Self-Reported Anxiety, General Medical Conditions, and Disability Bed Days
Abstract
OBJECTIVE: This study examined the effect of self-reported anxiety on the number of days persons with various general medical conditions spend in bed owing to disability. METHOD: Self-reported medical illness and disability data from a nationally representative household survey sample (N=20,884) were analyzed. RESULTS: Among respondents with general medical conditions, those with self-reported anxiety had a nearly fourfold greater length of disability (mean=18.0 bed days) than the nonanxious respondents (mean=4.8 bed days). After adjustment for differences in demographic characteristics and burden of general medical illness, anxiety was associated with an additional 3.8 bed days. CONCLUSIONS: Self-reported anxiety in combination with general medical conditions may be associated with extensive functional impairment. (Am J Psychiatry 1997; 154:1766–1768)
An estimated 26.9 million Americans will develop a diagnosable anxiety disorder at some point in their lives (1). Symptoms of anxiety are even more prevalent (2). The high prevalence of anxiety disorders and their associated disability contribute to their high cost to society. In 1990 the estimated direct and indirect costs of anxiety to society totaled $46.6 billion, or approximately one-third of the costs of all mental disorders. Nearly three-quarters of this amount was a result of lost productivity (3). Medically ill patients with co-occurring anxiety commonly report lower levels of functioning and well-being than those without comorbid anxiety (4).
We examined the effect of self-reported anxiety in combination with various general medical conditions on disability bed days in a large nationally representative sample.
METHOD
Data were drawn from the National Medical Expenditure Survey (5), a survey of family health and health care conducted by the Agency for Health Care Policy and Research that followed federal guidelines concerning informed consent. Survey respondents (N=38,446) were randomly selected and weighted to correspond to the population of the United States in 1987.
Survey participants were asked to keep a diary that included an enumeration of medical conditions responsible for periods of disability and the utilization of medical services to treat the disability. The diaries were reviewed quarterly. Surveys were conducted by telephone and in-person interviews.
Periods of disability were reported by respondents as the number of days in periods specified in response to the question, “Not including any days spent in a hospital, did [the person] stay in bed more than half of the day because of any illness or injury?” Respondents were subsequently asked, “What condition caused [the person] to stay in bed?” The verbatim responses were recorded. A modified four-digit ICD-9-CM system was used to classify the responses. Coding of the responses was conducted by trained medical coders using a two-stage verification process.
Only conditions sufficiently severe to warrant the use of a professional medical service or a prescription medication were included in our analysis. Self-reported anxiety was assessed if ICD code 300.0 (anxiety states) or 799.2 (nervousness) was listed as one of the medical conditions causing a period of disability. The patient's other medical condition codes were then grouped into 26 major diagnostic categories (6). Respondents were asked to date the onset of the anxiety condition and all general medical conditions. We defined co-occurrence to mean that anxiety and the general medical condition occurred within the same respondent during the same year.
The SUDAAN software package (7) was used to accommodate the survey sampling design and weights for calculation of all statistics. Wald chi-square statistics (8) were used to test for differences in the distribution of demographic characteristics between respondents with self-reported anxiety and those without. General linear regression (9) was used to calculate the expected number of bed days with adjustment for age (continuous variable), sex (male/female), race (white/nonwhite), and number of general medical conditions (continuous variable). The number of days associated with anxiety was calculated by multiplying the number of subjects with anxiety by the mean difference in bed days between the two study groups (with and without anxiety). We used t tests to detect differences between groups in the mean number of expected bed days (10). All statistical tests were two-tailed.
We used linear models to determine whether the temporal order of the self-reported anxiety was related to the number of bed days after controlling for age, sex, race, and number of general medical conditions. Separate models were run for subjects reporting both an anxiety condition and each of the reported medical conditions as well as overall.
RESULTS
Individuals with co-occurring self-reported anxiety (N=795) were significantly more likely than those without anxiety (N=20,089) to be older (mean age=58.0 years versus 36.0 years; t=33.2, df=101, p<0.0001), to be female (76.7% versus 55.0% χ2=98.5, df=1, p<0.0001), to have a low income (47.6% versus 30.1% χ2=59.4, df=2, p<0.0001), and to be nonworking (67.5% versus 49.0% χ2=73.3, df=1, p<0.0001). Race was not associated with anxiety. Respondents with anxiety conditions had significantly more co-occurring general medical conditions (mean=4.0 versus mean=2.9; t=16.5, df=101, p<0.0001).
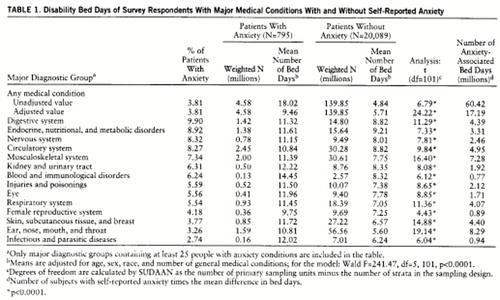
Table 1 shows the mean number of bed days within each major diagnostic category for the subjects with and without self-reported anxiety. The difference between the mean number of bed days for those with anxiety and those without was statistically significant (p<0.0001) within all major diagnostic category groups and overall.
Anxiety was present in 3.8% of the subjects with any general medical condition. Subjects with digestive system problems had the highest prevalence of anxiety (9.9%), followed closely by subjects with endocrine, nutritional, and metabolic problems (8.9%), nervous system problems (8.3%), and circulatory system problems (8.3%).
Self-reported anxiety accounted for an estimated 60.4 million days of lost productivity. After adjustment for age, sex, race, and number of general medical conditions, the analysis showed that 17.2 million days were lost because of anxiety. On average, respondents with self-reported anxiety and any other general medical condition reported periods of disability nearly four times as long as those without anxiety (mean=18.0 bed days versus mean=4.8 bed days). After adjustment, there was still a substantial difference (mean=9.5 bed days versus mean=5.7 bed days).
Nearly three-quarters of bed days (mean=13.2 days; 73.1%) occurred among individuals whose general medical condition was complicated by self-reported anxiety (mean=3.8 days; 39.6%, adjusted). The mean number of excess bed days associated with self-reported anxiety ranged from 5.2 for ear, nose, mouth, and throat disorders (10.8 minus 5.6) to 2.4 for endocrine, nutritional, and metabolic disorders (11.6 minus 9.2).
Self-reported anxiety was specified as occurring before the first medical condition one-third (31.7%) of the time. Anxiety came first most often in persons with infectious and parasitic diseases (98.1% 95% confidence interval=94.4–101.9) and ear, nose, mouth, and throat disorders (70.6% 95% confidence interval=63.5–77.7). The medical condition came first most often in persons with endocrine, nutritional, and metabolic disorders (68.9% 95% confidence interval=60.6–77.2) and circulatory system disorders (66.3% 95% confidence interval=61.1–71.5). Overall, this temporal order had no significant impact on the number of disability bed days (β=3.46, t=0.83, df=101, p=0.41).
DISCUSSION
We report evidence which suggests that self-reported anxiety greatly increases the functional impairment associated with a wide range of general medical disorders. We estimate that this anxiety is associated with a loss of more than 60 million days of productivity per year among the medically ill. This level of lost productivity is comparable to that for the common cold (62.4 million lost days) or pneumonia (40 million lost days) (11).
While our study does not permit us to comment on specific cause-and-effect relationships, it appears that when present, self-reported anxiety is associated with significantly more medical disability. These observations help place in broader perspective clinical findings that in individual patients, untreated anxiety is associated with loss of productivity and decreased functional well-being (12).
In our study, self-reported anxiety had an uncertain relationship to anxiety disorder diagnoses. We also have no information about the reliability of these subjective anxiety states.
Our findings suggest that there is a substantial and significant relationship between anxiety and an increased number of bed days among the medically ill. Across a range of medical conditions, anxiety serves as a nonspecific marker for greater severity of illness.
 |
Received Nov. 18, 1996; revisions received March 17 and June 16, 1997; accepted July 3, 1997. From Western Psychiatric Institute and Clinic/Department of Psychiatry, University of Pittsburgh Medical School; New York State Psychiatric Institute/Department of Psychiatry, College of Physicians and Surgeons, Columbia University, New York; and the Office of Research, American Psychiatric Association, Washington, D.C. Address reprint requests to Mr. Marcus, Western P sychiatric Institute and Clinic, 3811 O'Hara St., Pittsburgh, PA 15213. Supported by the Stanley Center for the Innovative Treatment of Bipolar Disorder and by a grant from the Van Ameringen Foundation to the American Psychiatric Association. T he authors thank Terri Tanielian for her assistance with this project .
1. Regier DA, Narrow WE, Rae DS, Manderscheid RW, Locke BZ, Goodwin FK: The de facto US mental and addictive disorders service system: Epidemiologic Catchment Area prospective 1-year prevalence rates of disorders and services. Arch Gen Psychiatry 1993; 50:85–94Crossref, Medline, Google Scholar
2. Olfson M, Broadhead EW, Weissman MM, Leon CL, Farber L, Hoven C, Kathol R: Subthreshold psychiatric symptoms in a primary care group practice. Arch Gen Psychiatry 1996; 53:880–886Crossref, Medline, Google Scholar
3. DuPont RL, Rice DP, Miller LS, Shiraki SS, Rowland CR, Harwood HJ: Economic costs of anxiety disorders. Anxiety 1996; 2(4):167–172Google Scholar
4. Sherbourne CD, Wells KB, Meredith LS, Jackson CA, Camp P: Comorbid anxiety disorder and the functioning and well-being of chronically ill patients of general medical providers. Arch Gen Psychiatry 1996; 53:889–895Crossref, Medline, Google Scholar
5. National Medical Expenditure Survey, 1987: Household Survey. Rockville, Md, US Department of Health and Human Services, Agency for Health Care Policy and Research, 1987Google Scholar
6. PC Grouper Software Version 96.1: HCFA DRG With HCFA Statistics. Wallingford, Conn, 3M Health Information Systems, 1996Google Scholar
7. Shah BV, Barnwell BG, Beiler GS: SUDAAN User's Manual, Version 6.40, 2nd ed. Research Triangle Park, NC, Research Triangle Institute, 1996Google Scholar
8. Thomas DR, Rau JNK: On the power of some goodness-of-fit tests under cluster sampling, in Proceedings of the American Statistical Association, Section on Survey Research Methods. Washington, DC, American Statistical Association, 1985, pp 291–296Google Scholar
9. Kish L, Frankel MR: Inference from complex samples. J Royal Statistical Society B 1974; 36:1–37Google Scholar
10. Kendall MG, Stuart A: The Advanced Theory of Statistics. New York, Hafner, 1973Google Scholar
11. Current estimates from the National Health Interview Survey. Vital Health Stat 10 1994; 193:49Google Scholar
12. Kouzis AC, Eaton WW: Emotional disability days: prevalence and predictors. Am J Public Health 1994; 84:1304–1307Google Scholar



