinical Interview for DSM-IV (SCID) (17) to determine whether there was a lifetime history of a major depressive episode meeting DSM-IV criteria. (The criteria for major depressive episode were conservatively used, as more depressive symptoms are required than in some other mood disorder diagnoses, i.e., cocaine-induced mood disorder or dysthymic disorder.) In addition, the patients were interviewed with the Addiction Severity Index (18) by an addiction counselor trained to administer the index. The Addiction Severity Index is an approximately 45-minute structured interview that provides information on alcohol, drug, psychiatric, medical, employment, legal, and family or social problem severities. Key items in each area are used to generate composite scores, which yield an assessment of overall problem severity in each area over the last 30 days. Composite scores range from 0.00 to 1.00, with higher scores indicating greater problem severity. The validity and reliability of the Addiction Severity Index have been shown to be high (reviewed in reference 18).
The patients completed four questionnaires: the Eysenck Personality Questionnaire (19), which yields neuroticism, extraversion, psychoticism, and lie-telling scores; the Foulds Hostility and Direction of Hostility Questionnaire (20), which yields a total hostility score; the Barratt Impulsivity Scale—7B Version (21), which yields scores for sensory stimulation, motor impulsivity, interpersonal impulsivity, cognitive impulsivity, and risk taking; and the Childhood Trauma Questionnaire (22, 23), the 34-item version, which yields scores for emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect and a weighted total score. After complete description of the study to the subjects, written informed consent was obtained. Not all patients completed all measures.
In the statistical analysis, Student’s t and chi-square tests were used. As many statistical tests were performed, a significance criteria of p<0.01 was used to reduce the probability of making a type I error. Odds ratios and 95% confidence intervals (CIs) were also calculated. To examine the strength of the relationships between suicide attempt and various risk factors, multivariate analysis was used. The putative risk factor was the independent variable, and suicide attempt was the dependent variable.
Results
Eighty-four of the 214 cocaine-dependent patients had attempted suicide at some time. These 84 patients had made a total of 175 suicide attempts (mean=2.1 attempts, range=1–9). Significantly more of the 84 cocaine-dependent patients who had attempted suicide were female (N=15) than of the 130 cocaine-dependent patients who had never attempted suicide (N=5) (χ2=10.23, df=1, p<0.001; odds ratio=5.55, 95% CI=2.01–16.40). The mean age of the cocaine-dependent patients who had attempted suicide was 40.8 years (SD=8.0), and their mean age at onset of cocaine abuse was 26.9 years (SD=9.1), compared with a mean=41.4 years (SD=7.3) and a mean=27.7 years (SD=8.6) for the cocaine-dependent patients who had never attempted suicide (n.s.). Fifty-seven of the 84 cocaine-dependent patients who had attempted suicide were African American, seven were Hispanic, and 20 were Caucasian, compared with 98, six, and 26, respectively, among the 130 cocaine-dependent patients who had never attempted suicide (n.s.). Six of the 84 patients who had attempted suicide were married, 29 were single, and 49 were separated, divorced, or widowed, compared with 15, 53, and 62, respectively, among the 130 patients who had never attempted suicide (n.s.).
Twenty-one of the 84 patients who had attempted suicide (25.0%) had a family history of suicidal behavior, compared with seven of the 130 patients who had never attempted suicide (5.4%) (χ2=15.58, df=1, p<0.0001; odds ratio=5.88, 95% CI=2.38–14.44). Fifteen of the 84 patients who had attempted suicide had a first- or second-degree relative who had attempted suicide, and six had a first- or second-degree relative who had committed suicide, compared with six and one, respectively, of the 130 patients who had never attempted suicide (χ2=8.67, df=1, p<0.003; odds ratio=4.49, 95% CI=1.66–12.08, and χ2=4.69, df=1, n.s., respectively).
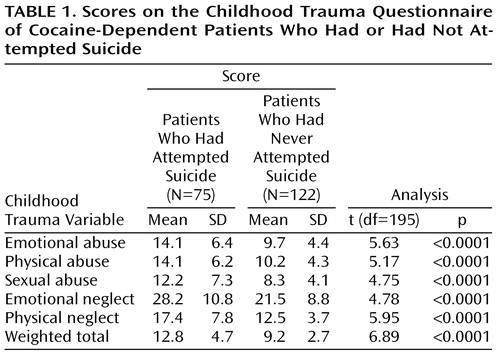
The cocaine-dependent patients who had attempted suicide had significantly higher childhood trauma scores for emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect than the cocaine-dependent patients who had never attempted suicide (Table 1). Multivariate analysis showed that physical neglect was significantly and independently associated with a suicide attempt (p<0.04).
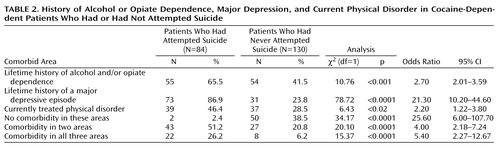
Forty-nine of the 84 patients who had attempted suicide (58.3%) had a lifetime history of alcohol dependence, compared with 45 of the 130 patients who had never attempted suicide (34.6%) (χ2=10.71, df=1, p<0.001; odds ratio=2.64, 95% CI=1.50–4.63). Sixteen of the 84 patients who had attempted suicide (19.0%) had a lifetime history of opiate dependence, compared with 12 of the 130 patients who had never attempted suicide (9.2%) (χ2=3.50, df=1, n.s.). Significantly more patients who had attempted suicide had a lifetime history of alcohol and/or opiate dependence, major depression, and a currently treated physical disorder (Table 2). The patients who had attempted suicide also had significantly higher psychiatry composite scores on the Addiction Severity Index (mean=0.42, SD=0.24) than the patients who had never attempted suicide (mean=0.23, SD=0.22) (t=3.88, df=153, p<0.0002).
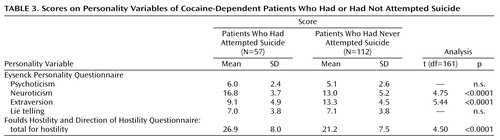
The patients who had attempted suicide had significantly lower extraversion and higher neuroticism scores on the Eysenck Personality Questionnaire. Multivariate analysis showed that both introversion and neuroticism were significantly and independently associated with a suicide attempt (p<0.0001 and p<0.0006, respectively). The patients who had attempted suicide also had significantly higher hostility scores on the Foulds Hostility and Direction of Hostility Questionnaire (Table 3). The suicide attempters did not score significantly higher on any of the subscales of the Barratt Impulsivity Scale (data not shown).
Discussion
Thirty-nine percent of the cocaine-dependent patients in the present study had attempted suicide at some time. Although this high percentage partly reflects the fact that this was a treatment-seeking group, it also reflects that cocaine dependence is a disorder associated with a greater risk of suicidal behavior. The study aimed to identify some of the characteristics of the cocaine-dependent patients who had attempted suicide. It was found, as hypothesized, that more had a family history of suicidal behavior; they reported significantly more childhood trauma; they had higher personality scores for introversion, neuroticism, and hostility; and they had experienced significantly more comorbidity with other substance dependence and psychiatric and physical disorders.
Although comorbidity is high among cocaine-dependent patients in general, a striking finding of the present study is the amount of comorbidity among the patients who had attempted suicide (24, 25). Significantly more had a lifetime history of alcohol dependence, and almost two-thirds had a lifetime history of either alcohol or opiate dependence. The suicide attempters had significantly higher psychiatry composite scores on the Addiction Severity Index; significantly more had a lifetime history of a major depressive episode, and most of these patients had received antidepressant medication. Significantly more of the patients who had attempted suicide (N=39, 46.4%) had a currently treated physical disorder than those who had not attempted suicide (N=37, 28.5%). Although the focus was restricted to the three comorbidities of alcohol and/or opiate dependence, major depression, or current physical disorder, only two (2.4%) of the patients who had attempted suicide did not have any of these three comorbidities, compared with 50 (38.5%) of the patients who had never attempted suicide. Conversely, comorbidity in two or three of these three areas was found in significantly more of the patients who had attempted suicide, with over a quarter of them having comorbidity in all three areas.
Significantly more of the cocaine-dependent patients who had attempted suicide had a family history of suicidal behavior. Such a family history has been shown in other diagnostic groups to be associated with suicide attempts (5). This result in the present study suggests that a family history of suicidal behavior in a cocaine-dependent patient may indicate that the patient has a greater risk for suicidal behavior. There were also highly significant differences between the two groups for childhood trauma. Cocaine-dependent patients who had attempted suicide had significantly higher scores for childhood emotional abuse, physical abuse, and sexual abuse, as well as higher scores for emotional neglect and physical neglect. These data are similar to the greater childhood trauma scores obtained among suicidal patients in other diagnostic groups and suggest that both childhood abuse and neglect may predispose a cocaine-dependent adult to exhibit suicidal behavior.
The personality findings of the present study are of interest. Cocaine-dependent patients who had attempted suicide had significantly lower scores on the Eysenck Personality Questionnaire for extraversion; i.e., they were more introverted. This introversion finding is consistent with a large literature reporting that suicide attempters are more introverted than nonattempters (reviewed in reference 13). The great majority of the cocaine-dependent patients were euthymic when they completed the Eysenck Personality Questionnaire, and it is noteworthy that Kendler et al. (26) showed, using the Eysenck Personality Questionnaire, that “neither the state of being depressed nor the scar of previous episodes of major depression significantly altered levels of extraversion.” We reported similarly in a study of depressed patients (9). That cocaine-dependent patients who had attempted suicide were more introverted is of interest, as extraversion has been shown to predict levels of social support (27, 28), and lack of social support may be particularly important when a cocaine-dependent individual is additionally suffering with major depression or another comorbidity.
The patients who had attempted suicide also had significantly higher Eysenck Personality Questionnaire scores for neuroticism. This is of interest, as a recent 21-year longitudinal birth cohort study of New Zealand children (29) showed that those who had attempted suicide by 21 years had significantly higher Eysenck neuroticism scores at age 14. These authors noted that previous studies had shown a link between neuroticism and suicide attempts. This group’s analysis of their prospective data suggested that the linkage between neuroticism scores in childhood and later suicide attempts was due to the fact that early neuroticism was related to later psychiatric disorder, particularly depression, which in turn was associated with suicidal behavior.
The patients who had attempted suicide in the present study did not score significantly higher on any of the five subscale scores of the version of the Barratt Impulsivity Scale that we used. However, the patients who had attempted suicide did score significantly higher for hostility on the Foulds Hostility and Direction of Hostility Questionnaire. Others have reported high hostility scores in patients who exhibited suicidal behavior (reviewed in reference 4).
The definition of a suicide attempt used in the present study did not require that the attempt lead to medical evaluation. This was deliberate because many cocaine-dependent patients who have suicidal intent and attempt suicide do not seek medical attention and/or are unable to gain access to health care. In fact, 37 of the 175 attempts made by the patients in the present study were self-destructive with intent to die and were assessed as suicide attempts, but they did not lead to contact with medical services. These 37 attempts were made by 31 patients, 14 of whom also made other suicide attempts that did lead to contact with medical services. A limitation imposed by the length of the two semistructured clinical and Addiction Severity Index interviews was that time permitted only the major depression section of the SCID to be used. Future studies using the complete SCID interview might yield further information about other axis I and II comorbidities. Future studies might also examine the degree of suicidal intent and medical lethality.
In summary, the clinical implications are that risk factors across the life cycle were associated with suicidal behavior in cocaine-dependent patients. Distal risk factors included a family history of suicide, childhood trauma, and neuroticism, hostility, and introversion. More proximal risk factors included the comorbidities of other substance dependence, major depression, and physical disorders. These results suggest a threshold-trigger model of suicidal behavior in cocaine-dependent patients with distal threshold-affecting factors, including family, childhood, and personality variables. Such individuals at a greater risk for suicide may have suicidal behavior triggered when they experience the problems associated with cocaine dependence, particularly when exposed to other triggering factors, such as comorbidity or other stresses.
 |
 |
 |
Received May 3, 2000; revisions received Sept. 26, 2000, and Jan. 12, 2001; accepted Feb. 1, 2001. From the Psychiatry Service, Department of Veterans Affairs, New Jersey Healthcare System. Address reprint requests to Dr. Roy, Psychiatry Service 116A, Department of Veterans Affairs, New Jersey Healthcare System, 385 Tremont Ave., East Orange, NJ 07018. Funded by grant DA-10336 from the National Institute on Drug Abuse.
1. Marzuk PM, Tardiff K, Leon AC, Stajic M, Morgan EB, Mann JJ: Prevalence of cocaine use among residents of New York City who committed suicide during a one-year period. Am J Psychiatry 1992; 149:371-375Link, Google Scholar
2. Petronis K, Samuels J, Moscicki E, Anthony J: An epidemiologic investigation of potential risk factors for suicide attempts. Soc Psychiatry Psychiatr Epidemiol 1990; 25:193-199Medline, Google Scholar
3. Beautrais AL, Joyce PR, Mulder RT, Fergusson DM, Deavoll BJ, Nightingdale SK: Prevalence and comorbidity of mental disorders in persons making serious suicide attempts: a case-controlled study. Am J Psychiatry 1996; 153:1009-1014Google Scholar
4. Nordstrom P, Shalling D, Asberg M: Temperamental vulnerability in attempted suicide. Acta Psychiatr Scand 1995; 92:155-160Crossref, Medline, Google Scholar
5. Roy A: Family history of suicide. Arch Gen Psychiatry 1983; 40:971-974Crossref, Medline, Google Scholar
6. Mullen P, Martin J, Anderson J, Romans S, Herbison P: Childhood sexual abuse and mental health in adult life. Br J Psychiatry 1993; 163:721-732Crossref, Medline, Google Scholar
7. Davidson J, Hughes D, George L, Blazer D: The association of sexual assault and attempted suicide within the community. Arch Gen Psychiatry 1996; 53:550-555Crossref, Medline, Google Scholar
8. Lipschitz D, Winegar R, Nicolaou A, Hartnick E, Wolfson M, Southwick S: Perceived abuse and neglect as risk factors for suicidal behavior in adolescent inpatients. J Nerv Ment Dis 1999; 187:32-39Crossref, Medline, Google Scholar
9. Roy A: Is introversion a risk factor for suicidal behavior in depression. Psychol Med 1998; 28:1457-1461Google Scholar
10. Rudd MD, Dahm PF, Rajab MH: Diagnostic comorbidity in persons with suicidal ideation and behavior. Am J Psychiatry 1993; 150:928-934Link, Google Scholar
11. Bronisch T, Wittchen H: Suicidal ideation and suicide attempts: comorbidity with depression, anxiety disorders, and substance abuse disorder. Eur Arch Psychiatry Clin Neurosci 1994; 244:93-98Crossref, Medline, Google Scholar
12. Conwell Y, Duberstein PR, Cox C, Herrman JH, Forbes NT, Caine ED: Relationship of age and axis I diagnoses in victims of completed suicide: a psychological autopsy study. Am J Psychiatry 1996; 153:1001-1008Google Scholar
13. Suominen K, Henriksson M, Suokas J, Isometsä E, Ostamo A, Lönnqvist J: Mental disorders and comorbidity in attempted suicide. Acta Psychiatr Scand 1996; 94:234-240Crossref, Medline, Google Scholar
14. Wonderlich U, Bronisch T, Wittchen H: Comorbidity patterns in adolescents and young adults with suicide attempts. Eur Arch Psychiatry Clin Neurosci 1998; 248:87-95Crossref, Medline, Google Scholar
15. Kessler RC, Borges G, Walters EE: Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry 1999; 56:617-626Crossref, Medline, Google Scholar
16. Roy A, Lamparski D, DeJong J, Moore V, Linnoila M: Characteristics of alcoholics who attempt suicide. Am J Psychiatry 1990; 147:761-765Link, Google Scholar
17. Spitzer RL, Williams JBW, Gibbon M: Structured Clinical Interview for DSM-IV (SCID). New York, New York State Psychiatric Institute, Biometrics Research, 1995Google Scholar
18. McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati H, Argeriou M: The Fifth Edition of the Addiction Severity Index. J Subst Abuse Treat 1992; 9:199-213Crossref, Medline, Google Scholar
19. Eysenck HJ, Eysenck SBG: Eysenck Personality Questionnaire Manual. London, Hodder and Stoughton, 1975Google Scholar
20. Foulds G: Personality and Personal Illness. London, Tavistock, 1965Google Scholar
21. Barratt E: Impulsivity: integrating cognitive, behavioral, biological and environmental data, in The Impulsive Client: Theory, Research, and Treatment. Edited by McCowan W, Shure M. Washington, DC, American Psychiatric Press, 1993, pp 39-119Google Scholar
22. Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, Sapareto E, Ruggiero J: Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry 1994; 151:1132-1136Google Scholar
23. Bernstein D, Ahluvalia T, Pogge D, Handelsman L: Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. J Am Acad Child Adolesc Psychiatry 1997; 36:340-348Crossref, Medline, Google Scholar
24. Rounsaville BJ, Anton SF, Carroll K, Budde D, Prusoff BA, Gawin F: Psychiatric diagnoses of treatment-seeking cocaine abusers. Arch Gen Psychiatry 1991; 48:43-51Crossref, Medline, Google Scholar
25. Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK: Comorbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area (ECA) Study. JAMA 1990; 264:2511-2518Google Scholar
26. Kendler K, Neale M, Kessler R, Heath A, Eaves L: A longitudinal twin study of personality and major depression in women. Arch Gen Psychiatry 1993; 50:853-862Crossref, Medline, Google Scholar
27. Furukawa T, Shibayama T: Intra-individual versus extra-individual components of social support. Psychol Med 1997; 27:1183-1191Google Scholar
28. Kendler KS: Social support: a genetic-epidemiologic analysis. Am J Psychiatry 1997; 154:1398-1404Google Scholar
29. Fergusson D, Woodward L, Horwood L: Risk factors and life processes associated with the onset of suicidal behaviour during adolescence and early adulthood. Psychol Med 2000; 30:23-39Crossref, Medline, Google Scholar



