Violence and Severe Mental Illness: The Effects of Substance Abuse and Nonadherence to Medication
Abstract
OBJECTIVE: Violent behavior among individuals with severe mental illness has become an important focus in community-based care. This study examines the joint effect of substance abuse and medication noncompliance on the greater risk of serious violence among persons with severe mental illness. METHOD: Involuntarily admitted inpatients with severe mental illness who were awaiting a period of outpatient commitment were enrolled in a longitudinal outcome study. At baseline, 331 subjects underwent an extensive face-to-face interview. Complementary data were gathered by a review of hospital records and a telephone interview with a family member or other informant. These data included subjects' sociodemographic characteristics, illness history, clinical status, medication adherence, substance abuse, insight into illness, and violent behavior during the 4 months that preceded hospitalization. Associations between serious violent acts and a range of individual characteristics and problems were analyzed by using multivariable logistic regression. RESULTS: The combination of medication noncompliance and alcohol or substance abuse problems was significantly associated with serious violent acts in the community, after sociodemographic and clinical characteristics were controlled. CONCLUSIONS: Alcohol or other drug abuse problems combined with poor adherence to medication may signal a higher risk of violent behavior among persons with severe mental illness. Reduction of such risk may require carefully targeted community interventions, including integrated mental health and substance abuse treatment. (Am J Psychiatry 1998; 155:226–231)
Violence committed by individuals with severe mental illness living in the community has become an increasing focus of concern among clinicians, policy makers, and the general public—often as the result of tragic, albeit uncommon events (1–3). In the current era of cost containment, in which the use of hospitalization is increasingly limited, there is a renewed priority on developing strategies for managing violence risk in the community. Such strategies may include formalized risk assessment procedures (4), closer monitoring of outpatient treatment, greater attention to substance abuse comorbidity, and efforts to improve treatment retention and compliance through intensive case management (5). Legal interventions such as court-mandated, community-based treatment or involuntary outpatient commitment are also being cited as promising methods of improving treatment adherence (6–9) and thereby reducing violence (1, 10).
As risk management strategies per se, a number of these approaches are being advocated on the strength of general clinical assumptions about what may cause mentally ill individuals to commit violent acts, but they lack the benefit of a solid research base that demonstrates the specific and interacting effects of major risk factors for violent behavior as they actually operate in the severely mentally ill population. Such effects are shaped not only by the features of major psychiatric disorder but by the social environments in which people with severe mental illness often live. The present article takes a step toward providing a better empirical understanding of violent behavior in individuals with severe mental illness by specifying the magnitude of violence risk represented by two key problems—substance abuse and medication noncompliance—and showing how these risk factors operate together in a group of 331 recently hospitalized severely mentally ill individuals.
A number of studies have linked medication noncompliance to decompensation and hospital readmission. Substance abuse comorbidity has also been associated with generally poor clinical outcomes among severely mentally ill individuals in the community (11–19). Haywood and co-workers (14) found high rates of alcohol or other drug abuse and medication noncompliance among a subgroup of state mental hospital patients who exhibited a pattern of multiple readmissions. Other studies of severely mentally ill individuals in the community have shown that substance abuse comorbidity is associated with medication and aftercare noncompliance (19, 20) as well as with violent behavior (21–25).
A new analysis by Swanson and colleagues (26) suggests that substance abuse, psychotic symptoms, and lack of contact with specialty mental health services in the community all are associated with greater risk of adult-lifetime violence among persons with severe mental illness. In a state forensic hospital population, Smith (27) found a significant relationship between medication noncompliance and violent acts in the community. Similarly, Bartels and colleagues (28) reported a relationship among noncompliance, hostility, and violence in a group of 133 outpatients with schizophrenia. Consistent with the findings of Bartels and colleagues, a new analysis from the same study presented here shows that both violent behavior and the combination of substance use with medication noncompliance are significant statistical predictors of police encounters for people with severe mental illness (29).
Taken together, these findings suggest that medication noncompliance may exert an effect on violence by means of a preexisting or concomitant relationship with alcohol or other drug abuse. Both of these variables—substance abuse and medication nonadherence—may combine to increase the risk of violence, or perhaps a third variable, such as poor insight into illness (30–34), may lead both to substance abuse and noncompliance and thus increase the risk of violence and institutional recidivism.
Lack of awareness of illness and need for treatment—termed poor insight into illness—has been associated with noncompliance, illness relapse, and recidivism (33–35), but systematic research has not linked poor insight with violence per se. For that matter, limited empirical evidence to date has implicated noncompliance as a direct risk factor for violent acts among severely mentally ill individuals or has documented its potential interaction with substance abuse while holding constant demographic and social-contextual variables (10, 11).
Identifying the relative and combined impact of specific risk factors is a necessary first step in designing more effective ways to prevent the violent and threatening behavior that often attends relapse and hospital recidivism in this population. Hence, the current study seeks to examine the effects of selected predictors of recent community violence in a multivariable analysis of 331 hospitalized individuals with severe mental illness.
METHOD
Data for this article are drawn from a randomized clinical trial (8) that examined the effectiveness of involuntary outpatient commitment and case management in reducing noncompliance with psychiatric treatment and preventing relapse, rehospitalization, reduced functioning, and other poor outcomes among people with severe mental illness. Because the present article will include only the baseline data of the 331 severely mentally ill subjects from the longitudinal study, the random assignment of subjects after their baseline interview will not be an issue here; hence, all the baseline data will be analyzed as one study group.
Involuntarily admitted patients were recruited from the admissions unit of a regional state psychiatric hospital and three other inpatient facilities that serve the catchment area in which the participating area mental health programs are located. Because involuntary admission is used extensively in public-sector psychiatric institutions in North Carolina (accounting for about 90% of admissions to the state mental hospitals), patients admitted to inpatient treatment under this status are quite representative of the population of persons with severe and persistent mental disorders—particularly the subgroup of repeatedly admitted (“revolving door”) patients in the public mental health system. Eligible patients were approached for informed consent to participate and included individuals with a primary diagnosis of a severe and persistent psychiatric disorder who were awaiting a period of court-ordered outpatient commitment. Of 374 identified eligible patients, about 11.5% (N=43) refused.
An extensive face-to-face interview was conducted with each respondent and by telephone with a designated family member or other informant who knew the respondent well. Interviews covered a wide variety of personal historical information, sociodemographic and clinical characteristics, and specific information about violent behavior and its surrounding context. In addition, a systematic review of the hospital record was conducted, including clinical assessments, treatment progress notes, and the legal section of the chart in which involuntary commitment petitions and criminal charges were noted.
In the direct interviews, subjects were asked specifically whether they had gotten into trouble with the law or had been arrested for physical or sexual assault. Each respondent was also asked specifically about getting into physical fights in the past 4 months in which someone was “hit, slapped, kicked, grabbed, shoved, bitten, hurt with a knife or gun, or had something thrown at them.” Subjects were also asked a series of questions about engaging in threatening behavior, defined as “saying or doing anything that makes a person afraid of being harmed by you—like saying you are going to hit them, demanding money, raising a fist, pointing a weapon, trying to pick a fight, following or chasing or stalking someone, or anything like that.” Family members or other collateral informants were asked similar questions about the subject's behavior.
For the present study, we used combined data from subjects, family members, and hospital records to adopt a severity threshold for serious violent events that included any assaultive act in which the respondent used a weapon against another person or made a threat with a weapon or that resulted in an injury to another person. This operational definition of serious violent behavior corresponds to level 1 violence as measured specifically in the MacArthur Research Network on Mental Health and the Law (36). A more detailed examination of the prevalence and characteristics of violent events in this study group is in preparation (unpublished 1997 study of J.W. Swanson et al.).
Medication noncompliance was measured by the subject's self-report or the report of a family member or collateral informant. Informants were asked 1) whether there had been prescription medications or shots (for mental or emotional health problems) that the subject was supposed to take but did not, or 2) whether the subject had never or almost never taken the shots or oral medications as prescribed. Insight into illness was assessed with the Insight and Treatment Attitudes Questionnaire (34), an 11-item scale that measures recognition of mental illness and the need for treatment. Low scores on the Insight and Treatment Attitudes Questionnaire have been shown to be predictive of poor treatment compliance and higher rates of hospital readmission (35).
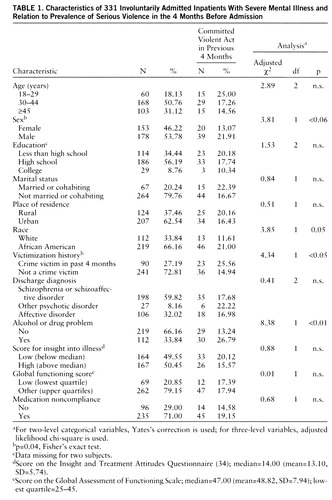
Overall, 17.8% of the study group (N=59) had engaged in serious violent acts that involved weapons or caused injury. Characteristics of the subjects are presented in table 1. Respondents in the group were predominantly male, younger, of lower educational level, and neither married nor cohabiting. The racial distribution of the cohort was about two-thirds African American and one-third white. This racial and sociodemographic composition is quite representative of the severely mentally ill population in these public hospitals and closely matches the sociodemographic composition of study subjects screened for the study. While a majority of respondents were city residents, a substantial proportion lived in rural areas and small towns.
The study group was made up predominantly of persons with psychotic disorders (schizophrenia, schizoaffective disorder, or other psychotic disorders). An additional 26.9% (N=89) had discharge diagnoses of bipolar disorder, and only a small minority—5.1% (N=17)—were diagnosed with major depression. While the current analysis used discharge diagnoses that incorporated chart review data, approximately one-third of the group were administered the Structured Clinical Interview for DSM-III-R (SCID) (37). These interviews showed a very high level of agreement with chart review diagnoses, which used all sources of available data; hence, the SCID assessments were discontinued.
The study interview elicited extensive data on lifetime and recent use of alcohol and illicit substances, including sedatives, cocaine, cannabis, stimulants, opioids, hallucinogens, inhalants, and other substances. It was found that 33.8% of the subjects (N=112) had used at least one type of illicit substance, 53.2% (N=176) had used alcohol, and 58.9% (N=195) had used either (or both) at least once a month during the 4 months before hospitalization. These rates reflect data combined from three sources: respondent's self-report, interview with family members or collateral informants, and hospital record review. In addition, 57.4% (N=112) of the users (33.8% of the total cohort) had “problems” related to alcohol or substance abuse according to one or more sources (e.g., problems with family, friends, job, or police or physical health problems due to drinking) or had a co-occurring diagnosis of substance use disorder at discharge. Since research suggests that use of alcohol or illicit drugs below a diagnostic abuse threshold by persons with major psychiatric disorders can lead to trouble and complicates treatment (16, 38), the present study uses co-occurring alcohol or drug use problems in the previous 4 months as the key severity threshold.
RESULTS
Table 1 shows selected characteristics of study subjects and the percent in each category who committed serious violent acts in the 4 months before admission. In all subsequent analyses, any serious violent act (i.e., assault or threat with a weapon or causing injury to another person) was used as the dependent variable. While most of these sample characteristics showed no significant bivariate relationship to violence, it can be seen that serious violent acts were more likely to be committed by subjects who were male, African American, or victims of crime in the previous 4 months and by those with co-occurring substance abuse problems. We used Fisher's exact test, an appropriate alternative statistic, to demonstrate significance for adjusted chi-square values that were close to significance. Victimization was used in this and subsequent analyses as a proxy contextual measure of exposure to crime and violence in the surrounding social environment (unpublished 1997 study of Hiday et al.), since victimized subjects are likely to feel more threatened and may engage in violent acts at least partly in self-protection. Preliminary data suggested that much of the bivariate association of race and violence could be explained by higher rates of criminal victimization in the particular communities of these African American subjects.
Surprisingly, urban residence in and of itself was not associated with serious violent acts nor was medication noncompliance or low insight into illness, as measured by the Insight and Treatment Attitudes Questionnaire. Also surprising was the lack of relationship of serious violent acts with the clinical characteristics of diagnosis and score on the Global Assessment of Functioning Scale.
Since some bivariate associations with violence were confounded by relationships among predictors, we next conducted multivariable logistic regression analyses that used demographic characteristics, diagnosis, victimization, alcohol or drug problems, insight into illness, and medication noncompliance as predictor variables. The dependent variable in these models was, again, a dichotomous measure of any serious violent acts in the previous 4 months, as determined from any one of three sources of information.
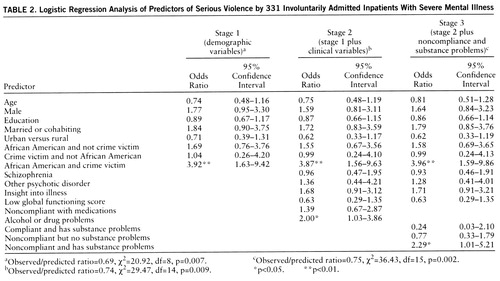
Variables were entered into the regression equations in three stages: 1) demographic variables (age, gender, education, marital status, urban residence, race, and victimization); 2) clinical variables (diagnosis, insight into illness, Global Assessment of Functioning Scale score, medication noncompliance, and alcohol or drug problems); and 3) terms that showed the single and combined effects of noncompliance and substance abuse problems on violence. Results are shown in table 2.
In stage 1, the combination of being African American and a crime victim was the only predictor of violence that emerged as statistically significant. Race and victimization were coded together in the manner shown because race was not of interest as an intrinsic individual risk factor but rather as a social designation that may correlate with environmental precipitants of violence. As shown by Hiday and colleagues (unpublished 1997 study) in related analyses of these data, African Americans were no more likely than whites to commit violent acts unless they also reported recent victimization. Similarly, the current analysis shows that African American crime victims were roughly twice as likely as African American nonvictims to have committed violent acts. Rates of violence among these African American nonvictims were not significantly higher than those of their white counterparts. This suggests that the apparent race effect is largely explained by social-environmental strains.
In stage 2, diagnosis, insight into illness, and noncompliance were not significant as main effects, while patients with substance abuse problems were twice as likely to have engaged in violent behavior. In stage 3, we followed the lead of prior studies, which, taken together, suggested a complex linkage among noncompliance, substance abuse, assaultiveness, and poor clinical outcomes. Specifically, we explored the potential for a combined effect of substance abuse and medication noncompliance on the risk of serious violent acts by creating a new dummy variable for subjects with both substance abuse and noncompliance to compare to subjects without one of these two attributes. It should be noted that these dummy variables are subcategories of subjects with these co-occurring attributes and not interaction terms as are often used in multivariable regression analyses.
These results suggest that the co-occurrence of substance abuse with medication noncompliance may explain much of the observed relationship of comorbidity with violence among the severely mentally ill. Specifically, it can be seen that those respondents with both noncompliance and substance abuse problems were more than twice as likely to commit violent acts, while those individuals with either of these problems alone had no greater risk of violence. Thus, compliant, substance-abusing, or non-substance-abusing and noncompliant severely mentally ill individuals were no more likely to commit violent acts than other individuals in the study.
A final model (not shown here) examined the risk of violence among respondents who, in addition to medication nonadherence and substance abuse, also manifested low insight into illness, as measured by the Insight and Treatment Attitudes Questionnaire score. This analysis also showed a high risk of violence in the group with all three of these risk factors, but the paucity of subjects in certain comparison groups (e.g., subjects with noncompliance, substance abuse, and high insight) makes this model less reliable.
DISCUSSION
In this study we examined a number of risk factors for violent behavior in a study group of recently hospitalized severely mentally ill individuals. In a multivariable model, the combination of substance abuse problems and medication noncompliance was found to be significantly associated with serious violent behavior that occurred in the 4-month period before hospitalization after key sociodemographic and clinical characteristics were controlled. Greater risk for violence was also likely associated with the combination of substance problems, medication noncompliance, and low levels of insight into illness, but we have less confidence in results that incorporate insight because low insight was highly correlated with these other variables.
Among the sociodemographic variables examined, only the combined effect of being victimized and African American was significant, while urban residence was not. One way to interpret this result is that the living environments in which many severely mentally ill African Americans find themselves—high-crime areas experienced as dangerous and threatening—explains much of the violence risk that might otherwise be statistically attributable to race per se.
These findings suggest generally that substance abuse problems, medication noncompliance, and low insight into illness operate together to increase violence risk. However, the study is limited in several ways. In these cross-sectional, retrospective analyses, the sequencing of pathways to violence among these risk factors is not possible. Future analyses will examine such causal relationships and pathways by using longitudinal data currently being collected in this study.
The findings presented here may not be generalizable to all persons with severe mental illness. Subjects in this study were involuntarily admitted and outpatient committed patients—individuals who exhibited “dangerous” or “gravely disabled” behavior and who were also judged to be at risk for poor outcomes in community treatment. However, while the subjects were arguably more severely impaired than many severely mentally ill patients, there is nothing to suggest that the relationship between violence and the predictors shown here would be different for less severely ill individuals. For example, controlling for level of functional impairment did not change these relationships.
Various interpretations of our findings are plausible. Noncompliance and substance abuse may be mutually reinforcing problems in that substance impairment may impede medication adherence while noncompliance, in turn, may lead to self-medicating with alcohol or illicit drugs (39). However, it is also possible that both variables—noncompliance and substance abuse—result from some other latent factor such as general disaffiliation from treatment or unspecified personality traits, although we have no evidence of these factors at present. We did not administer a personality inventory, which is another limitation to this study.
In sum, these findings shed light on a particular set of problems experienced by persons with severe mental disorders—specifically those who may fall into a self-perpetuating cycle of resistance to treatment, illness exacerbation, substance abuse, violent behavior, and institutional recidivism (1, 2, 19, 40). Adverse side effects and complicated dosing regimens can make it especially difficult for patients to take neuroleptic medications as prescribed. In turn, untreated psychopathology and distress may lead to alcohol and other drug abuse (39). Risk of violence may then increase as well because of substance use, exacerbation of psychiatric symptoms, or the influence of criminal environments in which illicit drugs are procured. Finally, violent behavior may further erode supportive social and therapeutic relationships and may precipitate involuntary commitment or incarceration (29). As these problems compound one another, conventional separate-track mental health and substance abuse treatment is unlikely to succeed (19, 20, 26).
Our data also suggest that effective community treatment for this population requires careful attention to medication adherence and the availability of integrated substance abuse and mental health treatment (16, 19). Specialized outpatient services focused on people with dually diagnosed severe mental illness are in short supply in many publicly funded mental health systems but may be crucial for effective management of violence risk in the era of cost containment.
 |
 |
Received March 11, 1997; revision received May 27, 1997; acc epted Aug. 29, 1997. From the Services Effectiveness Research Pr ogram, Department of Psychiatry and Behavioral Sciences, Duke University Medical Center, and the Department of Sociology and Anthropology, North Carolina State University, Raleigh. Address reprint requests to Dr. Swartz, Box 3173, Duke University Medical Center, Durham, NC 27710. Supported by NIMH grant MH-48103 and by the University of North Carolina-Chapel Hill/Duke Program on Services Research for People with Severe Mental Disorders (NIMH grant MH-51410).
1. Torrey EF: Violent behavior by individuals with serious mental illness. Hosp Community Psychiatry 1994; 45:653–662Abstract, Google Scholar
2. Mulvey EV: Assessing the evidence of a link between mental illness and violence. Hosp Community Psychiatry 1994; 45:663–668Abstract, Google Scholar
3. Monahan J, Steadman HJ (eds): Violence and Mental Disorder: Developments in Risk Assessment. Chicago, University of Chicago Press, 1994Google Scholar
4. Borum R, Swartz MS, Swanson JW: Assessing and managing violence risk in clinical practice. J Practical Psychiatry and Behavioral Health 1996; 2:205–215Crossref, Google Scholar
5. Dvoskin JA, Steadman HJ: Using intensive case management to reduce violence by mentally ill persons in the community. Hosp Community Psychiatry 1994; 45:679–684; correction, 45:1004Google Scholar
6. Geller JL: Clinical guidelines for the use of involuntary outpatient treatment. Hosp Community Psychiatry 1990; 41:749–755Abstract, Google Scholar
7. Hiday VA, Scheid-Cook TL: Outpatient commitment for “revolving door” patients: compliance and treatment. J Nerv Ment Dis 1991; 179:83–88Crossref, Medline, Google Scholar
8. Swartz MS, Burns BJ, Hiday VA, George LK, Swanson JW, Wagner HR: New directions in research on involuntary outpatient commitment. Psychiatr Serv 1995; 46:381–385Link, Google Scholar
9. Swanson JW, Swartz MS, George LK, Burns BJ, Hiday VA, Borum R, Wagner HR: Interpreting the effectiveness of involuntary outpatient commitment: a conceptual model. J Am Acad Psychiatry Law 1997; 25:5–16Crossref, Medline, Google Scholar
10. Buchanan A, David A: Compliance and the reduction of dangerousness. J Ment Health 1994; 3:427–429Crossref, Google Scholar
11. Pristach CA, Smith CM: Medication compliance and substance abuse among schizophrenic patients. Hosp Community Psychiatry 1990; 41:1345–1348Google Scholar
12. Casper ES, Regan JR: Reasons for admission among six profile subgroups of recidivists of inpatient services. Can J Psychiatry 1993; 38:657–661Crossref, Medline, Google Scholar
13. Drake RE, Wallach MA, Teague GB, Freeman DH, Paskus TS, Clark TA: Housing instability and homelessness among rural schizophrenic patients. Am J Psychiatry 1991; 148:330–336Link, Google Scholar
14. Haywood TW, Kravitz HM, Grossman LS, Cavanaugh JL Jr, Davis JM, Lewis DA: Predicting the “revolving door” phenomenon among patients with schizophrenic, schizoaffective, and affective disorders. Am J Psychiatry 1995; 152:856–861Link, Google Scholar
15. Bartels SJ, Drake RE, Wallach MA: Long-term course of substance use disorders among patients with severe mental illness. Psychiatr Serv 1995; 46:248–251Link, Google Scholar
16. Drake RE, Bartels SJ, Teague GB, Noordsy DL, Clark RE: Treatment of substance abuse in severely mentally ill patients. J Nerv Ment Dis 1993; 181:606–611Crossref, Medline, Google Scholar
17. Bartels SJ, Teague GB, Drake RE, Clark RE, Bush PW, Noordsy DL: Substance abuse in schizophrenia: service utilization and costs. J Nerv Ment Dis 1993; 181:227–232Crossref, Medline, Google Scholar
18. Drake RE, Wallach MA: Mental patients' attraction to the hospital: correlates of living preference. Community Ment Health J 1992; 28:5–12Crossref, Medline, Google Scholar
19. Osher FC, Drake RE: Reversing a history of unmet needs: approaches to care for persons with co-occurring addictive and mental disorders. Am J Orthopsychiatry 1996; 66:4–11Crossref, Medline, Google Scholar
20. Owen RR, Fischer EP, Booth BB, Cuffel BJ: Medication noncompliance and substance abuse among patients with schizophrenia. Psychiatr Serv 1996; 47:853–858Link, Google Scholar
21. Swanson JW: Mental disorder, substance abuse, and community violence: an epidemiological approach, in Violence and Mental Disorder: Developments in Risk Assessment. Edited by Monahan J, Steadman HJ. Chicago, University of Chicago Press, 1994, pp 101–136Google Scholar
22. Swanson JW, Borum R, Swartz MS, Monahan J: Psychotic symptoms and disorders and the risk of violent behavior in the community. Criminal Behavior and Ment Health 1996; 6:309–329Crossref, Google Scholar
23. Smith J, Hucker S: Schizophrenia and substance abuse. Br J Psychiatry 1994; 165:13–21Crossref, Medline, Google Scholar
24. Salloum IM, Daley DC, Cornelius JR, Kirisci L, Thase ME: Disproportionate lethality in psychiatric patients with concurrent alcohol and cocaine abuse. Am J Psychiatry 1996; 153:953–955Link, Google Scholar
25. Cuffel BJ, Shumway M, Chouljian TL, Macdonald T: A longitudinal study of substance use and community violence in schizophrenia. J Nerv Ment Dis 1994; 182:704–708Crossref, Medline, Google Scholar
26. Swanson JW, Estroff SE, Swartz MS, Borum R, Lachicotte W, Zimmer C, Wagner HR: Violence and severe mental disorder in clinical and community populations: the effects of psychotic symptoms, comorbidity, and lack of treatment. Psychiatry 1997; 60:1–22Crossref, Medline, Google Scholar
27. Smith LD: Medication refusal and the rehospitalized mentally ill inmate. Hosp Community Psychiatry 1989; 40:491–496Abstract, Google Scholar
28. Bartels SJ, Drake RE, Wallach MA, Freeman DH: Characteristic hostility in schizophrenic outpatients. Schizophr Bull 1991; 17:163–171Crossref, Medline, Google Scholar
29. Borum R, Swanson JW, Swartz MS, Hiday VA: Substance abuse, violent behavior and police encounters among persons with severe mental disorders. J Contemporary Criminal Justice 1997; 13:236–249Crossref, Google Scholar
30. Amador XF, Strauss DH, Yale SA, Flaum MM, Endicott J, Gorman JM: Assessment of insight in psychosis. Am J Psychiatry 1993; 150:873–879Link, Google Scholar
31. David AS: Insight and psychosis. Br J Psychiatry 1990; 156:798–808Crossref, Medline, Google Scholar
32. Markova IS, Berrios GE: Insight in clinical psychiatry revisited. Compr Psychiatry 1995; 36:367–376Crossref, Medline, Google Scholar
33. McEvoy JP, Appelbaum PS, Apperson LJ, Geller JL, Freter S: Why must some schizophrenic patients be involuntarily committed? the role of insight. Compr Psychiatry 1989; 30:13–17Crossref, Medline, Google Scholar
34. McEvoy JP, Apperson LJ, Appelbaum PS, Ortlip P, Brecosky J, Hammill K, Geller JL, Roth LH: Insight in schizophrenia: its relationship to acute psychopathology. J Nerv Ment Dis 1989; 177:43–47Crossref, Medline, Google Scholar
35. McEvoy JP, Freter S, Everett G, Geller JL, Appelbaum PS, Apperson LJ, Roth LH: Insight and the clinical outcome of schizophrenic patients. J Nerv Ment Dis 1989; 177:48–51Crossref, Medline, Google Scholar
36. Steadman HJ, Monahan J, Appelbaum PS, Grisso T, Mulvey EP, Roth LH, Robbins PC, Klassen D: Designing a new generation of risk assessment research, in Violence and Mental Disorder: Developments in Risk Assessment. Edited by Monahan J, Steadman HJ. Chicago, University of Chicago Press, 1994, pp 287–318Google Scholar
37. Spitzer RL, Williams JBW, Gibbon M, First MB: User's Guide for the Structured Clinical Interview for DSM-III-R (SCID). Washington, DC, American Psychiatric Press, 1990Google Scholar
38. Drake RE, Alterman AI, Rosenberg SR: Detection of substance use disorders in severely mentally ill patients. Community Ment Health J 1993; 29:175–192Crossref, Medline, Google Scholar
39. Pristach CA, Smith CM: Self-reported effects of alcohol use on symptoms of schizophrenia. Psychiatr Serv 1996; 47:421–423Link, Google Scholar
40. Hiday VA: The social context of mental illness and violence. J Health Soc Behav 1995; 36:122–137Crossref, Medline, Google Scholar



