Posttraumatic Stress Disorder and Functioning and Quality of Life Outcomes in a Nationally Representative Sample of Male Vietnam Veterans
Abstract
OBJECTIVE: Although posttraumatic stress disorder (PTSD) is a highly prevalent and often chronic condition, the relationship between PTSD and functioning and quality of life remains incompletely understood. METHOD: The authors undertook an archival analysis of data from the National Vietnam Veterans Readjustment Study. The study subjects consisted of the nationally representative sample of male Vietnam veterans who participated in the National Vietnam Veterans Readjustment Study. The authors estimated PTSD at the time of the interview with the Mississippi Scale for Combat-Related Posttraumatic Stress Disorder. They examined the following outcomes: diminished well-being, physical limitations, bed day in the past 2 weeks, compromised physical health status, currently not working, and perpetration of violence. Logistic models were used to determine the association between PTSD and outcome; adjustment was made for demographic characteristics and comorbid psychiatric and other medical conditions. RESULTS: The risks of poorer outcome were significantly higher in subjects with PTSD than in subjects without PTSD in five of the six domains. For the outcome domains of physical limitations, not working, compromised physical health, and diminished well-being, these significantly higher risks persisted even in the most conservative logistic models that removed the shared effects of comorbid psychiatric and other medical disorders. CONCLUSIONS: The suffering associated with combat related-PTSD extends beyond the signs and symptoms of the disorder to broader areas of functional and social morbidity. The significantly higher risk of impaired functioning and diminished quality of life uniquely attributable to PTSD suggests that PTSD may well be the core problem in this group of difficult to treat and multiply afflicted patients. (Am J Psychiatry 1997; 154:1690–1695)
Posttraumatic stress disorder (PTSD) is a highly prevalent, often chronic, condition that afflicts both combat veterans (1, 2) and civilians (3, 4). Despite evidence that impaired functioning and diminished quality of life are debilitating outcomes in individuals suffering from other psychiatric disorders, the relationship between PTSD and functional status and quality of life remains incompletely understood. A series of large-scale, population-based reports has established that functional morbidity is associated with depressive, anxiety, and substance abuse disorders (5–9). None of these studies, however, examined PTSD. The fourth edition of DSM specifies for the first time that patients diagnosed with PTSD demonstrate “clinically significant distress or impairment in social, occupational, or other important areas of functioning” (DSM-IV). Therefore, comprehensive empirical documentation of the impact of PTSD on functioning and quality of life outcomes is now a research imperative (10, 11).
Most previous smaller-scale investigations suggest that traumatic events and perhaps PTSD may be associated with functional impairment in a variety of domains (12, 13). These include perceptions of poorer health and poorer physical health (14–16), greater violence and criminality (17), and poorer role and social functioning (18, 19). Yet, the literature to date relating traumatic events and PTSD to impaired functioning has a number of limitations. First, nearly all of these studies focus on a single outcome domain and therefore fail to elucidate for PTSD the profile of functional impairment that has been broadly defined for other psychiatric disorders (6, 8, 9). Second, previous investigations have not adjusted for comorbid psychiatric or other medical disorders that may account for the association between PTSD and poorer functional status. Last, no investigations have assessed the association between PTSD and physical limitations or days spent in bed, two important outcomes from a health policy perspective.
Thus, no empirical work exists that comprehensively assesses impairments in functioning and quality of life outcomes associated with combat-related PTSD. Our investigation addressed these questions through an archival analysis of data collected in the National Vietnam Veterans Readjustment Study (1). The National Vietnam Veterans Readjustment Study is, to date, the most comprehensive collection of information regarding the association of combat-related PTSD with functioning and quality of life. In earlier analyses of these data, higher levels of war zone stress exposure and greater PTSD symptom levels were shown to be generally associated with significantly more lifetime readjustment problems (1, 20–22).
The present study extends the initial findings of the National Vietnam Veterans Readjustment Study in three ways. First, we used variables that related PTSD assessed at the time of interview to functioning and quality of life also assessed at the time of interview and did not include historical variables such as lifetime diagnoses or Vietnam war zone stress exposure. Second, we analyzed multiple outcome domains and report on two outcomes that were not analyzed in the results of the original study: current physical limitations and bed days. Third, we adjusted for comorbid psychiatric and other medical disorders in order to clarify associations between PTSD and functional outcomes. Our hypothesis was that having PTSD at the time of the interview would be strongly associated with poorer outcomes across domains and that the association would remain even after adjustment for the effects of comorbid psychiatric and other medical conditions.
METHOD
Subjects
The National Vietnam Veterans Readjustment Study was completed in the late 1980s and included a cohort of 1,200 male veterans of the Vietnam theater (those veterans who served in Vietnam or its surrounding waters or airspace). Each participant completed the National Survey of the Vietnam Generation, a household interview lasting approximately 5 hours. After complete description of the study to the subjects, written informed consent was obtained. The survey response rate was 83%. Previous analyses demonstrated no important differences between respondents and nonrespondents (22).
These subjects were a nationally representative, probability sample of all 3.1 million male veterans who served in Vietnam (1). National Vietnam Veterans Readjustment Study estimates of the distribution of selected sociodemographic characteristics have been reported previously (1). Most veterans were middle aged and married at the time of the interview. Over 50% of subjects had attended some college. Approximately 17% of veterans were from African American or Hispanic ethnic backgrounds.
PTSD Diagnosis
PTSD symptom level at the time of interview was assessed with the Mississippi Scale for Combat-Related Posttraumatic Stress Disorder (23), a 35-item self-report questionnaire that includes assessment of intrusion, avoidance, and arousal symptoms, derived from DSM criteria for the disorder. For this study a cutoff score of 94 was used as the threshold for estimating a diagnosis of current PTSD. This cutoff yields a prevalence rate for PTSD of 15.3%, compared to the 15.2% rate reported in the National Vietnam Veterans Readjustment Study, which used a more complex and accurate diagnostic algorithm not available for our approach to the data set. In a subsample of the National Vietnam Veterans Readjustment Study of 316 male veterans, the Mississippi scale cutoff of 94 yielded a sensitivity of 75% and specificity of 84% when compared to PTSD diagnosis by expert clinicians using a structured clinical interview (24). When this cutoff was used, 242 subjects met criteria for PTSD, while 948 did not; 10 subjects did not adequately complete the scale and were therefore excluded from the analyses.
Nonpsychiatric Medical Comorbidity
Comorbid nonpsychiatric medical conditions at the time of the survey were assessed by responses to interviewer questions. Male veterans were asked if in the past 12 months they had been bothered by any one of over 30 chronic medical conditions (e.g., asthma, arthritis, diabetes, hypertension, stroke, atherosclerosis, cancer, cirrhosis, hepatitis, peptic ulcer disease, anemia, chronic skin conditions such as eczema or psoriasis, kidney disease, urinary tract or prostate difficulties, deafness, blindness, seizures, paralysis, amputation, or any other condition that seriously affected their health). These items were summed, and the result was rescaled to yield a 0–4-point scale in which any sum of four or greater was assigned a value of four. The original results revealed that approximately 60% of subjects reported one or more chronic nonpsychiatric medical conditions (1).
Psychiatric Comorbidity
Psychiatric disturbances at the time of the interview were diagnosed with the National Institute of Mental Health Diagnostic Interview Schedule version III-A (25). We were interested only in disorders occurring within the past 6 months; prevalences were previously reported to be 2.8% for depression, 11.2% for alcohol abuse or dependence, 1.8% for drug abuse or dependence, and 0.9% for panic disorder (1).
Outcome Definition and Measurement
Outcome variables were derived from a variety of survey-based questions; all outcomes were defined as dichotomous variables. In order to focus on concurrent relationships we selected outcomes that were contemporaneous with or only a year before the interview. We report the following six outcome domains.
1. Bed day in the past 2 weeks. Bed days were assessed from a single survey item that asked subjects, “When was the last time you had to stay in bed all or part of the day because of physical illness or injury?” Responses to this question were used to classify respondents into two categories: “Yes” (any bed day in the last 2 weeks) or “No” (no bed day in the past 2-week period).
2. Working versus not working (role functioning). A single question assessed subjects' ability to function in a particular role on the job, at home, or in school. Those subjects who were gainfully employed (N=1,033) or active with schoolwork (N=2) or housework (N=2) were categorized as working (26). Subjects reporting unemployment (N=61), permanent layoff or inability to work because of disability (N=40), or institutionalization (N=9) were categorized as not working. Subjects who were retired (N=18) or temporarily off work (N=29) were excluded from this analysis. In bivariate analyses neither retirement (p=0.38, Fisher's exact test) (27) nor being temporarily off work (p=0.07, Fisher's exact test) was significantly associated with current PTSD.
3. Subjective well-being. The items on this scale were derived from two national studies of the American population that focused on questions of well-being and satisfaction with life experience (28). The scale combined two 3-point items that assessed subjects' overall satisfaction with their life and their sense of well-being. The final outcome variable was dichotomous, with scores on the sum of the two items of 2 or 3 as one category and 4, 5, or 6 as the other. The former category was conceptualized as diminished subjective well-being and the latter as moderate to good subjective well-being.
4. Self-reported physical health status. Physical health status was assessed from a single survey item, “Would you say your physical health in general is excellent, very good, good, fair, or poor?” Responses were dichotomized into fair/poor versus good/very good/excellent.
5. Current physical functioning. Current physical functioning was assessed with the Rand Health Insurance Experiment 14-item functional limitations battery (29). The 14 interview items target limitations in self-care activities (feeding, bathing, dressing, and using the toilet), mobility (getting around indoors, outdoors, or in the community), physical activities (running, walking, using stairs, lifting, bending), and role activities (work, school, or household activities) and inability to engage in leisure activities (hobbies, clubs, or sports). Subjects who responded positively to at least one of the items were categorized as having a current physical limitation.
6. Perpetration of violent interpersonal acts in the past year. The severe violence scale of the Conflict Tactics Scale (30) was used to assess interpersonal violence. Six questions graded by severity of perpetration were included. These ranged from “During the past year, how often did you kick, bite, or hit someone with a fist?” to “During the past year, how often did you actually use a knife or a gun on another person?” Responses were dichotomized as either acknowledging at least one violent event in the past year or denying any violent event in the past year.
Data Analysis
The National Vietnam Veterans Readjustment Study data were obtained by a stratified random sampling strategy that violates the simple random sampling assumptions of the common statistical packages. In this situation, common statistical procedures would produce accurate point estimates (when properly weighted) but inaccurate (typically underestimated) variances, with the consequence of type I errors in statistical tests (31). Therefore, we performed all statistical tests presented in the tables by using SUDAAN (32), a software package for the analysis of survey data. SUDAAN uses a first-order Taylor series approximation to estimate variance for data sampled under complex survey designs. Prevalences, odds ratios, and confidence intervals presented in the tables are weighted to be nationally representative estimates for all Vietnam veterans. Sample sizes are unweighted.
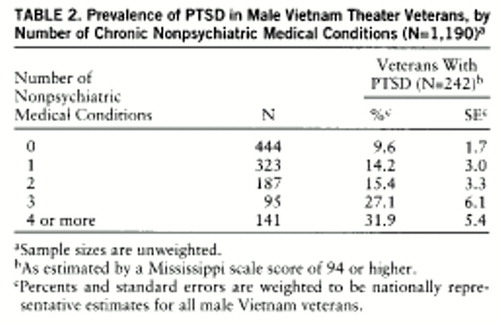
Previous analyses from the National Vietnam Veterans Readjustment Study demonstrated higher risks of comorbid psychiatric and other medical illness in subjects with PTSD than in subjects without PTSD (1). In order to better understand the role of comorbid disorders as potential confounders in the relationship between PTSD and functional outcomes, we assessed the prevalence of PTSD in subjects with comorbid psychiatric and other medical disorders.
For each of the six outcomes (e.g., bed day in the past 2 weeks) we ascertained the bivariate associations between PTSD and the outcome. We then constructed six separate logistic regression models (one for each dichotomous outcome variable). We entered the following independent variables into each of the six logistic models: 1) demographic characteristics including age, ethnicity, marital status, educational attainment, and region of country; 2) comorbid disorders including psychiatric disorders (i.e., major depression, alcohol abuse or dependence, drug abuse or dependence, and panic disorder) and other medical conditions; and 3) PTSD. Variables were entered into each logistic model simultaneously.
RESULTS
The prevalence of PTSD was markedly greater in subjects with current comorbid psychiatric disorders than in subjects without current psychiatric comorbidity (table 1). Indeed, most subjects with depression, panic disorder, or drug abuse also met criteria for PTSD, as did about one in three subjects with alcohol abuse. These results demonstrate how frequently PTSD co-occurs with affective, substance abuse, and anxiety disorders in this cohort of male Vietnam veterans.
The prevalence of PTSD also increased consistently with the number of self-reported chronic diseases (table 2). Only 9.6% of subjects reporting no chronic conditions had PTSD, whereas 31.9% of subjects with four or more conditions had PTSD.
We next examined the relationships among the functional outcomes. The correlations among the outcome measures ranged from 0.03 to 0.47. Only the 0.47 correlation, that of current physical functioning and self-reported physical health status, exceeded 0.35, suggesting that the outcome domains were neither orthogonal nor so highly correlated that they could serve as proxies for one another. Thus, we used each one separately.
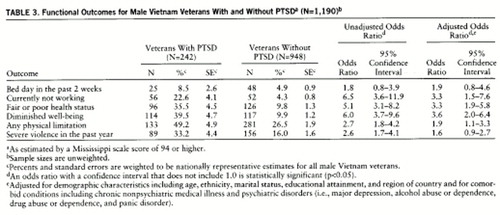
Subjects with PTSD demonstrated consistently higher risks of functional impairment; for five of the six outcomes the risks of impaired functioning in those with PTSD exceeded 20% (table 3). Poorer outcomes were significantly more common in subjects with PTSD than in subjects without PTSD in all domains except bed day in the past 2 weeks (table 3).
Adjustment for demographic characteristics and comorbid psychiatric and other medical disorders in logistic models showed that subjects with PTSD continued to have a statistically significant higher risk of diminished well-being, fair or poor physical health, currently not working, and physical limitations than did veterans without PTSD (table 3). For bed day in the past 2 weeks and perpetration of severe violence in the past year, the comparisons between subjects with PTSD and without PTSD did not achieve statistical significance.
DISCUSSION
This investigation demonstrates that PTSD is associated with a broad spectrum of functional impairment that includes diminished well-being, compromised physical health, physical limitations, greater perpetration of violence, and currently not working. These findings in this nationally representative sample of male Vietnam veterans suggest that the suffering associated with combat-related PTSD extends beyond the signs and symptoms of the disorder to multiple domains of functional impairment. The impairments in physical health and functioning, role functioning, social functioning, and emotional well-being not only reflect diminished quality of life for individual veterans, but also have marked and measurable costs to society through more days spent off work, unemployment, and interpersonal violence. It is also likely that these impairments are associated with greater health care utilization (1, 33, 34).
The associations between PTSD and poorer functional outcomes are clearly evident even with the most conservative modeling that assesses the unique effects of PTSD after shared effects due to comorbid psychiatric and other medical conditions are removed. Only two outcomes, bed days and perpetration of severe violence, were not significantly associated with PTSD after control for these other factors.
There are a number of important considerations in interpreting the results of our investigation. We note that in this cross-sectional study we cannot determine the historical development of PTSD relative to comorbid psychiatric disorders or functional limitations. In those cases in which PTSD developed before and may be causally related to comorbid conditions, our final models may be somewhat conservative and provide underestimates of the strength of the association between PTSD and functional impairment. Similar considerations regarding causality apply to the outcome variables as well. For instance, unemployment may affect psychological well-being. Thus, unemployment may worsen PTSD symptoms (35).
We used self-reports to assess both predictor and outcome variables. Currently there is some debate as to the validity of self-reported outcomes in the assessment of quality of life among patients suffering psychiatric disorders (36, 37). We used previously validated scales or scale items to assess physical limitations (29), severe violence (30), and well-being (28). Previous investigations suggest that physical health status and bed days are valid as self-reported measures. Self-reports of poorer physical health status are associated with poorer clinical outcomes including mortality (34). Self-reports of bed days are associated with objective measures of health care utilization (6) and hospitalization (38).
Use of the self-report Mississippi scale score as the sole indicator of PTSD ordinarily would raise concerns about diagnostic accuracy. However, our ability to compare the sensitivity and specificity of the Mississippi scale scores with structured clinical interview diagnoses from expert clinicians in the same data set, in conjunction with our use of a cutoff that yields the same prevalence estimate of current PTSD as that of the National Vietnam Veterans Readjustment Study, reduces these concerns substantially.
Beyond these methodological considerations, this study clearly demonstrates that like other major psychiatric syndromes, PTSD is associated with a broad profile of functional impairment and a diminished quality of life. Furthermore, the combined observations of significantly elevated risk of poorer outcomes in subjects with PTSD even after adjustment for comorbid disorders, and high prevalences of PTSD in subjects with comorbid disorders, suggests that PTSD contributes substantially to the functional impairment observed in this nationally representative cohort of male veterans.
These findings raise questions regarding the extent to which functional impairment previously attributed to depression, substance abuse, anxiety disorders, or other medical conditions may actually be posttraumatic sequelae in populations exposed to trauma. These questions are germane not only among combat veterans, but also among America's civilian populations in which there is mounting evidence that traumatic events and PTSD are endemic (3, 39, 40). Reports from the National Vietnam Veterans Readjustment Study (1, 22) and other studies (39, 41, 42), including most recently the National Comorbidity Survey (3), have documented high rates of psychiatric disorders other than PTSD in exposed populations. Kessler et al. (3) reported that in men, PTSD occurs as a primary disorder before other psychiatric comorbidity between 29% and 51% of the time. Thus, as health services and treatment outcomes researchers study the individual suffering, impaired functioning, and costly social morbidity associated with psychiatric disorders in populations exposed to trauma, they will need to consider that in many instances PTSD may well be the core disorder contributing to any observed functional impairments or diminished quality of life.
 |
 |
 |
Presented in part at the Robert Wood Johnson Clinical Scholars National Meeting, Fort Lauderdale, Fla., Nov. 8–11, 1995. Received Aug. 8, 1996; revision received June 4, 1997; accepted July 17, 1997. From the Robert Wood Johnson Clinical Scholars Program, University of California, San Francisco and Los Angeles; VA Medical Center, San Francisco; and Departments of Psychiatry and General Internal Medicine and Institute for Health and Aging, University of California, San Francisco. Address reprint requests to Dr. Zatzick, Department of Psychiatry, University of California, Davis Medical Center, 4430 V St., Sacramento, CA 95817. Supported in part by the Department of Veterans Affairs and the Robert Wood Johnson Foundation.
1. Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS: Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. New York, Brunner/Mazel, 1990Google Scholar
2. Health status of Vietnam veterans, I: psychosocial characteristics: the Centers for Disease Control Vietnam Experience Study. JAMA 1988; 259:2701–2707Google Scholar
3. Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB: Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995; 52:1048–1060Google Scholar
4. Breslau N, Davis GC, Andreski P, Peterson E: Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry 1991; 48:216–222Crossref, Medline, Google Scholar
5. Sherbourne CD, Wells KB, Judd LL: Functioning and well-being of patients with panic disorder. Am J Psychiatry 1996; 153:213–218Link, Google Scholar
6. Wells KB, Stewart A, Hays RD, Burnam MA, Rogers W, Daniels M, Berry S, Greenfield S, Ware J: The functioning and well-being of depressed patients: results from the Medical Outcomes Study. JAMA 1989; 262:914–919Crossref, Medline, Google Scholar
7. Markowitz JS, Weissman MM, Ouellette R, Lish JD, Klerman GL: Quality of life in panic disorder. Arch Gen Psychiatry 1989; 46:984–992Crossref, Medline, Google Scholar
8. Ormel J, VonKorff M, Ustun TB, Pini S, Korten A, Oldehinkel T: Common mental disorders and disability across cultures: results from the WHO Collaborative Study on Psychological Problems in General Health Care. JAMA 1994; 272:1741–1748Google Scholar
9. Spitzer RL, Kroenke K, Linzer M, Hahn SR, Williams JBW, DeGruy FV III, Brody D, Davies M: Health-related quality of life in primary care patients with mental disorders: results from the PRIME-MD 1000 Study. JAMA 1995; 274:1511–1517Google Scholar
10. Hales RE, Zatzick DF: What is PTSD? (editorial). Am J Psychiatry 1997; 154:143–145Link, Google Scholar
11. Group for the Advancement of Psychiatry Committee on Psychopathology: Taking issue: outcomes assessment and psychiatric services (editorial). Psychiatr Serv 1994; 45:1165Link, Google Scholar
12. Warshaw MG, Fierman E, Pratt L, Hunt M, Yonkers KA, Massion AO, Keller MB: Quality of life and dissociation in anxiety disorder patients with histories of trauma or PTSD. Am J Psychiatry 1993; 150:1512–1516Google Scholar
13. Conway T, Hu TC, Warshaw C, Kim P, Bullon A: Violence victims' perception of functioning and well-being: a survey from an urban public hospital walk-in clinic. J Natl Med Assoc 1995; 87:407–412Medline, Google Scholar
14. Friedman M, Schnurr P: The relationship between trauma, post-traumatic stress disorder and physical health, in Neurobiological and Clinical Consequences of Stress: From Normal Adaptation to Post-Traumatic Stress Disorder. Edited by Friedman M, Charney D. Philadelphia, Lippincott-Raven, 1995, pp 507–524Google Scholar
15. Wolfe J, Schnurr PP, Brown PJ, Furey J: Posttraumatic stress disorder and war-zone exposure as correlates of perceived health in female Vietnam war veterans. J Consult Clin Psychol 1994; 62:1235–1240Google Scholar
16. Golding J: Sexual assault history and limitations in physical functioning in two general population samples. Res Nurs Health 1996; 19:33–44Crossref, Medline, Google Scholar
17. Chemtob CM, Hamada RS, Roitblat HL, Muraoka MY: Anger, impulsivity, and anger control in combat-related posttraumatic stress disorder. J Consult Clin Psychol 1994; 62:827–832Crossref, Medline, Google Scholar
18. Jordan BK, Marmar CR, Fairbank JA, Schlenger WE, Weiss DS, Hough RL, Kulka RA: Problems in families of male Vietnam veterans with posttraumatic stress disorder. J Consult Clin Psychol 1992; 60:916–926Crossref, Medline, Google Scholar
19. Carroll EM, Rueger DB, Foy DW, Donahoe CP: Vietnam combat veterans with posttraumatic stress disorder: analysis of marital and cohabitating adjustment. J Abnorm Psychol 1985; 94:329–337Crossref, Medline, Google Scholar
20. Rosenheck R, Fontana A: A model of homelessness among male veterans of the Vietnam War generation. Am J Psychiatry 1994; 151:421–427Link, Google Scholar
21. Fontana A, Rosenheck R: Attempted suicide among Vietnam veterans: a model of etiology in a community sample. Am J Psychiatry 1995; 152:102–109Link, Google Scholar
22. Jordan BK, Schlenger WE, Hough RL, Kulka RA, Fairbank JA, Marmar DS, Marmar CM: Lifetime and current prevalence of specific psychiatric disorders among Vietnam veterans and controls. Arch Gen Psychiatry 1991; 48:207–215Crossref, Medline, Google Scholar
23. Keane TM, Caddell JM, Taylor KL: Mississippi Scale for Combat-Related Posttraumatic Stress Disorder: three studies in reliability and validity. J Consult Clin Psychol 1988; 56:85–90Crossref, Medline, Google Scholar
24. Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-III-R—Non-Patient Version (SCID-NP). New York, New York State Psychiatric Institute, Biometrics Research, 1987Google Scholar
25. Robins LN, Helzer JE, Croughan J, Ratcliff KS: The National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Arch Gen Psychiatry 1981; 38:381–389Crossref, Medline, Google Scholar
26. Stewart A, Ware J (eds): Measuring Functioning and Well-Being: The Medical Outcomes Study Approach. Durham, NC, Duke University Press, 1992Google Scholar
27. Fleiss JL: Statistical Methods for Rates and Proportions, 2nd ed. New York, John Wiley & Sons, 1981Google Scholar
28. Veroff J, Douvan E, Kulka RA: The Inner American: A Self-Portrait From 1957–1976. New York, Basic Books, 1981Google Scholar
29. Stewart A, Ware J, Brook R: Construction and Scoring of Aggregate Functional Status Measures, vol 1. Santa Monica, Calif, Rand Corp, 1982Google Scholar
30. Straus M: The conflict tactics scale and its critics: an evaluation and new data on validity and reliability, in Physical Violence in American Families: Risk Factors and Adaptation to Violence in 8,145 Families. Edited by Straus M, Gelles R. New Brunswick, NJ, Transaction, 1990, pp 49–73Google Scholar
31. Lee ES, Forthofer RN, Lorimor RJ: Analysis of complex sample survey data: problems and strategies. Sociological Methods and Research 1986; 1–2:69–100Google Scholar
32. Shah B, Folsom R, Lavange L, Boyle K, Wheeles S, Williams R: Statistical Methods and Mathematical Algorithms Used in SUDAAN. Research Triangle Park, NC, Research Triangle Institute, 1993Google Scholar
33. Rosenheck R, Fontana A: Do Vietnam-era veterans who suffer from posttraumatic stress disorder avoid VA mental health services? Milit Med 1995; 160:136–142Google Scholar
34. Wilson IB, Cleary PD: Linking clinical variables with health-related quality of life: a conceptual model of patient outcomes. JAMA 1995; 273:59–65Crossref, Medline, Google Scholar
35. Ezzy D: Unemployment and mental health: a critical review. Soc Sci Med 1993; 37:41–52Crossref, Medline, Google Scholar
36. Health status of Vietnam veterans, II: physical health: the Centers for Disease Control Vietnam Experience Study. JAMA 1988; 259:2708–2714Google Scholar
37. Atkinson M, Zibin S, Chuang H: Characterizing quality of life among patients with chronic mental illness: a critical examination of the self-report methodology. Am J Psychiatry 1997; 154:99–105Link, Google Scholar
38. Wagner EH, Lacoix AZ, Grothaus LC, Hecht JA: Responsiveness of health status measures to change among older adults. J Am Geriatr Soc 1993; 41:241–248Crossref, Medline, Google Scholar
39. Breslau N, Davis GC: Posttraumatic stress disorder in an urban population of young adults: risk factors for chronicity. Am J Psychiatry 1992; 149:671–675Link, Google Scholar
40. Norris FH: Epidemiology of trauma: frequency and impact of different potentially traumatic events on different demographic groups. J Consult Clin Psychol 1992; 60:409–418Crossref, Medline, Google Scholar
41. Fierman EJ, Hunt MF, Pratt LA, Warshaw MG, Yonkers KA, Peterson LG, Epstein-Kaye TM, Norton HS: Trauma and posttraumatic stress disorder in subjects with anxiety disorders. Am J Psychiatry 1993; 150:1872–1874Google Scholar
42. Cottler LB, Compton WM III, Mager D, Spitznagel EL, Janca A: Posttraumatic stress disorder among substance users from the general population. Am J Psychiatry 1992; 149:664–670Link, Google Scholar



