Deliberate Self-Harm in a Nonclinical Population: Prevalence and Psychological Correlates
Abstract
OBJECTIVE: Research on deliberate self-harm (intentionally injuring oneself without suicidal intent) has focused on clinical and forensic populations. Studying only these populations, which typically have serious psychopathology, may lead to inflated estimates of the association between self-harm and psychiatric disorder, as well as of the prevalence of deliberate self-harm. The present study investigated the prevalence and correlates of deliberate self-harm in a large group of nonclinical subjects. METHOD: Participants were 1,986 military recruits, 62% of whom were men, who were participating in a study of peer assessment of personality traits and pathology. Individuals who did and did not report a history of self-harm were compared on measures of personality and psychopathology. RESULTS: Approximately 4% of the participants reported a history of deliberate self-harm. Compared with participants without a history of deliberate self-harm, self-harmers scored higher on self- and peer-report measures of borderline, schizotypal, dependent, and avoidant personality disorder symptoms and reported more symptoms of anxiety and depression. Item-level analyses indicated that peers viewed self-harmers as having strange and intense emotions and a heightened sensitivity to interpersonal rejection. CONCLUSIONS: About one of every 25 members of a large group of relatively high-functioning nonclinical subjects reported a history of self-harm. Self-harmers had more symptoms of several personality disorders than non-self-harmers, and their performance across measures suggested that anxiety plays a prominent role in their psychopathology. Future research should investigate whether psychotherapies or psychiatric medications known to reduce symptoms of anxiety can be effective in treating deliberate self-harm.
Deliberate self-harm is defined as the intentional injuring of one’s own body without apparent suicidal intent (1). Other names for this behavior include superficial-moderate self-mutilation (2), self-injurious behavior (3, 4), parasuicide (5), and self-wounding (6). Deliberate self-harm is encountered frequently in psychiatric hospitals (7) and also in outpatient settings (8). Deliberate self-harm may be found in patients with a variety of diagnoses, including substance abuse, eating disorders, posttraumatic stress disorder, major depression, anxiety disorders, and schizophrenia (9, 10), as well as each of the personality disorders (11) and especially borderline personality disorder (4, 10, 12, 13).
Deliberate self-harm occurs in nonclinical populations as well. Approximately 4% of the general population (14) and 14% of college students (15) have reported a history of deliberate self-harm. A recent study found that as many as 35% of college students report having performed at least one self-harm behavior in their lifetime (16). There is evidence that deliberate self-harm has become more prevalent in recent years. Several studies have found higher rates of self-harm in individuals from younger generations (10, 14, 17, 18).
Efforts to develop a taxonomy of deliberate self-harm behaviors have been under way for more than three decades (e.g., references 1, 2, 19, 20). Nevertheless, the only mention of deliberate self-harm in DSM-IV-TR is as a symptom of borderline personality disorder. Although research findings are consistent with the idea that deliberate self-harm is an important symptom of borderline personality disorder, studies have also indicated that self-harm occurs across a variety of diagnoses, as well as in nonclinical subjects. As a result, many researchers study deliberate self-harm as a behavioral phenomenon in its own right, rather than as a symptom of borderline personality disorder. This approach—studying a particular psychological phenomenon rather than the diagnosis with which it is associated—may be particularly suited to the investigation of behaviors with poorly understood underlying mechanisms (21). At present, a basic understanding of self-harm, including its classification, diagnosis, and treatment, is still lacking.
Better understanding of deliberate self-harm is important for effective management of this behavior (22). There are no proven treatments (23). Dialectical behavior therapy has shown promise for reducing the number of deliberate self-harm episodes and hospitalizations in women with borderline personality disorder, although more research is needed to determine the extent of the efficacy of this intervention, the reasons for its efficacy, and the degree to which it should be adopted in community mental health settings (23, 24). Unfortunately, it is not uncommon for therapists to become frustrated or upset by a patient’s self-harm, and many therapists have to manage their own reactions even as they attempt to manage the self-harm behaviors of their patients (25, 26). To improve clinical practice, it is important to increase our knowledge of deliberate self-harm.
What we do know about deliberate self-harm comes primarily from research with patient populations. Skin cutting appears to be the most common form of deliberate self-harm, occurring in at least 70% of individuals who deliberately harm themselves (3, 14, 27–29). Between 21% and 44% of self-harmers bang or hit themselves, and between 15% and 35% burn their skin (3, 27–29). Most individuals who deliberately harm themselves use more than one method (3, 16, 27). Age at onset typically is between 14 and 24 years (3, 27).
It is unclear whether self-harm is more common in women than in men, although some researchers appear to take for granted that self-harm is more common in women (e.g., references 5, 30). Studies of adults in clinical settings have reported inconsistent results. Whereas Zlotnick et al. (10) found higher rates of deliberate self-harm in women, several other studies found self-harm to be equally prevalent in men and women (13, 14, 18, 29). Two studies of nonclinical subjects also did not find gender differences (14, 16).
Reports of associations between deliberate self-harm and psychopathological variables are pervasive in the literature. Findings linking deliberate self-harm and borderline personality traits (11, 31, 32), suicidality (3, 18, 28, 33, 34), dissociation (4, 10, 14, 17, 29, 31, 32, 34, 35), and anxiety (12–14, 34) (but see reference 33) have been replicated frequently. Posttraumatic stress disorder also appears to occur more frequently in patients who harm themselves (17).
Findings regarding substance abuse, depression, and eating disorders are less clear. Several studies have reported associations between substance abuse and deliberate self-harm (10, 28, 34), but other studies have not confirmed this relationship (18, 33). Mixed results have also been found for depression. Whereas elevated levels of depression are often reported in self-harmers (3, 13, 14), two studies did not find effects for depression (12, 35). Self-harmers do not appear more likely to have a diagnosis of major depression (13, 18) (but see reference 33). Some evidence indicates that major depression is less common in psychiatric patients who deliberately harm themselves than non-self-harming patients (11, 28). Results regarding eating disorders are also equivocal. Higher rates of eating disorders in deliberate self-harm patients have been reported (33, 34), but Zlotnick et al. (10) found no relationship between self-harm and eating disorders. A study of female inpatients with eating disorders found a 35% lifetime rate of self-injury (36). This study did not include a comparison group, however, so it is unclear whether this figure is higher than the prevalence of self-harm in female psychiatric inpatients in general.
Suggestions of an important link between deliberate self-harm and childhood trauma have a long history (e.g., reference 19). Evidence for this association is ample (4, 13, 14, 17, 28, 29, 31, 34, 37, 38). There is also evidence that patients who deliberately harm themselves experience more traumatic events as adults (34, 38). It should be noted, however, that not all studies have confirmed a link between deliberate self-harm and childhood trauma (32, 35).
The studies summarized here have some limitations in their generalizability and scope. For example, these studies focused on clinical populations disposed to major forms of psychopathology. Studies involving such subjects may inflate the association between deliberate self-harm and psychopathology, as well as the prevalence of deliberate self-harm. Investigations of self-harm in people without major psychiatric disorders may better elucidate the nature of deliberate self-harm. Another shortcoming is that existing studies have focused on associations between deliberate self-harm and axis I disorders or borderline personality disorder, but they have not investigated links with other personality disorders or normal personality traits. Establishing both the pathological and normal personality correlates of deliberate self-harm would aid in the diagnosis and treatment of individuals who deliberately harm themselves. Finally, studies of deliberate self-harm have relied on interviews or the self-reports of participants to measure psychological variables. Unfortunately, verbal reports about one’s own mental processes can be inaccurate and misleading (39). People are frequently unable to view themselves realistically. There is, at best, a modest correlation between the ways in which people describe themselves and the ways in which they are perceived by others (40, 41). Assessing the personality and psychopathology of self-harmers through instruments that do not rely on self-reports could improve the validity of the findings.
The present analyses were conceived in response to these limitations. We examined deliberate self-harm in a large group of nonclinical subjects who are not disposed to major psychopathology (military recruits), investigated the relationship between deliberate self-harm and all 10 DSM-IV personality disorders as well other pathological and nonpathological traits, and utilized both self-reports and peer reports to assess personality disorders.
Method
Participants
The participants were 1,986 Air Force recruits, 62% of whom were men, who were participating in a larger study of the peer assessment of personality traits and pathology (42, 43). All participants signed informed consent agreements that described the study and informed them that participation was voluntary. The participants were enlisted men and women who would eventually receive assignments as military police, mechanics, computer technicians, or other support services personnel. Their mean age was 20 years (SD=5), their mean IQ was 104, and 99% were high school graduates. Sixty-five percent of the participants were Caucasian, 17% were African American, 4% were Hispanic, 3% were Asian, 1% were Native American, and 10% listed their race as “other.” Twenty-five recruits who reported a history of attempted suicide were not included in the study to ensure that only self-harm without suicidal intent would be analyzed. An additional 20 participants were not included because they scored more than two standard deviations above the mean on the Invalidity Index of the Schedule for Nonadaptive and Adaptive Personality (44).
The participants were members of 50 “flights,” groups of 35–52 recruits who go through basic training together. Fourteen of these flights were single-sex male flights, four were single-sex female flights, and 32 were mixed-gender flights. Recruits in a given flight spend almost all of their time together and get to know each other quite well. After a complete description of the study to the subjects, written informed consent was obtained.
Measures
Schedule for Nonadaptive and Adaptive Personality
The Schedule for Nonadaptive and Adaptive Personality is a self-report questionnaire derived from factor analysis (44). It is composed of 375 true/false items designed to assess trait dimensions in the domain of personality pathology. It includes 12 trait scales, three temperament scales, six validity scales, and diagnostic scales that measure the symptoms of the 10 DSM-IV personality disorders. Dimensional scores from the diagnostic, temperament, and trait scales were used to measure personality disorder symptoms and other pathological and nonpathological personality traits.
Deliberate self-harm
Two items from the Schedule for Nonadaptive and Adaptive Personality were used to measure deliberate self-harm. The items were 1) “When I get very tense, hurting myself physically somehow calms me down” and 2) “I have hurt myself on purpose several times.” Participants who endorsed either item were considered to have a history of intentional self-harm. As mentioned earlier, recruits who endorsed the item, “I have tried to commit suicide,” were not included in this study so that only self-harm without suicidal intent would be investigated.
Peer Inventory of Personality Disorders
The Peer Inventory of Personality Disorders was created specifically for a larger project on the peer assessment of personality traits and pathology (43). It includes 105 items that describe specific personality characteristics. Eighty-one items are based on the DSM-IV features of personality disorders. These items were constructed by translating the DSM-IV criteria into lay language. For example, the DSM-IV borderline criterion “inappropriate, intense anger or difficulty controlling anger (e.g., frequent displays of temper, constant anger, recurrent physical fights)” was translated as “has sudden, even violent outbursts of anger.” The remaining 24 items are based on positive characteristics and are mixed together with the personality disorder items to minimize the emphasis on pathological personality traits. For each item, participants were asked to nominate at least one member of their group who exhibited the characteristic in question.
In the present study, interrater reliability for Peer Inventory of Personality Disorders scores (i.e., the average correlation between two participants for the sum of the items in a personality disorder scale) was found to be very good, ranging from 0.67 for schizoid personality disorder to 0.91 for narcissistic personality disorder (45). Agreement between peer- and self-reports of personality disorder features has tended to be modest at best (41). The r values for the correlation of peer- and self-reports were between 0.21 and 0.30 in the present study (43).
Beck Depression Inventory and Beck Anxiety Inventory
The Beck Depression Inventory and Beck Anxiety Inventory served as measures of depression and anxiety. The Beck Depression Inventory is a 21-item instrument that measures cognitions and symptoms often observed in depressed inpatients (46). It is a widely used screening tool for depression. The Beck Anxiety Inventory is a 21-item instrument that assesses the severity of anxiety symptoms (47).
Procedure
Participants were administered the Schedule for Nonadaptive and Adaptive Personality, the Peer Inventory of Personality Disorders, the Beck Depression Inventory, and the Beck Anxiety Inventory at the end of 6 weeks of basic training. Members of each basic training group were tested simultaneously in a large computer lab during a single 2-hour session. Each participant sat at a workstation with a computer. The Peer Inventory of Personality Disorders was presented on the computer screen. Items were listed one by one at the top of the computer screen, and the names of all other members of the group (excluding the name of the participant completing the Peer Inventory of Personality Disorders) appeared below each trait description. For each item, participants were asked to nominate members of their peer group who exhibited the characteristic in question by using the following scale: 0 (never this way), 1 (sometimes this way), 2 (usually this way), and 3 (always this way).
For each participant, the total number of nominations received on 10 sets of items (corresponding to the criteria for the 10 DSM-IV personality disorders) was computed. This number was then divided by the number of available nominators for each participant. This procedure ensured that participants in larger peer groups would not be scored as having more peer-reported personality pathology solely as a result of having more peers available to nominate them. Peer Inventory of Personality Disorders scores for the 10 sets of items corresponding to the 10 DSM-IV personality disorders were used as an index of peer-reported personality disorder.
Results
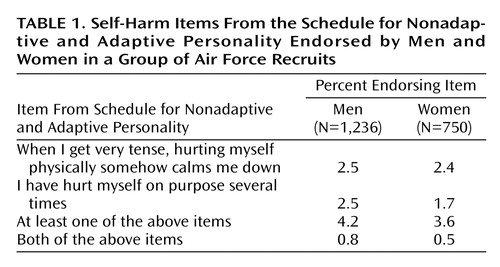
We first analyzed the percentage of participants endorsing the Schedule for Nonadaptive and Adaptive Personality self-harm items (Table 1). The item “When I get very tense, hurting myself physically somehow calms me down” was endorsed by 2.5% of the men and 2.4% of the women. The item “I have hurt myself on purpose several times” was endorsed by 2.5% of the men and 1.7% of the women. Approximately 4% of participants endorsed at least one of these items; less than 1% endorsed both items.
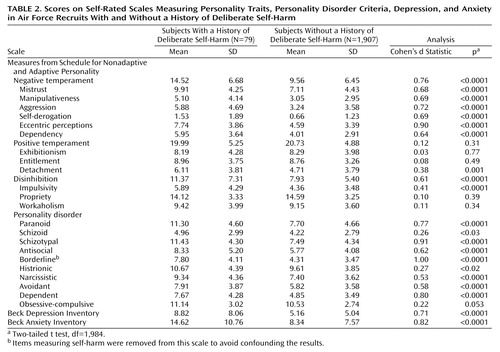
Next, participants who did and did not endorse a history of deliberate self-harm were compared on their mean scores on the 15 trait scales of the Schedule for Nonadaptive and Adaptive Personality, the 10 Schedule for Nonadaptive and Adaptive Personality diagnostic scales, the Beck Depression Inventory, and the Beck Anxiety Inventory (by using two-tailed t tests, df=1,984) (Table 2). Participants who reported a history of deliberate self-harm scored higher on negative temperament, mistrust, manipulativeness, aggression, self-derogation, eccentric perceptions, dependency, detachment, disinhibition, impulsivity, and all the DSM-IV personality disorder diagnostic scales, except for the obsessive-compulsive personality disorder scale. Analyses of variance (ANOVAs) indicated that none of the relations between deliberate self-harm and pathological personality features were different for women, compared with men.
Scores on the Beck Depression Inventory and the Beck Anxiety Inventory were also higher in the self-harm group. Post hoc ANOVAs indicated that gender moderated the relationship between deliberate self-harm and both depression (F=5.89, df=1, 1,982, p<0.02) and anxiety (F=5.53, df=1, 1,982, p<0.02). Differences between self-harmers and non-self-harmers on the depression and anxiety scales were larger for men than for women. Post hoc analyses also indicated that the Beck Anxiety Inventory maintained a substantial unique relationship to deliberate self-harm when the effects of depression were controlled (F=16.27, df=1, 1,983, p<0.0001). The association between depression and deliberate self-harm was considerably smaller after the effects of anxiety were controlled (F=4.02, df=1, 1,983, p<0.05).
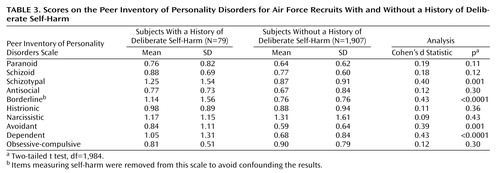
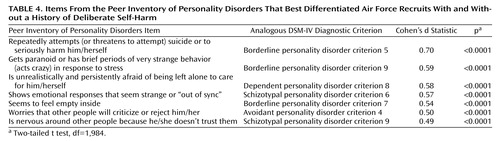
Mean scores on the 10 Peer Inventory of Personality Disorders scales for the participants who did and did not endorse a history of deliberate self-harm were compared by using two-tailed t tests (df=1,984) (Table 3). The participants who reported a history of deliberate self-harm received more peer nominations on the schizotypal, borderline, avoidant, and dependent personality disorder scales. No differences were found for the paranoid, schizoid, antisocial, histrionic, narcissistic, and obsessive-compulsive personality disorder scales. Last, we analyzed group differences on the Peer Inventory of Personality Disorders at the level of individual diagnostic criteria (Table 4). Compared to non-self-harmers, self-harmers were most often nominated by their peers for attempting suicide or serious self-harm (DSM-IV borderline personality disorder criterion 5), acting paranoid or crazy in response to stress (borderline personality disorder criterion 9), feeling unrealistically afraid of being left alone (dependent personality disorder criterion 8), showing strange emotional responses (schizotypal personality disorder criterion 6), feeling empty inside (borderline personality disorder criterion 7), worrying about social rejection (avoidant personality disorder criterion 4), and being nervous around and mistrustful of others (schizotypal personality disorder criterion 9).
Discussion
The present study examined the prevalence and correlates of deliberate self-harm in a large group of military recruits. Approximately 4% of the participants reported a history of self-harm, although less than 1% endorsed both items assessing deliberate self-harm. The lack of substantial concordance between responses to the items is not surprising. The first item, “When I get tense, hurting myself physically somehow calms me down,” conveys a specific function of self-harm (i.e., to calm oneself when tense) with which participants endorsing the second item, “I have hurt myself on purpose several times,” might not identify. Similarly, the second item would be endorsed only by those with a history of multiple deliberate self-harm episodes, whereas individuals who deliberately harmed themselves once or a few times might be more likely to relate to the content of the first item. It is likely that the participants endorsing both items have on average harmed themselves more chronically than those who endorsed only one item. Our pattern of results is consistent with that reported by Briere and Gil (14). They found that 4% of the general population in the United States indicated a history of deliberate self-harm, with 0.3% reporting that they had engaged in this behavior often.
Prevalence rates of deliberate self-harm in the present study were roughly equivalent for men and women. This finding is perhaps unexpected, since it is often reported that self-harm is more common in women than men (5, 30). Several studies, however, have not found a difference in the prevalence of self-harm for men and women (13, 14, 18, 29). This lack of a gender difference has also been found in studies involving nonclinical subjects (14, 16). Although these findings seem to run counter to clinical wisdom, prevalence rates of deliberate self-harm may indeed be similar for men and women.
Regarding the correlates of deliberate self-harm, military recruits with a history of deliberate self-harm reported substantially more personality pathology, including more features of all of the DSM-IV personality disorders except obsessive-compulsive personality disorder. These findings are consistent with studies indicating higher rates of personality disorder in psychiatric patients who deliberately harm themselves (11, 28). Moreover, self-harmers were perceived by their peers as exhibiting more features of the schizotypal, borderline, avoidant, and dependent personality disorders, compared to non-self-harmers. Our results support the DSM-IV classification of deliberate self-harm as a symptom of borderline personality disorder but also indicate that self-harm may be present in individuals with traits of other personality disorders. We can have some confidence in this pattern of results because it occurred regardless of whether personality disorder was assessed by using self- or peer reports. Unfortunately, no other studies with nonclinical subjects have examined the relationship between deliberate self-harm and personality disorders. It is therefore not possible to determine if these data can be generalized to other nonclinical populations.
A criterion-level analysis of the Peer Inventory of Personality Disorders yielded further insight into how self-harmers are perceived by their peers. Individuals who deliberately harmed themselves were more often nominated as having repeatedly attempted suicide or self-harm (DSM-IV borderline personality disorder criterion 5), acted paranoid or crazy in response to stress (borderline personality disorder criterion 9), been unrealistically afraid of being left alone (dependent personality disorder criterion 8), showed strange emotions (schizotypal personality disorder criterion 6), seemed to feel empty inside (borderline personality disorder criterion 7), worried about social rejection (avoidant personality disorder criterion 4), and been nervous around and mistrustful of others (schizotypal personality disorder criterion 9). Although self-harmers were distinguished by meeting some of the criteria for several personality disorders, a relatively coherent “self-harm personality profile” emerged. According to their peers, self-harmers tended to have strange and intense emotions and a heightened sensitivity to interpersonal rejection.
An unanticipated finding was that self-harmers and non-self-harmers scored equivalently on a measure of positive temperament. It appears that individuals who deliberately harm themselves do not differ in their capacity to experience positive affect, even though they have more pathological personality traits and a propensity for negative affect. This finding may be interpreted in the context of the tripartite model of anxiety and depression (48). The tripartite model states that both anxiety and depression are associated with negative affect, but only depression is distinguished by diminished positive affect. The absence of a relationship between positive temperament and deliberate self-harm may indicate that individuals who deliberately harm themselves are more anxious than depressed. Findings regarding depression and anxiety supported this model. While both depression and anxiety scores were higher in self-harmers than in non-self-harmers, anxiety maintained a substantial unique relationship to deliberate self-harm over and above depression. The association between depression and deliberate self-harm was considerably smaller after the analysis controlled for the effects of anxiety. These results may help in interpretation of findings regarding the functions of self-harm. Self-harmers have reported experiencing a sense of relief after episodes of deliberate self-harm (14), and there is physiological evidence that self-harmers experience a reduction in tension after an episode of self-harm (49). Taken together, the findings from past research and the present study suggest that self-harmers tend to be anxious and that self-harming is a method of reducing anxiety.
Our analyses also revealed that the relationships of deliberate self-harm with both depression and anxiety were different for men and women. There were stronger associations between self-harm and both depression and anxiety for men than for women. Although many studies of psychiatric patients have found higher levels of depression in self-harmers (3, 13, 14, 34), two studies that included only female subjects did not find self-harmers to be more depressed than comparison subjects (28, 35). Similarly, a study in which 79% of the participants were women did not find an association between anxiety and self-harm (33). It is possible that anxiety is more central to the psychopathology of male than female self-harmers. More research is needed, however, to investigate to what extent this pattern generalizes to clinical and other nonclinical populations.
This study contributes to the literature on deliberate self-harm in several ways. Perhaps most important, this study elucidated the axis II correlates of self-harm in a nonclinical population. Individuals reporting a history of self-harm had more traits of the borderline, schizotypal, dependent, and avoidant personality disorders as measured by both self- and peer reports. This study’s inclusion of nonclinical subjects may have allowed for a cleaner examination of the psychopathological correlates of self-harm than would be possible in studies involving psychiatric patients, who by definition have psychiatric disorders. Second, we presented data suggesting that self-harmers are better characterized as anxious than depressed. This finding contributes to our understanding of self-harm as a means for reducing anxiety and may help inform the development of interventions. For example, it may be useful to investigate the efficacy of psychotherapies or psychiatric medications known to reduce symptoms of anxiety. A third contribution of this study is that it provides converging evidence for findings reported by Briere and Gil (14) regarding the prevalence of deliberate self-harm. Findings from both their study and the present study indicated that approximately 4% of the nonclinical population has harmed themselves at least once, that less than 1% has chronically engage in self-harm, and that prevalence rates are similar for men and women. To our knowledge, no other studies have examined the prevalence of deliberate self-harm in a group of nonclinical subjects other than college students.
An important limitation of the present research was that the measurement of self-harm was based on two self-report items. A multi-item scale would have been more reliable. The validity of our items was supported by their strong relationship to peer reports of self-harm behaviors. Nevertheless, these items did not assess the type, frequency, or severity of deliberate self-harm. Ideally a standardized and comprehensive instrument for assessing self-harm behaviors would have been used. To our knowledge, no adequate measure exists, and there is a need for such an instrument to be developed (36). Perhaps the most important next step for future research on self-harm is the development of a detailed clinical interview to assess the presence, phenomenology, and functions of deliberate self-harm.
 |
 |
 |
 |
Received Sept. 17, 2002; revision received Jan. 10, 2003; accepted Jan. 13, 2003. From the Department of Psychology, University of Virginia, Charlottesville, Va. Address reprint requests to Dr. Turkheimer, Department of Psychology, University of Virginia, 102 Gilmer Hall, P.O. Box 400400, Charlottesville, VA 22904-4400; [email protected] (e-mail). Preparation of this paper was supported in part by NIMH grant MH-51187 and an NIMH National Research Service Award.
1. Pattison EM, Kahan J: The deliberate self-harm syndrome. Am J Psychiatry 1983; 140:867–872Link, Google Scholar
2. Favazza AR, Rosenthal RJ: Diagnostic issues in self-mutilation. Hosp Community Psychiatry 1993; 44:134–140Abstract, Google Scholar
3. Herpertz S: Self-injurious behavior: psychopathological and nosological characteristics in subtypes of self-injurers. Acta Psychiatr Scand 1995; 91:57–68Crossref, Medline, Google Scholar
4. van der Kolk BA, Perry JC, Herman JL: Childhood origins of self-destructive behavior. Am J Psychiatry 1991; 148:1665–1671Link, Google Scholar
5. Ogundipe LO: Suicide attempts vs deliberate self-harm (letter). Br J Psychiatry 1999; 175:90Crossref, Medline, Google Scholar
6. Tantam D, Whittaker J: Personality disorder and self-wounding. Br J Psychiatry 1992; 161:451–464Crossref, Medline, Google Scholar
7. Favazza AR: Why patients mutilate themselves. Hosp Community Psychiatry 1989; 40:137–145Abstract, Google Scholar
8. Suyemoto KL, MacDonald ML: Self-cutting in female adolescents. Psychotherapy 1995; 32:162–171Crossref, Google Scholar
9. Haw C, Hawton K, Houston K, Townsend E: Psychiatric and personality disorders in deliberate self-harm patients. Br J Psychiatry 2001; 178:48–54Crossref, Medline, Google Scholar
10. Zlotnick C, Mattia JI, Zimmerman M: Clinical correlates of self-mutilation in a sample of general psychiatric patients. J Nerv Ment Dis 1999; 187:296–301Crossref, Medline, Google Scholar
11. Herpertz S, Sass H, Favazza A: Impulsivity in self-mutilative behavior: psychometric and biological findings. J Psychiatr Res 1997; 31:451–465Crossref, Medline, Google Scholar
12. Simeon D, Stanley B, Frances A, Mann JJ, Winchel R, Stanley M: Self-mutilation in personality disorders: psychological and biological correlates. Am J Psychiatry 1992; 149:221–226Link, Google Scholar
13. Stanley B, Gameroff MJ, Michalsen V, Mann JJ: Are suicide attempters who self-mutilate a unique population? Am J Psychiatry 2001; 158:427–432Link, Google Scholar
14. Briere J, Gil E: Self-mutilation in clinical and general population samples: prevalence, correlates, and functions. Am J Orthopsychiatry 1998; 68:609–620Crossref, Medline, Google Scholar
15. Favazza AR, DeRosear L, Conterio K: Self-mutilation and eating disorders. Suicide Life Threat Behav 1989; 19:352–361Medline, Google Scholar
16. Gratz KL: Measurement of deliberate self-harm: preliminary data on the Deliberate Self-Harm Inventory. J Psychopathology and Behavioral Assessment 2001; 23:253–263Crossref, Google Scholar
17. Shearer SL: Phenomenology of self-injury among inpatient women with borderline personality disorder. J Nerv Ment Dis 1997; 182:524–526Google Scholar
18. Soloff PH, Lis JA, Kelly T, Cornelius J, Ulrich R: Self-mutilation and suicidal behavior in borderline personality disorder. J Personal Disord 1994; 8:257–267Crossref, Google Scholar
19. Graff H, Mallin R: The syndrome of the wrist cutter. Am J Psychiatry 1967; 124:36–42Link, Google Scholar
20. Rosenthal RJ, Rinzler C, Wallsh R, Klausner E: Wrist-cutting syndrome: the meaning of a gesture. Am J Psychiatry 1972; 128:1363–1368Link, Google Scholar
21. Persons JB: The advantages of studying psychological phenomena rather than psychiatric diagnoses. Am Psychol 1986; 41:1252–1260Crossref, Medline, Google Scholar
22. Himber J: Blood rituals: self-cutting in female psychiatric patients. Psychotherapy 1994; 31:620–631Crossref, Google Scholar
23. Linehan MM: The empirical basis of dialectical behavior therapy: development of new treatments versus evaluation of existing treatments. Clin Psychol Sci Practice 2000; 7:113–119Crossref, Google Scholar
24. Scheel KR: The empirical basis of dialectical behavior therapy: summary, critique, and implications. Clin Psychol Sci Practice 2000; 7:68–96Crossref, Google Scholar
25. Favazza AR: Repetitive self-mutilation. Psychiatr Annals 1992; 22:60–63Crossref, Google Scholar
26. Feldman MD: The challenge of self-mutilation: a review. Compr Psychiatry 1988; 29:252–269Crossref, Medline, Google Scholar
27. Favazza AR, Conterio K: Female habitual self-mutilators. Acta Psychiatr Scand 1989; 79:283–289Crossref, Medline, Google Scholar
28. Langbehn DR, Pfohl B: Clinical correlates of self-mutilation among psychiatric inpatients. Ann Clin Psychiatry 1993; 5:45–51Crossref, Medline, Google Scholar
29. Nijman HLI, Dautzenberg M, Merckelbach HLGJ, Jung P, Wessel I, Campo J: Self-mutilating behavior in psychiatric inpatients. Eur Psychiatry 1999; 14:4–10Crossref, Medline, Google Scholar
30. Suyemoto KL: The functions of self-mutilation. Clin Psychol Rev 1998; 18:531–554Crossref, Medline, Google Scholar
31. Zweig-Frank H, Paris J, Guzder J: Psychological risk factors for dissociation and self-mutilation in female patients with borderline personality disorder. Can J Psychiatry 1994; 39:259–264Crossref, Medline, Google Scholar
32. Zweig-Frank H, Paris J, Guzder J: Psychological risk factors and self-mutilation in male patients with BPD. Can J Psychiatry 1994; 39:266–268Crossref, Medline, Google Scholar
33. Dulit RA, Fyer MR, Leon AC, Brodsky BS, Frances AJ: Clinical correlates of self-mutilation in borderline personality disorder. Am J Psychiatry 1994; 151:1305–1311Link, Google Scholar
34. Turell SC, Armsworth MW: Differentiating incest survivors who self-mutilate. Child Abuse Negl 2000; 24:237–249Crossref, Medline, Google Scholar
35. Brodsky BS, Cloitre M, Dulit RA: Relationship of dissociation to self-mutilation and childhood abuse in borderline personality disorder. Am J Psychiatry 1995; 152:1788–1792Link, Google Scholar
36. Paul T, Schroeter K, Dahme B, Nutzinger DO: Self-injurious behavior in women with eating disorders. Am J Psychiatry 2002; 159:408–411Link, Google Scholar
37. Carroll J, Schaffer C, Spensley J, Abramowitz SI: Family experiences of self-mutilating patients. Am J Psychiatry 1980; 137:852–853Link, Google Scholar
38. Zlotnick C, Shea MT, Recupero P, Bidadi K, Pearlstein T, Brown P: Trauma, dissociation, impulsivity, and self-mutilation among substance abuse patients. Am J Orthopsychiatry 1997; 67:650–654Crossref, Medline, Google Scholar
39. Nisbett RE, Wilson TD: Telling more than we can know: verbal reports on mental processes. Psychol Rev 1977; 84:231–259Crossref, Google Scholar
40. John OP, Robins RW: Determinants of interjudge agreement on personality traits: the big five domains, observability, evaluativeness, and the unique perspective of the self. J Pers 1993; 61:521–551Crossref, Medline, Google Scholar
41. Klonsky ED, Oltmanns TF, Turkheimer E: Informant reports of personality disorder: relation to self-report, and future research directions. Clin Psychol Sci Practice 2002; 9:300–311Crossref, Google Scholar
42. Oltmanns TF, Turkheimer E: Perceptions of the self and other regarding pathological personality traits, in Proceedings of the 3rd Annual Meeting of the Society for Personality and Social Psychology. Rochester, NY, SPSP, 2002, p 14Google Scholar
43. Thomas C, Turkheimer E, Oltmanns TF: Factorial structure of pathological personality traits as evaluated by peers. J Abnorm Psychol 2003; 112:81–91Crossref, Medline, Google Scholar
44. Clark LA: Schedule for Nonadaptive and Adaptive Personality: Manual for Administration, Scoring, and Interpretation. Minneapolis, University of Minnesota Press, 1996Google Scholar
45. Oltmanns TF, Turkheimer E, Thomas C: Perceptions of the self and others in relation to personality disorders, in Proceedings of the 12th Annual Meeting of the American Psychological Society. Washington, DC, APS, 2000, p 34Google Scholar
46. Beck AT, Steer RA, Garbin MG: Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev 1988; 8:77–100Crossref, Google Scholar
47. Beck AT, Epstein N, Brown G, Steer RA: An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988; 56:893–897Crossref, Medline, Google Scholar
48. Clark LA, Watson D: Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. J Abnorm Psychol 1991; 100:316–336Crossref, Medline, Google Scholar
49. Brain KL, Haines J, Williams CL: The psychophysiology of self-mutilation: evidence of tension reduction. Arch Suicide Res 1998; 4:227–242Google Scholar



