Ethnic and Sex Differences in Suicide Rates Relative to Major Depression in the United States
Abstract
OBJECTIVE: Suicide rates differ between ethnic groups in the United States. Since suicide is commonly associated with a mood disorder, the authors compared suicide rates relative to depression rates in five ethnic groups in the United States. METHOD: Rates of major depression were generated from the Epidemiologic Catchment Area study and the Hispanic Health and Nutrition Epidemiologic Survey. Sociodemographic effects were determined by examining depression rates for respondents who were separated or divorced, earning low incomes, or not working for pay. The survey data were analyzed with age and sex standardization to generate 1-year prevalence rates of major depression. The depression rates of the different ethnic groups were compared and were examined in relation to suicide rates. RESULTS: The 1-year prevalence rates of major depression were 3.6% for whites, 3.5% for blacks, 2.8% for Mexican Americans, 2.5% for Cuban Americans, and 6.9% for Puerto Ricans. Compared to the rate for whites, the rate of depression was significantly higher in Puerto Ricans and significantly lower in Mexican Americans. Relative to the depression rates, the annual suicide rates were higher for males than for females. Mexican American and Puerto Rican males had lower relative suicide rates than white males. CONCLUSIONS: Identifying reasons for differences in suicide rates relative to depression among ethnic groups and between males and females may suggest interventions to reduce suicide rates. Some possibilities are that depression differs in form or severity or that unidentified factors protect against suicide in different subgroups.
Major depression has a 17% lifetime prevalence in the U.S. general population (1), yet rates of major depression differ among ethnic groups (1–6). Suicide is the eighth leading cause of death in the United States (7), and most suicide victims suffer from major depression around the time of death (8–10). Thus, rates of major depression are related to suicide rates (11, 12). However, estimates of suicide rates in people with affective disorders range from 9% to 60% (13). Although differences in methods of identifying major depression in suicide victims and differences in access to treatment by different subject groups may contribute to this discrepancy, other factors may be relevant, such as differences between the sexes or among ethnic groups in suicide rates relative to depression rates. We know of no published reports of studies comparing the 1-year prevalence of major depression among whites, blacks, Mexican Americans, Cuban Americans, and Puerto Ricans in the United States. Furthermore, to our knowledge there have been no studies of suicide rates relative to major depression rates in these ethnic groups. If differences exist, the reasons for the differences may suggest strategies for reducing suicide rates. We decided to determine whether the 1-year prevalence of major depression varies across five major ethnic groups in the United States, whether the suicide rate relative to depression varies among ethnic groups, and whether three sociodemographic factors—disrupted marital status, low income, and not working for pay (14, 15)—explain the results.
Method
Data Sources
The data were gathered in the Epidemiologic Catchment Area (ECA) study (1980–1984) (16) and the Hispanic Health and Nutrition Epidemiologic Survey (1982–1984) (3) and have been previously reported (3–5). Both surveys used the National Institute of Mental Health Diagnostic Interview Schedule (DIS) (17) to establish DSM-III diagnoses. We used the 1-year prevalence rates of major depression for blacks, whites, and Los Angeles Hispanics for persons aged 20 to 74 years from the ECA study, which was conducted in five sites in the United States. That study used a two-stage, stratified, clustered sample of respondents both in the community and in institutions. Only community rates are reported here. We also used depression rates for Puerto Ricans in mainland United States, Mexican Americans, and Cuban Americans from the Hispanic Health and Nutrition Epidemiologic Survey data, conducted by the National Center for Health Statistics. This study surveyed the three largest Hispanic groups in the geographic areas in which they were most concentrated. The Hispanic Health and Nutrition Epidemiologic Survey used a complex, multistage, stratified, clustered sample of respondents aged 6 months to 74 years (only subjects aged 20 to 74 years were included in this analysis).
The responses to the DIS were subjected to a computer algorithm that generated DSM-III diagnoses for major depression in the last year. Subjects were categorized as depressed if they gave affirmative responses to questions about the presence of current major depression (excluding bereavement) or responded that an episode of major depression had ended within the last year.
We used the U.S. suicide rates reported by Desenclos and Hahn (18), which are based on the Centers for Disease Control National Center for Health Statistics Mortality Detail Data Tapes 1986–1988. This time period is near the periods covered by the depression data but does not overlap them. Age-adjusted death rates per 100,000 person years (all ages) were calculated on the basis of the 1980 census and 1987 postcensus age- and sex-specific population estimates. Eighteen states and the District of Columbia report mortality by Hispanic origin. National population estimates for Hispanics, non-Hispanic whites, and non-Hispanic blacks were extrapolated from these geographic areas by taking into account the proportion of the U.S. total that these areas represented for non-Hispanic blacks and whites, Hispanics, and specific Hispanic subgroups.
Statistical Analysis
The 1-year prevalence rates of major depression for each subgroup were standardized to the sex and age distribution of the 1987 midyear population of persons of Hispanic origin in the United States (19). We standardized the rates to the age and sex distribution of the 1987 midyear Hispanic population so that we could compare the 1-year prevalence rates of major depression across ethnic groups in relation to the suicide rates for these groups, which were based on 1987 U.S. population estimates. Standardization was done according to the methods of Breslow and Day (20). Weights were calculated in accordance with the methods of Pothoff et al. (21). The rates and proportions were calculated to provide estimates as though the ECA study and Hispanic Health and Nutrition Epidemiologic Survey had the same age and sex distributions as the 1987 midyear Hispanic population. Standard errors were derived as described by Fleiss (22). All analyses were done by using the frequency procedure (PROC FREQ) in SAS version 6.09 (SAS Institute, Cary, N.C.) (23). We compared 1-year depression rates across ethnic groups by using an overall chi-square test (24). Then we compared the rate for whites with the rate for each of the other ethnic groups, using the chi-square test. We also compared differences between the rates of depression in women and men in the five ethnic groups by using the Breslow-Day test for homogeneity of ratios (20).
The annual suicide rates (reported per 100,000 persons) were divided by 1,000 to represent suicides per 100 persons in each group. This rate was then divided by the annual prevalence rate of depression per 100 persons in each group. This provides an estimate of the number of suicides per year per case of major depression per year in each group.
To determine whether effects of sociodemographic variables on differences in depression rates among ethnic groups might account for differences in suicide, we calculated the rates of major depression for subjects with three sociodemographic characteristics considered to be risk factors for suicide: low income, not working for pay, and disrupted marital status. A logistic regression analysis (25) was conducted to examine the effects of these three sociodemographic variables on the depression rate for each ethnic group.
Results
Table 1 shows the 1-year prevalence rates for major depression across the different ethnic groups in the United States. We included the ECA Los Angeles site’s Hispanic group because most of those subjects were Mexican American (26). This group could thus serve as a comparison group for the Mexican American population studied in the Hispanic Health and Nutrition Epidemiologic Survey, a sample drawn from the Southwest, including California. The 95% confidence intervals (CIs) for these two populations overlap, with a wider CI for the smaller (Los Angeles) sample. The similar results support comparison of the results of these two surveys. Although the differences in rates of major depression for Mexican American men and Los Angeles Hispanic men in the three groups with specific sociodemographic characteristics (data to be presented later) may indicate that the results of the two surveys are not completely comparable, the CIs for separated and divorced men mostly overlapped, and those for men with low incomes and not working for pay completely overlapped, findings that also support the comparability of the survey results.
The rates of depression among the five ethnic groups were different overall. The 1-year prevalence rate of major depression was lower for Mexican Americans than for whites. In contrast, Puerto Ricans had a higher rate of major depression than did whites.
Among men, the depression rates across ethnic groups were different. Mexican American men had a lower rate of major depression than did whites, whereas Puerto Rican men had a higher rate than whites (Table 1). Like their male counterparts, Puerto Rican women had a higher rate of depression than did whites in the same gender group. However, Mexican American women did not have a significantly lower rate of depression than white women.
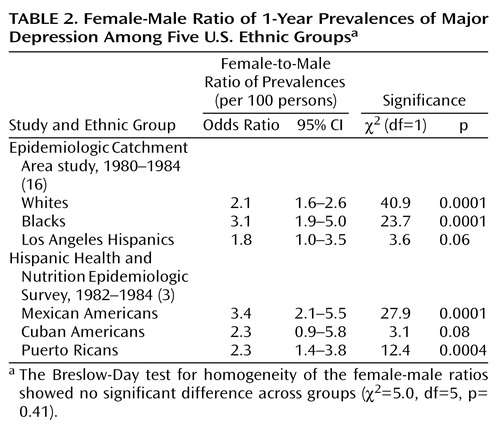
We also compared the depression rates of women and men in the five groups. Consistently, the rates of women were about twice those of men (Table 2).
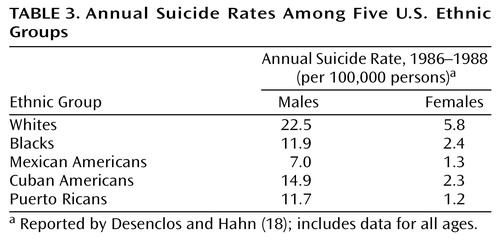
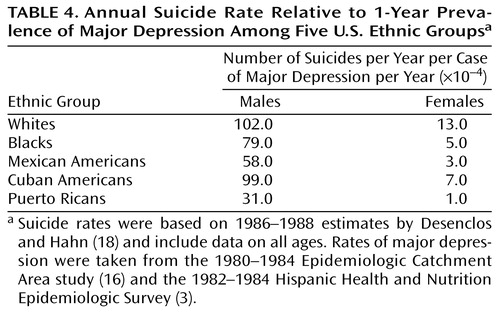
The suicide rates were higher in males than in females among all groups (Table 3). White males and females had the highest suicide rates relative to depression rates (Table 4). Mexican American and Puerto Rican males appeared to be better protected from suicide relative to 1-year prevalence of major depression than were the other groups (Table 4).
Among the females, blacks and Cuban Americans had a relative suicide rate, that is, in relation to the rate of major depression, that was about one-half that of whites. Mexican American and Puerto Rican females had the lowest relative suicide rates, about one-quarter and less than one-tenth that of white females, respectively (Table 4).
To determine whether the differences in suicide rates relative to the number of cases of major depression were due to variations in the rates of major depression associated with sociodemographic factors, we examined major depression rates for groups with sociodemographic characteristics that may confer risk for suicide (Table 5 and Table 6).
Among men (Table 5), only Puerto Ricans had a significantly higher depression rate, relative to that of white men, if they belonged to the “at risk” sociodemographic group with low incomes (odds ratio=3.99, 95% CI=1.28–12.39, χ2=5.71, df=1, p<0.02). The rate was not higher for Puerto Rican men with disrupted marital status (odds ratio=2.55, 95% CI=0.68–9.56, χ2=1.93, df=1, p<0.17) or those not working for pay (odds ratio=0.65, 95% CI=0.21–1.98, χ2=0.57, df=1, p<0.45).
Puerto Rican women (Table 6) also were at higher risk for depression, relative to white women, if they were in the group with low income (odds ratio=2.16, 95% CI=1.24–3.77, χ2=7.40, df=1, p<0.007) but not if they had disrupted marital status (odds ratio=1.42, 95% CI=0.82–2.48, χ2=1.55, df=1, p<0.22) or were not working for pay (odds ratio=0.84, 95% CI=0.46–1.56, χ2=0.31, df=1, p<0.58).
In general, the differences in suicide rates (Table 3) did not parallel the differences in 1-year prevalence rates of major depression among the subjects in the three groups with sociodemographic characteristics associated with suicide risk (Table 5 and Table 6). For example, the depression rates among the men in the three sociodemographic groups were not different from the rates for their ethnic groups as a whole, except for Puerto Rican men, who showed a higher depression rate if they had low income. However, the Puerto Rican males had the lowest suicide rate relative to the rate of major depression, suggesting that their higher risk for depression when they are impoverished does not translate to more frequent suicide. The finding was similar among females.
Discussion
We found that the relationship between the 1-year prevalence of major depression and the annual suicide rate varied among five ethnic groups and by gender. Puerto Ricans as a whole and by gender had higher depression rates than whites. Mexican Americans as a whole and men, but not women, had significantly lower rates of depression than whites. Males of all ethnic groups had suicide rates relative to major depression that were an order of magnitude higher than those of the females from the corresponding ethnic group. Among males, whites, Cuban Americans, and blacks had the highest suicide rates relative to the rates of major depression. Puerto Rican males appeared to be relatively protected. Among females, whites had the highest relative suicide rate and Mexican American and Puerto Rican females had the lowest rates.
Prevalence of Depression in Five Ethnic Groups
Although Mexican Americans had a modestly lower 1-year prevalence of depression than whites, Cuban Americans, blacks, and whites had similar, although not identical, rates. In contrast, the 1-year prevalence of major depression for Puerto Ricans in the United States was about double that for whites. Potter et al. (5) suggested that since the rates of major depression in Puerto Rico have been shown to be the same as in the general U.S. population (27), perhaps the migratory process selectively involves Puerto Ricans with higher levels of psychological distress. Alternatively, Vera et al. (28) reported that Puerto Ricans in the New York area, most of whom are impoverished, have the same depression rate as impoverished Puerto Ricans on the island. This is supported by our finding that Puerto Ricans with incomes of less than $5,000 per year had significantly higher depression rates than their counterparts. We also found that Puerto Ricans as a whole had a higher depression rate than whites. It has been suggested that Puerto Ricans in New York have a different response style, leading them to report more symptoms (29). It is unclear why island Puerto Ricans as a whole would not show this tendency when asked about psychiatric symptoms (27). Furthermore, that impoverished Puerto Ricans both in New York and in Puerto Rico would show similar rates of major depression (28) that differ from the rate for the general population of Puerto Rico (27) suggests that differences in depression rates between New York Puerto Ricans and whites or other Hispanic groups are related to issues other than national origin or identification, possibly socioeconomic.
Relation of Depression and Suicide Rates
Studies from a number of countries have indicated mood disorders in approximately 60% of suicide victims: Finland, 59% (10); Hungary, 58% (30); Australia, 55% (31); England, 70% (32); Sweden, 59% (33). These studies have been conducted in largely white populations. However, the apparent stability of the percentage of suicide victims with mood disorders before death is striking, suggesting a close relationship between depression rates and suicide rates. Consideration of ethnicity and gender demonstrates a more complex picture.
The difference in the relationship between suicide rate and 1-year prevalence of major depression among ethnic groups in the United States is remarkable. Possible explanations include comorbid conditions associated with higher suicide rates, such as substance abuse, alcoholism, or borderline personality disorder, cultural and child-rearing environments, adequacy of antidepressant treatment, genetics, and neurobiology. For these groups, there are few data about comorbidity or other factors, such as history of physical abuse, that have significant influences on suicidal behavior in the context of major depression (14).
We found that Mexican Americans and Puerto Ricans of both genders and Cuban American females had lower suicide rates than expected given their depression rates. Black females also seemed to have a lower suicide rate given their depression rate, although the same was not true for black males. The finding that the suicide rate was almost as high for black males as for white males, proportional to their depression rates, was unexpected. Moreover, a study showing a lower suicide rate among blacks did not account for the rate of major depression (34). Explanations offered included the role of black churches, a bias in reporting, differences in social integration, and differences in emotional expressiveness (34, 35). Our results suggest that protective factors may be restricted to black females only. Further study is needed to identify these protective factors.
Our finding that, compared to non-Hispanic whites, Puerto Ricans and Mexican Americans of both genders and Cuban American females, but not Cuban American males, have a lower suicide rate relative to the rate of major depression is also unexplained. Cuban Americans, Puerto Ricans, Mexican Americans, blacks, and non-Hispanic whites are different ethnically. Cuban Americans are more frequently white, whereas Mexican Americans and Puerto Ricans tend to be mixed racially, with Puerto Ricans having a significant black contribution and Mexican Americans having a significant indigenous contribution. Moreover, cultural differences among these groups should not be underestimated. The same historical and geographic factors that contribute to differences in racial composition also contribute to cultural heterogeneity. In addition, reasons for immigration differ because of historical and political circumstances. For example, many Cuban Americans have immigrated to the United States for political rather than economic reasons. Differences in suicide rates relative to major depression warrant study so that factors that protect against suicide in major depression may be uncovered.
Reported suicide rates are lower in Cuba, Puerto Rico, and Mexico than in the United States (36). Furthermore, the suicide rate for Hispanics in the United States is almost one-half that for non-Hispanic whites (18, 37, 38). Although the relationship between suicide rate and major depression has not been addressed in these studies, Hoppe and Martin (37) offered the concepts of familism and fatalism as contributors to lower suicide rates among Hispanics. Familism, an emphasis on close relationships with extended kinship, may offer protection against stress. Fatalism, the expectation of adversity, may be an adaptive stance in the setting of chronic stress. Both may serve to lower suicide risk in the context of depression.
Relation of Sociodemographic Variables to Depression and Suicide
Variables linked to suicide include unemployment (15), marital isolation (14), and socioeconomic status (14). In our study, the differences in the rates of major depression among members of the five ethnic groups in those socioeconomic categories did not follow the pattern for suicide rates. In fact, the rate of major depression appeared to be influenced by low income only among Puerto Rican men and women. Yet Puerto Ricans were among the most protected from suicide given their high depression rate.
Methodologic Limitations
One of the study’s limitations is that the data about depression come from two surveys. Apart from specific differences in sampling techniques, the ECA study’s main purpose was to assess the prevalence of psychiatric disorders in five sites in the United States, by constructing samples similar to the U.S. population as a whole. The ECA study did not distinguish among Hispanic subgroups. The Hispanic Health and Nutrition Epidemiologic Survey, in contrast, sought information regarding health and nutrition, including but not restricted to psychiatric disorders. This survey targeted three Hispanic subgroups. However, between one-third and one-half of the respondents in the Hispanic Health and Nutrition Epidemiologic Survey did not receive the depression assessment. Alcohol use was the only other psychiatric variable that was assessed systematically. Also, this survey did not cover undocumented immigrants. In addition, both the ECA study and the Hispanic Health and Nutrition Epidemiologic Survey used the DIS administered by lay interviewers, the results of which have been shown to differ from results when clinicians interview the same subjects only a few weeks later (23).
Also, depression is only one factor leading to suicide. This study did not address substance abuse, schizophrenia, and psychosocial determinants. Also, there are no data with which to investigate factors such as familism or the role of religion in lowering suicide rates relative to depression across ethnic groups.
Another limitation is the assessment of suicide rates. Because only some states in the United States report mortality by Hispanic origin, the suicide rate for each Hispanic subgroup was extrapolated from the rates for states that do report whether or not the decedent was Hispanic. Furthermore, suicide rates may be obscured by accidents or violence. In addition, the suicide rates were from 1986 to 1988. The ECA data were collected between 1980 and 1984, and the Hispanic Health and Nutrition Epidemiologic Survey data were collected between 1982 and 1984. Thus, the 1-year prevalence rates of depression are from 3 to 7 years before the years for which suicide rates are reported. The depression rates for both samples were adjusted to the postcensus estimates for the population for 1987 to address this issue. However, considerations such as the economic environment, which changed over the course of the decade, and its possible differential effects on suicide rates and prevalence of depression could not be addressed. In addition, the suicide rates reported cover ages under 20 and over 74, which are not covered in the reports of depression prevalence.
A further limitation is the use of a general categorization for whites and blacks. Blacks and whites in the United States are of heterogeneous cultural backgrounds and countries of origin. Depression rates that appear similar for Hispanics when taken together, but not when Hispanics are considered as subgroups, might also vary if blacks or whites were to be considered as subgroups categorized by country of origin.
Summary
Mexican Americans and Puerto Ricans as a whole, and black and Cuban American females, have lower 1-year suicide rates relative to 1-year prevalence rates of major depression than do whites. Males in all ethnic groups had higher relative suicide rates than females in their respective ethnic groups. The robustness of the finding suggests the presence of as-yet undetermined biological, genetic, or cultural protective factors for suicide. The identification of these factors may guide suicide prevention efforts.
 |
 |
 |
 |
 |
 |
Received April 5, 2000; revisions received Nov. 13, 2000, and March 5, 2001; accepted March 30, 2001. From the Conte Center for the Neuroscience of Mental Disorders: The Neurobiology of Suicidal Behavior and the Department of Clinical Genetic Epidemiology, New York State Psychiatric Institute and Columbia University. Address reprint requests to Dr. Oquendo, Department of Neuroscience, New York State Psychiatric Institute, Unit 42, 1051 Riverside Dr., New York, NY 10032. Supported by NIMH grants MH-35636, MH-46745, MH-37592, and MH-30906.
1. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8-19Crossref, Medline, Google Scholar
2. Jones-Webb RJ, Snowden LR: Symptoms of depression among blacks and whites. Am J Public Health 1993; 83:240-244Crossref, Medline, Google Scholar
3. Moscicki EK, Rae DS, Regier DA, Locke BZ: The Hispanic Health and Nutrition Examination Survey: depression among Mexican Americans, Cuban Americans, and Puerto Ricans, in Health and Behavior: Research Agenda for Hispanics—Research Monograph 1. Edited by Gaviria M, Arana J. Chicago, University of Illinois, 1987, pp 145-159Google Scholar
4. Narrow WE, Rae DS, Moscicki EK, Locke BZ: Depression among Cuban Americans. Soc Psychiatry Psychiatr Epidemiol 1990; 25:260-268Crossref, Medline, Google Scholar
5. Potter LB, Rogler LH, Moscicki EK: Depression among Puerto Ricans in New York City. Soc Psychiatry Psychiatr Epidemiol 1995; 30:185-193Crossref, Medline, Google Scholar
6. Somervell PD, Leaf PJ, Weissman MM, Blazer DG, Bruce ML: The prevalence of major depression in black and white adults in five United States communities. Am J Epidemiol 1989; 130:725-735Crossref, Medline, Google Scholar
7. Stoff DM, Mann JJ: The Neurobiology of Suicide: From the Bench to the Clinic. New York, New York Academy of Sciences, 1997Google Scholar
8. Carlson GA, Rich CL, Grayson P, Fowler RC: Secular trends in psychiatric diagnoses of suicide victims. J Affect Disord 1991; 21:127-132Crossref, Medline, Google Scholar
9. Dorpat TL, Ripley HS: A study of suicide in the Seattle area. Compr Psychiatry 1960; 1:349-359Crossref, Medline, Google Scholar
10. Henriksson MM, Aro HM, Marttunen MJ, Heikkinen ME, Isometsä ET, Kuoppasalmi KI, Lönnqvist JK: Mental disorders and comorbidity in suicide. Am J Psychiatry 1993; 150:935-940Link, Google Scholar
11. Rihmer Z, Barsi J, Veg K, Katona CLE: Suicide rates in Hungary correlate negatively with reported rates of depression. J Affect Disord 1990; 20:87-91Crossref, Medline, Google Scholar
12. Rutz W, Von Knorring L, Wálinder J: Frequency of suicide on Gotland after systematic postgraduate education of general practitioners. Acta Psychiatr Scand 1989; 80:151-154Crossref, Medline, Google Scholar
13. Goodwin FK, Jamison KR: Suicide, in Manic-Depressive Illness. New York, Oxford Press, 1990, pp 227-244Google Scholar
14. Malone KM, Haas GL, Sweeney JA, Mann JJ: Major depression and the risk of attempted suicide. J Affect Disord 1995; 34:173-185Crossref, Medline, Google Scholar
15. Platt S: Unemployment and suicidal behaviour. Soc Sci Med 1984; 19:93-115Crossref, Medline, Google Scholar
16. Weissman MM, Bruce ML, Leaf PJ, Florio LP, Holzer C: Affective disorders, in Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. Edited by Robins LN, Regier DA. New York, Free Press, 1991, pp 53-80Google Scholar
17. Robins LN, Helzer JE, Croughan J, Ratcliff KS: The National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Arch Gen Psychiatry 1981; 38:381-389Crossref, Medline, Google Scholar
18. Desenclos JC, Hahn RA: Years of potential life lost before age 65, by race, Hispanic origin, and sex—United States, 1986-1988. Mor Mortal Wkly Rep CDC Surveill Summ 1992; 41:13-23Medline, Google Scholar
19. Hollman FW: United States Population Estimates, by Age, Sex, Race, and Hispanic Origin:1980 to 1998: Publication 25-1095. Washington, DC, US Government Printing Office, 1990Google Scholar
20. Breslow N, Day NL: Statistical Methods in Cancer Research: The Design and Analysis of Cohort Studies, vol II. Lyon, France, Iarc Scientific, 1987Google Scholar
21. Pothoff R, Woodbury MA, Manton KG: “Equivalent sample size” and “equivalent degrees of freedom” refinements for inference using survey weights under superpopulation models. J Am Statistical Assoc 1992; 87:383-389Google Scholar
22. Fleiss JL: Statistical Methods for Rates and Proportions, 2nd ed. New York, John Wiley & Sons, 1981Google Scholar
23. Weissman MM, Bland RC, Canino GJ, Faravelli C, Greenwald S, Hwu HG, Joyce PR, Karam EG, Lee CK, Lellouch J, Lépine JP, Newman SC, Rubio-Stipec M, Wells JE, Wickramaratne PJ, Wittchen HU, Yeh EK: Cross-national epidemiology of major depression and bipolar disorder. JAMA 1996; 276:293-299Crossref, Medline, Google Scholar
24. Siegel S: Nonparametric Strategies for the Behavioral Sciences. New York, McGraw-Hill, 1956, pp 175-179Google Scholar
25. Hasmer D, Lemeshow S: Applied Logistic Regression. New York, John Wiley & Sons, 1989, pp 27-34Google Scholar
26. Regier DA, Robins LN: Introduction, in Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. Edited by Robins LN, Regier DA. New York, Free Press, 1991, pp 1-10Google Scholar
27. Canino GJ, Bird HR, Shrout PE, Rubio-Stipec M, Bravo M, Martinez R, Sesman M, Guevara LM: The prevalence of specific psychiatric disorders in Puerto Rico. Arch Gen Psychiatry 1987; 44:727-735Crossref, Medline, Google Scholar
28. Vera M, Alegria M, Freeman D, Robles RR, Rios R, Rios CF: Depressive symptoms among Puerto Ricans: island poor compared with residents of the New York City area. Am J Epidemiol 1991; 134:502-510Crossref, Medline, Google Scholar
29. Coelho VLD, Strauss ME, Jenkins JH: Expression of symptomatic distress by Puerto Rican and Euro-American patients with depression and schizophrenia. J Nerv Ment Dis 1998; 186:477-483Crossref, Medline, Google Scholar
30. Arató M, Demeter E, Rihmer Z, Somogyi E: Retrospective psychiatric assessment of 200 suicides in Budapest. Acta Psychiatr Scand 1988; 77:454-456Crossref, Medline, Google Scholar
31. Chynoweth R, Tonge JI, Armstrong J: Suicide in Brisbane: a retrospective psychosocial study. Aust NZ J Psychiatry 1980; 14:37-45Crossref, Medline, Google Scholar
32. Barraclough B, Bunch J, Nelson B, Sainsbury P: One hundred cases of suicide. Br J Psychiatry 1974; 125:355-373Crossref, Medline, Google Scholar
33. Beskow J: Suicide and mental disorder in Swedish men. Acta Psychiatr Scand Suppl 1979; 277:1-138Medline, Google Scholar
34. Griffith EH, Bell CC: Recent trends in suicide and homicide among blacks. JAMA 1989; 262:2265-2269Crossref, Medline, Google Scholar
35. Shaffer D, Gould M, Hicks RC: Worsening suicide rate in black teenagers. Am J Psychiatry 1994; 151:1810-1812Link, Google Scholar
36. La Vecchia C, Lucchini F, Levi F: Worldwide trends in suicide mortality, 1955-1989. Acta Psychiatr Scand 1994; 90:53-64Crossref, Medline, Google Scholar
37. Hoppe SK, Martin HW: Patterns of suicide among Mexican Americans and Anglos, 1960-1980. Soc Psychiatry 1986; 21:83-88Crossref, Medline, Google Scholar
38. Smith JC, Mercy JA, Warren CW: Comparison of suicides among Anglos and Hispanics in five Southwestern states. Suicide Life Threat Behav 1985; 15:14-26Crossref, Medline, Google Scholar



