Disability and Quality of Life in Social Phobia: Epidemiologic Findings
Abstract
OBJECTIVE: Social phobia in clinical studies is vividly associated with extensive disability and reduced quality of life. It is difficult to obtain a clear portrayal of the impairment associated with social phobia in community samples. Furthermore, it has been unclear in prior studies to what extent indices were attributable to social phobia as opposed to comorbid major depression. The authors examined relevant data from the Ontario Health Survey Mental Health Supplement. METHOD: The Ontario Health Survey Mental Health Supplement, a survey of more than 8,000 residents of Ontario, Canada, aged 15–64, used the University of Michigan Composite International Diagnostic Interview to assign DSM-III-R diagnoses. Several indicators of disability and quality of life were included. The authors compared these indices for persons with and without social phobia and adjusted where indicated for the effects of major depression and relevant sociodemographic factors. RESULTS: Persons with social phobia were impaired on a broad spectrum of measures, ranging from dropping out of school to experiencing disability in one’s main activity. They were also significantly more likely than persons without social phobia to rate themselves as “low functioning” on the Quality of Well-Being Scale and to report dissatisfaction with many aspects of life. Depressive comorbidity seemed to contribute only modestly to these outcomes. CONCLUSIONS: Social phobia can be a serious, disabling anxiety disorder associated with marked reduction in quality of life. Impairment in social phobia is substantial, even in the absence of comorbid major depression.
Social phobia (also known as social anxiety disorder) has drawn increased attention as a highly prevalent—although often unrecognized—anxiety disorder (1–4). Studies in three different countries have placed the 1-year prevalence of social phobia in the 5%–8% range, making it the most common anxiety disorder and one of the most common psychiatric disorders (5–7).
Although social phobia is irrefutably common, it has been more difficult to establish the extent to which it should be considered a “serious” mental disorder from a public health perspective. In clinical study groups, patients with social phobia have been clearly shown in a number of studies to experience substantial functional impairment (8, 9). In a study of 44 patients with social phobia, Safren et al. (10) showed that these patients perceived their quality of life to be relatively poor. Moreover, quality of life in that study was inversely related to the severity of social phobia.
In a study that measured a related construct—illness intrusiveness, the extent to which an illness interferes with functioning—Antony et al. (11) found that 49 patients with social phobia reported substantial interference with their day-to-day functioning in multiple domains. In that study patients with social phobia reported a level of illness intrusiveness that was comparable to that experienced by patients with panic disorder and patients with obsessive-compulsive disorder. When compared indirectly to patients with a variety of other chronic illnesses (e.g., multiple sclerosis, rheumatoid arthritis, and end-stage renal disease), patients with social phobia demonstrated comparable or more severe perceived impairment. Thus, from the perspective of patients with social phobia who seek treatment, the extent of their disability and the reduction in quality of life is substantial.
From an epidemiologic perspective, it has been more difficult to ascertain the extent of impairment associated with social phobia. In large part, this is because the premier contemporary psychiatric epidemiologic surveys, including the Epidemiologic Catchment Area Study (ECA) (12) and the National Comorbidity Survey (13), were not intended to assess disability to any great extent. Thus, although each of these studies has demonstrated particular adversities associated with social phobia (e.g., greater suicidal ideation, financial problems, and greater likelihood of seeking help from a professional) (1, 14), a more fine-grained analysis in this regard has been lacking. An exception is the report from the Durham site of the ECA study, which included additional questions pertinent to the assessment of functional disability (15). Persons diagnosed with social phobia in that study, in addition to poor employment performance and reduced social interaction, reported more difficulties in school during adolescence. The findings pertaining to academic difficulties have yet to be replicated, to our knowledge.
Although the aforementioned studies were unable to paint a complete picture of the impairment associated with social phobia in the community, they have provided a very thorough perspective on the extent to which social phobia is comorbid with other psychiatric conditions (1, 5, 14, 15). In fact, lifetime comorbidity with other disorders, such as major depression, is the rule rather than the exception among patients with social phobia (16, 17). From the converse perspective, social phobia is known to be the most commonly occurring anxiety disorder among people with mood disorders (18, 19). Prior studies have shown that comorbidity probably accounts for at least some of the impairment associated with social phobia in the community (1, 15). As such, in order to convincingly demonstrate that impairment is associated with social phobia per se, rather than a comorbid condition such as depression, it becomes necessary to demonstrate impairment when the effects of depressive comorbidity are removed from the equation.
The goal of this study was to examine the range and breadth of disability and reduced quality of life associated with social phobia in the community. Although multiple forms of comorbidity (e.g., alcohol abuse, depression, and other anxiety disorders) undoubtedly affect functioning in persons with social phobia, it was not possible to simultaneously adjust for all forms of comorbidity. We therefore made the decision to focus on the comorbid disorder that, independently, is known to be associated with extreme reductions in quality of life in community samples—major depression (20, 21). This is also the most common form of comorbidity seen in patients with social phobia (17). An additional goal of our study was to examine functioning across the two subtypes of social phobia—the generalized and nongeneralized forms, respectively. Initial reports have suggested that the latter is associated with more pervasive functional impairment (14, 22), a finding we wished to explore further in the present study.
To accomplish these goals, we analyzed data from the Mental Health Supplement to the Ontario Health Survey, a large Canadian epidemiologic survey that was contemporary, and nearly identical in design, to that of the National Comorbidity Survey (6). A difference in design was that the Mental Health Supplement included an extensive set of questions intended to provide a detailed assessment of disability associated with psychiatric disorders in the community (23). This enabled us to gain a more complete perspective on functional impairment in social phobia than had previously been possible in a community survey.
Method
Survey
The methodology of the Mental Health Supplement to the Ontario Health Survey is covered in detail elsewhere (6, 24). Briefly, the Mental Health Supplement was a province-wide, cross-sectional epidemiologic survey of psychiatric disorders among those aged 15 years and older living in household dwellings in Ontario, Canada. Respondents for the Mental Health Supplement were drawn from households (N=13,002) participating in the Ontario Health Survey. One person per household was selected to complete the survey, and 9,953 (76.5%) participated. The instrument used to measure psychiatric disorder (the University of Michigan Composite International Diagnostic Interview) was identical to that used in the National Comorbidity Survey (13). Field trials of the Composite International Diagnostic Interview show it to be a highly reliable instrument for almost all diagnoses except mania and psychosis (25).
In the Mental Health Supplement, the University of Michigan Composite International Diagnostic Interview provided prevalence data on 14 DSM-III-R psychiatric disorders: anxiety disorders (social phobia, simple phobia, agoraphobia, panic disorder, and generalized anxiety disorder), affective disorders (major depressive disorder, dysthymia, and manic disorder), bulimia nervosa, substance use disorders (alcohol, marijuana, and other substance abuse or dependence), and antisocial behaviors (antisocial personality disorder and adult antisocial behavior).
Although an abbreviated interview was administered to respondents aged 65 years and older, this interview did not discuss social phobia. Consequently, the data reported here are based on material from respondents aged 15–64 (N=8,116).
Subtyping Social Phobia
Diagnoses of social phobia were dichotomously subtyped according to the criteria we used previously in analyses of National Comorbidity Survey data (14). These criteria were empirically derived from a latent class analysis of social phobic fears. When we used these definitions, if a respondent endorsed social fears exclusively in large- or small-group public speaking settings, a diagnosis of the speaking fears subtype of social phobia was applied. If other social fears (e.g., eating in public or writing while someone is watching) were endorsed, then a diagnosis of the more general, or complex, form of social phobia was applied. In analyses of National Comorbidity Survey data, the complex fears subtype of social phobia has been shown to be associated with greater comorbidity and increased help seeking compared to the speaking fears subtype (14). The complex fears subtype of social phobia found in epidemiologic samples is felt to be roughly equivalent to what is referred to as “generalized social phobia” in clinical groups (22, 26).
Assessment of Disability and Functioning
The Mental Health Supplement to the Ontario Health Survey incorporates multiple measures of disability. Disability is conceptualized in broad terms as limitations in functioning manifested in various life domains and associated with the presence of disorder.
Definitions of Disability
The measure of dysfunction in main activity is based on questions about limitations in work or school performance or opportunities. The questions ask how well respondents have been able to perform their main activity (work, school, household chores, or volunteering) and whether they attribute difficulties in performance to mental health or substance abuse problems. Responses of “very well,” “quite well,” or “fairly well” were coded as satisfactory function, whereas “not too well” or “not well” were coded as dysfunction. Questions about childcare, getting around the neighborhood, getting out of the house, and personal care were used to assess dysfunction in other daily activities. The frame of reference for these questions was the past 12 months.
Troubled relationships were assessed by asking how well respondents got along with various people (e.g., family, friends, or co-workers) in the last 6 months. Response choices were as indicated, and responses of “not too well” or “not well” in any relationship category were coded as troubled relationships.
Functioning in usual activities in the previous 30 days was assessed in the following manner. Respondents were asked, because of mental health problems (“problems with your emotions, nerves or mental health, or with your use of alcohol or drugs”), 1) how many days in the prior 30 they were totally unable to do the things they normally did, 2) how many days in the prior 30 they had to cut down on what they did or accomplished less, and 3) how many days in the prior 30 it took an extreme effort to perform their usual level of work. Because the time frame of these questions was recent (i.e., in the past 30 days), we focused on current diagnoses of social phobia.
Dissatisfaction was measured by using a series of questions about satisfaction in five different life domains: main activity, family relationships, friendships, leisure activities, and income by using a 6-point scale (extremely satisfied, quite satisfied, fairly satisfied, fairly dissatisfied, quite dissatisfied, or extremely dissatisfied). Any of three negative responses (fairly, quite, or extremely dissatisfied) were coded as dissatisfaction.
Quality of life was assessed with the Quality of Well-Being Scale (27). This empirically validated scale assessed seven indicators: energy, control of emotions, state of morale, interest in life, perceived stress, perceived health status, and satisfaction about relationships. Scores on the Quality of Well-Being Scale, which ranged from 0 to 42, were categorized (on the basis of their distribution in the sample) for the purposes of logistic regression analyses into states of “very low or low well-being” (scores of 0–24, which included 17.9% [N=1,453] of the respondents) or “medium or high well-being” (scores of 25–42, which included 82.1% [N=6,663] of the respondents). Cronbach’s coefficient alpha for the Quality of Well-Being Scale in this sample was 0.85. Scholastic difficulties were assessed by asking respondents whether they had ever repeated or failed a grade and whether they had left school before grade 12.
Statistical Analytic Approach
Logistic regression analysis was used to calculate odds ratios for the various disability and quality-of-life variables as a function of diagnosis. Specifically, the odds ratios reflected the likelihood of persons with social phobia experiencing one of the outcomes, compared to persons without social phobia. To achieve one of the primary aims of our study—namely, to determine if major depressive disorder was a confounding variable with respect to outcomes—respondents were stratified into those with and without major depression, and odds ratios with 95% confidence intervals (CIs) were calculated for each stratum (i.e., social phobia with major depression and social phobia without major depression) (28). To summarize the data, odds ratios and 95% CIs were plotted for the relationship between outcome and each of three independent variables: 1) all persons with social phobia, 2) only nondepressed persons with social phobia, and, 3) as a comparator, all persons with major depressive disorder. The data plots provide an index of the relative effects of social phobia, social phobia in the absence of depressive comorbidity, and major depression. Since the latter disorder has been established in the literature to have strong deleterious effects on functioning and health-related quality of life (20, 21), we felt that including it would provide a perspective on the relative “potency” of the effects of social phobia.
All prevalence estimates of psychiatric disorders were weighted. However, frequencies (i.e., “N”) in Table 1 refer to unweighted values, whereas rates and proportions in tables and text refer to weighted values, adjusted for the sampling framework.
The time frames for the diagnoses and the specific outcomes under consideration were matched as closely as possible for each of the relevant analyses. For example, functioning in usual activities in the prior 30 days was examined in relationship to past-30-day (i.e., current) diagnoses; dysfunction in daily activities, which was asked in reference to the prior 12 months, was examined in relationship to past-year diagnoses; and dropping out of school early was examined in relation to lifetime diagnoses. When looking at the indexes of satisfaction and Quality of Well-Being Scale scores, however, we used a lifetime time frame. We reasoned that early-onset psychiatric disorders such as social phobia could have long-lasting effects on these dimensions of quality of life and that it would be most appropriate to look at these outcomes from a lifelong perspective. This, it should be noted, provided the most conservative estimate of the effects of social phobia (and major depression, which was included as a point of reference); when past-year or current diagnoses were analyzed, the odds ratios were in all cases larger than those obtained by using lifetime diagnoses. For these analyses, we had sufficient statistical power to examine the independent contributions of social phobia and major depressive by adjusting for each (along with age, gender, and social class) in a simultaneous multiple regression analysis. This presentation of the data permits the direct comparison of the relative strengths of these associations.
When it was feasible to do so, social phobia subtypes (i.e., speaking only versus other, more generalized types) (14) were compared and contrasted. For all logistic regression analyses (unless otherwise specified), social class (of parents, categorized as having blue- or white-collar jobs), gender, and age (categorized as shown in Table 1) were simultaneously entered as covariates to provide for odds ratios that were adjusted for these variables.
Because of the complex sampling design (24), standard errors were computed by using first-order Taylor series approximation of the deviations of estimates from their expected values (29) with the computer program SUDAAN Version 6.4 (30).
Results
Prevalence and Sociodemographic Characteristics
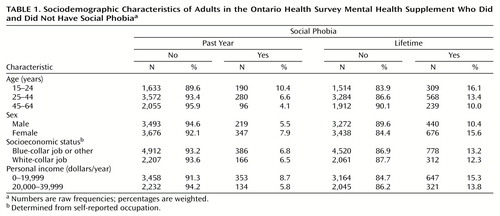
One-year and lifetime prevalence rates of social phobia in the Mental Health Supplement were 6.7% (SE=0.5%) and 13.0% (SE=0.6%), respectively. The rates are very consistent with those obtained from the National Comorbidity Survey (5), and they illustrate that social phobia is an extremely common condition. Presented in Table 1 are the sociodemographic characteristics of persons with and without social phobia. Also, consistent with findings from the National Comorbidity Survey (5), lifetime social phobia in the Mental Health Supplement was associated with a significantly greater likelihood of being female (odds ratio adjusted for age group and socioeconomic status=1.56, 95% CI=1.27–1.92; Wald χ2=17.12, df=1, p<0.001) and of being young (odds ratio adjusted for gender and socioeconomic class=1.85, 95% CI=1.36–2.51 for the 15–24-year-old age group and adjusted odds ratio=1.48, 95% CI=1.11–1.99 for the 25–44-year-old age group; reference age group was 45–64-year-olds; Wald χ2=15.75, df=2, p<0.001). Social phobia in the Mental Health Supplement was not significantly associated with social class (white-collar job versus blue-collar job or other; odds ratio adjusted for age group and sex=1.12, 95% CI=0.89–1.42; Wald χ2=0.92, df=1, p=0.34) or personal income ($0–$19,999 versus $20,000–$39,999; adjusted odds ratio=1.02, 95% CI=0.75–1.38; Wald χ2=0.01, df=1, p=0.92).
Subtypes of Social Phobia
Lifetime prevalence of the subtype of social phobia consisting solely of speaking fears was 7.0% (SE=0.5%), whereas lifetime prevalence of the subtype consisting of more generalized or complex fears was 5.9% (SE=0.4%). That is, approximately one-half (54.0%) of the persons with social phobia in the Mental Health Supplement had the speaking fear subtype of social phobia, whereas the remainder (46.0%) had the complex fears subtype of social phobia. The same patterns of association with sociodemographic factors seen for social phobia as a whole generally held true for the two subtypes of social phobia (e.g., both types were more common in women; data not shown).
Comorbidity With Major Depression
Lifetime prevalence of major depression in the Mental Health Supplement was 8.3% (11.3% for women and 5.2% for men). Lifetime social phobia in the Mental Health Supplement was associated with a significantly greater likelihood of experiencing lifetime major depression (χ2=33.98, df=1, p<0.001; odds ratio=3.32, 95% CI=2.45–4.49). Approximately one-third (33.8%) of the persons with lifetime social phobia had a lifetime diagnosis of major depression; on a 12-month basis, comorbidity was 15.7%. From the converse perspective, approximately one-fifth (19.5%) of the persons with lifetime major depression had a lifetime diagnosis of social phobia. These findings confirm the strong association between social phobia and major depression that has been seen in other epidemiologic surveys (1, 7, 14, 16, 17, 31).
Nearly all of the comorbidity between social phobia and major depression was explained by the association of the complex fears subtype of social phobia with major depression. The lifetime complex fears subtype of social phobia was strongly associated with lifetime major depression (χ2=42.24, df=1, p<0.001; odds ratio=6.41, 95% CI=4.56–9.01), whereas the lifetime speaking fears subtype of social phobia was not (χ2=0.06, df=1, p=0.81; odds ratio=1.06, 95% CI=0.67–1.68). Once again, these findings were consistent with those obtained in the National Comorbidity Survey (14).
Functional Impairment in Social Phobia
Dysfunction in daily activities
A diagnosis of social phobia within the past year was associated with a significantly greater likelihood of reporting dysfunction in one’s main activity (odds ratio=8.48, 95% CI=4.57–15.71; Wald χ2=46.06, df=1, p<0.001) or other daily activities (odds ratio=7.94, 95% CI=4.70–13.42; Wald χ2=60.03, df=1, p<0.001), adjusting for the effects of age group, sex, and social class. Persons with the complex fears subtype of social phobia were much more likely to be impaired on both indexes than were persons with the speaking fears subtype of social phobia. Adjusted odds ratios for the comparison of the complex fears subtype with the speaking fears subtype of social phobia were 9.46 (dysfunction in main activity: 95% CI=2.62–34.07; Wald χ2=11.80, df=1, p<0.001) and 8.60 (dysfunction in other daily activities: 95% CI=2.69–27.46; Wald χ2=13.19, df=1, p<0.001), respectively.
Past-year major depressive disorder was more strongly associated with dysfunction in daily activities than was past-year social phobia but not significantly (Figure 1; note overlapping CIs). Similarly, the effects of social phobia remained strong, even in the absence of major depressive comorbidity (Figure 1).
Troubled relationships
A past-year diagnosis of social phobia was associated with a greater likelihood of reporting dysfunction in one’s interpersonal relationships, but this effect failed to attain statistical significance after adjustment for the effects of age group, gender, and social class (adjusted odds ratio=1.87, 95% CI=0.87–3.99; Wald χ2=2.61, df=1, p=0.11). The complex fears subtype of social phobia was significantly more likely than the speaking fears subtype to show this association (odds ratio=3.23, 95% CI=1.02–10.24; Wald χ2=3.95, df=1, p<0.05).
Past-year major depression was more strongly associated than was past-year social phobia with dysfunction in relationships but not significantly so (Figure 1). Similarly, the effects of social phobia with or without major depressive comorbidity did not differ significantly (Figure 1).
Functioning in usual activities in the past 30 days
Responses on this measure were highly skewed, with only 1.4%, 2.6%, and 2.9% of the respondents reporting any days totally disabled, days of reduced activity, or days where extreme effort was required, respectively. We therefore dichotomized responses into 0 days affected by mental illness versus 1 or more days affected.
A past-year diagnosis of social phobia (after adjustment for age group, gender, and socioeconomic status) was associated with a statistically significantly greater likelihood of 1) being unable to perform one’s usual activities for at least 1 day in the past 30 days (adjusted odds ratio=8.77, 95% CI=3.99–19.29; Wald χ2=29.12, df=1, p=0.001), 2) a reduction in activity or accomplishing less at least 1 day in the past 30 days (adjusted odds ratio=4.39, 95% CI=2.00–9.65; Wald χ2=13.52, df=1, p<0.001), and 3) requiring extreme effort to perform one’s usual activities for at least 1 day in the past 30 days (adjusted odds ratio=4.98, 95% CI=3.54–10.43; Wald χ2=19.57, df=1, p<0.001). The magnitude of these associations was several-fold stronger for the complex fears subtype of social phobia than for the speaking fears subtype, but small cell sizes yielded very large CIs that precluded definitive interpretation.
As shown in Figure 2, current major depressive disorder had a more profound impact on each of these indexes than did current social phobia, although these differences did not reach statistical significance (note overlapping CIs). Similarly, the relationship between current social phobia and these indexes was not significantly different in the absence of current major depressive comorbidity (Figure 2).
Scholastic difficulties
A lifetime diagnosis of social phobia was associated with a significantly greater likelihood of having failed a grade (adjusted odds ratio=1.77, 95% CI=1.38–2.28; Wald χ2=20.14, df=1, p<0.001) after adjustment for age group, gender, and socioeconomic status. The association between social phobia and failing a grade was significantly stronger among persons with the complex fears subtype of social phobia than among those with the speaking fears subtype (when compared directly, adjusted odds ratio=1.87, 95% CI=1.18–2.97; Wald χ2=7.00, df=1, p=0.008).
A total of 38.1% (SE=2.5%) of the persons with social phobia did not complete high school, compared to 30.1% (SE=1.1%) of persons without social phobia. After adjustment for age group, gender, and socioeconomic status, a lifetime diagnosis of social phobia was associated with a significantly greater likelihood of leaving school early (i.e., before graduating from high school) (adjusted odds ratio=1.77, 95% CI=1.39–2.26; Wald χ2=21.36, df=1, p<0.001). There was no significant difference in the likelihood of dropping out of school when comparing the complex fears subtype of social phobia to the speaking fears subtype (adjusted odds ratio=1.36, 95% CI=0.88–2.10; Wald χ2=1.95, df=1, p=0.16). The presence or absence of comorbid lifetime major depressive disorder had no significant impact on these outcomes.
Satisfaction and Quality of Life in Social Phobia
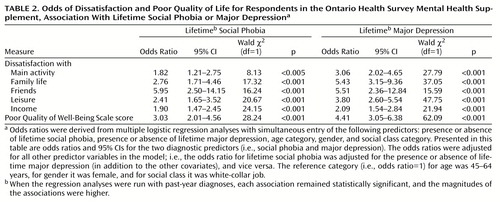
Dissatisfaction with various life domains
A lifetime diagnosis of social phobia was associated with a significantly greater likelihood of reporting dissatisfaction with one’s main activity, family life, friends, leisure activities, and income (Table 2) after adjustment for age group, gender, and presence or absence of lifetime major depression. The complex or generalized type of social phobia exhibited even stronger associations with dissatisfaction with main activity (adjusted odds ratio=2.69, 95% CI=1.38–5.25; Wald χ2=8.46, df=1, p=0.004) and family life (adjusted odds ratio=3.15, 95% CI=1.57–6.31; Wald χ2=10.46, df=1, p=0.001) but was similar to social phobia as a whole on the other domains.
As shown in Table 2, major depression (after adjustment for the effects of age group, gender, and lifetime social phobia) was also associated with dissatisfaction on each of these measures, with the magnitude of these associations being similar to (or, for some variables, slightly stronger than) those seen for social phobia. Nevertheless, even when they were adjusted for lifetime major depressive comorbidity (as shown in Table 2), the associations with social phobia remained statistically significant and robust. When past-year diagnoses were examined (instead of lifetime diagnoses), the associations with social phobia remained statistically significant and were, in all instances, greater in magnitude (data not shown).
Quality of well-being
A lifetime (Table 2) or past-year (adjusted odds ratio=2.96, 95% CI=1.98–4.43; Wald χ2=27.95, df=1, p<0.001) diagnosis of social phobia was associated with a significantly greater likelihood of reporting poor quality of well-being after adjustment for age group, gender, and lifetime major depression. When the past-year complex fears subtype of social phobia was contrasted directly with the past-year speaking fears subtype of social phobia, the former was found to be associated with a several-fold greater likelihood of reporting poor quality of well-being (adjusted odds ratio=3.46, 95% CI=1.68–7.15; Wald χ2=11.26, df=1, p<0.001).
Conclusions
Social phobia (social anxiety disorder) has achieved sufficient notoriety in the past decade and a half that it can no longer be termed a “neglected anxiety disorder” (31). In recent years we have come to recognize that social phobia is common (5, 7), highly comorbid with other conditions such as depression (1, 17, 26, 32), and, unfortunately, largely underrecognized and undertreated in primary care (3, 33, 34). From studies of clinical, treatment-seeking groups, we have also come to understand that social phobia can be a debilitating disorder (4, 8, 9, 15). These findings have galvanized interest in social phobia among mental health providers and researchers alike.
Despite the availability of these findings, there have been very few data demonstrating that persons with social phobia in the community are impaired by their disorder. Relying on treatment-seeking persons with social phobia to gauge the extent of impairment and reduced quality of life associated with this disorder may provide a skewed portrayal of these indexes, for several reasons. First, treatment-seeking individuals are likely to be a more severe subset of the population of persons with social phobia and, as such, are unlikely to be representative of most persons with the disorder. Second, treatment-seeking patients with social phobia may be coming in for treatment because of a comorbid disorder, such as major depression. In this instance, the measurement of impairment may be confounded by the presence of the comorbid disorder and its own attendant difficulties. Thus, in order to gain an accurate perspective on the burden of illness associated with social phobia in the community—which would be among the factors that would designate it as a public health problem worthy of more serious consideration—we felt that it was necessary to examine impairment and reduced quality of life in a community setting and to account for possible confounds (e.g., major depression and social class) in the assessment of these outcomes.
We found that social phobia was a common condition, with 12-month and lifetime prevalence rates mirroring those found in a similar study, the National Comorbidity Survey (5, 13). We also found that social phobia could be divided into two subtypes, one characterized by problems with speaking (in front of large or small groups) only and another characterized by other social fears (almost always in combination with speaking fears). In the National Comorbidity Survey, we found that approximately two-thirds of the patients had the complex fears subtype of social phobia (14), whereas the proportion was closer to one-half in the present study. Although it was not a large discrepancy, the reasons for this difference between studies are unknown and should be further explored in new surveys that provide a more detailed and comprehensive assessment of socially fearful situations.
The central findings from this study were remarkably robust on nearly all fronts. On virtually every index of functional impairment and life satisfaction, persons with social phobia fared worse than persons without social phobia. Even when the analyses were adjusted statistically or stratified for the presence of major depression—which, as expected, was itself associated with great functional adversity—social phobia carried with it a large, independent burden of illness. Adjustment for social class and gender which, to the best of our knowledge, has not been attempted in prior analyses, modified some of the relationships, in some cases more clearly highlighting the effects of social phobia on particular outcomes (e.g., scholastic difficulties and early school dropout).
On many indexes of functioning and quality of life, patients with the complex fears subtype of social phobia were noted to fare worse than did persons with the speaking fears subtype of social phobia. This finding is consistent with the observation from clinical studies that the generalized type of social phobia—which would be subsumed by our broader epidemiologic designation of the complex fears subtype of social phobia—is a more severe, serious illness than the nongeneralized type (2, 4, 14). From a public health perspective, it is this form of the disorder that we feel deserves the most critical attention.
There are several limitations to this study that deserve mention. First, it should be understood that although we focused on assessing the impact of the most predominant form of comorbidity, major depression, we did not control for the possible presence of other comorbid disorders such as panic disorder, generalized anxiety disorder, or substance abuse. To stratify illness on the basis of each of these variables would have been impossible, resulting in cell sizes that would have been too small to permit interpretation. Nonetheless, we must consider the possibility that these unaccounted-for forms of comorbidity may have influenced our findings.
Second, it should be noted that the measures of disability and dissatisfaction used in this study—although considerably more detailed and comprehensive than those used in prior community surveys of social phobia—are still fairly generic. They do not approach the fine-grained analysis of disability that can be accomplished when questions that are specifically pertinent to social phobia (e.g., “To what extent did your social anxiety interfere with your education?”) are utilized. This is a shortcoming of the present study compared to those conducted with clinical groups (8). It is our expectation—although this remains to be confirmed—that were such disorder-specific measures administered to a community sample of persons with social phobia, the magnitude of their disability and reduced quality of life would be even more impressive than that revealed here. The need for studies that use this approach in community samples has been documented (35).
In summary, we found that persons with social phobia in the community reported extensive functional disability, less life satisfaction, and a lower quality of well-being compared to persons without social phobia. These associations are explained only in part by comorbidity with major depression and little or not at all by group differences in age, gender, or social class. Taken together with findings from prior studies (7–11, 14, 15), this demonstration of pervasive impairment and reduced quality of life in social phobia should encourage public health policy makers to include social phobia among other “serious” mental disorders and to implement systematic efforts to treat and/or prevent it.
Finally, we wish to draw attention to the finding that persons with social phobia in the community report a greater likelihood of failing a grade or dropping out of school early, compared to persons without social phobia. These are associations not found, to the best of our knowledge, in any other anxiety or depressive disorder. This finding is compatible with an earlier report by Davidson and colleagues (15) and points to the need for school-based programs to identify and treat social phobia in children and adolescents. Such a strategy offers the hope of preventing some of the adverse outcomes highlighted in this report. Whether or not this hope will be realized will depend, of course, on the conduct of systematic, prospective research.
 |
 |
Received July 21, 1999; revisions received Dec. 21, 1999, and March 1, 2000; accepted May 3, 2000. From the Anxiety and Traumatic Stress Disorders Program, Department of Psychiatry, University of California at San Diego; and the VA San Diego Healthcare System, La Jolla, Calif. Address reprint requests to Dr. Stein, Anxiety and Traumatic Stress Disorders Program, Department of Psychiatry (0985), University of California, San Diego, La Jolla, CA 92093-0985; [email protected] (e-mail).Supported by a research grant from SmithKline Beecham Pharmaceuticals, Philadelphia.The government of the Province of Ontario, Canada, provided access to the data from the Ontario Health Survey Mental Health Supplement. Mariette J. Chartier, R.N., M.Sc., and John R. Walker, Ph.D., provided help during the planning stages of this project.
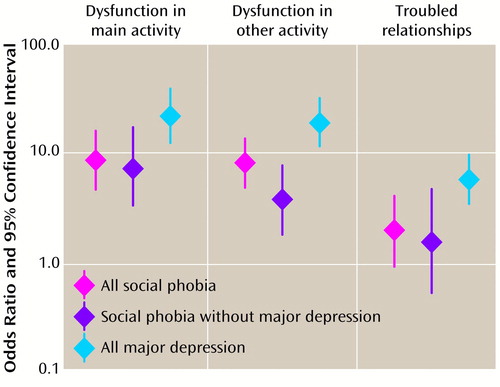
Figure 1. Odds of Dysfunction or Troubled Relationships in the Past Year for Respondents in the Ontario Health Survey Mental Health Supplement With Social Phobia or Major Depression in the Past Yeara
aThe odds ratios were adjusted by using SUDAAN software to account for sampling framework. Overlapping CIs indicate that odds ratios are not significantly different
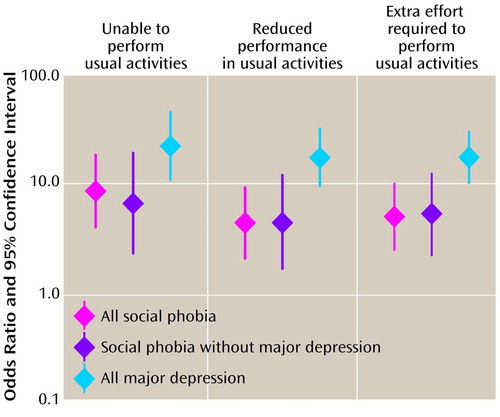
Figure 2. Odds of Difficulty in Usual Activities in the Past 30 Days for Respondents in the Ontario Health Survey Mental Health Supplement With Social Phobia or Major Depression in the Past 30 Daysa
aThe odds ratios were adjusted by using SUDAAN software to account for sampling framework. Overlapping CIs indicate that odds ratios are not significantly different.
1.. Schneier FR, Johnson J, Hornig CD, Liebowitz MR, Weissman MM: Social phobia: comorbidity and morbidity in an epidemiological sample. Arch Gen Psychiatry 1992; 49:282–288Crossref, Medline, Google Scholar
2.. Stein MB: How shy is too shy? Lancet 1996; 347:1131–1132Google Scholar
3.. Weiller E, Bisserbe JC, Boyer P, Lepine JP, Lecrubier Y: Social phobia in general health care: an unrecognized undertreated disabling disorder. Br J Psychiatry 1996; 168:169–174Crossref, Medline, Google Scholar
4.. den Boer JA: Social phobia: epidemiology, recognition, and treatment. Br Med J 1997; 315:796–800Crossref, Medline, Google Scholar
5.. Magee WJ, Eaton WW, Wittchen HU, McGonagle KA, Kessler RC: Agoraphobia, simple phobia, and social phobia in the National Comorbidity Survey. Arch Gen Psychiatry 1996; 53:159–168Crossref, Medline, Google Scholar
6.. Offord DR, Boyle MH, Campbell D, Goering P, Lin E, Wong M, Racine YA: One-year prevalence of psychiatric disorder in Ontarians 15 to 64 years of age. Can J Psychiatry 1996; 41:559–563Crossref, Medline, Google Scholar
7.. Wittchen H-U, Nelson CB, Lachner G: Prevalence of mental disorders and psychosocial impairments in adolescents and young adults. Psychol Med 1998; 28:109–126Crossref, Medline, Google Scholar
8.. Schneier FR, Heckelman LR, Garfinkel R, Campeas R, Fallon BA, Gitow A, Street L, Del Bene D, Liebowitz MR: Functional impairment in social phobia. J Clin Psychiatry 1994; 55:322–331Medline, Google Scholar
9.. Wittchen H-U, Beloch E: The impact of social phobia on quality of life. Int Clin Psychopharmacol 1996; 11(suppl 3):15–23Google Scholar
10.. Safren SA, Heimberg RG, Brown EJ, Holle C: Quality of life in social phobia. Depress Anxiety 1997; 4:126–133Crossref, Google Scholar
11.. Antony MM, Roth D, Swinson RP, Huta V, Devins GM: Illness intrusiveness in individuals with panic disorder, obsessive-compulsive disorder, or social phobia. J Nerv Ment Dis 1998; 186:311–315Crossref, Medline, Google Scholar
12.. Robins LN, Helzer JE, Weissman MM, Orvaschel H, Gruenberg E, Burke JD Jr, Regier DA: Lifetime prevalence of specific psychiatric disorders in three sites. Arch Gen Psychiatry 1984; 41:949–958Crossref, Medline, Google Scholar
13.. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8–19Crossref, Medline, Google Scholar
14.. Kessler RC, Stein MB, Berglund PA: Social phobia subtypes in the National Comorbidity Survey. Am J Psychiatry 1998; 155:613–619Link, Google Scholar
15.. Davidson JRT, Hughes DL, George LK, Blazer DG: The epidemiology of social phobia: findings from the Duke Epidemiologic Catchment Area Study. Psychol Med 1993; 23:709–718Crossref, Medline, Google Scholar
16.. Merikangas KR, Angst J: Comorbidity and social phobia: evidence from clinical, epidemiologic, and genetic studies. Eur Arch Psychiatry Clin Neurosci 1995; 244:297–303Crossref, Medline, Google Scholar
17.. Kessler RC, Stang P, Wittchen H-U, Stein MB, Walters EE: Lifetime comorbidities between social phobia and mood disorders in the US National Comorbidity Survey. Psychol Med 1999; 29:555–567Crossref, Medline, Google Scholar
18.. Merikangas KR, Angst J, Eaton WW, Canino G, Rubio-Stipec M, Wacker H, Wittchen H-U, Andrade L, Essau C, Whitaker A, Kraemer H, Robins LN, Kupfer DJ: Comorbidity and boundaries of affective disorders with anxiety disorders and substance misuse: results of an international task force. Br J Psychiatry 1996; 168:58–67Crossref, Google Scholar
19.. Pini S, Cassano GB, Simonini E, Savino M, Russo A, Montgomery SA: Prevalence of anxiety disorders comorbidity in bipolar depression, unipolar depression and dysthymia. J Affect Disord 1997; 42:145–153Crossref, Medline, Google Scholar
20.. Hays RH, Wells KB, Sherbourne CD, Rogers W, Spritzer K: Functioning and well-being outcomes of patients with depression compared with chronic general medical illnesses. Arch Gen Psychiatry 1995; 52:11–19Crossref, Medline, Google Scholar
21.. Wells KB, Sherbourne CD: Functioning and utility for current health of patients with depression or chronic medical conditions in managed, primary care practices. Arch Gen Psychiatry 1999; 56:897–904Crossref, Medline, Google Scholar
22.. Wittchen H-U, Stein MB, Kessler RC: Social fears and social phobia in a community sample of adolescents and young adults: prevalence, risk factors and co-morbidity. Psychol Med 1999; 29:309–323Crossref, Medline, Google Scholar
23.. Goering P, Lin E, Campbell D, Doyle MH, Offord DR: Psychiatric disability in Ontario. Can J Psychiatry 1996; 41:564–571Medline, Google Scholar
24.. Boyle MH, Offord DR, Campbell D, Catlin G, Goering P, Lin E, Racine YA: Mental health supplement to the Ontario Health Survey: methodology. Can J Psychiatry 1996; 41:549–558Crossref, Medline, Google Scholar
25.. Kessler RC, Wittchen H-U, Abelson JM, McGonagle KA, Schwarz N, Kendler KS, Knauper B, Zhao S: Methodological studies of the Composite International Diagnostic Interview (CIDI) in the US National Comorbidity Survey (NCS). Int J Methods in Psychiatr Res 1998; 7:33–55Crossref, Google Scholar
26.. Stein MB, Chavira DA: Subtypes of social phobia and comorbidity with depression and other anxiety disorders. J Affect Disord 1998; 50:S11–S16Google Scholar
27.. McDowell I, Newell C: Measuring Health: A Guide to Rating Scales and Questionnaires. New York, Oxford University Press, 1987, pp 125–133Google Scholar
28.. Kahn HA, Sempos CT: Statistical Methods in Epidemiology. New York, Oxford University Press, 1989Google Scholar
29.. Woodruff RS, Causey BD: Computerized method for approximating the variance of a complicated estimate. J Am Stat Assoc 1976; 71:315–321Crossref, Google Scholar
30.. Shah BV, Barnwell BG, Hunt PN, Lavange LM: SUDAAN User’s Manual, Version 6.0. Research Triangle Park, NC, Research Triangle Institute, 1992Google Scholar
31.. Liebowitz MR, Gorman JM, Fyer AJ, Klein DF: Social phobia: review of a neglected anxiety disorder. Arch Gen Psychiatry 1985; 42:729–736Crossref, Medline, Google Scholar
32.. Warner V, Weissman MM, Mufson L, Wickramaratne PJ: Grandparents, parents, and grandchildren at high risk for depression: a three-generation study. J Am Acad Child Adolesc Psychiatry 1999; 38:289–296Crossref, Medline, Google Scholar
33.. Bisserbe JC, Weiller E, Boyer P, Lepine JP, Lecrubier Y: Social phobia in primary care: level of recognition and drug use. Int Clin Psychopharmacol 1996; 11:25–28Crossref, Medline, Google Scholar
34.. Stein MB, McQuaid JR, Laffaye C, McCahill ME: Social phobia in the primary care setting. J Fam Pract 1999; 48:514–519Medline, Google Scholar
35.. Mendlowicz MV, Stein MB: Quality of life in individuals with anxiety disorders. Am J Psychiatry 2000; 157:669–682Link, Google Scholar



