Treatment of Bereavement-Related Major Depressive Episodes in Later Life: A Controlled Study of Acute and Continuation Treatment With Nortriptyline and Interpersonal Psychotherapy
Abstract
OBJECTIVE: The authors tested the hypothesis that nortriptyline and interpersonal psychotherapy, alone and in combination, are superior to placebo in achieving remission of bereavement-related major depressive episodes. METHOD: Eighty subjects, aged 50 years and older, with major depressive episodes that began within 6 months before or 12 months after the loss of a spouse or significant other were randomly assigned to a 16-week double-blind trial of one of four treatment conditions: nortriptyline plus interpersonal psychotherapy (N=16), nortriptyline alone in a medication clinic (N=25), placebo plus interpersonal psychotherapy (N=17), or placebo alone in a medication clinic (N=22). The protocol required that the acute-phase double-blind treatment be ended after 8 weeks if Hamilton depression scale ratings had not improved by 50%. Remission was defined as a 17-item Hamilton scale score of 7 or lower for 3 consecutive weeks. RESULTS: The rate of remission for nortriptyline plus interpersonal psychotherapy was 69% (N=11); for medication clinic, nortriptyline, 56% (N=14); for placebo plus interpersonal psychotherapy, 29% (N=5); and for medication clinic, placebo, 45% (N=10). In a generalized logit model, there was a significant effect of nortriptyline over placebo but no interpersonal psychotherapy effect and no nortriptyline-by-interpersonal psychotherapy interaction. Rates of all-cause attrition were lowest in the nortriptyline plus interpersonal psychotherapy group. CONCLUSIONS: Nortriptyline was superior to placebo in achieving remission of bereavement-related major depressive episodes. The combination of medication and psychotherapy was associated with the highest rate of treatment completion. These results support the use of pharmacologic treatment of major depressive episodes in the wake of a serious life stressor such as bereavement.
Conjugal bereavement is a common life event for older Americans. The annual incidence of spousal loss through death has been estimated to be 1.6% for elderly men and 3.0% for elderly women (1). About 800,000 persons in the United States become newly widowed each year, and most of them are in the later years of life (2).
Conjugal bereavement is frequently associated with symptoms of a major depressive episode, with subsyndromal depressive symptoms, or with posttraumatic distress. About one-third of widows and widowers meet the DSM criteria for a major depressive episode 1 month after the death of the spouse, one-fourth 2–7 months after the death, and approximately 15% 13 months after the death (3–5). Thus, of the approximately 800,000 persons who are widowed each year, at least 120,000 will suffer from prolonged and potentially serious major depression (6). It is likely that even larger numbers of bereaved spouses will suffer painful but subsyndromal depressive symptoms. Moreover, conjugal bereavement is a risk factor for suicide in later life, particularly for men. As noted in a review by Conwell (7), a separated, divorced, or widowed status places the elderly at higher risk for suicide. A disproportionate number of elderly persons who commit suicide are living alone at the time of death, suggesting social isolation as a risk factor (8). Finally, not only are there negative changes in mental health accompanying bereavement, but also negative changes in physical health and an increased mortality rate usually accompany widowhood, particularly among men (9, 10).
Despite these well-documented public health costs and psychiatric complications of bereavement and bereavement-related depression, we know of no controlled data on the treatment of bereavement-related depression with either pharmacotherapy or psychotherapy. Both the Institute of Medicine (11) and the National Institutes of Health Consensus Conference on the Diagnosis and Treatment of Depression in Late Life (12) noted the lack of controlled trials and recommended that such studies be considered a public health priority. Accordingly, we undertook a randomized, placebo-controlled clinical trial to examine the efficacy of an antidepressant medication (nortriptyline) and of a manual-based interpersonal psychotherapy (13). We hypothesized that treatment with nortriptyline, interpersonal psychotherapy, or their combination would be superior to placebo in bringing about remission of major depressive episodes. We also hypothesized an interactive effect of nortriptyline and interpersonal psychotherapy in which the two treatments in combination would be better than either alone and better than placebo.
METHOD
We recruited 80 subjects into the study over a 7-year period, beginning in March 1991 and concluding in February 1998. Recruitment for this study was difficult and labor-intensive, as we recently detailed in a description of our methods of recruitment (14). Briefly, most subjects were self-referred in response to print advertisements or letters sent from the investigators to surviving spouses identified in obituaries. Relatively few patients were clinically referred.
To be included in the study, potential subjects were required to meet the criteria of the Schedule for Affective Disorders and Schizophrenia—Lifetime Version (SADS-L) (15) and the Research Diagnostic Criteria (RDC) (16) for a definite current major depressive episode (nonpsychotic and nonbipolar, with no history of chronic intermittent depression or dysthymia). Forty-eight subjects were diagnosed with the SADS-L and 32 with the Structured Clinical Interview for DSM-IV (17), which replaced the SADS-L as our primary diagnostic instrument in 1996. The onset of the episode was required to fall in the period between 6 months before the death of the spouse and 12 months after the death. Episodes could be either single or recurrent. No other diagnoses, with the exception of generalized anxiety disorder, panic disorder, and posttraumatic stress disorder, were allowed. Diagnostic reliability was ensured through the use of a structured diagnostic assessment together with independent clinical confirmation by a senior psychiatrist (M.D.M., R.E.P.). A bereavement intensity score of 45 or more on the Texas Revised Inventory of Grief (18) was required as an indication of active grieving. Finally, to be eligible for the study, subjects were required to provide written informed consent. The recruitment, assessment, and treatment protocols were approved by our biomedical institutional review board.
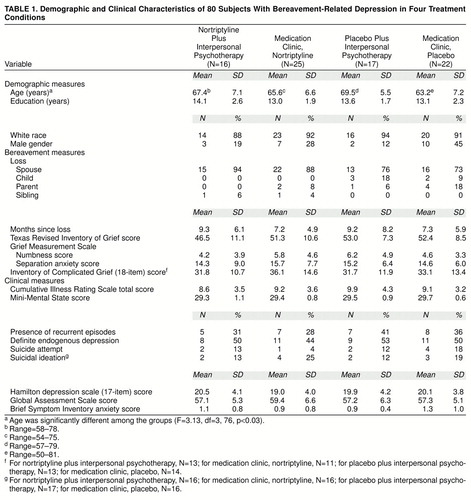
As shown in table 1, subjects were randomly assigned to one of our treatment groups: 1) nortriptyline and interpersonal psychotherapy, 2) nortriptyline in a medication clinic, 3) placebo and interpersonal psychotherapy, or 4) placebo in a medication clinic. Most subjects were white female outpatients with mild to moderate episodes of major depression and some associated functional impairment. Most were in their 60s; however, the group randomly assigned to medication clinic, placebo, was significantly younger than the other groups. About two-thirds of the total study group reported that they were in their first lifetime episode of major depression, and a substantial minority reported either suicidal ideation (17%) or a history of suicide attempts (11%). About one-half the study group met the RDC or DSM-IV criteria for definitely endogenous or melancholic episodes. Typically, subjects had lost a spouse or significant other 7–9 months earlier (median=32 weeks, with no difference between treatment groups). The treatment groups did not differ significantly on measures of bereavement intensity (Texas Revised Inventory of Grief [18], Grief Measurement Scale [(19], [ 20], [ and Inventory of Complicated Grief 21]). There was also no significant difference in depression severity (Hamilton Depression Rating Scale [22]), cognitive impairment (Mini-Mental State [23]), or the Brief Symptom Inventory (24) measure of anxiety. Because the groups differed in age, as noted above, age was used as a covariate in the major outcome analysis. The distribution of all other demographic, bereavement, and clinical measures was equal among the groups.
The numbers of subjects in the four treatment conditions differ because we enlarged the scope of the study from a two-cell design initially (nortriptyline versus placebo) to the current four-cell design 2 years after beginning recruitment. Sixteen subjects were recruited into the original two-cell study and 64 into the four-cell study. Pretreatment Hamilton depression ratings averaged 18 among subjects in the two-cell study and 20 among subjects in the four-cell study (nonsignificant difference). We added a psychotherapy condition because our pilot data had suggested that antidepressant medication did not lessen the intensity of bereavement (25) and because of the clinical need to develop effective interventions for elderly patients who either cannot or will not take antidepressant medication. In this context, we adopted the current 2 × 2 factorial design as a test of both the main effects of the drug and psychotherapy and their hypothesized interaction on the resolution of bereavement-related major depression.
Treatment Design, Rationale, and Integrity
After baseline evaluation, including a 14-day psychotropic-drug-free observation period to ensure stability of symptom severity, patients were randomly assigned to treatment in one of four cells, stratified by the presence of single versus recurrent episodes of major depression: 1) medication clinic, nortriptyline, 2) medication clinic, placebo, 3) interpersonal psychotherapy plus nortriptyline, and 4) interpersonal psychotherapy plus placebo. Both subjects and treating clinicians were kept blind to placebo or nortriptyline assignment. Procedures for the implementation of medication clinic treatment and for interpersonal psychotherapy followed manuals developed by the investigators (available on request from the first author). Nortriptyline and placebo tablets were of identical size (9 mm in diameter), weight (250 mg), and appearance. They were prepared by research pharmacist Dr. Umesh Banakar and certified for content by one of us (J.M.P.) under Food and Drug Administration IND 37603 to J.M.P (sponsor) and to C.F.R. (investigator).
At the time we were developing this study in 1990–1991, we chose nortriptyline for two reasons: 1) our literature review for the Agency on Health Care Policy and Research’s Depression Panel Guideline Report on the treatment of geriatric depression concluded that the then-available database supporting the efficacy of nortriptyline was the best for any antidepressant at that time (26), and 2) our open pilot work with nortriptyline in bereavement-related depression supported its efficacy and safety (25) as well as its favorable side effects profile (27). Similarly, we chose interpersonal psychotherapy because, as originally developed by Klerman et al. (13), it included a specific focus on bereavement. In addition, in our recently completed study of nortriptyline and interpersonal psychotherapy in the maintenance therapies of late-life depression (28), we had found that interpersonal psychotherapy could be combined with a tablet (either placebo or nortriptyline), was “user-friendly” for elderly depressed patients (especially in the hands of experienced therapists), and was clinically relevant to the complex task of helping older patients adjust to the loss of a spouse.
Patients assigned to a medication clinic condition were seen weekly during the acute treatment phase by the same two clinicians, one of whom was a co-investigator psychiatrist (R.E.P.) blind to treatment assignment (nortriptyline or placebo). The same clinicians provided either medication clinic treatment or interpersonal psychotherapy, depending on random assignment. All patients received symptom and side effect evaluations and education about depression as a medical illness. Patients in the medication clinic condition received no specific psychotherapy. The starting dose of nortriptyline was 25 mg h.s. for the first week, increased in 25-mg increments each week thereafter on the basis of clinical and blood level data. Blood samples for ascertaining nortriptyline levels were drawn at each visit, which lasted about 30 minutes weekly. Plasma nortriptyline levels were determined in the laboratory of the psychopharmacologist co-investigator (J.M.P.) with the use of previously published methods of high-performance liquid chromatography (29). All treatment visits, regardless of medication clinic or psychotherapy assignment, included orthostatic pulse and blood pressure readings, weight determination, and clinical evaluations and ratings (Hamilton depression scale, Beck Depression Inventory, Global Assessment Scale [30], and Asberg side effect rating scale [31]). These data were reviewed weekly by a nonblind monitoring committee consisting of the principal investigator (C.F.R.) and a co-investigator (M.D.M.). This committee adjusted the dose of nortriptyline to ensure a steady-state plasma level of at least 50 ng/ml but no more than 120 ng/ml. The measure of grief intensity, the Texas Revised Inventory of Grief, was administered monthly.
For the patients assigned to interpersonal psychotherapy, the treatment was delivered weekly during 50-minute sessions by experienced clinicians (two masters of social work, one master of education, and one doctoral-level clinical psychologist). The psychotherapists were trained to and maintained at research levels of proficiency in interpersonal psychotherapy by two of the co-investigators (E.F. and C.C.). These same clinicians also provided medication clinic treatment to the patients randomly assigned to the medication clinic.
All medication clinic and interpersonal psychotherapy sessions were audiotaped for rating of elements specific to the interpersonal psychotherapy and medication clinic conditions, in order to ensure treatment integrity and compliance with manual-based treatment delivery procedures. In previous analyses of rating scale factor scores (interpersonal psychotherapy or medication clinic), for interpersonal psychotherapy sessions each clinician-therapist demonstrated higher interpersonal psychotherapy factor scores than medication clinic scores. Conversely, for medication clinic sessions, every clinician-therapist demonstrated higher medication clinic factor scores than interpersonal psychotherapy factor scores. In discriminant function analyses using factor scores, we have consistently obtained significant discriminations, with over 80% of interpersonal psychotherapy sessions and medication clinic sessions being accurately classified (32). These data demonstrate that project clinicians were able to deliver interpersonal psychotherapy to bereaved depressed persons in a way that could be discriminated from medication clinic treatment by blind raters. We monitored compliance with pharmacotherapy both behaviorally (e.g., through education of patients and family members, pharmacy pill counts, and weekly reminders and checks) and pharmacologically (e.g., by examination of nortriptyline blood levels over time).
Subjects who achieved remission of symptoms (a 17-item Hamilton depression scale score of 7 or lower for 3 consecutive weeks) entered into continuation therapy (also double-blind) for an additional 16 weeks, to ensure stability of clinical response. Subjects who did not achieve at least a 50% reduction in Hamilton depression score by week 8 of double-blind treatment were deemed to be nonresponders and were treated openly. After continuation treatment, subjects were gradually withdrawn from treatment over 6 weeks and followed up for 2 years, to assess the stability of their response to treatment. We maintain an interrater reliability of no more than 2 points’ difference in total ratings on the Hamilton depression scale.
We used a generalized logit model to test the difference in remission rates between treatment groups (33). Maximum likelihood estimates of the main effect parameters of nortriptyline and interpersonal psychotherapy and of their interaction were derived and tested with Wald chi-square statistics (34). Age was used as a covariate.
RESULTS
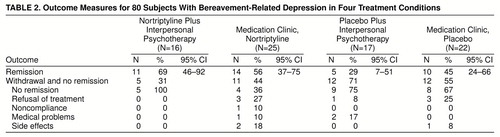
Table 2 shows the rates of remission in the four treatment conditions (intent-to-treat study group), together with 95% confidence intervals and reasons for termination from the study (no remission, treatment refusal, noncompliance, medical problems, and side effects). The overall dichotomous outcome (remission/no remission) linear model with age as a covariate detected a significant drug effect (χ2=4.74, df=1, p<0.03) but no main effect of interpersonal psychotherapy (χ2=0.02, df=1, p=0.89) and no nortriptyline-by-interpersonal psychotherapy interaction (χ2=1.62, df=1, p=0.20). Age was not a significant covariate (χ2=0.01, df=1, p=0.98). Rates of all-cause attrition were lowest (and hence rates of treatment completion were highest) in the combined treatment condition (nortriptyline plus interpersonal psychotherapy) as compared with the other three groups (χ2=4.24, df=1, p=0.04). Results of the major outcome analysis were the same when only subjects who participated in the four-cell study were used. Gender did not influence remission rates across the four treatment groups.
We further tested the hypothesis of an interaction between nortriptyline and interpersonal psychotherapy in two ways. An interaction of drug and psychotherapy could be manifested as an additive effect of using the two treatment modalities together. We detected a small difference in effect size (Cohen’s h=0.27) between the combined treatment condition (nortriptyline plus interpersonal psychotherapy) and the medication clinic, nortriptyline, condition. (This small effect size would require a study group of over 200 to detect a significant benefit of interpersonal psychotherapy in addition to the drug.) An interaction could also be manifested if interpersonal psychotherapy interacts with nortriptyline in a qualitatively different way from its interaction with placebo. In this context, the chi-square test for the two interpersonal psychotherapy groups (interpersonal psychotherapy plus nortriptyline and interpersonal psychotherapy plus placebo) was significant (χ2=5.11, df=1, p=0.02). However, the comparison of remission rates in the combined treatment condition with those in the other three conditions did not produce significant results with either a logit model or chi-square tests.
The rate of relapse into major depression during the 16-week period of continuation therapy was low in all four treatment conditions: none of 11 responders in the nortriptyline plus interpersonal psychotherapy condition, one of 14 in the medication clinic, nortriptyline, condition, one of five in the interpersonal psychotherapy plus placebo condition, and none of 10 in the medication clinic, placebo, condition. We saw no differential effect of treatment on rates of decline in bereavement intensity (Texas Revised Inventory of Grief, Inventory of Complicated Grief). The overall decrease in Texas Revised Inventory of Grief scores was from 50.1 to 38.4 across 16 weeks of treatment.
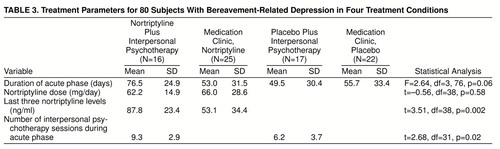
Table 3 summarizes treatment intensity parameters in each of the four treatment conditions. The protocol required the termination of double-blind treatment if patients had failed to show a 50% reduction in Hamilton depression score after 8 weeks in acute treatment, or sooner if the clinician-therapist and blinded psychiatrist were uncomfortable with double-blind treatment (e.g., because of suicidal ideation). Thus, the duration of acute-phase double-blind treatment tended to be shorter in the three monotherapy conditions than in the combined treatment condition. Nortriptyline doses were comparable in the two nortriptyline conditions, although (unintentionally) nortriptyline levels were significantly higher in the nortriptyline plus interpersonal psychotherapy condition. Similarly, patients in the nortriptyline plus interpersonal psychotherapy condition received significantly more interpersonal psychotherapy sessions than their counterparts in the placebo plus interpersonal psychotherapy condition. The shorter duration of double-blind, acute-phase therapy in the interpersonal psychotherapy plus placebo condition reflected the higher rate of failure to improve by at least 50% on Hamilton depression ratings by 8 weeks of treatment, hence the need to break the double blind sooner to be in compliance with protocol and institutional review board requirements.
DISCUSSION
To our knowledge, this trial is the first randomized, double-blind placebo-controlled evaluation of a pharmacotherapy (nortriptyline) and of interpersonal psychotherapy in the acute-phase treatment of bereavement-related major depression. The data confirmed the primary study hypothesis of the superior efficacy of nortriptyline over placebo but failed to show a difference between interpersonal psychotherapy and placebo. With regard to the prediction of a combined or synergistic effect of nortriptyline and interpersonal psychotherapy, the results were mixed. The dichotomous outcome linear model did not detect an interaction. However, a direct pairwise comparison of the two relevant conditions, nortriptyline plus interpersonal psychotherapy and placebo plus interpersonal psychotherapy, did show a significant difference in response rates, providing preliminary support for the hypothesis that interpersonal psychotherapy may interact differently with nortriptyline than with placebo. (An alternative interpretation is that this difference reflects only a drug-placebo difference.) In addition, the use of nortriptyline plus interpersonal psychotherapy was associated with the lowest rate of attrition overall and the highest rate of treatment completion. Our view is that the presence of an active antidepressant medication reduced the burden of depressive symptoms to a greater extent than did placebo, perhaps facilitating engagement in interpersonal psychotherapy and retention in treatment.
Although we failed to detect a main effect of interpersonal psychotherapy, this failure may be the result of the small study group size or an artifact of the protocol requirement to break the double-blind if patients were failing to show improvement by 8 weeks. It is possible that continuing with the double-blind treatment for 16 weeks would have resulted in a confirmation of the hypothesized superiority of interpersonal psychotherapy over placebo. The placebo response rate in this study (45%) is higher than the 13% placebo response rate reported by Georgotas et al.( 35) in their study of nortriptyline and phenelzine for nonbereavement major depression in subjects aged 55 and older. The observation of a 45% placebo response rate could reflect something about bereavement-related depression, including the value of a supportive medication clinic even without a specific psychotherapy. It is perhaps just as likely, however, that the absence of a higher response rate for interpersonal psychotherapy alone reflects the need for a psychotherapy more specific to bereavement and/or the possible advantage of combining interpersonal psychotherapy with an active antidepressant medication. This combination was associated with the highest treatment completion rate of the four treatment conditions observed in the study.
We found no differential effect of any treatment condition on bereavement intensity per se, as measured by scores on the Texas Revised Inventory of Grief and the Inventory of Complicated Grief. Why the symptoms of grief apparently do not resolve with the same clarity as the symptoms of depression is, we believe, an issue of considerable conceptual and theoretical, as well as clinical, importance. The current data support the results of our pilot study (25) and confirm the preliminary work of others (36) in finding differences both in the magnitude of symptom reduction (i.e., much greater for depressive symptoms than for symptoms of bereavement) and in time course (i.e., much slower for bereavement). There are at least two possible explanations for this phenomenon. The first is that depressive symptoms may represent biological dysregulation (e.g., sleep and appetitive disturbances) more amenable to pharmacologic intervention, while persisting grief may represent unresolved problems of loss and difficulty in performing role transition tasks. Psychotherapy may need to be longer and/or more specific to facilitate resolution of grief. A second possibility, however, is that persistence of grief is not necessarily abnormal or pathological. Preoccupation with the memory of the lost spouse might be the normal or necessary sequela of genuine attachment and part of a necessary sustenance of life.
The results of this study support the indication for pharmacologic treatment of major depressive episodes in the wake of a serious life stressor such as bereavement. Relieving the burden of such symptoms may allow bereaved persons to better carry on with the work of grief.
Received May 14, 1998; revision received Aug. 21, 1998; accepted Oct. 2, 1998. From the Mental Health Clinical Research Centers for Late- and Mid-Life Mood Disorders, Department of Psychiatry, University of Pittsburgh Medical Center, Western Psychiatric Institute and Clinic. Address reprint requests to Dr. Reynolds, Western Psychiatric Institute and Clinic, 3811 O’Hara St., Pittsburgh, PA 15213; [email protected] (e-mail). Supported by NIMH grants MH-52247, MH-30915, MH-37869, and MH-00295. The authors thank the study coordinators (Maryann Schlernitzauer, M.S.N., and Jacqueline Stack, M.S.N.) and the clinician-therapists (Lin Eherenpreis, M.S.W., Lee Wolfson, M.Ed., Rebecca Silberman, Ph.D., and Jean Zaltman, M.S.W.) and staff of the Late-Life Depression Clinic of the Department of Psychiatry, University of Pittsburgh Medical Center.
 |
 |
 |
1. Murrell SA, Himmelfarb S: Effects of attachment bereavement and pre-event conditions on subsequent depressive symptoms in older adults. Psychol Aging 1989; 4:166–172Crossref, Medline, Google Scholar
2. Bruce ML, Kim K, Leaf PJ, Jacobs S: Depressive episodes and dysphoria resulting from conjugal bereavement in a prospective community sample. Am J Psychiatry 1990; 147:608–611Link, Google Scholar
3. Clayton PJ, Halikas JA, Mauria WL: The depression of widowhood. Br J Psychiatry 1972; 120:71–78Crossref, Medline, Google Scholar
4. Jacobs SC: Measures of the psychological distress of bereavement, in Biopsychosocial Aspects of Bereavement. Edited by Zisook S. Washington, DC, American Psychiatric Press, 1987, pp 125–138Google Scholar
5. Zisook S, Shuchter SR: Depression through the first year after the death of a spouse. Am J Psychiatry 1991; 148:1346–1352Link, Google Scholar
6. Zisook S: Diagnostic and treatment considerations in depression associated with late-life bereavement, in Diagnosis and Treatment of Depression in Late Life: Results of the NIH Consensus Development Conference. Edited by Schneider LS, Reynolds CF III, Lebowitz BD, Friedhoff AJ. Washington, DC American Psychiatric Press, 1994, pp 419–436Google Scholar
7. Conwell Y: Suicide in the elderly. Ibid, pp 397–418Google Scholar
8. National Center for Health Statistics: Advance Report of Final Mortality Statistics. Washington, DC, National Center for Health Statistics, 1992Google Scholar
9. Jacobs SC, Ostfeld AM: An epidemiological review of the mortality of bereavement. Psychosom Med 1977; 39:344–357Crossref, Medline, Google Scholar
10. Thompson LW: Bereavement and adjustment disorders, in Geriatric Psychiatry. Edited by Busse EW, Blazer DG. Washington, DC, American Psychiatric Press, 1989, pp 459–473Google Scholar
11. Osterweis M, Solomon F, Green M: Bereavement: Reactions, Consequences, and Care. Washington, DC, National Academy Press, 1984Google Scholar
12. National Institutes of Health: NIH consensus conference: diagnosis and treatment of depression in late life. JAMA 1992; 268:1018–1024Crossref, Medline, Google Scholar
13. Klerman GL, Weissman MM, Rounsaville BJ, Chevron E: Interpersonal Psychotherapy of Depression. New York, Academic Press, 1984Google Scholar
14. Schlernitzauer M, Bierhals AJ, Geary MD, Prigerson HG, Stack JA, Miller MD, Pasternak RE, Reynolds CF: Recruitment methods for intervention research in bereavement-related depression: five years’ experience. Am J Geriatr Psychiatry 1998; 6:67–74Medline, Google Scholar
15. Spitzer RL, Endicott J: Schedule for Affective Disorders and Schizophrenia—Lifetime Version, 3rd ed. New York, New York State Psychiatric Institute, Biometrics Research, 1979Google Scholar
16. Feighner JP, Robins E, Guze SB, Woodruff RA Jr, Winokur G, Munoz R: Diagnostic criteria for use in psychiatric research. Arch Gen Psychiatry 1972; 26:57–63Crossref, Medline, Google Scholar
17. First MB, Spitzer RL, Williams JBW, Gibbon M: Structured Clinical Interview for DSM-IV. Washington, DC, American Psychiatric Press, 1995Google Scholar
18. Faschingbauer TR: Texas Revised Inventory of Grief Manual. Houston, Honeycomb Publishing, 1981Google Scholar
19. Jacobs SC, Kasl SV, Ostfeld AM, Berkman L, Charpentier P: The measurement of grief: age and sex variation. Br J Med Psychol 1986; 59:305–310Crossref, Medline, Google Scholar
20. Jacobs SC, Kasl SV, Ostfeld AM, Berkman L, Kosten TR, Charpentier P: The measurement of grief: bereaved vs non-bereaved. Hospice J 1986; 2(4):21–35Google Scholar
21. Prigerson HG: Inventory of Complicated Grief, in Comparative Evaluation of Rating Scales for Clinical Psychopharmacology. Edited by Van Riezen H. Dublin, Elsevier Press, 1996Google Scholar
22. Hamilton M: A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23:56–62Crossref, Medline, Google Scholar
23. Folstein MF, Folstein SE, McHugh PR: “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12:189–198Crossref, Medline, Google Scholar
24. Derogatis LR, Melisaratos N: The Brief Symptom Inventory: an introductory report. Psychol Med 1983; 13:595–605Crossref, Medline, Google Scholar
25. Pasternak R, Reynolds CF, Schlernitzauer M, Hoch CC, Buysse DJ, Houck PR, Perel JM: Acute open-trial nortriptyline therapy of bereavement-related depression in late life. J Clin Psychiatry 1991; 52:307–310Medline, Google Scholar
26. Reynolds CF III, Schneider LS, Lebowitz BD, Kupfer DJ: Treatment of depression in elderly patients: guidelines for primary care, in Diagnosis and Treatment of Depression in Late Life: Results of the NIH Consensus Development Conference. Edited by Schneider LS, Reynolds CF III, Lebowitz BD, Friedhoff AJ. Washington, DC, American Psychiatric Press, 1994, pp 463–490Google Scholar
27. Miller MD, Pollock BG, Rifai AH, Paradis CF, Perel JM, George C, Stack JA, Reynolds CF: Longitudinal analysis of nortriptyline side effects in elderly depressed patients. J Geriatr Psychiatry Neurol 1991; 4:226–230Crossref, Medline, Google Scholar
28. Reynolds CF, Frank E, Perel J, Mazumdar S, Kupfer DJ: Maintenance therapies for late-life recurrent major depression: research and review circa 1996, in Geriatric Psychopharmacology. Edited by Nelson JC. New York, Marcel Dekker, 1998, pp 127–142Google Scholar
29. Foglia JP, Stiller RL, Perel JM: The measurement of plasma nortriptyline and its isomeric 10-OH metabolites (abstract). Clin Chem 1987; 33:1024Google Scholar
30. Endicott J, Spitzer RL, Fleiss JL, Cohen J: The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry 1976; 33:766–771Crossref, Medline, Google Scholar
31. Asberg M: Dose effects of antidepressant medication in different populations. J Affect Disord 1986; suppl 2:S1–S67Google Scholar
32. Wagner EF, Frank E, Steiner SC: Discriminating maintenance treatments for recurrent depression: development and implementation of a rating scale. J Psychother Pract Res 1992; 22:281–291Google Scholar
33. Agresti A: Analysis of Ordinal Categorical Data. New York, John Wiley & Sons, 1984Google Scholar
34. SAS/STAT User"s Guide, version 6, 4th ed. Cary, NC, SAS Institute, 1989Google Scholar
35. Georgotas A, McCue RE, Hapworth W, Friedman E, Kim OH, Welkowitz J, Chang I, Cooper TB: Comparative efficacy and safety of MAOIs vs TCAs in treating depression in the elderly. Biol Psychiatry 1986; 21:1155–1166Crossref, Medline, Google Scholar
36. Jacobs SC, Nelson JC, Zisook S: Treating depression of bereavement with antidepressants: a pilot study. Psychiatr Clin North Am 1987; 10:501–510Crossref, Medline, Google Scholar