Evaluating Three Treatments for Borderline Personality Disorder: A Multiwave Study
Abstract
Objective: The authors examined three yearlong outpatient treatments for borderline personality disorder: dialectical behavior therapy, transference-focused psychotherapy, and a dynamic supportive treatment. Method: Ninety patients who were diagnosed with borderline personality disorder were randomly assigned to transference-focused psychotherapy, dialectical behavior therapy, or supportive treatment and received medication when indicated. Prior to treatment and at 4-month intervals during a 1-year period, blind raters assessed the domains of suicidal behavior, aggression, impulsivity, anxiety, depression, and social adjustment in a multiwave study design. Results: Individual growth curve analysis revealed that patients in all three treatment groups showed significant positive change in depression, anxiety, global functioning, and social adjustment across 1 year of treatment. Both transference-focused psychotherapy and dialectical behavior therapy were significantly associated with improvement in suicidality. Only transference-focused psychotherapy and supportive treatment were associated with improvement in anger. Transference-focused psychotherapy and supportive treatment were each associated with improvement in facets of impulsivity. Only transference-focused psychotherapy was significantly predictive of change in irritability and verbal and direct assault. Conclusions: Patients with borderline personality disorder respond to structured treatments in an outpatient setting with change in multiple domains of outcome. A structured dynamic treatment, transference-focused psychotherapy was associated with change in multiple constructs across six domains; dialectical behavior therapy and supportive treatment were associated with fewer changes. Future research is needed to examine the specific mechanisms of change in these treatments beyond common structures.
Impulsivity, diminished nonaffective constraint, negative affectivity, and emotional dysregulation are core characteristics of borderline personality disorder (1 – 3) . The prevalence of borderline personality disorder in the community is approximately 1.3% to 1.4% (4 , 5) . This chronic and debilitating syndrome is associated with high rates of medical and psychiatric utilization of services (6 , 7) . Psychopharmacology notwithstanding, psychotherapy represents the recommended primary technique for treating borderline personality disorder (8) . Dialectical behavior therapy (9) has demonstrated superiority over treatment as usual (10) and therapy by community experts (11) .
Other therapeutic approaches, such as psychodynamic treatments, continue to be prominent in the treatment of borderline personality disorder, as supported by the APA Practice Guideline (8) and prior research (12) . A promising psychodynamic treatment approach is an object relations approach called transference-focused psychotherapy (13) . Transference-focused psychotherapy is an effective treatment using patients as their own comparisons (14) and has demonstrated superiority over treatment as usual (unpublished data by KN Levy et al. available from the authors).
A necessary and first step in illuminating effective treatments for borderline personality disorder is to show that a given treatment is associated with significant improvement in the disorder—improvement in relevant dimensions of pathology beyond self-damaging behaviors. Empirical evidence should show that candidate treatments, such as dialectical behavior therapy and psychodynamic approaches, are systematically related to change in a number of substantive domains of clinical significance. A recent influential review reported that existing therapies for borderline personality disorder remain experimental, and more “real-world” studies are necessary (15) .
We examined patients who were taken from the community and reliably diagnosed with borderline personality disorder. Patients were randomly assigned to transference-focused psychotherapy, dialectical behavior therapy, or supportive treatment for 1 year. Our study has characteristics of both efficacy and effectiveness studies. Similar to an efficacy study, we used random assignment to treatments, manualized treatments, blind raters, therapists blind to all baseline assessments, and specific and reliably measured outcome variables. Similar to an effectiveness study, however, we included a range of borderline personality disorder patients. Therapists provided treatment in their private offices in the community rather than in a university or hospital setting. Medication treatment was decided on an individual basis so that the use or nonuse of medication and medication type and amount were not standardized.
Method
Participants
The patients were men and women between the ages of 18 and 50 (mean age: 30.9 [SD=7.85] years) who met DSM-IV criteria (16) for borderline personality disorder. Individuals with comorbid psychotic disorders, bipolar I disorder, delusional disorder, delirium, dementia, and/or amnestic as well as other cognitive disorders were excluded. Those with active substance dependence were also excluded, although patients with past substance dependence and past and current substance abuse were included. Patients were recruited from New York City and the adjacent tri-state area.
Assessments and Procedures
Patients were screened for age and location in telephone interviews. Suitable individuals were assessed in face-to-face evaluations by trained evaluators prior to their assignment to treatment. Each participant received a diagnosis of borderline personality disorder based on DSM-IV criteria as assessed by the International Personality Disorders Examination (17) . High levels of reliability were obtained for the number of DSM-IV borderline personality disorder criteria met by each subject (single rater intraclass correlation coefficient [1, 1]=0.83). An acceptable level of reliability for borderline personality disorder diagnosis was obtained (kappa=0.64). Exclusion diagnoses were based on the Structured Clinical Interview for DSM-IV (SCID) (18) .
Domains of outcome
A priori, we chose suicidality, aggression, and impulsivity as primary outcome domains and anxiety, depression, and social adjustment as secondary outcome domains. The variables of interest were assessed at baseline and at 4, 8, and 12 months (termination of treatment). Thus, each study participant was measured on the same variables at approximately the same intervals at four points in time; however, the assessment intervals varied slightly. Measures and outcome domains are provided in Table 1 .
Treatment and therapists
After initial assessments, patients were randomly assigned to one of the three outpatient treatment conditions for 1 year. Additionally, all patients were evaluated for pharmacotherapy at entry into the study by one of three study psychiatrists who were blind to psychotherapy assignment. A medication algorithm (19) was used to guide the pharmacological treatment.
The three psychotherapies were delivered with attention to preserving their integrity and ecological validity (20) . Therefore, dialectical behavior therapy consisted of a weekly individual and group session and available telephone consultation. Transference-focused psychotherapy consisted of two individual weekly sessions, and supportive treatment consisted of one weekly session, which could be supplemented with additional sessions as needed.
The primary focus of transference-focused psychotherapy is on the dominant affect-laden themes that emerge in the relationship between patient and therapist. It has been hypothesized that dialectical behavior therapy operates through the learning of emotion regulation skills in the validating environment provided by the treatment (9) . Supportive treatment (21) provides emotional support—advice on the daily problems facing the patient with borderline personality disorder. The therapist follows and manages the transference but explicitly does not use interpretations.
In the present study, each of the three psychotherapies was administered and supervised by a treatment condition leader. Dialectical behavior therapy was supervised by Barbara Stanley, Ph.D., transference-focused psychotherapy by Frank Yeomans, M.D., and supportive treatment by Ann Appelbaum, M.D., all of whom are acknowledged experts. A total of 19 therapists were selected by the treatment condition leaders based on prior demonstration of competence in their respective modality. All therapists had advanced degrees in social work, psychology, or psychiatry, with at least 2 years of prior experience treating patients with borderline personality disorder. All therapists were monitored and supervised weekly by treatment condition leaders who were available to observe videotaped sessions, provide feedback, and rate therapists for adherence and competence.
Statistical Analysis of Change
We used individual growth curve analysis to investigate change in the dimensions of symptoms and functioning over time (22 – 26) . The individual growth curve approach hypothesizes that, for each individual, the continuous outcome variable is a specified function of time called the individual growth trajectory, plus error. This trajectory is specified as a simple linear function of time containing two important unknown individual growth parameters—an intercept and a slope—that determine the shape of individual true growth over time. The individual intercept parameter represents the net “elevation” of the trajectory over time. The individual slope parameter represents the rate of change over time and in this study is the within-person rate of change in the dependent variable over time. Individual growth trajectories are specified at level 1 and capture individual change over time. A level 2 model is then used to investigate the way that the individual growth parameters at level 1 are related to between-subjects factors.
The hypothesized level 1 and level 2 statistical models were fitted simultaneously using hierarchical linear modeling (full maximum likelihood) (27) . First, we conducted a set of “unconditional” growth analyses (24 , 26) , in which we posited a linear individual-change trajectory at level 1. Such unconditional analyses partition the outcome variation into variance components that describe the net variation in slope and intercept across individuals.
We fitted two sets of “conditional” (level 2) analyses that examined systematic interindividual differences in the intercept and slope values from level 1. The first set of level 2 conditional analyses examined whether age at entry into the study predicted change. The second set of conditional analyses represented the central analyses for the study, namely the use of the between-subjects factor of the treatment group (transference-focused psychotherapy, supportive treatment, dialectical behavior therapy) to explain differences in level 1 intercept and slope values. Importantly, the conditional model for these analyses deleted the intercepts in each of the two level 2 equations. Deletion of the intercepts from the level 2 equations allows for easy inspection of the fixed effects associated with each treatment. It also allows for straightforward evaluation of the null hypothesis that membership in a given treatment group is not associated with an intercept or slope that differs from zero. The level 2 models yield “fixed effects” in the prediction of the slope and intercept values at level 1. Additionally, level 2 models yield estimates of residual variance that describe remaining interindividual variability in the individual slopes and intercepts after accounting for the fixed effects (available upon request from the authors).
Using each subject’s date of birth and exact assessment dates, the time between assessments for each participant was calculated in months and then centered on age at entry into the study for each participant. Centering the assessment intervals on age at entry and including age at entry as a predictor at level 2 account for each participant’s unique chronological age when he or she began the study and cause the individual level 1 intercepts to represent the true value of the first (time 1) assessments as the participants’ “initial status.” Individual growth curves were derived only for those participants who had completed three or four assessment waves.
Results
Patient Characteristics
Between 1998 and 2003, 336 patients were referred to our project. Of the 336 referrals, 129 either did not meet criteria or decided not to schedule an intake interview. We interviewed 207 individuals for at least one evaluation session; of these, 109 were eligible for randomization. Exclusions were because of the following reasons: did not meet criteria for borderline personality disorder (N=34), age (N=30), current substance dependence (N=9), psychotic disorder (N=8), bipolar I disorder (N=6), IQ below 80 (N=2), scheduling conflict (N=1), and dropouts (N=8). Of the 109 participants eligible for randomization, 90 were randomized to treatment. There were no differences in terms of demographics, diagnostic data, or severity of psychopathology between those who were randomized to treatment and those who were not. Patient characteristics are provided in Table 2 (number of lifetime axis II disorders: mean=2.49 [SD=1.13]). More detail regarding participant referral and selection, rater and participant characteristics, and assessment of reliability is available elsewhere (28) . The present analyses are based on the patients for whom we obtained three or more data points, which included 23 transference-focused psychotherapy patients, 17 dialectical behavior therapy patients, and 22 supportive treatment patients, indicating continuation into the 9- to 12-month period.
Medication Treatment
At treatment onset, 70% of dialectical behavior therapy, 65% of supportive treatment, and 52% of transference-focused psychotherapy patients were placed on medication. The percentage of patients receiving medication remained relatively constant throughout the 1-year treatment period. Any difference in the percentage of patients receiving medication in the three treatment cells cannot be attributed to symptom severity, since there were no significant differences between the three groups of patients at time 1 on the domain measures.
Individual Growth Curve Analyses
An unconditional growth model was fitted for all domains, providing estimates of the average elevation and rate of change parameters and their natural variation across all participants at entry into the study. The estimated average elevation of the individual growth trajectories at entry into the study (intercepts) differed significantly from zero for all domain dimensions (all p<0.001). These results were expected, since the borderline personality disorder patients were relatively impaired. Notably, the estimated average rates of change (i.e., slopes) also differed significantly from zero for all of the domain dimensions, except for the Barratt Factor 3 impulsivity and anxiety dimensions (29) , indicating that much change over time was evident in the data (all p=≤0.05).
The first set of level 2 conditional analyses examined whether the age at which a participant entered the study was related to change on the various domain variables, irrespective of treatment group. Statistically, age at entry into the study was not significantly related to intercept (level) values for any of the domain dimensions. Age at entry into the study was also essentially unrelated to the slope (rate of change) values for the domain dimensions, except for global functioning (p<0.02), suicidality (past week) (p<0.05), and Barratt Factor 1 impulsivity (p<0.02). Thus, differing developmental levels reflected, albeit crudely, through chronological age were not related to elevation and rate of change in the domain dimensions. Therefore, age at entry was not included in the second set of level 2 conditional analyses. Additionally, age at entry did not differ significantly across the three treatment groups (F=1.26, df=2, 59, p=0.30).
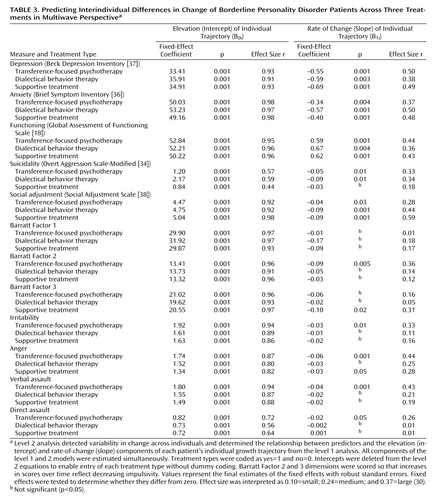
The second set of level 2 conditional analyses investigated the impact of the three treatments on the level and rate of change (slope) in the participants. As noted previously, the intercept was deleted from each of the two level 2 equations in order to facilitate direct examination of the effect of each treatment group on the level and rate of change. In these analyses, we determined whether the level and rate of change observed for any of the treatment groups differed significantly from zero. With respect to the rate of change (or slope), the null hypothesis would be that a treatment has no impact on change, and therefore it should not be statistically related to change (or growth) over time. Table 3 contains the fixed effects and variance components associated with each level 2 predictor (i.e., treatment group), the approximate p value for testing that these effects are zero in the population, and an estimate of the “effect size r” (30) .
With respect to elevation, each of the three treatment groups was a statistically significant predictor of individual elevation parameters in the domain variables (all p<0.001, “large” effect sizes). Given that the cohort consisted of subjects diagnosed with borderline personality disorder, it was expected that the elevations would all differ from zero.
The critical growth parameter for this study is the individual slope parameter as it directly indexes the rate and direction of individual change over time. The prediction of slope (change) at level 2 by each of the three treatments was significant for depression, anxiety, global functioning, and social adjustment (all p<0.05); the direction of effects was toward symptom improvement. Both transference-focused psychotherapy and dialectical behavior therapy were significantly associated with improvement in suicidality over time, and both transference-focused psychotherapy and supportive treatment were significantly associated with improvement in anger over time. Only transference-focused psychotherapy was significantly predictive of symptom improvement in Barratt Factor 2 impulsivity, irritability, verbal assault, and direct assault. Supportive treatment alone was predictive of improvement in Barratt Factor 3 impulsivity. None of the three treatments was associated with improvement in Barratt Factor 1 impulsivity. Thus, transference-focused psychotherapy predicted significant improvement in 10 of the 12 variables, dialectical behavior therapy in five of the 12 variables, and supportive treatment in six of the 12 variables.
We also refit the level 2 models examining treatment effects for the global functioning, suicidality, and Barratt Factor 1 domains, including both the treatment group and age at entry variables. For both the global functioning and suicidality domains, inclusion of the age at entry variable made the significant associations between the three treatment types and improvement in these domains stronger. Inclusion of age at entry for Barratt Factor 1 did not alter the nonsignificant relationships between the treatment types and this variable as found in the initial conditional analyses ( Table 2 ).
The hierarchical linear model approach allows for hypothesis testing using the method of contrast analysis. We conducted one contrast analysis for each domain of analysis based on theoretical predictions contained in the treatment manuals (15 , 27) and the results of prior research. In short, to conserve space, we found that only one contrast was close to statistically reliable, namely a contrast of slope coefficients that posited that transference-focused psychotherapy and dialectical behavior therapy should show stronger relationships with decreases in suicidal behavior than supportive treatment (and transference-focused psychotherapy and dialectical behavior therapy should not differ [i.e., transference-focused psychotherapy=dialectical behavior therapy>supportive treatment]). This contrast of slope coefficients approached significance (χ 2 =2.17, df=1, p<0.07; one-tailed).
We also conducted an intent-to-treat analysis. Such an analysis is used to determine whether those participants dropping out of the various treatment cells have affected the pattern of findings across the treatments compared with when the analyses are restricted to only those completing the study. We carried forward the last known value for a variable for any participant who was assessed once or twice in the protocol. For those participants who dropped out of the study, we assumed assessments at 4, 8, or 12 months as time intervals. Therefore, the intent-to-treat analysis database contained all those participants analyzed in the “completer” analyses as well as those who had data carried forward as described above. In the intent-to-treat analysis, the same variables of interest were analyzed using the identical hierarchical linear model procedure described previously. The results for the intent-to-treat analysis did not differ in terms of the pattern of findings from those obtained through the “completer” analyses. The p values attached to each of the significance tests for the coefficients for the intercept and slope variables were, as one would expect, higher, given the greater degrees of freedom. These results suggest that participant attrition did not substantially alter the findings obtained in the completer analyses.
One must consider the possible impact of medication on change, specifically whether medication interacted differentially with any of the three treatments to amplify change for patients in one or more of the treatments. To examine this possibility, we conducted a parallel set of growth curve analyses on only those subjects who had been medicated at the study entry and through at least the third assessment. In short, the pattern of findings (direction of effects, effect sizes) across the 12 dependent variables for the three treatments in this restricted cohort where medication was held constant was highly similar to that reported in Table 3 for the entire cohort.
Discussion
The major finding of this randomized controlled trial was that transference-focused psychotherapy, dialectical behavior therapy, and supportive treatment showed some significant relation to positive change in multiple domains across 1 year of outpatient treatment. This pattern suggests that these structured treatments for borderline personality disorder are generally equivalent with respect to broad positive change in borderline personality disorder (31) . Nonetheless, some differences emerged across the three treatments in relation to change. For the primary outcome variables, both transference-focused psychotherapy and dialectical behavior therapy were significantly associated with improvement in suicidality, whereas transference-focused psychotherapy and supportive treatment were associated with improvement in anger. Only transference-focused psychotherapy was significantly predictive of symptom improvement in Barratt Factor 2 impulsivity, irritability, verbal assault, and direct assault. Supportive treatment alone was predictive of improvement in Barratt Factor 3 impulsivity. Regarding secondary outcome variables, each of the three treatments was significantly predictive of the rate of change in a positive direction for depression, anxiety, global functioning, and social adjustment. Overall, transference-focused psychotherapy was predictive of significant improvement in 10 of the 12 variables across the six domains, dialectical behavior therapy in five of the 12, and supportive treatment in six of the 12.
Only one contrast analysis yielded a tendency toward significance, which suggests that transference-focused psychotherapy and dialectical behavior therapy, the two treatments with a specific focus on the reduction of suicidal behaviors in borderline personality disorder patients, were more effective than a general supportive treatment.
Four design issues in this study deserve comment. To our knowledge, this is the first randomized controlled trial design that examines three well-described (manualized) treatments for borderline personality disorder, one of which (dialectical behavior therapy) is considered by many to be a standard treatment in the field, which represents a design of the highest level of control (32) . Second, although transference-focused psychotherapy and supportive treatment share many of the same basic techniques, they differ in a way that allows for a component of therapeutic control (transference-focused psychotherapy employs transference interpretation as a possible mechanism of change, whereas supportive treatment does not). Third, our design combines features of both efficacy and effectiveness studies. Patients from a large tri-state metropolitan area were referred to us, and inclusion/exclusion criteria were based on criteria used in clinical practice. Patients were assessed at a community-serving, university-affiliated hospital, and the treatments were delivered by community practitioners in their private offices. One might expect attenuated outcomes with the treatments delivered in the community, without the structure and the expectancies provided by a university setting in which many randomized controlled studies of this kind are conducted. Finally, we report both completer and intent-to-treat analyses and thus address both the internal and external validity of the study. Completer analyses speak to the issue of sufficient dose, whereas intent-to-treat analyses provide generalizability to the community.
There are three areas of limitation in the present study. Similar to other statistical methods, statistical power in multilevel modeling of growth curves is a function of four factors: cohort size, variance in the cohort, size of the effect being studied, and the number of data waves available. Although reliable a priori effect sizes were not available for our three treatments and we did not wish to constrain the patient characteristics in an artificial manner to reduce variability, we feel that a larger cohort and more data waves might have yielded more significant results because of increased power. Ethical constraints did not allow a no-treatment comparison group for self-destructive and highly suicidal borderline personality disorder patients. In a similar fashion, it was not possible to standardize medications across these patients whose pathology called for individualized medication treatments. However, we note that the pattern of results observed for the medicated subgroup of patients was highly similar to that observed for the full cohort.
The general equivalence of outcome across the three treatments studied suggests that there may be different routes to symptom change in patients with borderline personality disorder. In contrast to dialectical behavior therapy, which focuses directly on skills to help the patient regulate emotion and reduce symptoms, transference-focused psychotherapy focuses on developing greater self-control through the integration of representations of self and other as they are activated in the relationship with the therapists. In this study, transference-focused psychotherapy effects were observed across a broader range of outcome domains than dialectical behavior therapy and supportive treatment. Given the pervasiveness and chronicity of borderline personality disorder, future research will need to examine the maintenance of these symptom changes and specification of the mechanisms through which treatments relate to outcome (33) .
1. Depue RA, Lenzenweger MF: A neurobehavioral model of personality disturbance, in Major Theories of Personality Disorder, 2nd ed. Edited by Lenzenweger MF, Clarkin JF. New York, Guilford, 2005, pp 391–453Google Scholar
2. Paris J: The classification of personality disorders should be rooted in biology. J Personal Disord 2000; 14:127–136Google Scholar
3. Trull TJ: Structural relations between borderline personality disorder features and putative etiological correlates. J Abnorm Psychol 2001; 110:471–481Google Scholar
4. Lenzenweger MF, Loranger AW, Korfine L, Neff C: Detecting personality disorders in a nonclinical population: application of a two-stage procedure for case identification. Arch Gen Psychiatry 1997; 54:345–351Google Scholar
5. Lenzenweger MF, Lane M, Loranger AW, Kessler RC: DSM-IV personality disorders in the National Comorbidity Survey Replication (NCS-R). Biol Psychiatry (in press)Google Scholar
6. Bender DS, Dolan RT, Skodol AE, Sanislow CA, Dyck IR, McGlashan TH, Shea MT, Zanarini MC, Oldham JM, Gunderson JG: Treatment utilization by patients with personality disorders. Am J Psychiatry 2001; 158:295–302Google Scholar
7. Zanarini MC, Frankenburg FR, Hennen J, Silk KR: Mental health service utilization by borderline personality disorder patients and axis II comparison subjects followed prospectively for 6 years. J Clin Psychiatry 2004; 65:28–36Google Scholar
8. Oldham JM, Gabbard GO, Goin MK, Gunderson J, Soloff P, Spiegel D, Stone M, Phillips KA: Practice guideline for the treatment of patients with borderline disorder. Am J Psychiatry 2001; 158 (suppl):1–52Google Scholar
9. Linehan MM: Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York, Guilford, 1993Google Scholar
10. Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard H: Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch Gen Psychiatry 1991; 48:1060–1064Google Scholar
11. Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, Korslund KE, Tutek DA, Reynolds SK, Lindenboim N: Two-year randomized controlled trial and follow-up of dialectical behavior theapy vs. therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry 2006; 63:757–766Google Scholar
12. Bateman A, Fonagy P: Effectiveness of partial hospitalization in the treatment of borderline personality disorder: a randomized controlled trial. Am J Psychiatry 1999; 156:1563–1569Google Scholar
13. Clarkin JF, Yeomans F, Kernberg OF: Psychotherapy of Borderline Personality. New York, John Wiley and Sons, 1999Google Scholar
14. Clarkin JF, Foelsch PA, Levy KN, Hull JW, Delaney JC, Kernberg OF: The development of a psychodynamic treatment for patients with borderline personality disorder: a preliminary study of behavioral change. J Personal Disord 2001; 15:487–495Google Scholar
15. Binks CA, Fenton M, McCarthy L, Lee T, Adams CE, Duggan C: Psychological therapies for people with borderline personality disorder. Cochrane Database Syst Rev 2006; 25:CD005652Google Scholar
16. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, 1994Google Scholar
17. Loranger A: International Personality Disorder Examination (IPDE) Manual. Odessa, Fla, Psychological Assessment Resources, Inc., 1999Google Scholar
18. First MB, Gibbon M, Spitzer RL, Williams JBW: User’s Guide for the Structured Clinical Interview for DSM-IV Axis I Research Version (SCID-1), version 2.0, New York, New York State Psychiatric Institute, Biometrics Research, 1996Google Scholar
19. Soloff PH: Psychopharmacology of borderline personality disorder. Psychiatr Clin North Am 2000; 23:169–192Google Scholar
20. Elkin J, Pilkonis P, Docherty JP, Stosky SM: Conceptual and methodological issues in comparative studies of psychotherapy and psychopharmacology, I: active ingredients and mechanisms of change. Am J Psychiatry 1988; 145:909–917Google Scholar
21. Rockland LH: Supportive Therapy for Borderline Patients: A Psychodynamic Approach. New York, Guilford, 1992Google Scholar
22. Rogosa D, Brandt D, Zimowski M: A growth curve approach to the measurement of change. Psychol Bull 1982; 92:726–748Google Scholar
23. Rogosa DR, Willett JB: Understanding correlates of change by modeling individual differences in growth. Psychometrika 1985; 50:203–228Google Scholar
24. Singer JD, Willett JB: Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York, Oxford University Press, 2003Google Scholar
25. Raudenbush SW, Bryk AS: Hierarchical Linear Models: Applications and Data Analysis Methods, 2nd ed. Thousand Oaks, Calif, Sage Publications, 2002Google Scholar
26. Lenzenweger MF, Johnson MD, Willett JB: Individual growth curve analysis illuminates stability and change in personality disorder features: the longitudinal study of personality disorders. Arch Gen Psychiatry 2004; 61:1015–1024Google Scholar
27. Raudenbush SW, Bryk AS, Congdon R: HLM-6: Hierarchical Linear and Nonlinear Modeling. Lincolnwood, Ill, Scientific Software International, 2005Google Scholar
28. Critchfield KL, Levy KN, Clarkin JF: The Personality Disorders Institute/Borderline Personality Disorder Research Foundation randomized control trial for borderline personality disorder: reliability of axis I and II diagnoses. Psychiatry Q 2007; 78:15–24Google Scholar
29. Patton JH, Stanford MS, Barratt ES: Factor structure of the Barratt Impulsiveness Scale. J Clin Psychol 1995; 51:768–774Google Scholar
30. Rosenthal R, Rosnow RL: Essentials of Behavioral Research: Methods and Data Analysis, 2nd ed. New York, McGraw-Hill, 1991Google Scholar
31. Roth A, Fonagy P: What Works for Whom? A Critical Review of Psychotherapy Research, 2nd ed. New York, Guilford, 2005Google Scholar
32. Gabbard GO, Gunderson JG, Fonagy P: The place of psychoanalytic treatments within psychiatry. Arch Gen Psychiatry 2002; 59:505–510Google Scholar
33. Clarkin JF, Levy KN: Special issue: putative mechanisms of action in the psychotherapy treatment of borderline personality disorder. J Clin Psychol 2006; 62:405–516Google Scholar
34. Coccaro EF, Harvey PD, Kupsaw-Lawerence E, Herbert JL, Bernstein DP: Development of neuropharmacologically based behavioral assessments of impulsive aggressive behavior. J Neuropsychiatry Clin Neurosci 1991; 3(suppl):s44–s51Google Scholar
35. Coccaro EF, Kavoussi RJ: Fluoxetine and impulsive-aggressive behavior in personality disordered subjects. Arch Gen Psychiatry 1997; 54:1081–1088Google Scholar
36. Derogatis LR: Brief Symptom Inventory (BSI): Administration, Scoring, and Procedures Manual, 3rd ed. Minneapolis, National Computer Systems, 1993Google Scholar
37. Beck AT, Steer RA, Brown GK: Manual for the Beck Depression Inventory, 2nd ed. San Antonio, Tex, Psychological Corp, 1996Google Scholar
38. Weissman MM, Bothwell S: Assessment of social adjustment by patient self-report. Arch Gen Psychiatry 1976; 33:1111–1115Google Scholar