Depression Among Cocaine Abusers in Treatment: Relation to Cocaine and Alcohol Use and Treatment Outcome
Abstract
OBJECTIVE: The authors investigated the theoretical and clinical role of depression among cocaine abusers in treatment. METHOD: Eighty-nine cocaine-abusing patients underwent 2 weeks of substance abuse treatment. Posttreatment major depressive disorder, depressive symptoms before and after substance abuse treatment, and alcohol diagnoses were assessed and their relation to pretreatment substance use, cravings in high-risk situations, and 3-month follow-up status was examined. RESULTS: High rates of major depressive disorder were found but were unrelated to pretreatment substance use. The decrease in depressive symptoms during treatment was independent of major depressive disorder or alcohol diagnoses and predicted treatment attrition. Higher levels of depressive symptoms during treatment were associated with greater urge to use cocaine, alcohol, and other drugs in high-risk situations. Concurrent major depressive disorder and depressive symptoms did not predict cocaine use at follow-up. However, patients who had an alcohol relapse episode experienced more depressive symptoms during treatment than did those who abstained. CONCLUSIONS: The results highlight the relationship of depression to alcohol use among cocaine abusers and suggest a need for further studies of the association between depression and substance use disorders. (Am J Psychiatry 1998; 155:220–225)
The prevalence of psychiatric symptoms among individuals who seek treatment for alcohol and drug dependence creates significant diagnostic and treatment planning difficulties (1). Greater attention has been afforded to the prevalence and features of psychiatric symptoms among individuals who seek treatment for cocaine abuse (2–4). Of particular importance are the extent of depressive disorders and symptoms, changes in depressive symptoms with abstinence, and the influence of these variables on length of stay, course, and outcome.
Investigations of psychiatric comorbidity among cocaine abusers have indicated high levels of psychopathology, particularly for depressive disorders (5). Lifetime prevalences of DSM-III-R depressive disorders among cocaine abusers in treatment range from about 20% to 47% (5–7), and 28%–53% of cocaine abusers are diagnosed with concurrent major depressive disorders (6, 8). Depressive disorders have been the most commonly diagnosed comorbid condition among cocaine abusers.
The effects of short- and longer-term cocaine abstinence on depressive symptoms are also of interest. Indeed, one difficulty in assessing concurrent depression among cocaine abusers results from the greater depressive symptoms that are apparent in the first 3–5 days after cessation of cocaine use (the “crash”) (2). Furthermore, since 27%–75% of cocaine abusers in treatment may also meet criteria for current alcohol abuse or dependence (9; unpublished 1993 paper of D.J. Rohsenow et al.), chronic or recent alcohol use may also contribute to the initial elevations in depressive symptoms. Crash or withdrawal-induced elevations in depressive symptoms can create difficulty in accurately diagnosing current or lifetime depressive disorders among substance abusers during this time, so it may be preferable to postpone diagnosing major depressive disorder until after these symptoms have abated (1, 10, 11).
Elevated depressive symptoms due to the crash period, excessive alcohol use, or crises that led to admission would likely decrease during the first few weeks of cessation and stabilize with continued abstinence. Consistent with this hypothesis, cocaine abusers have shown significant decreases in depressive symptoms over 4-week and 12-week courses of treatment (4, 7). This depressive symptom improvement may be rapid—substantially decreasing during the first week and stabilizing during the next 3 weeks of treatment (12). Alcoholic inpatients also have shown a significant decrease in levels of depression during the first 3 weeks after treatment entry (1, 13); this decrease was greater for those with either secondary depression or no depression diagnosis than for those with primary major depressive disorder (1). Thus, the role of major depressive disorder in depressive symptom change among cocaine abusers needs to be studied. Furthermore, given the co-occurrence of alcohol abuse and depression (14), the role of alcohol abuse in the changes in depressive symptoms of cocaine abusers also bears investigation. In particular, it would be useful to determine whether concurrent alcohol abuse or dependence influences the course of change in depressive symptoms in cocaine abusers during treatment.
The role of cravings or urges to use has been of increasing interest among researchers. Urges to drink have been found to be elevated among alcoholics who report more depressive symptoms (15). Furthermore, urges to drink and urges to use cocaine in simulated high-risk situations predicted 6-month drinking outcomes of alcoholics (16) and 3-month cocaine use outcomes of cocaine abusers (unpublished 1997 paper of P.M. Monti et al.), respectively. The relationship in cocaine abusers between major depressive disorder or depressive symptoms and urges to use cocaine and other drugs in simulated high-risk situations would therefore be of interest.
The extent to which major depressive disorder affects cocaine use after treatment may have important treatment implications. For example, among cocaine abusers given placebo, the six with secondary depression diagnoses had poorer treatment retention and reduced their cocaine use less than did the 25 patients with no depression diagnosis (17). However, the small study size precludes firm conclusions. On the other hand, among 139 outpatient cocaine abusers, those with lifetime affective disorder (20% of the group) had significantly longer periods of continuous abstinence than those without such a history (7). A third study found no significant relationship between depressive symptoms and cocaine use outcomes (18). Although antidepressant medications sometimes result in reductions in cocaine use (7), no consistent beneficial results have been seen across controlled trials (unpublished 1993 paper of J. Grabowski and B. Johnson). Furthermore, antidepressants were no more effective for cocaine abusers with affective disorder than for those without it (7). Thus, existing data yield discrepant findings with regard to the influence of depression on treatment course. Since concurrent alcohol diagnoses sometimes result in poorer outcomes for cocaine abusers (19), and depression among alcoholics is associated with poorer outcomes (20), the role that alcohol diagnoses play in the effects of depression on outcome for cocaine abusers needs to be investigated.
In summary, available research on comorbid depression among cocaine abusers suggests that 1) a high prevalence of co-occurring depressive symptoms and diagnoses exists, 2) initially elevated depressive symptoms abate considerably with abstinence, 3) limited evidence exists regarding the influence of depressive symptoms on treatment course and outcome, and 4) concurrent alcohol abuse or dependence may affect any of these relationships but has rarely been investigated. Additional studies are needed to provide clearer evidence regarding the role of depression in treatment outcomes for both cocaine and alcohol use among cocaine abusers.
The current study was designed to investigate several questions related to the comorbidity of depression with alcohol and cocaine use and relapse among cocaine abusers. First, we expected that high levels of depressive symptoms would be related to pretreatment levels of alcohol and cocaine use and to the presence of an alcohol abuse or dependence diagnosis. Second, we expected that level of depressive symptoms would be positively associated with potential relapse risk in terms of urge to use drugs or alcohol in an assessment of reactions to simulated high-risk situations. (Following the recommendations of Kozlowski and Wilkinson [21], the term “urge” will be used instead of “craving” to reflect the full continuum of desire to use, rather than only extreme desire to use.) Third, we predicted that depressive symptoms would decrease significantly during the course of treatment and that this decrease would be greater for those with comorbid alcohol diagnoses and for those without a major depressive disorder diagnosis. Fourth, we hypothesized that higher levels of pretreatment depressive symptoms would be associated with treatment attrition. Finally, we expected that level of depressive symptoms and a diagnosis of major depressive disorder would predict relapse episodes and the extent of subsequent use of both alcohol and cocaine.
METHOD
Subjects
The 89 participants were drawn from a cocaine abuse treatment outcome study described elsewhere (10; unpublished 1997 paper of P.M. Monti et al.). Patients were recruited from two private substance abuse treatment programs—a rural residential substance abuse facility (N=57) and an urban partial-hospital substance abuse program at a psychiatric hospital (N=32)—that combined a 12-step model with a psychosocial learning-based model. Participants were not actively psychotic and met criteria for cocaine abuse (N=1) or dependence (N=88) according to the Structured Clinical Interview for DSM-III-R—Patient Version (SCID-P) (22). Of 63 patients administered the SCID-P alcohol diagnosis section, 69.8% (N=44) also had concomitant alcohol abuse or dependence diagnoses. The mean age of the study group was 28.6 years (SD=6.7, range=18–53), 73.0% (N=65) were male, 58.4% (N=52) were employed, 50.6% (N=45) were married or cohabiting, 87.6% (N=78) were Caucasian, 6.7% (N=6) were black, and 3.4% (N=3) were Hispanic. After complete description of the study, written informed consent was obtained.
Procedures and Instruments
In-person assessments were conducted at pretreatment (after detoxification if needed), posttreatment, and 1 and 3 months after discharge. Pretreatment assessment was completed over 3 days within a mean of 5.6 days (SD=3.8) after admission, an average of 12.4 days (SD=19.1) after last cocaine use, and an average of 6.1 days (SD=4.9) after the last use of alcohol. The mean interval between pre- and posttreatment assessment was 12.2 days (SD=6.4).
Quantity and frequency of alcohol use and frequency of cocaine use were assessed with the Time Line Follow Back interview (23). The pretreatment interview covered the 180 days before admission; at the 1- and 3-month follow-up assessments, the interview covered the previous 30 and 60 days, respectively. Confidentiality of information was assured, and breath analyzer tests were used to ensure a zero blood alcohol level at time of interview. Urine drug screens (which used the enzyme-multiplied immunoassay technique, with confirmation by gas chromatography and mass spectrometry) and reports from collateral informants were obtained at the 1-month and 3-month interviews for confirmation. The Addiction Severity Index (24), administered at pretreatment, provided alcohol and drug use composite scores. The Cocaine Specific Skills Test (unpublished 1993 paper of D.J. Rohsenow et al.) was administered at posttreatment (N=83) to assess urge to use and self-efficacy in eight simulated high-risk situations for cocaine use. Each situation was presented by audiotape, with participants rating their urge to use and self-efficacy on 7-point Likert scales. Ratings of urge to use cocaine, alcohol, and other drugs will be used in this study. The internal consistency of the urge scales is high (unpublished 1997 paper of P.M. Monti et al.).
The SCID-P mood disorders and substance abuse sections were administered to provide alcohol, cocaine, and current major depressive disorder diagnostic information and age at onset of these disorders. When the SCID-P major depressive disorder section was administered, the criteria for determining organicity were modified such that nonprescribed substance use (including alcohol) was not considered to be organic (2). Since the SCID-P alcohol diagnosis section was added to the study assessment battery after the study was underway, it was administered to a subset of 70.8% (N=63) of the patients at pretreatment. The SCID-P mood disorders section was administered at posttreatment to minimize any effects of withdrawal on the diagnosis of current depression. Because the SCID-P was added to the protocol after the study was underway and because of early discharges, 82.0% (N=73) of the patients were administered the SCID-P mood disorders section. The Modified Hamilton Rating Scale for Depression (25), a 25-item assessment of depressive symptom severity that has demonstrated validity, was administered at pretreatment (N=89) and posttreatment (N=77).
RESULTS
Research interviewers were trained to a criterion of 80% agreement on the modified Hamilton depression scale and SCID-P, after which interrater reliability was assessed on 25% of the modified Hamilton depression scale and 50% of the SCID-P major depressive disorder interviews. Research interviewers had 100% agreement for diagnosis of current major depressive disorder. Interrater agreement for the modified Hamilton depression scale assessed by the intraclass correlation coefficient (ICC) was high (ICC=0.94).
Age, education, Addiction Severity Index drug and alcohol composite scores, percentage of cocaine use days, gender, race, posttreatment modified Hamilton depression scale scores, and diagnosis of current major depressive disorder were compared by treatment setting by using t tests for continuous variables and chi-square tests for categorical variables. Subject characteristics did not differ significantly by site for any of these variables except years of education (t=2.60, df=87, p<0.05) and Addiction Severity Index drug composite score (t=2.67, df=87, p<0.05). Years of education completed was lower for patients at the rural (mean=11.7, SD=1.8) than at the urban (mean=12.8, SD=2.2) facility. Addiction Severity Index drug scores were higher for patients at the rural (mean=0.28, SD=0.11) than at the urban (mean=0.21, SD=0.10) facility.
The number of subjects included in each analysis varied depending on the variables investigated (see assessment descriptions for clarification). The various subsamples were compared to subjects not in the analyses by using t tests and chi-square tests for age, education, Addiction Severity Index drug and alcohol composite scores, percentage of cocaine use days, gender, and race. For each analysis, there were no differences between patients included in the analysis and patients not included because of missing data.
Time Line Follow Back data collected at the 1-month and 3-month follow-up interviews were combined to provide 90 days of information and then compared to urine drug screen reports. Of the participants who reported complete abstinence, 7.3% (N=3) had cocaine-positive urine results. These patients were recoded as having used cocaine, and their number of cocaine use days during follow-up was estimated from baseline by using regression estimation procedures (3.4% of the total study group).
Of the 73 patients administered the SCID-P mood disorders section, 43.8% (N=32) met criteria for current major depressive disorder, and 50.7% (N=37) met criteria for lifetime major depressive disorder. Average age at onset of the first major depressive episode was 22.0 years (SD=5.9). The mean number of SCID-P current depressive symptoms endorsed was 4.0 (SD=3.5), and the mean number endorsed by those with a current major depressive disorder was 7.3 (SD=1.2). Mean score on the modified Hamilton depression scale was 20.2 (SD=10.0) at pretreatment (indicative of moderate depression), and 14.0 (SD=9.3) at posttreatment (indicative of mild depression).
The relation of current major depressive disorder and posttreatment scores on the modified Hamilton depression scale to other demographic variables was examined by using t tests, chi-square analyses, and correlation coefficients where appropriate. Major depressive disorder was not significantly related to age, ethnicity, education, marital status, or employment status, but more patients in the currently depressed group (37.5%, N=12) than in the nondepressed group (17.1%, N=7) were female (χ2=3.89, df=1, p<0.05). Posttreatment scores on the modified Hamilton depression scale were not significantly related to any demographic variable.
Since depression diagnosis differed by gender, possible confounds of gender with other demographic and cocaine use history indicators were explored. Men and women were not significantly different in age, education, marital status, employment, Addiction Severity Index drug and alcohol composite scores, SCID-P alcohol diagnosis, percentage of pretreatment cocaine use days, and race.
The substance use variables investigated included age at onset of cocaine abuse or dependence from the SCID-P, number of pretreatment cocaine use days from the Time Line Follow Back interview, and the following Addiction Severity Index measures: age at first cocaine use, number of years of using cocaine, and Addiction Severity Index drug composite score. Neither current major depressive disorder diagnosis nor posttreatment score on the modified Hamilton depression scale was significantly related to any of these pretreatment measures; t tests and correlation coefficients were used where appropriate.
The relation of number of pretreatment alcohol use days from the Time Line Follow Back interview and the Addiction Severity Index alcohol composite score to depression was assessed with t tests for major depressive disorder diagnosis and correlation coefficients for posttreatment scores on the modified Hamilton depression scale. None of the relationships was significant except that those subjects with higher alcohol composite scores showed higher posttreatment scores on the modified Hamilton depression scale (r=0.26, N=77, p<0.05).
Patients with alcohol abuse or dependence diagnoses were compared to those without a concurrent alcohol diagnosis for current major depressive disorder diagnosis and posttreatment score on the modified Hamilton depression scale. Alcohol diagnosis was not significantly related to either variable according to t test and chi-square analyses.
The relation of major depressive disorder and posttreatment score on the modified Hamilton depression scale to posttreatment urges to use cocaine, alcohol, and other drugs examined in the Cocaine Specific Skills Test was assessed. None of the t tests with major depressive disorder was significant. Higher scores on the modified Hamilton depression scale were related to greater urges to use cocaine (r=0.38, N=77, p<0.001), alcohol (r=0.30, N=77, p<0.001), and other drugs (r=0.22, N=77, p<0.05).
A 2×2 mixed between-group and repeated measures analysis of variance (ANOVA) was conducted for 65 subjects that compared pretreatment and posttreatment scores on the modified Hamilton depression scale for patients with and without major depressive disorder. Significant main effects were found for time (F=39.68, df=1,63, p<0.001) and for major depressive disorder diagnosis (F=10.81, df=1,63, p<0.01). Pretreatment scores (mean=19.8, SD=10.2) were higher than posttreatment scores (mean=13.4, SD=9.0). Scores were also higher for those with a major depressive disorder diagnosis than for those without major depressive disorder. The interaction was not significant. To compare these results with those of Brown et al. (1), we coded the patients as having a diagnosis of primary, secondary, or no current depression in relation to cocaine dependence on the basis of symptom chronology for each disorder. Only 64 patients were coded because some patients were missing data on age at onset of current major depression. Eight (12.5%) of the patients whose onset of current depression occurred before the onset of cocaine disorder were coded as having primary depression. Fifteen (23.4%) of the patients whose onset of current depression occurred after the onset of cocaine disorder were coded as having secondary depression. Forty-one (64%) had no current depression diagnosis. A 2×3 mixed between-group and repeated measures ANOVA was conducted that compared pretreatment and posttreatment scores on the modified Hamilton depression scale among the primary, secondary, and no depression groups. Significant main effects were found for time (F=16.36, df=1,53, p<0.01) and for depression diagnosis (F=4.35, df=2,53, p<0.05). The interaction was not significant. Higher mean scores on the modified Hamilton depression scale were seen in the patients with a diagnosis of secondary depression (mean=20.19, SD=8.47) than in those diagnosed with primary depression (mean=18.58, SD=12.24) or no depression (mean=14.09, SD=7.57) (p<0.05, Student Newman-Keuls follow-up tests).
A 2×2 mixed between-group and repeated measures ANOVA was conducted that compared pretreatment and posttreatment scores on the modified Hamilton depression scale for patients with alcohol abuse or dependence and those without an alcohol diagnosis. The main and interaction effects were not significant.
The relation of initial depressive symptom severity to treatment attrition was investigated by correlating pretreatment scores on the modified Hamilton depression scale to number of days in treatment. Pretreatment number of days of cocaine use and alcohol use were also correlated to number of days in treatment as possible confounds. Length of stay was not significantly correlated with pretreatment use of cocaine (r=0.02, N=101) or alcohol (r=–0.02, N=100) but was significantly correlated with pretreatment score on the modified Hamilton depression scale (r=–0.19, N=102, p<0.05). Patients with more depressive symptoms left treatment earlier.
Forty of 78 patients (51.3%) reported cocaine use during the follow-up period or were coded as having used cocaine because of discrepant urine drug screen results. Thirty-two patients (41.0%) used alcohol during the follow-up period. In chi-square analysis, cocaine relapse status and alcohol relapse status were significantly related (χ2=19.51, df=1, p<0.001). The patients experienced relapse episodes that involved both alcohol and cocaine (33.3%, N=26), alcohol only (7.6%, N=6), or cocaine only (17.9%, N=14); 41.0% (N=32) remained abstinent.
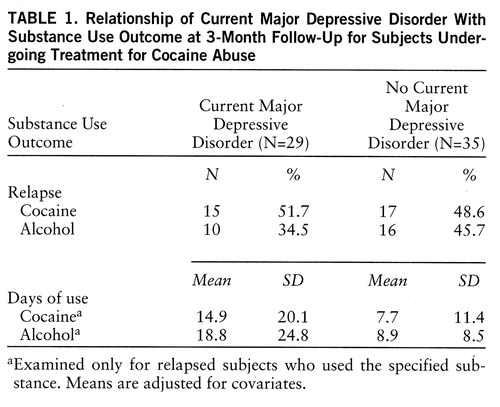
Current major depressive disorder diagnosis was not significantly related to cocaine relapse status in a 2×2 chi-square analysis (table 1). Number of cocaine use days during follow-up was log transformed and abstainers eliminated to correct skewness (>2.0). Analysis of covariance (ANCOVA) revealed that major depressive disorder diagnosis was not significantly related to number of cocaine use days among cocaine relapsers during follow-up after we controlled for pretreatment cocaine use days (table 1 shows adjusted means).
A 2×2 mixed between-group and repeated measures ANCOVA that controlled for pretreatment cocaine use showed that pretreatment and posttreatment scores on the modified Hamilton depression scale were not significantly related to cocaine use status at follow-up in either main or interaction effects. The number of cocaine use days during follow-up was not significantly related to pretreatment or posttreatment scores on the modified Hamilton depression scale according to partial correlations that controlled for pretreatment cocaine use days (table 1 shows adjusted means).
Among patients who drank at all during the follow-up period, 38.5% (N=10) had a current major depressive disorder diagnosis at posttreatment. In a 2ö 2 chi-square analysis, current major depressive disorder diagnosis was not significantly related to alcohol relapse status. Number of drinking days was log transformed and abstaining patients were eliminated to correct skewness. An ANCOVA that controlled for pretreatment alcohol use days indicated that major depressive disorder diagnosis was not significantly related to number of drinking days.
Pretreatment and posttreatment scores on the modified Hamilton depression scale were investigated as predictors of alcohol relapse status at follow-up by using a 2×2 mixed between-group and repeated measures ANCOVA that controlled for pretreatment alcohol use (N=59). A significant main effect was found for alcohol relapse status (F=4.48, df=1,56, p<0.05), with those who relapsed experiencing greater depressive symptoms during treatment (mean=19.8, SD=10.1) than those who abstained (mean=15.5, SD=8.65). The interaction was not significant. Partial correlations that controlled for pretreatment alcohol use days among those with any alcohol use showed that number of drinking days during follow-up was not significantly related to pretreatment or posttreatment scores on the modified Hamilton depression scale.
DISCUSSION
As seen in previous studies (4), cocaine abusers in treatment had high rates of current and lifetime major depressive disorder, and depressive symptoms decreased significantly during treatment. This decrease in depressive symptoms occurred independent of the co-occurrence of major depressive disorder and alcohol diagnoses. Nonetheless, higher levels of depressive symptoms during treatment were significantly associated with greater urge to use cocaine, alcohol, and other drugs as measured by the Cocaine Specific Skills Test. Finally, higher levels of depressive symptoms significantly predicted treatment attrition and alcohol relapse, although concurrent major depressive disorder diagnosis was not significantly associated with cocaine or alcohol use over follow-up.
Depressive symptoms decreased significantly and rapidly during treatment, which is consistent with other studies of cocaine abusers (4, 7, 12) and alcoholics (1, 13). No relationships were found between major depressive disorder diagnosis and degree of improvement in depressive symptoms during treatment. Depressive symptoms were higher both pre- and posttreatment for patients with major depressive disorder than for those without this diagnosis. Furthermore, we found no difference in the rate of decrease in depressive symptoms as a function of comorbid alcohol diagnosis. However, higher pretreatment levels of depressive symptoms were associated with significantly shorter lengths of stay. Therefore, despite the fact that depressive symptoms improved rapidly during substance abuse treatment, patients with higher pretreatment depressive symptoms were at risk for early treatment termination. Whether attrition resulted from greater difficulties in engaging in the treatment process or perhaps to a perception that their depression was not being addressed, this finding suggests that early attention to depressive symptoms is warranted.
It is of interest that a diagnosis of major depressive disorder and depressive symptoms were unrelated to pretreatment frequency of cocaine and alcohol use and to alcohol diagnosis. However, subjects with higher levels of depressive symptoms during treatment had higher Addiction Severity Index alcohol composite scores. This indicates that cocaine abusers who reported more depressive symptoms were also expressing greater concern and problems with alcohol before treatment.
This study allowed an examination of the effects of depression on relapse risks through assessment of the degree to which patients reported greater urges to use cocaine, alcohol, or other drugs in response to eight simulated high-risk situations. Results clearly showed a strong relationship between depressive symptoms and urge to use each substance, such that patients with higher levels of depression had greater urges. These data are consistent with social learning formulations in which dysphoric affect is hypothesized to increase urges to use by increasing the salience or incentive value of the positive reinforcing effects of drugs (15). However, neither a diagnosis of depression nor severity of depressive symptoms was related to cocaine relapse status or to the number of cocaine use days among those individuals who relapsed. These results are consistent with available evidence (7, 18), which suggested that depression status among cocaine abusers in treatment has not generally been a significant predictor of poorer cocaine use outcomes.
Depression diagnosis during treatment was not related to alcohol relapse status or to number of drinking days. However, patients who experienced an alcohol relapse episode had higher levels of depressive symptoms during treatment than those who did not relapse, after pretreatment levels of alcohol use had been controlled. Thus, depressive symptoms were a stronger predictor of alcohol relapse status than was depression diagnosis. Furthermore, depressive symptoms appear to indicate a risk of relapse to alcohol but not to cocaine.
It is of interest that level of depressive symptoms during treatment was significantly related to alcohol relapse despite a significant remission of depressive symptoms during treatment. These data suggest that depressive symptoms are an important indicator of possible posttreatment alcohol use. Since a majority of cocaine abusers have concurrent alcohol diagnoses (9; unpublished 1993 paper of D.J. Rohsenow et al.), depressive symptoms are of concern with regard to their alcohol relapse. We have recently demonstrated that adding cognitive behavior treatment for depression to standard alcohol treatment results in improvements in depressive symptoms during treatment and alcohol use outcomes at follow-up (26). Results of the current study suggest that this treatment may be a useful adjunct for alcohol-involved cocaine abusers as well. Future research should examine more closely the relationship between depressive symptoms during treatment and alcohol relapse and the possible role of cognitive behavior treatment for depression in reducing alcohol relapse among cocaine abusers.
Overall, the present study serves to provide further evidence of the importance of addressing depression during substance abuse treatment. While limited by a relatively small study group size and by the fact that alcohol diagnoses were obtained for only 70% of the total group, these findings suggest the need for further studies of both theoretical and clinical associations between depression and relapse. The results specifically point to the need to study separately the mechanisms involved in relapses to cocaine and alcohol use, since depressive symptoms may affect these outcomes differently. Future studies that investigate the role of depression coping skills training in the treatment of comorbid depression and substance use disorders appear warranted.
 |
Received Aug. 9, 1996; revision received June 13, 1997; accepted July 17, 1997. From Butler Hospital/Brown University School of Medicine and the Brown University Center for Alcohol and Addiction Studies, Providence, R.I. Address reprint requests to Dr. Brown, Butler Hospital/Brown University, 345 Blackstone Blvd., Providence, RI 02906. Supported by National Institute on Drug Abuse grants DA-04859 and DA-08511. The authors thank Cheryl Eaton, M.A., for her data analyses.
1. Brown SA, Inaba RK, Gillin JC, Schuckit MA, Stewart MA, Irwin MR: Alcoholism and affective disorder: clinical course of depressive symptoms. Am J Psychiatry 1995; 152:45–52Link, Google Scholar
2. Gawin FH, Kleber HD: Abstinence symptomatology and psychiatric diagnosis in cocaine abusers. Arch Gen Psychiatry 1986; 43:107–113Crossref, Medline, Google Scholar
3. Rounsaville BJ, Anton SF, Carroll K, Budde D, Prusoff BA, Gawin F: Psychiatric diagnoses of treatment-seeking cocaine abusers. Arch Gen Psychiatry 1991; 48:43–51Crossref, Medline, Google Scholar
4. Weiss RD, Mirin SM, Griffin MI, Michael JL: Psychopathology in cocaine abusers: changing trends. J Nerv Ment Dis 1988; 176:719–725Crossref, Medline, Google Scholar
5. Kilbey NM, Breslau N, Andreski P: Cocaine use and dependence in young adults: associated psychiatric disorders and personality traits. Drug Alcohol Depend 1992; 29:283–290Crossref, Medline, Google Scholar
6. Kleinman PH, Miller AB, Millman RB, Woody GE, Todd T, Kemp J, Lipton DS: Psychopathology among cocaine abusers entering treatment. J Nerv Ment Dis 1990; 178:442–447Crossref, Medline, Google Scholar
7. Carroll KM, Rounsaville BI, Gordon LT, Nich C, Jatlow P, Bisighini RM, Gawin F: Psychotherapy and pharmacotherapy for ambulatory cocaine abusers. Arch Gen Psychiatry 1994; 51:177–187Crossref, Medline, Google Scholar
8. Weiss RD, Mirin SM, Michael JL, Sollogub AC: Psychopathology in chronic cocaine abusers. Am J Drug Alcohol Abuse 1986; 12:17–29Crossref, Medline, Google Scholar
9. Carroll KM, Power MD, Bryant K, Rounsaville BJ: One-year follow-up status of treatment-seeking cocaine abusers: psychopathology and dependence severity as predictors of outcome. J Nerv Ment Dis 1993; 181:71–79Crossref, Medline, Google Scholar
10. Weiss RD, Mirin SM, Griffin ML: Methodological considerations in the diagnosis of coexisting psychiatric disorders in substance abusers. Br J Addict 1992; 87:179–187Crossref, Medline, Google Scholar
11. Schuckit MA: Alcoholic patients with secondary depression. Am J Psychiatry 1983; 140:711–714Link, Google Scholar
12. Husband SD, Marlowe DB, Lamb RJ, Iguchi MY, Bux DA, Kirby KC, Platt JJ: Decline in self-reported dysphoria after treatment entry in inner-city cocaine addicts. J Consult Clin Psychol 1996; 64:221–224Crossref, Medline, Google Scholar
13. Brown SA, Schuckit MA: Changes in depression among abstinent alcoholics. J Stud Alcohol 1988; 49:412–417Crossref, Medline, Google Scholar
14. Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK: Comorbidity of mental disorders with alcohol and other drug abuse. JAMA 1990; 264:2511–2518Google Scholar
15. Rohsenow DJ, Monti PM, Abrams DB, Rubonis AV, Niaura RS, Sirota AD, Colby SM: Cue elicited urge to drink and salivation in alcoholics: relationship to individual differences. Advances in Behavior Res and Therapy 1992; 14:195–210Crossref, Google Scholar
16. Monti PM, Abrams DB, Binkoff JA, Zwick WR, Liepman MR, Nirenberg TD, Rohsenow DR: Communication skills training, communication skills training with family, and cognitive behavioral mood management training for alcoholics. J Stud Alcohol 1990; 51:263–270Crossref, Medline, Google Scholar
17. Ziedonis DM, Kosten TR: Depression as a prognostic factor for pharmacological treatment of cocaine dependence. Psychopharmacol Bull 1991; 27:337–343Medline, Google Scholar
18. Carroll KM, Nich C, Rounsaville BJ: Differential symptom reduction in depressed cocaine abusers treated with psychotherapy and pharmacotherapy. J Nerv Ment Dis 1995; 183:251–259Crossref, Medline, Google Scholar
19. Carroll KM, Rounsaville BJ, Bryant KJ: Alcoholism in treatment-seeking cocaine abusers: clinical and prognostic significance. J Stud Alcohol 1993; 54:199–208Crossref, Medline, Google Scholar
20. O'Sullivan K, Rynne C, Miller J, O'Sullivan S, Fitzpatrick V, Hux M, Cooney J, Clare A: A follow-up study on alcoholics with and without co-existing affective disorder. Br J Psychiatry 1988; 152:813–819Crossref, Medline, Google Scholar
21. Kozlowski LT, Wilkinson DA: Use and misuse of the concept of craving by alcohol, tobacco, and drug researchers. Br J Addict 1987; 82:31–36Crossref, Medline, Google Scholar
22. Spitzer RL, Williams JBW, Gibbon M: Structured Clinical Interview for DSM-III-R—Patient Version (SCID-P). New York, New York State Psychiatric Institute, Biometrics Research, 1987Google Scholar
23. Sobell LC, Maisto S, Sobell MB, Cooper AM: Reliability of alcohol abusers' self-reports of drinking behavior. Behav Res Ther 1979; 17:157–160Crossref, Medline, Google Scholar
24. McLellan AT, Luborsky L, Woody GE, O'Brien CP: An improved diagnostic evaluation instrument for substance abuse patients: the Addiction Severity Index. J Nerv Ment Dis 1980; 168:26–33Crossref, Medline, Google Scholar
25. Miller IW, Bishop S, Norman WH, Maddever H: The Modified Hamilton Rating Scale for Depression: reliability and validity. Psychiatry Res 1985; 14:131–142Crossref, Medline, Google Scholar
26. Brown RA, Evans DM, Miller IW, Burgess ES, Mueller TI: Cognitive-behavioral treatment for depression in alcoholism. J Consult Clin Psychol 1997; 65:715–726Crossref, Medline, Google Scholar



