Mental Disorders and Disability Among Patients in a Primary Care Group Practice
Abstract
OBJECTIVE: This article examines social and occupational disability associated with several DSM-IV mental disorders in a group of adult primary care outpatients. METHOD: The subjects were 1,001 primary care patients (aged 18–70 years) in a large health maintenance organization. Data on each patient's sociodemographic characteristics and functional disability, including scores on the Sheehan Disability Scale, were collected at the time of a medical visit. A structured diagnostic interview for current DSM-IV disorders was then completed by a mental health professional over the telephone within 4 days of the visit. RESULTS: The most prevalent disorders were phobias (7.7%), major depressive disorder (7.3%), alcohol use disorders (5.2%), generalized anxiety disorder (3.7%), and panic disorder (3.0%). A total of 8.3% of the patients met the criteria for more than one mental disorder. The proportion of patients with co-occurring mental disorders varied by index disorder from 50.0% (alcohol use disorder) to 89.2% (generalized anxiety disorder). Compared with patients who had a single mental disorder, patients with co-occurring disorders reported significantly more disability in social and occupational functioning. After adjustment for other mental disorders and demographic and general health factors, compared with patients with no mental disorder, only patients with major depressive disorder, bipolar disorder, phobias, and substance use disorders had significantly increased disability, as measured by the Sheehan Disability Scale. CONCLUSIONS: Primary care patients with more than one mental disorder are common and highly disabled. Individual mental disorders have distinct patterns of psychiatric comorbidity and disability. (Am J Psychiatry 1997; 154:1734–1740)
Epidemiologic research in community and clinical settings reveals a strong correlation between mental disorder and impaired occupational and social functioning (1–3). Primary care patients with depressive and anxiety disorders have poorer social, role, and occupational functioning than patients without these disorders. Depressive disorders have also been associated with a larger number of disability days and poorer role functioning than several common general medical diseases, including arthritis, hypertension, and diabetes (4).
Longitudinal studies of primary care patients provide evidence for the disabling effects of mood and anxiety disorders (5, 6). Patients whose psychiatric symptoms substantially improve over time show corresponding improvements in social and occupational functioning. In contrast, patients whose psychiatric symptoms do not substantially improve have no or little change in their level of disability (6).
The link between specific mental disorders and functional disability may be confounded by the co-occurrence of multiple mental disorders within the same individual. In one study (7), for example, approximately two-thirds of primary care patients with a current depressive disorder also met the criteria for an anxiety disorder. Recent epidemiologic studies (1, 8) have sought to determine the unique contribution of individual mental disorders to disability in primary care populations.
In a World Health Organization (WHO) study (8), primary care patients with isolated ICD-10 mental disorders reported greater occupational and physical disability than patients without a mental disorder. Across a range of mental disorders, patients who met the criteria for only one disorder tended to have poorer occupational and role functioning than patients with no mental disorder but better functioning than patients with multiple mental disorders.
In a separate study, Spitzer and co-workers (1) examined the association between broad mental disorder groups and impaired functioning. After controlling for other mental and general medical disorders, they found that anxiety and mood disorders were significantly associated with impaired social and role functioning. In contrast, alcohol use disorders were not significantly associated with impaired role or social functioning.
In this study we extended this line of research to a wide range of individual DSM-IV mental disorders. We examined relationships between these disorders and measures of social and occupational disability to evaluate the effects of mental disorders, in isolation and in combination, on social and occupational functioning.
METHOD
The data in this report were collected for a study of a new procedure for assessing mental disorders in primary care, the Symptom-Driven Diagnostic System for Primary Care (9). The study was conducted at the Kaiser Permanente Medical Center in Oakland, Calif., which serves over 160,000 members.
A randomly selected group of patients with already scheduled appointments at the Department of Medicine were invited to participate in the study. Eligible patients included new and continuing patients who had appointments that had been made at least 3 days in advance, were between 18 and 70 years of age, could read and write English, were able to complete the study forms, and were scheduled for face-to-face contact with their primary care physicians. Only patients who gave written informed consent were enrolled in the study.
A total of 1,001 patients participated in the study. This represented 88.6% of the patients who originally agreed to participate and 40.0% of those invited to participate in the study during a prescreening interview. The most common reason offered for refusing to participate at the prescreening interview was lack of time, and the most common reasons for dropping out after initially agreeing to participate were failure to arrive for the medical appointment on time or missing the appointment altogether.
The basic demographic and service utilization characteristics of the study subjects were compared with those of a simple randomly selected group of 5,005 patients drawn from the same population of clinic visits. The study group and the larger group were similar in age (mean=49.2 years versus mean=49.7 years), sex (63.0% female versus 58.1% female), number of general medical visits in the past year (mean=4.2 versus mean=4.2), and the percentage who had ever been seen in the Department of Psychiatry (12.0% versus 12.7%).
Patients who met the prescreening eligibility criteria and provided verbal consent to participate were invited to report to the medical clinic for study intake one-half hour before their regularly scheduled appointment. At study intake, patients completed a history form that included demographic data, a brief medical checklist, questions on use of mental health services, and disability items. Disability was measured with the Sheehan Disability Scale (10, 11), which is a composite of three self-rated 10-point Likert response subscales (0=no disability, 1–3=mild, 4–6=moderate, 7–9=marked, 10=extreme) to assess work, family, and social functioning during the past month. In addition, disability items derived from the National Institute of Mental Health Epidemiologic Catchment Area Program (12) were used to self-rate “getting along with your partner” (marital distress) and whether the patient had missed work due to emotional problems during the past month.
Patients were also asked whether, during the past month, they had discussed an emotional problem with their doctor; talked to a psychiatrist, psychologist, psychotherapist, social worker, family therapist, or drug counselor; or been to Alcoholics Anonymous. A positive response to any of these questions was considered as recent use of mental health care.
Within 4 days following the index medical visit, a mental health professional contacted each subject by telephone to administer the Structured Clinical Interview for DSM-III-R (SCID) (13), which had been modified to reflect DSM-IV criteria. Thirteen mental health professionals (nine psychiatrists and six nonphysicians with extensive mental health care experience) were trained to administer the structured interviews. One hundred randomly selected audiotapes of interviews were blindly rated by the investigators; because of low within-rater base rates and nearly complete agreement between raters and reviewers (all diagnoses in 91.6% of cases), it was frequently not possible to calculate Cohen's kappa (14).
Eighty-four percent of the structured interviews were completed within 2 days after the index medical visit, and the other interviews were completed within 4 days after the medical visit. The revised SCID covered major depressive disorder, panic disorder, generalized anxiety disorder, obsessive-compulsive disorder (OCD), and alcohol and drug abuse and dependence. A shorter structured interview based on DSM-IV criteria, the Mini International Neuropsychiatric Interview (15), was also administered to diagnose bipolar disorder, anorexia nervosa, bulimia nervosa, posttraumatic stress disorder (PTSD), specific phobia, social phobia, agoraphobia, and antisocial personality disorder. Previous research (16) demonstrates high concordance between the Mini International Neuropsychiatric Interview and the SCID for these diagnoses.
Some of the analyses involved patients who met criteria for multiple mental disorders. In these analyses, 10 diagnostic groups were considered: major depressive disorder, generalized anxiety disorder, PTSD, OCD, panic disorder, phobia, antisocial personality disorder, alcohol use disorders, drug use disorders, and eating disorders. Patients with panic disorder and agoraphobia were considered to have one disorder. In some analyses, alcohol and drug use disorders were considered together as substance use disorders.
In the statistical analyses, between-group comparisons of categorical variables were made with the chi-square test, except when the expected cell size fell below five, in which case Fisher's exact test was used. Group comparisons of Sheehan Disability Scale scores were made with analysis of variance followed by Tukey's honestly significant difference test of pairwise comparisons (alpha=0.05).
Multivariate analyses were used to examine associations of each disorder with the disability measures while demographic and clinical factors were controlled. The 10 disorders and patients' age, sex, race, marital status, and perceived physical health status as measured on a 5-point Likert response scale were entered as independent variables in logistic regression analyses to examine the strength of associations with the categorical disability measures. Multiple linear regression was used to examine association of these independent variables with Sheehan Disability Scale scores.
RESULTS
Demographic characteristics of the subjects are presented in table 1. The study group was predominantly female, married, and between 31 and 60 years of age. It was also racially diverse, and most subjects had received at least some college education. A majority of the subjects reported that their total annual family income was between $25,000 and $69,999.
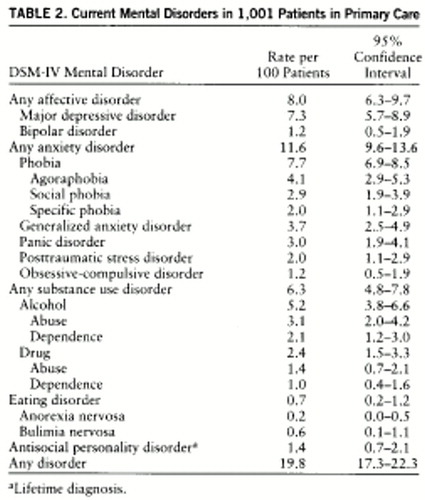
Table 2 displays the rates of current mental disorders in the study group. Approximately one-fifth (19.8%) of the patients met the criteria for at least one of the disorders under study. Anxiety disorders were the most common group of disorders, followed by affective disorders and substance use disorders.
Approximately 8.3% (N=83) of the patients met the criteria for more than one mental disorder. As a group, the patients with more than one mental disorder had significantly higher Sheehan Disability Scale scores than the patients with a single disorder (mean score=16.2, SD=8.4, versus mean=9.5, SD=7.5; t=5.5, df=188, p<0.001) and were significantly more likely to report recent loss of work time (50.6% versus 33.9% χ2=5.5, df=1, p<0.02). These two patient subgroups did not significantly differ with respect to recent mental health care utilization (37.3% versus 26.1%) or marital distress (18.3% versus 18.5%).
Major Depressive Disorder
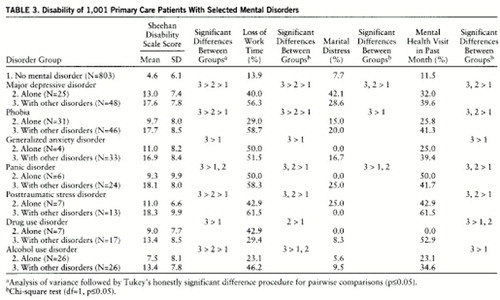
Major depressive disorder, which occurred in 7.3% of the patients, was the single most common mental disorder. Nearly two-thirds (65.8%, N=48) of the 73 patients with major depressive disorder met the criteria for at least one other mental disorder. This was most commonly generalized anxiety disorder (58.3%, N=28 of 48), panic disorder (35.4%), agoraphobia (35.4%), or social phobia (31.3%). In the univariate analysis, the patients with major depressive disorder alone were significantly more likely than the patients without a mental disorder to report recent loss of work time, marital distress, and mental health care utilization. These patients also had significantly higher Sheehan Disability Scale scores (table 3).
After controlling for age, sex, race, marital status, perceived physical health status, and other mental disorders, we found that the patients with major depressive disorder had an estimated 7.5 times greater risk of marital distress, a 2.2 times greater risk of recent missed time at work, and a 1.9 times greater risk of recent mental health service utilization (table 4). There was also a significant positive association between major depressive disorder and Sheehan Disability Scale score after adjustment for the other demographic and clinical variables.
Phobias
The rate of current phobias was 7.7%. Most of the 77 patients with phobia (59.7%, N=46) met the criteria for at least one other mental disorder. The most commonly associated diagnoses were major depressive disorder (56.5%, N=26 of 46), generalized anxiety disorder (37.0%), panic disorder (34.8%, excluding panic disorder and agoraphobia), and alcohol use disorders (30.4%).
In the univariate analysis, patients with phobia alone had higher Sheehan Disability Scale scores and were more likely to report recent work time loss and a mental health visit than the patients without a mental disorder, but they had lower Sheehan Disability Scale scores and were less likely to report recent loss of work time than the patients with phobia and another mental disorder (table 3). After we controlled for the potentially confounding effects of demographic factors, perceived health status, and other mental disorders, phobia was significantly associated with Sheehan Disability Scale score but not the other disability measures (table 4).
Generalized Anxiety Disorder
Thirty-seven patients (3.7%) met the criteria for generalized anxiety disorder. The vast majority of the patients with generalized anxiety disorder (89.2%, N=33) also met the criteria for another mental disorder. Major depressive disorder was the most commonly associated disorder (84.8%, N=28 of 33), followed by agoraphobia (33.3%), panic disorder (30.3%), social phobia (30.3%), and specific phobia (30.3%).
Patients with generalized anxiety disorder and another disorder had significantly higher Sheehan Disability Scale scores than patients without a mental disorder and were significantly more likely to report having missed work and having made a mental health visit during the past month (table 3). No significant associations between generalized anxiety disorder and the various disability measures were observed following adjustment for possible confounding variables (table 4).
Panic Disorder
Twenty-four (80.0%) of the 30 patients with panic disorder also met the criteria for another mental disorder. The most commonly co-occurring disorders were major depressive disorder (70.8%, N=17 of 24), social phobia (50.0%), specific phobia (41.7%), and generalized anxiety disorder (41.7%). The patients with panic disorder and other mental disorders were more likely to report marital distress and had significantly higher Sheehan Disability Scale scores than the patients with panic disorder alone and those with no mental disorder (table 3).
The patients with panic disorder alone were significantly more likely than the patients with no mental disorder to report recent loss of work time or a mental health visit (table 3). However, the associations between panic disorder and the disability measures were not significant after adjustment for demographic and other clinical variables (table 4).
Substance Use Disorders
The study group included 24 patients (2.4%) who met criteria for current drug abuse or dependence and 52 (5.2%) who met the criteria for alcohol abuse or dependence (table 2). The most common drugs of abuse or dependence were cannabis (N=13), cocaine (N=6), and sedatives (N=5).
Most of the 63 patients with a substance use disorder (58.7%, N=37) met the criteria for at least one other mental disorder. Thirteen patients met the criteria for both alcohol and drug use disorders. Among the patients with an alcohol use disorder, major depressive disorder (N=8) and agoraphobia (N=8) were the most common comorbid mental disorders not involving substance use. Specific phobia (N=5) and agoraphobia (N=5) were the most common co-occurring disorders among the patients with drug use disorders. After we controlled for potentially confounding factors, substance use disorders were significantly associated with Sheehan Disability Scale score and recently missing time at work (table 4).
Posttraumatic Stress Disorder
Nearly two-thirds of the 20 patients with PTSD (65%, N=13) also met the criteria for another mental disorder. The most common comorbid disorders were phobia (69.2%, N=9 of 13), major depressive disorder (53.8%), and bipolar disorder (38.5%). In the univariate analysis, the patients with PTSD alone had significantly higher Sheehan Disability Scale scores and were significantly more likely to report marital distress and recent mental health service use than the patients without a mental disorder (table 3). In the multivariate analyses, PTSD was significantly associated with making a recent mental health visit, but not the other disability measures (table 4).
Other Disorders
A majority of the patients who met the criteria for OCD (83.3%, N=10 of 12), bipolar disorder (75.0%, N=9 of 12), antisocial personality disorder (64.2%, N=9 of 14), or an eating disorder (71.4%, N=5 of 7) also met the criteria for other mental disorders. Several patients with OCD also had phobia (N=9) or major depressive disorder (N=7). Substance use disorders tended to occur in combination with bipolar disorder (N=4), antisocial personality disorder (N=4), and eating disorders (N=4).
After adjustment for the effects of diagnostic and other variables, bipolar disorder was significantly associated with Sheehan Disability Scale score and recent loss of work time (table 4). In these analyses, OCD, eating disorders, and antisocial personality disorder were not significantly associated with any of the disability measures. Six patients with bipolar disorder reported receiving mental health care in the past month.
DISCUSSION
We found that major depressive disorder, bipolar disorder, phobia, and substance use disorders were independently and significantly associated with a composite measure of work, family, and social disability. The two affective disorders, major depressive disorder and bipolar disorder, were associated with the largest decrements in functioning. These findings support the recent emphasis on the management of major depressive disorder in primary care (17) and suggest that attention should also be directed toward the management of bipolar disorder in primary care. Bipolar disorder was particularly strongly associated with having missed time at work.
Phobia had a modest association with social disability. In an earlier study (18), primary care patients with social phobia uncomplicated by major depression reported poorer overall health than patients without a mental disorder. We extend this finding by demonstrating that primary care patients with phobia by itself report significantly poorer social, family, and work functioning than patients without a mental disorder. Although phobia that occurs with other mental disorders increases disability, phobia alone may be an important source of impairment and should not be minimized in practice.
The current observation that substance use disorders are independently associated with social disability contrasts with the earlier study that failed to demonstrate a unique association between alcohol use disorders and impaired social or role functioning (1). This discrepancy may be related to the greater power achieved in our study by combining drug and alcohol use disorders or to differences in how disability was measured. It is also possible that the patients with substance use disorders in our study group were simply more severely ill than the patients with alcohol use disorders identified in the earlier study.
Consistent with the WHO study (8), we found that restricting the analysis to primary care patients in whom there is no comorbid mental disorder tends to diminish the level of disability. Across a range of disorders and disability measures, patients with a single mental disorder tended to be less disabled than patients with multiple disorders, but they were more disabled than patients with no mental disorder. These relationships underscore the importance of assessing psychiatric comorbidity in primary care. The high frequency of untreated comorbid cases should stimulate efforts to improve the diagnosis and treatment of primary care patients with complex psychiatric symptom profiles.
A strict application of DSM-IV exclusion criteria for generalized anxiety disorder would lower our overall rate estimate of 3.7% (N=37) to 0.4% (N=4). The DSM-IV criteria for generalized anxiety disorder require that “the focus of the anxiety and worry is not confined to features of an Axis I disorder” and “the disturbance is not due to the direct physiological effects of a substance” (p. 436). If it is assumed that generalized anxiety disorder is a residual diagnostic category that exists only in the absence of other related axis I disorders, then the study group of 1,001 cases yielded only four cases of generalized anxiety disorder. For heuristic reasons, however, we report overall results without imposing the diagnostic hierarchy described in DSM-IV. With a more detailed diagnostic evaluation, it might have been possible to separate the comorbid cases into those with primary generalized anxiety disorder and those with symptoms of generalized anxiety disorder due to another axis I disorder.
When comorbid and noncomorbid cases are combined, our rate estimates for individual mental disorders are generally consistent with earlier research in primary care. Specifically, our estimates fall near or within the range of previously published rates (shown in parentheses): phobia, 7.7% (5.8%–13.0% [19–22]); major depression, 7.3% (2.2%–14.1% [8, 19, 20, 22–26]); generalized anxiety disorder, 3.7% (1.6%–11.9% [8, 19, 20, 23, 26]); alcohol abuse, 3.1% (2.6%–8.2% [8, 20, 21, 23, 24, 26]); panic disorder, 3.0% (1.1%–6.2% [8, 19, 20, 23, 24, 26]); OCD, 1.2% (0.7%–2.2% [19–21, 23]); and bipolar disorder, 1.2% (0.7%–0.9% [20, 24]).
This report is constrained by several limitations in the study design. First, the diagnostic interviews were conducted over the telephone rather than in person. While the emerging literature suggests generally good agreement between these two modes of interview administration (27–30), illicit drug use may be an important exception, since it has been found to be underreported in telephone interviews (31). Second, because the study was set in a large, urban health maintenance organization and included few patients from the extremes of the income distribution, the results may not necessarily generalize to other primary care patients in other treatment settings or to population-based samples. Population-based research reveals marked urban/rural (32) and income-related (33) differences in the prevalence of individual mental disorders. Third, patients were examined for 16 common mental disorders rather than the full range of DSM-IV disorders. A more comprehensive diagnostic interview would be expected to uncover even higher aggregate rates of disorder and higher rates of psychiatric comorbidity. Fourth, a substantial number of the sampled patients did not participate in the study. Although we cannot be certain of the effect of nonresponse on the rate estimates, the finding that the respondents were similar in basic demographic composition and prior psychiatric visits to a large group randomly selected from the same primary care population suggests that the responders were representative of the clinic population as a whole. Nonresponse rates are not available from the other two published studies that examined psychiatric comorbidity and disability in primary care (1, 8). Fifth, despite the large study group size, high rates of psychiatric comorbidity limited the number of available patients with some individual mental disorders alone.
Primary care patients who meet criteria for more than one current mental disorder are common, highly disabled, and most often untreated. Furthermore, some mental disorders (e.g., generalized anxiety disorder and panic disorder) rarely occur in isolation. Outcome studies are needed to increase our understanding of the clinical course and effective treatment of primary care patients with comorbid mental disorders.
 |
 |
 |
 |
Received April 7, 1997; revision received Aug. 5, 1997; accepted Aug. 8, 1997. From the Department of Psychiatry, College of Physicians and Surgeons, Columbia University, and New York State Psychiatric Institute; Cornell University Medical College, New York; Kaiser Permanente Medical Center, Oakland, Calif.; the Department of Psychiatry, University of South Florida, Tampa; and the Department of Psychiatry, University of Iowa School of Medicine, Iowa City. Address reprint requests to Dr. Olfson, Department of Psychiatry, College of Physicians and Surgeons, Columbia University, 722 West 168th St., New York, NY 10032. The Upjohn Company sponsored and supported the development of the Symptom-Driven Diagnostic System for Primary Care. The authors thank Carrie Miller, Ph.D., Lena Verdeli, M.A., M.Sc., Laura Portera, and Joy Pelayo for their contributions to the project; the participating Kaiser Permanente physicians and nurses; and the assessment interviewers at the University of South Florida.
1. Spitzer RL, Kroenke K, Linzer M, Hahn SR, Williams JBW, DeGruy FV III, Brody D, Davies M: Health-related quality of life in primary care patients with mental disorders: results from the PRIME-MD 1000 Study. JAMA 1995; 274:1511–1517Google Scholar
2. Broadhead WE, Blazer DG, George LK, Tse CK: Depression, disability days, and days lost from work in a prospective epidemiologic survey. JAMA 1990; 264:2524–2528Google Scholar
3. Hecht H, Zerssen D, Wittchen HU: Anxiety and depression in a community sample: the influence of comorbidity on social functioning. J Affect Disord 1990; 18:137–144Crossref, Medline, Google Scholar
4. Wells KB, Stewart A, Hays RD, Burnam MA, Rogers W, Daniels M, Berry S, Greenfield S, Ware J: The functioning and well-being of depressed patients: results from the Medical Outcomes Study. JAMA 1989; 262:914–919Crossref, Medline, Google Scholar
5. Von Korff M, Ormel J, Katon W, Lin EHB: Disability and depression among high utilizers of health care: a longitudinal analysis. Arch Gen Psychiatry 1992; 49:91–100Crossref, Medline, Google Scholar
6. Ormel J, Von Korff M, vanden Brink W, Katon W, Brilman E, Oldehinkel T: Depression, anxiety and disability show synchrony of change. Am J Public Health 1993; 83:385–390Crossref, Medline, Google Scholar
7. Sherbourne CD, Jackson CA, Meredith LS, Camp P, Wells KB: Prevalence of comorbid anxiety disorders in primary care outpatients. Arch Fam Med 1996; 5:27–34Crossref, Medline, Google Scholar
8. Ormel J, Von Korff M, Ustun B, Pini S, Korten A, Oldehinkel T: Common mental disorders and disability across cultures: results from the WHO collaborative study on psychological problems in general health care. JAMA 1994; 272:1741–1748Google Scholar
9. Leon AC, Olfson M, Weissman MM, Portera L, Fireman BH, Blacklow RS, Hoven C, Broadhead WE: Brief screens for mental disorders in primary care. J Gen Intern Med 1996; 11:426–430Crossref, Medline, Google Scholar
10. Leon AC, Shear MK, Portera L, Klerman GL: Assessing impairment in patients with panic disorders: the Sheehan Disability Scale. Soc Psychiatry Psychiatr Epidemiol 1992; 27:78–82Crossref, Medline, Google Scholar
11. Sheehan DV: The Anxiety Disease. New York, Charles Scribner's Sons, 1983Google Scholar
12. Markowitz JS, Weissman MM, Ouellette R, Lish JD, Klerman GL: Quality of life in panic disorder. Arch Gen Psychiatry 1989; 46:984–992Crossref, Medline, Google Scholar
13. Spitzer RL, Williams JBW, Gibbon M, First MB: The Structured Clinical Interview for DSM-III-R (SCID), I: history, rationale, and description. Arch Gen Psychiatry 1992; 49:624–629Crossref, Medline, Google Scholar
14. Fleiss JL: The Design and Analysis of Clinical Experiments. New York, John Wiley & Sons, 1986Google Scholar
15. Sheehan D, Janavs J, Knapp E, Sheehan M, Baker R: Mini International Neuropsychiatric Interview, Clinician Rated, version 4.0. Tampa, University of South Florida College of Medicine, 1992Google Scholar
16. Sheehan DV, Lecrubier Y, Sheehan KH, Janavs J, Weiller E: Comparison of the Mini International Neuropsychiatric Interview (MINI) With the SCID-P and the CIDI: a validity study (abstract). Psychopharmacol Bull 1995; 31:616Google Scholar
17. Depression Guideline Panel: Depression in Primary Care, vol 2: Treatment of Major Depression. Clinical Practice Guideline 5. Agency for Health Care Policy and Research publication 93-0551. Rockville, Md, US Department of Health and Human Services, April 1993Google Scholar
18. Weiller E, Bisserbe J-C, Boyer P, Lepine J-P, Lecrubier Y: Social phobia in general health care: an unrecognised undertreated disabling disorder. Br J Psychiatry 1996; 168:169–174Crossref, Medline, Google Scholar
19. Zinbarg RE, Barlow DH, Liebowitz M, Street L, Broadhead E, Katon W, Roy-Byrne P, Lepine J-P, Teherani M, Richards J, Brantley PJ, Kraemer H: The DSM-IV field trial for mixed anxiety-depression. Am J Psychiatry 1994; 151:1153–1162Google Scholar
20. Schulberg HC, Saul M, McClelland M, Ganguli M, Christy W, Frank R: Assessing depression in primary medical and psychiatric practices. Arch Gen Psychiatry 1985; 42:1164–1170Google Scholar
21. Cleary PD, Merle M, Bush BT, Warburg MM, Delbanco TL, Aronson MD: Prevalence and recognition of alcohol abuse in a primary care population. Am J Med 1988; 85:466–471Crossref, Medline, Google Scholar
22. Hoeper EW, Nycz GR, Cleary PD, Regier DA, Goldberg ID: Estimated prevalence of RDC mental disorder in primary care. Int J Ment Health 1979; 8:6–15Google Scholar
23. Leon AC, Olfson M, Broadhead WE, Barrett JE, Blacklow RS, Keller MB, Higgins ES, Weissman MM: Prevalence of mental disorders in primary care: implications for screening. Arch Fam Med 1995; 4:857–861Crossref, Medline, Google Scholar
24. Blacker CVR, Clare AW: The prevalence and treatment of depression in general practice. Psychopharmacology (Berl) 1988; 95(suppl):S14–S17Google Scholar
25. Barrett JE, Barrett HA, Oxman TE, Gerber PD: The prevalence of psychiatric disorders in a primary care practice. Arch Gen Psychiatry 1988; 45:1100–1106Google Scholar
26. Von Korff M, Shapiro S, Burke JD, Teitlebaum M, Skinner EA, German P, Turner RW, Klein L, Burns B: Anxiety and depression in a primary care clinic. Arch Gen Psychiatry 1987; 44:152–156Crossref, Medline, Google Scholar
27. Wells KB, Burnam MA, Leake B, Robins LN: Agreement between face-to-face and telephone administered versions of the depressive section of the NIMH Diagnostic Interview Schedule. J Psychiatr Res 1988; 22:207–220Crossref, Medline, Google Scholar
28. Paulson SA, Crowe RR, Noyes R, Pfohl B: Reliability of the telephone interview in diagnosing anxiety disorders. Arch Gen Psychiatry 1988; 45:62–63Crossref, Medline, Google Scholar
29. Watson CG, Anderson PED, Thomas D, Nyberg K: Comparison of telephone and face to face Diagnostic Interview Schedules. J Nerv Ment Dis 1992; 180:534–535Crossref, Medline, Google Scholar
30. Simon GE, Revicki D, Von Korff ML: Telephone assessment of depression severity. J Psychiatr Res 1993; 27:247–252Crossref, Medline, Google Scholar
31. Gfroerer JC, Hughes AL: The feasibility of collecting drug abuse data by telephone. Pub Health Rep 1991; 106:384–393Medline, Google Scholar
32. Blazer D, George LK, Landerman R, Pennybacker M, Melville ML, Woodbury M, Manton KG, Jordan K, Locke B: Psychiatric disorders: a rural/urban comparison. Arch Gen Psychiatry 1985; 42:651–656Crossref, Medline, Google Scholar
33. Bruce ML, Takeuchi DT, Leaf PJ: Poverty and psychiatric status: longitudinal evidence from the New Haven Epidemiologic Catchment Area study. Arch Gen Psychiatry 1991; 48:470–474Crossref, Medline, Google Scholar



