Gender Differences in the Prescribing of Antipsychotic Drugs
Abstract
OBJECTIVE: The aim of this article is to offer recommendations and rationale for gender-specific antipsychotic treatment. METHOD: The author summarizes reviews of recent literature in psychiatric clinical trials, pharmacology, drug safety, toxicology, obstetrics and gynecology, and pediatrics. RESULTS: The pharmacokinetics and pharmacodynamics of antipsychotic drugs differ in women and men and are influenced by gender-specific factors such as body build, diet, smoking, concurrent medication, exercise, substance use, and hormonal transitions. In general, and for some drugs in particular, women require lower doses in order to stay well. Because preliminary drug testing is not done in pregnant women, the issue of effective dosing during pregnancy is unstudied, and safety for fetuses and nursing infants may not become evident until a drug is widely used. Specific adverse effects on issues crucial to women (e.g., parenting) have not been well studied, but some side effects, such as weight gain, passivity, hypotension, and hyperprolactinemia, are reported to be particularly problematic for women. Some serious side effects are more often seen among women than among men. CONCLUSIONS: Optimal maintenance regimens of antipsychotics for women and men are not the same.
Antipsychotic prescription guidelines do not differentiate between male and female patients, yet human studies have shown that the pharmacokinetics and the pharmacodynamics of drugs differ between the two sexes (1–4). Women’s bodies, on average, contain 25% more adipose tissue than those of men, and most antipsychotic drugs are lipophilic—i.e., accumulate in lipid stores (5). To minimize the resulting side effects, should there be longer intervals between doses in women than men? Women undergo menstrual cycles, and many take contraceptive pills during adulthood. What is known about interactions between hormones and antipsychotics? Should dose regimens in women be altered during menstrual cycles, pregnancy, the postpartum period, and menopause (3, 4, 6–9)? Women in treatment for schizophrenia, more so than men, take a variety of adjunct drugs in addition to antipsychotics. In other words, there are more opportunities for drug interaction, culminating in the possibility of lowered or raised antipsychotic serum levels. Combined with lifestyle factors such as smoking, coffee drinking, or alcohol intake, subsequent divergence from optimum levels of the drug in the brain can be significant (10, 11). Pregnancy and breast-feeding require an understanding of pharmacokinetics in the pregnant woman, the fetus, and the neonate as well as knowledge about developmental risks, the impact of drugs on labor and delivery, the potential for withdrawal reactions in the infant, behavioral toxicity, and drug concentrations in breast milk (12–22).
Antipsychotic drugs are frequently prescribed for untoward behavior (e.g., aggressive behavior) as much as for psychotic symptoms (23). Reported higher prescribed doses in men may be due to this and not to response factors. Rates of side effects to most drugs are reported to be higher in women than in men (24). Is this true for antipsychotic drugs? Does it imply that women are systematically overdosed, since most side effects are dose related? Neurotransmitter numbers diminish with age at different rates in women and men (25). Should aging men and women be prescribed different drug regimens (26)? When clinicians write a prescription for a patient with schizophrenia, should it matter whether the person in front of them is a man or a woman?
Before discussing antipsychotic drug issues, it is important to first understand gender differences in schizophrenia and how they can affect medication needs at different stages of illness.
Gender Differences Not Specific to Schizophrenia
From early in its formation, the brain is structurally and functionally a sexually dimorphic organ (27). Infants come into the world with CNSs inclined toward more male or more female modes of response. Their anatomic sex evokes somewhat different expectations from caregivers, and, as their sexually dimorphic traits unfold, they elicit increasingly divergent responses from their social milieus. Such responses shape subsequent conduct in gender-appropriate ways, as do societal, parental, and peer pressures (28). “Genderized” ways of behaving become progressively reinforced by biological imperatives and by learning. Brain dimorphism, hormonal differences, and gender-specific behavior help explain why many neuropsychiatric disorders express themselves differently in the two sexes (29). This includes schizophrenia. Sex differences that affect drug response in schizophrenia include the following (30, 31):
| 1. | Diagnosis is delayed in women. | ||||
| 2. | Deficit symptoms are more prevalent in men. | ||||
| 3. | Therapeutic alliance is stronger in women. | ||||
| 4. | Men smoke more and use more substances of abuse. | ||||
| 5. | Women have more comorbid problems (mood problems, sleep disturbances, pain conditions, allergies, endocrine disturbances, eating disorders, personality disorders, psychophysiological disorders); i.e., they require more concomitant medications. | ||||
Making the Diagnosis in Women and Men
The diagnosis of schizophrenia is usually made between ages 15 and 25. During those 10 years, schizophrenia is diagnosed in 12 men to every 10 women (32). This may be because the onset of schizophrenia is delayed in women. Many reasons for such a possibility have been considered: greater vulnerability of the male brain because of slower maturation (33), greater exposure to birth injury in males (34), a neuroprotective effect of female hormones (35), less lateralization of the female brain (36), and greater exposure of males to head trauma (37). It may be that men come to medical attention earlier than women because of the nature of their behavior when they are psychotic, or it may be that women with schizophrenia are initially misdiagnosed. Narrow diagnostic criteria for schizophrenia exclude those whose initial episode is brief and affect laden (32), and these individuals are mainly women (38).
Earlier onset of schizophrenia (i.e., in men) usually means a more severe course of illness (39). On the other hand, a delayed diagnosis (i.e., in women) is a potential problem for treatment because long-lasting symptoms have been shown in prospective studies to be relatively nonresponsive to antipsychotic drugs (40, 41). A schizophrenic illness initially diagnosed as depression or a bipolar disorder (i.e., in women) means that antidepressants and mood stabilizers have preceded treatment with antipsychotics. Such prior treatment can “prime” neural networks and result in an unanticipated antipsychotic response later (42).
Between ages 25 and 35, equal numbers of men and women are diagnosed with schizophrenia (32). After age 35, a first visit to the psychiatris is 50% more frequent in woment with schizophrenia (32). Very late onset of schizophrenia is also much more common in women than in men (43). In other words, first-episode samples are composed of younger men and older women. It is, therefore, important to control for age when comparing results of drug response in women and men in first-episode studies.
Course of Schizophrenia in Women and Men
Despite the possibility that their illness comes to treatment late, women with schizophrenia experience less severe symptoms, fewer hospitalizations, shorter admissions, more posthospitalization employment, less trouble with the law, and more intimate relationships than men with schizophrenia (30, 31). This has led to the conjecture that the response to antipsychotic drug treatment is more robust in women than in men (44). Superior outcome may have little to do with response to treatment and more with treatment adherence, life style, social supports, the advantage of later onset, and relative hormonal protection (45, 46). The corollary is that if women are doing better, their maintenance antipsychotic doses need not be as high as those of men.
Schizophrenia mortality from unnatural factors (suicide, accident, homicide) is significantly higher in men than in women (47). As proportionately more seriously ill men in the schizophrenia population die, the levels of acuity between the two sexes begin to approximate, and indeed, in older age, the severity of illness is similar between the two sexes. This is true not only with respect to hospitalization variables such as the number and frequency of admissions and the lengths of stay but also with respect to mental status at follow-up, social adaptation, and occupational status. In older age, there may be less need for gender-specific prescribing (26, 48).
Antipsychotic Treatment Response and Serum Levels in Men and Women
Genetics, age, height, weight, lean-fat ratio, diet, exercise, concurrent disease, smoking and alcohol, and the administration of concomitant drugs all contribute to antipsychotic drug response, as does end-organ sensitivity. Together, these factors can account for a 10-fold variability in the dose needed for effective response. Men and women show differences in all of these variables, either as a result of the action of sex-specific hormones or of divergent gender roles. So the stage is set for a somewhat different response to medication in the two sexes.
In a prospective drug-naive population, antipsychotic response was shown to be superior in women (49), and in a chronically ill population, men were found to require twice as high a dose as women for effective maintenance (50). But studies comparing response in men and women are few. As a group, women have higher antipsychotic plasma levels than men after receiving the same dose of drug (51). Male sex was associated with nonresponse at 1 year in a first-episode sample (52) but not with likelihood of relapse after response (53). In the most methodologically rigorous study, with age of onset, course of illness, prior hospitalizations, and premorbid functioning controlled, no gender-specific difference was found in neuroleptic dose or dose by weight (54).
It has been postulated that hormonal fluctuations within phases of the menstrual cycle may influence pharmacokinetics and pharmacodynamics of drugs. Menstrual cycle variations do occur in renal, cardiovascular, hematological, and immune systems (4) and could theoretically also affect protein binding and the volume of distribution of a particular compound. When age and menstrual status (but not menstrual phase) were controlled, one study found no dose-by-sex difference (55). One group found no effect of menstrual cycle on cytochrome enzymes 2D6, 3A, or 1A2, suggesting that antipsychotic levels should be impervious to menstrual phase (56–58). Smoking status, as we will see, has strong effects on the metabolism of certain drugs, and one research team has speculated that such antipsychotic dose differences as have been found between men and women are due to more men smoking and smoking more heavily than women (59).
Goff et al. (60) compared prescribed antipsychotic dose in smokers and nonsmokers. Current smokers received a mean dose of 1160 mg/day in chlorpromazine equivalents, while nonsmokers were given 542 mg/day in chlorpromazine equivalents. Overall, multivariate analysis of covariance demonstrated a significant main effect for smoking status but not gender or the interaction between gender and smoking.
After an oral dose, plasma concentrations of haloperidol (metabolized by means of CYP2D6) are significantly lower in smokers than in nonsmokers (61, 62). Smoking may induce CYP2D6, but the story is probably more complicated. A recent study found no significant difference in the haloperidol concentration-to-dose ratio between nonsmokers and smokers. In patients with a non-2D6*10 homozygous genotype, smokers had a significantly lower haloperidol concentration-to-dose ratio than nonsmokers, but this was not the case for smokers with a 2D6*10 homozygous genotype (63). This suggests that the effect of smoking on the concentration-to-dose ratios of drugs depends on a person’s genotype (64). Kelly et al. (65), in a fixed-dose study, found that women had higher plasma concentrations of olanzapine than men. But the greater prevalence of smoking in men could have been responsible for these findings, since tobacco is an inducer of CYP1A2, the main metabolizing enzyme for olanzapine (66, 67). Taking smoking and other factors into account, however, the consensus for olanzapine is that there continues to be a tendency for higher concentrations in women. Being a woman, shown through recent therapeutic drug models, accounted for 27% of observed interindividual variability (68, 69). The enzyme CYP1A2 appears to be less active in women than in men, leading to relatively higher blood concentrations in women, not only of olanzapine (65, 69) but also of clozapine (70). A recent study of patient-related variables on clozapine concentrations found nonsignificantly higher median steady-state plasma concentrations in women than in men and higher concentrations in nonsmokers than in smokers (71). Neither gender nor age apparently has a significant effect on plasma levels of ziprasidone, which is metabolized by CYP3A4 (72).
Drug Interactions
Women are more likely than men to be taking antidepressants, mood stabilizers, analgesics, and contraceptives or hormone replacements, and these agents can interact with antipsychotics, especially those processed mainly by the CYP2D6 enzyme subsystem. In a retrospective analysis of 168 patients taking haloperidol, those treated with concomitant antiepileptic drugs showed a mean ratio of steady state to dose that was 27% lower than those not taking antiepileptic drugs (73). Carbamazepine reduced the median concentration-to-dose ratio of olanzapine (primarily metabolized by means of CYP1A2 with contributions from CYP2D6) by 38% (66, 74) but did not clinically affect the level of ziprasidone (CYP3A4) (75). Patients treated with antiparkinsonian drugs showed a 25% higher mean concentration-to-dose ratio of haloperidol than those not taking antiparkinsonian drugs (73). Neither menopause nor estrogen replacement therapy altered intestinal or hepatic CYP3A activity (which is mainly responsible for the metabolism of ziprasidone and quetiapine) relative to a comparison group of young women (76), nor did the administration of a contraceptive pill (77). Ziprasidone, co-administered with ethinyl estradiol and levonorgestrel, did not lead to a loss of contraceptive efficacy nor increase the risk of adverse events (78).
Long-term administration of St. John’s wort, however, resulted in a significant and selective induction of CYP3A activity in the intestinal wall—i.e., it potentially reduced the efficacy of ziprasidone and quetiapine (79). Selective serotonin-specific reuptake inhibitors (SSRIs) (fluoxetine, citalopram, paroxetine, and fluvoxamine) were significantly associated with 4.6-fold higher concentrations of risperidone. Significantly higher concentrations (29%) of the active metabolite (by means of CYP2D6) 9-hydroxy-risperidone were also observed in patients with biperiden co-medication (80). The SSRI fluvoxamine is a potent inhibitor of CYP1A2 (81). The level of drugs metabolized through this route can be increased 400–1,000-fold if fluvoxamine is co-administered. Oral contraceptives also inhibit this enzyme.
When determining effective doses of antipsychotics, smoking status and adjunct medication (including herbal products) are important pieces of information. Blood levels should be taken when patients are concomitantly taking SSRIs, carbamazepine, or antiparkinsonian drugs, and women must be asked about contraceptive medication (82) and hormone replacement.
Volume of Distribution
The volume of distribution of lipophilic drugs, such as antipsychotics, is greater in women than in men; blood volume is smaller, but lipid compartments are larger. In women, the proportion of adipose tissue ranges from an average of 33% in postpubertal younger women to 48% in the elderly (in contrast with 18% in young men and 36% in elderly men [51]). This prolongs the half-life of antipsychotics in the body, leading to accumulation over time, a phenomenon that becomes important when administering depot injections. After a steady state is achieved, dosing intervals for women should be longer than for men (83, 84).
Aging
Aging brings with it a decrease in intracellular water, a decrease in protein binding, and a decrease in tissue mass. This, plus an increase in total body fat, means that concentrations of antipsychotics in the brain are higher and the body reservoir is increased; hence, drugs accumulate in the tissues. Drug metabolism decreases because of relative enzymatic inactivity, decreased blood flow to the liver, and decreased liver mass. Renal excretion is progressively impaired with age. These factors act synergistically to increase the effect of antipsychotic medications in old age in both sexes. The free versus protein-bound fraction of haloperidol in serum, for instance, increases with age and is significantly higher in the elderly than in middle-age adults (85). Women may be most at risk from too high doses because of a relatively greater lipid-lean ratio—i.e., more storage space for drug accumulation (51). A greater amount of adipose tissue in women argues for lower doses to prevent unnecessary side effects.
Treatment Side Effects
The incidence and severity of antipsychotic side effects are heavily dependent on a serum level that, in turn, depends on prescribed dose, treatment adherence, metabolism, and volume of distribution. Acute dystonia, long thought to be more prevalent among men, has been shown, in a first-episode, fixed-dose, 10-week study, to occur, at equivalent doses, more often in women (86). Earlier clinical studies had not taken into account the fact that young male patients were commonly given higher doses than women. Tardive dyskinesia, still frequently cited as most common in elderly women, has been shown by a cohort (as distinct from a cross-sectional) study to be more of a risk factor for elderly men (87), although its severity may be relatively greater in women in their later years (88).
A statistical analysis of sex differences in all adverse drug events has shown that, although equal numbers of such events were reported for men and women, those reported for women were more serious (24). An example for antipsychotics is the rare side effect of pulmonary embolism, a problem with drugs with an affinity for the serotonin 5-HT2A receptor. This complication appears to be more common in women (89).
A better-studied example of a significant sex difference in the toxicity of antipsychotics is the drug-induced cardiac arrhythmia known as torsades de pointes, which is secondary to a prolonged QT interval (24). Women have longer QT intervals than men on average, but the QT interval is mainly genotype dependent (90). Emergency use of high-dose intravenous drugs that prolong the QT interval, such as haloperidol, may be especially dangerous in women (91).
Severity aside, side effects of antipsychotic medications may hold different significance for men and women. On the whole, men are most disturbed by the effects that interfere with performance, especially sexual performance; women are more distressed by effects that detract from their appearance (92). Obesity is particularly stigmatizing for women, and antipsychotic-induced increases in body mass index are more prevalent in women than in men (93, 94). The future health effects/risks of antipsychotic-induced obesity (e.g., diabetes mellitus, hypertension, cardiovascular disease, and hyperlipidemia) are serious for men and women (95–98), and women may be more at risk for some of these complications (99). Obesity also has specific adverse effects on labor and delivery in women (100) and on the incidence of neural tube defects in their infants (101).
The results of several trials confirm that women are more susceptible to drug-induced hyperprolactinemia than men (102, 103). A recent review of the literature indicates that prolactin concentrations can rise to 10 times normal levels during antipsychotic treatment, and as a consequence, in some studies, up to 78% of female patients have been reported to suffer from amenorrhea with or without galactorrhea (104). Studies in women with hyperprolactinemia resulting from pituitary tumors have demonstrated high rates of osteoporosis believed to result from secondary hypoestrogenism. Women taking drugs that raise prolactin levels show decreased bone mineral density relative to women treated with drugs less prone to increase prolactin (105, 106). Individuals with schizophrenia are at increased risk for osteoporosis and bone fractures, not only from low estrogen levels but also from poor diet, lack of exercise, cigarette smoking, and polydipsia. Some antipsychotic medications may further increase the risk of fractures by causing dizziness, orthostatic hypotension, and falls (107). Anticholinergic effects also increase the risk of falling (108).
A question has also been raised about the connection between prolactin elevation and breast cancer (109, 110), but studies that have found increased rates of breast cancer in women with schizophrenia have not controlled for two potent breast cancer risks: age at first giving birth and parity status. The younger a woman is at the time of her first pregnancy and the more children she has, the less likely she is to develop breast cancer. When this is taken into account, the risk of breast cancer is not increased in women with schizophrenia treated with dopamine antagonists (111).
All antipsychotics have the potential to interfere with sexual function in both men and women (112–114). This is a complex effect and is not directly related to hyperprolactinemia (115).
Some side effects, such as sedation and orthostatic hypotension, are equally prevalent in the two sexes and may interfere with optimal functioning. In women with parenting responsibilities, however, these relatively benign side effects can have serious consequences—e.g., loss of child custody (116).
Most side effects are dose related, and side effects in women may indicate that they are being overmedicated. Alternatively, women may show particular sensitivity to certain side effects (and men to others). The consequence of side effects may be gender specific.
Pregnancy
Guidelines for prescribing antipsychotics during pregnancy and lactation include the following (12–22, 117–123):
| 1. | Consider nondrug options | ||||
| 2. | Avoid drugs if possible during weeks 6–10 | ||||
| 3. | Use antipsychotics about which most is known during pregnancy | ||||
| 4. | Keep doses low before delivery | ||||
| 5. | Increase dose postpartum | ||||
| 6. | Have patient take medications just before infant’s longest sleep of the day | ||||
| 7. | Consult with pediatrician | ||||
Optimal prescription of antipsychotics during pregnancy is complicated by altered pharmacokinetics across the three trimesters, fear of teratogenesis, need to safeguard the smooth progress of labor and delivery, need to prevent withdrawal effects in the neonate, and concerns about subtle effects on the infant’s neurodevelopment. The latter concerns are also present during breast-feeding. Plasma volume increases by about 50% during pregnancy and body fat also increases, expanding the volume of drug distribution. Blood flow to the kidneys rises, as does the glomerular filtration rate, thus speeding renal elimination. Many liver enzymes are activated during pregnancy, so drugs are metabolized more quickly, consequently increasing the rate of clearance. The end result is that plasma drug concentration is lowered during pregnancy. At the same time, because of increasing titers of sex steroids acting on neurotransmitter receptors, some pregnant women may not require high drug concentrations in order to stay symptom-free. Changes in physiology begin in early gestation and are most pronounced in the third trimester of pregnancy. Further changes occur during labor, with some returning to baseline within 24 hours of delivery, while others remain for up to 12 weeks postpartum (15, 17, 22). There are relatively few specific data on pharmacokinetics/dynamics in pregnancy, so therapeutic guidelines must be based on observational studies and basic principles.
The use of medications during pregnancy and lactation requires critical attention to the timing of exposure, the dose and duration of use, and fetal susceptibility. Essentially all psychotropic drugs pass through the placenta. The aim of management of women with schizophrenia during pregnancy and the postpartum period is to achieve an optimal balance between minimizing fetal and neonatal exposure to drugs and the deleterious consequences of a psychotic mother. Usually monotherapy with the lowest effective dose of a drug for the shortest period necessary is the best strategy. If possible, drug exposure during the first trimester is best avoided (19). The use of low-potency phenothiazines during the first trimester probably increases the risk of congenital abnormalities by an additional four cases per 1,000 (124).
A recent study of over 2,000 births to mothers diagnosed with schizophrenia compared to over a million births to women without schizophrenia (125) found significantly increased risks for stillbirth, infant death, preterm delivery, low birth weight, and small size for gestational age among the offspring of women with schizophrenia. Women with an episode of schizophrenia during pregnancy had the highest risks. Control for a higher incidence of smoking during pregnancy among the subjects as well as for single motherhood, maternal age, parity, maternal education and country of birth, and pregnancy-induced hypertensive diseases in a multiple regression model reduced the risk. But even after adjustments, there was a doubled risk for women with an episode of schizophrenia during pregnancy in relation to women in the comparison group. The risks for preterm delivery and low birth weight were significantly elevated for all subjects (125). It is impossible to tell from this study how much of the poorer outcome can be attributed to antipsychotic treatment.
Another study of over 2,000 children of women with schizophrenia found that these infants had an increased risk of postneonatal death largely explained by an increase in sudden infant death syndrome. They also had a marginally statistically significant increase in the risk of congenital malformations (126). The same study found that women with schizophrenia had fewer antenatal care visits than pregnant women in the general population and that their babies tended to have lower APGAR scores. Subjects were at increased risk of interventions such as cesarean section, assisted vaginal delivery, amniotomy, and pharmacological stimulation of labor (127). The authors concluded that their findings must be interpreted against a backdrop of presumed differences in socioeconomic status, substance abuse, smoking, and medication use between subjects with schizophrenia and comparison subjects.
Fetal circulation, compared with maternal circulation, contains less protein, leaving more of the drug unbound—i.e., facilitating entry into the brain. Liver enzymes are relatively inactive in the fetus, increasing the possibility of toxic effects. Excretion is relatively prolonged. In addition, the blood-brain barrier is incomplete, and the nervous system is immature and, therefore, it is more sensitive to drug effects (128). Teratogenic effects are both dose and time dependent, with organs at the greatest risk during their period of fastest development. Week 6 to week 10 is the most vulnerable period. Besides organ malformation, potential risks to the fetus are spontaneous abortion, growth retardation, and immediate neonatal effects, such as extrapyramidal and withdrawal symptoms. Neurodevelopmental effects of antipsychotic drugs have never been demonstrated in humans but remain a theoretical concern (129).
Not much is yet known about the newer drugs. Clozapine poses special potential risks for the fetus: seizure and agranulocytosis. Thus far, olanzapine appears relatively safe. Twenty-three prospectively and 11 retrospectively ascertained pregnancy reports on pregnant women treated with olanzapine were collected in the Lilly Worldwide Pharmacovigilance Safety Database. Spontaneous abortion occurred in 13%, stillbirth in 5%, and prematurity in 5%—all within the range of normal historic control rates. There were no major malformations (117).
Most experts suggest minimal use—no use, if possible—of antipsychotics during weeks 6–10 of gestation to prevent teratogenesis and low doses before expected delivery to prevent toxicity and withdrawal in the infant, with immediate resumption of a full dose after delivery because of the high risk of the mother’s decompensation postpartum (12, 13, 16, 20).
Lactation
A drug that is safe for use during pregnancy may not be safe for the nursing infant. Exposure to antipsychotic medication in breast milk markedly differs from exposure to antipsychotics by the fetus during pregnancy (118). The non-protein-bound (free) drug in the blood of the nursing mother enters breast milk at a rate that depends on its lipid solubility. The more fat-soluble the drug, the more of it enters. How much antipsychotic drug is present in breast milk at any one time depends mainly on the lipid concentration of the breast milk, which is different in foremilk and hindmilk and changes over time. An important factor is the temporal relationship between maternal drug ingestion and the time of nursing. The neonate’s metabolic and excretory functions mature over time but are relatively underdeveloped at birth. Immature liver enzymes cannot detoxify drugs efficiently nor can the immature kidney competently eliminate drugs. Metabolic pathways in existence at these early stages of development are not always the same ones that exist later, so the metabolites of a drug in the neonate may differ from those in the adult. Relatively low protein binding in the infant increases the serum concentration of free drug that crosses into the brain, and all tissue concentrations are relatively high because of the small volume of distribution (118).
The literature suggests that infant serum concentrations of antipsychotics are largely unpredictable. Clinical risk assessment is compromised by sparse data, as studies in breast-feeding women and their infants are ethically difficult to conduct. A literature review (119) concluded that women who are vulnerable to postpartum exacerbation of psychiatric disorders are placed in a difficult position, often choosing to abandon the drugs they need to keep well or going to the other extreme and foregoing breast-feeding with all its known benefits to the infant and to the mother-child bond. These authors advise that parents be provided with all known available information and that the psychiatrist involve the pediatrician in monitoring the infant’s exposure. Della-Giustina and Chow (120) offer the following advice to physicians advising nursing mothers:
| 1. | Determine if medication is necessary. | ||||
| 2. | Choose the safest drug available, that is, one that has been proven safe when administered directly to infants, has a low milk-to-plasma ratio, has a short half-life, has a high molecular weight, has high protein binding in maternal serum, is ionized in maternal plasma, and is relatively nonlipophilic. | ||||
| 3. | Consult with the infant’s pediatrician. | ||||
| 4. | Advise the mother to take her medication just after she has breast-fed the infant or just before the infant’s longest sleep period. | ||||
| 5. | If there is a possibility that a drug may put the health of the infant at risk, monitor infant serum drug levels. | ||||
The rule of thumb is that, for any drug in breast milk, infants should be exposed to less than 10% of the dose per weight that would be prescribed to them directly. In one study of olanzapine (121), seven breast-fed infants were exposed to a calculated olanzapine dose of approximately 1%. The olanzapine was below the detection limit in the infant plasma, and there were no adverse effects. The authors of another olanzapine study (122) (N=9) came to the same conclusion. Premature infants are at relatively higher risk; the possibility of toxicity is reduced as the infant grows. Novel agents, the safety for which there are few data, are better avoided, and clozapine is a problem because of the frequent blood monitoring it requires. Multiple medications are best avoided (123), as are smoking, alcohol, and over-the-counter medications.
Recommendations
Gender needs to be taken into account when prescribing. Inquiries into symptom fluctuation over the menstrual phase and into diet, smoking habits, substance use, contraceptive pills, over-the-counter and herbal preparations, and prescribed medications are essential. The body’s lean-fat ratio is important to consider, as most antipsychotics are lipophilic. Familiarity with metabolic pathways, metabolites, and interactions of all prescribed drugs is important. Dose-response predictions will vary from person to person (130). Menopausal status, age, and renal functioning are crucial information. Inquiries need to be made into the effects of hypotension, passivity, sedation, and sexual dysfunction in the context of the patient’s home situation. Contraception choices require repeated discussion, and every woman needs to be considered as potentially pregnant. During pregnancy, antipsychotic doses should be as low as possible and blood levels frequently monitored. The dose needs to be raised after delivery and the pros and cons of breast-feeding seriously weighed. Mother and infant need frequent monitoring during the postpartum period. Inadequate or overzealous psychopharmacological intervention at this time may jeopardize the mother’s ability to retain custody of her child and may have far-reaching consequences for the life of the mother and child. Optimal prescribing in pregnant women not only will improve patient well-being but also will enhance the safety of their infants and the integrity of the family.
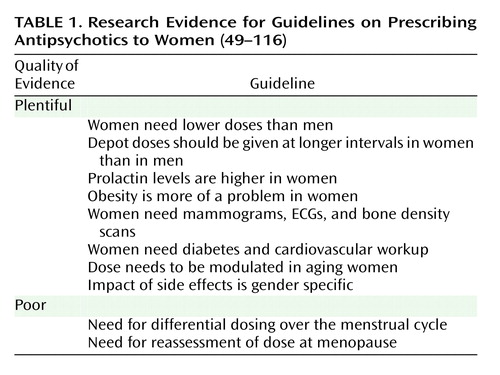
In conclusion, prescribing for a woman is not the same as prescribing for a man (Table 1).
 |
Received Aug. 6, 2003; revision received Oct. 20, 2003; accepted Oct. 31, 2003. From the Centre for Addiction and Mental Health, Department of Psychiatry, University of Toronto, 250 College St., Toronto, Ont., Canada, M5T 1R8; [email protected] (e-mail).
1. Anthony M, Berg MJ: Biologic and molecular mechanisms for sex differences in pharmacokinetics, pharmacodynamics, and pharmacogenetics, part I. J Womens Health Gend Based Med 2002; 11:601–615Crossref, Medline, Google Scholar
2. Anthony M, Berg MJ: Biologic and molecular mechanisms for sex differences in pharmacokinetics, pharmacodynamics, and pharmacogenetics, part II. J Womens Health Gend Based Med 2002; 11:617–629Crossref, Medline, Google Scholar
3. Harris RZ, Benet LZ, Schwartz JB: Gender effects in pharmacokinetics and pharmacodynamics. Drugs 1995; 50:222–239Crossref, Medline, Google Scholar
4. Kashuba AD, Nafziger AN: Physiological changes during the menstrual cycle and their effects on the pharmacokinetics and pharmacodynamics of drugs. Clin Pharmacokinet 1998; 34:203–218Crossref, Medline, Google Scholar
5. Beierle I, Meibohm B, Derendorf H: Gender differences in pharmacokinetics and pharmacodynamics. Int J Clin Pharmacol Ther 1999; 37:529–647Medline, Google Scholar
6. Flores Perez J, Juarez Olguin H, Flores Perez C, Perez Guille G, Guille Perez A, Camacho Vieyra A, Toledo Lopez A, Carrasco Portugal M, Lares Asseff I: Effects of gender and phase of the menstrual cycle on the kinetics of ranitidine in healthy volunteers. Chronobiol Int 2003; 20:485–494Medline, Google Scholar
7. Haddad L, Milke P, Zapata L, de la Fuente JR, Vargas-Vorackova F, Lorenzana-Jimenez M, Corte G, Tamayo J, Kaplan M, Marquez M, Kershenobich D: Effect of the menstrual cycle in ethanol pharmacokinetics. J Appl Toxicol 1998; 18:15–18Crossref, Medline, Google Scholar
8. Kamimori GH, Joubert A, Otterstetter R, Santaromana M, Eddington ND: The effect of the menstrual cycle on the pharmacokinetics of caffeine in normal, healthy eumenorrheic females. Eur J Clin Pharmacol 1999; 55:445–449Crossref, Medline, Google Scholar
9. Rowan JP: “Estrophasic” dosing: a new concept in oral contraceptive therapy. Am J Obstet Gynecol 1999; 180:302–306Crossref, Medline, Google Scholar
10. Balant-Gorgia AE, Gex-Fabry M, Balant LP: Therapeutic drug monitoring and drug-drug interactions: a pharmacoepidemiological perspective. Therapie 1996; 51:399–402Medline, Google Scholar
11. Gex-Fabry M, Balant-Gorgia AE, Balant LP: Therapeutic drug monitoring databases for postmarketing surveillance of drug-drug interactions. Drug Saf 2001; 24:947–959Crossref, Medline, Google Scholar
12. American Academy of Pediatrics Committee on Drugs: Use of psychoactive medication during pregnancy and possible effects on the fetus and newborn. Pediatrics 2000; 105:880–887Crossref, Medline, Google Scholar
13. Boyle RJ: Effects of certain prenatal drugs on the fetus and newborn. Pediatr Rev 2002; 23:17–24Crossref, Medline, Google Scholar
14. Craig M, Abel K: Drugs in pregnancy: prescribing for psychiatric disorders in pregnancy and lactation. Best Pract Res Clin Obstet Gynaecol 2001; 15:1013–1030Crossref, Medline, Google Scholar
15. Dawes M, Chowienczyk PJ: Drugs in pregnancy: pharmacokinetics in pregnancy. Best Pract Res Clin Obstet Gynaecol 2001; 15:819–826Crossref, Medline, Google Scholar
16. Ernst CL, Goldberg JF: The reproductive safety profile of mood stabilizers, atypical antipsychotics, and broad-spectrum psychotropics. J Clin Psychiatry 2002; 63(suppl 4):42–55Google Scholar
17. Frederiksen MC: Physiologic changes in pregnancy and their effect on drug disposition. Semin Perinatol 2001; 25:120–123Crossref, Medline, Google Scholar
18. Gjere NA: Psychopharmacology in pregnancy. J Perinat Neonatal Nurs 2001; 14:12–25Crossref, Medline, Google Scholar
19. Patton SW, Misri S, Corral MR, Perry KF, Kuan AJ: Antipsychotic medication during pregnancy and lactation in women with schizophrenia: evaluating the risk. Can J Psychiatry 2002; 47:959–965Crossref, Medline, Google Scholar
20. Shehata HA, Nelson-Piercy C: Drugs in pregnancy: drugs to avoid. Best Pract Res Clin Obstet Gynaecol 2001; 15:971–986Crossref, Medline, Google Scholar
21. Winans EA: Antipsychotics and breastfeeding. J Hum Lact 2001; 17:344–347Crossref, Medline, Google Scholar
22. Wyska E, Jusko WJ: Approaches to pharmacokinetic/pharmacodynamic modeling during pregnancy. Semin Perinatol 2001; 25:124–132Crossref, Medline, Google Scholar
23. Peralta V, Cuesta MJ, Caro F, Martinez-Larrea A: Neuroleptic dose and schizophrenic symptoms: a survey of prescribing practices. Acta Psychiatr Scand 1994; 90:354–357Crossref, Medline, Google Scholar
24. Miller MA: Gender-based differences in the toxicity of pharmaceuticals—the Food and Drug Administration’s perspective. Int J Toxicol 2001; 20:149–152Crossref, Medline, Google Scholar
25. Kaasinen V, Kemppainen N, Nagren K, Helenius H, Kurki T, Rinne JO: Age-related loss of extrastriatal dopamine D(2)-like receptors in women. J Neurochem 2002; 81:1005–1010Crossref, Medline, Google Scholar
26. Lindamer LA, Lohr JB, Harris MJ, McAdams LA, Jeste DV: Gender-related clinical differences in older patients with schizophrenia. J Clin Psychiatry 1999; 6:61–67Google Scholar
27. Goldstein JM, Kennedy DN, Caviness VS Jr: Brain development, XI: sexual dimorphism (image, neuro). Am J Psychiatry 1999; 156:352Link, Google Scholar
28. Maccoby EE, Jacklin CN: Psychological sex differences, in Scientific Foundations of Developmental Psychiatry. Edited by Rutter M. London, Heinemann Medical, 1980, pp 92–100Google Scholar
29. Earls F: Sex differences in psychiatric disorders: origins and developmental influences. Psychiatr Dev 1987; 1:1–23Google Scholar
30. Usall J, Araya S, Ochoa S, Busquets E, Gost A, Marquez M (Assessment Research Group in Schizophrenia [NEDES]): Gender differences in a sample of schizophrenic outpatients. Compr Psychiatry 2001; 42:301–305Crossref, Medline, Google Scholar
31. Hafner H: Gender differences in schizophrenia. Psychoneuroendocrinology 2003; 28(suppl 2):17–54Google Scholar
32. Castle DJ: Epidemiology of women and schizophrenia, in Women and Schizophrenia. Edited by Castle DJ, McGrath J, Kulkarni J. Cambridge, UK, Cambridge University Press, 2000, pp 19–33Google Scholar
33. Benes FM, Tutle M, Khan Y, Farol P: Myelination of a key relay zone in the hippocampal formation occurs in human brain during childhood, adolescence, and adulthood. Arch Gen Psychiatry 1994; 51:477–484Crossref, Medline, Google Scholar
34. Kirov G, Jones PB, Harvey I, Lewis SW, Toone BK, Rifkin L, Sham P, Murray RM: Do obstetric complications cause the earlier age at onset in male than female schizophrenics? Schizophr Res 1996; 20:117–124Crossref, Medline, Google Scholar
35. Seeman MV: Psychopathology in women and men: focus on female hormones. Am J Psychiatry 1997; 154:1641–1647Link, Google Scholar
36. Medland SE, Geffen G, McFarland K: Lateralization of speech production using verbal/manual dual tasks: meta-analysis of sex differences and practice effects. Neuropsychologia 2002; 40:1233–1239Crossref, Medline, Google Scholar
37. Lalloo R, Sheiham A: Risk factors for childhood major and minor head and other injuries in a nationally representative sample. Injury 2003; 34:261–266Crossref, Medline, Google Scholar
38. Marneros A, Pillmann F, Haring A, Balzuweit S, Bloink R: Features of acute and transient psychotic disorders. Eur Arch Psychiatry Clin Neurosci 2003; 253:167–174Crossref, Medline, Google Scholar
39. Jarbin H, Ott Y, Von Knorring AL: Adult outcome of social function in adolescent-onset schizophrenia and affective psychosis. J Am Acad Child Adolesc Psychiatry 2003; 42:176–183Crossref, Medline, Google Scholar
40. Bottlender R, Sato T, Jager M, Wegener U, Wittmann J, Strauss A, Moller HJ: The impact of the duration of untreated psychosis prior to first psychiatric admission on the 15-year outcome in schizophrenia. Schizophr Res 2003; 62:37–44Crossref, Medline, Google Scholar
41. Harrigan SM, McGorry PD, Krstev H: Does treatment delay in first-episode psychosis really matter? Psychol Med 2003; 33:97–110Crossref, Medline, Google Scholar
42. Antelman SM, Levine J, Gershon S: Time-dependent sensitization: the odyssey of a scientific heresy from the laboratory to the door of the clinic. Mol Psychiatry 2000; 5:350–356Crossref, Medline, Google Scholar
43. Howard R, Rabins PV, Seeman MV, Jeste DV (International Late-Onset Schizophrenia Group): Late-onset schizophrenia and very-late-onset schizophrenia-like psychosis: an international consensus. Am J Psychiatry 2000; 157:172–178Link, Google Scholar
44. Seeman MV: Interaction of sex, age, and neuroleptic dose. Compr Psychiatry 1983; 24:125–128Crossref, Medline, Google Scholar
45. Meltzer HY, Rabinowitz J, Lee MA, Cola PA, Ranjan R, Findling RL, Thompson PA: Age at onset and gender of schizophrenic patients in relation to neuroleptic resistance. Am J Psychiatry 1997; 154:475–482Link, Google Scholar
46. Torgalsboen AK: Full recovery from schizophrenia: the prognostic role of premorbid adjustment, symptoms at first admission, precipitating events and gender. Psychiatry Res 1999; 88:143–152Crossref, Medline, Google Scholar
47. Mortensen P, Juel K: Mortality and causes of death in first admitted schizophrenic patients. Br J Psychiatry 1993; 163:183–189Crossref, Medline, Google Scholar
48. Jeste DV, Lindamer LA, Evans J, Lacro JP: Relationship of ethnicity and gender to schizophrenia and pharmacology of neuroleptics. Psychopharmacol Bull 1996; 32:243–251Medline, Google Scholar
49. Szymanski S, Lieberman JA, Alvir JM, Mayerhoff D, Loebel A, Geisler S, Chakos M, Koreen A, Jody D, Kane J, Woerner M, Cooper T: Gender differences in onset of illness, treatment response, course, and biologic indexes in first-episode schizophrenic patients. Am J Psychiatry 1995; 152:698–703Link, Google Scholar
50. Melkersson KI, Hulting AL, Rane AJ: Dose requirement and prolactin elevation of antipsychotics in male and female patients with schizophrenia or related psychoses. Br J Clin Pharmacol 2001; 51:317–324Crossref, Medline, Google Scholar
51. Pollock BG: Gender differences in psychotropic drug metabolism. Psychopharmacol Bull 1997; 33:235–241Medline, Google Scholar
52. Robinson DG, Woerner MG, Alvir JMJ, Geisler S, Koreen A, Sheitman B, Chakos M, Mayerhoff D, Bilder R, Goldman R, Lieberman JA: Predictors of treatment response from a first episode of schizophrenia or schizoaffective disorder. Am J Psychiatry 1999; 156:544–549Link, Google Scholar
53. Robinson D, Woerner MG, Alvir JM, Bilder R, Goldman R, Geisler S, Koreen A, Sheitman B, Chakos M, Mayerhoff D, Lieberman JA: Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Arch Gen Psychiatry 1999; 56:241–247Crossref, Medline, Google Scholar
54. Pinals DA, Malhotra AK, Missar CD, Pickar D, Breier A: Lack of gender differences in neuroleptic response in patients with schizophrenia. Schizophr Res 1996; 22:215–222Crossref, Medline, Google Scholar
55. Magharious W, Goff DC, Amico E: Relationship of gender and menstrual status to symptoms and medication side effects in patients with schizophrenia. Psychiatry Res 1998; 77:159–166Crossref, Medline, Google Scholar
56. Kashuba AD, Nafziger AN, Kearns GL, Leeder JS, Shirey CS, Gotschall R, Gaedigk A, Bertino JS Jr: Quantification of intraindividual variability and the influence of menstrual cycle phase on CYP2D6 activity as measured by dextromethorphan phenotyping. Pharmacogenetics 1998; 8:403–410Crossref, Medline, Google Scholar
57. Kashuba AD, Bertino JS Jr, Rocci ML Jr, Kulawy RW, Beck DJ, Nafziger AN: Quantification of 3-month intraindividual variability and the influence of sex and menstrual cycle phase on CYP3A activity as measured by phenotyping with intravenous midazolam. Clin Pharmacol Ther 1998; 64:269–277Crossref, Medline, Google Scholar
58. Kashuba AD, Bertino JS Jr, Kearns GL, Leeder JS, James AW, Gotschall R, Nafziger AN: Quantitation of three-month intraindividual variability and influence of sex and menstrual cycle phase on CYP1A2, N-acetyltransferase-2, and xanthine oxidase activity determined with caffeine phenotyping. Clin Pharmacol Ther 1998; 63:540–551Crossref, Medline, Google Scholar
59. Salokangas RK, Saarijarvi S, Taiminen T, Lehto H, Niemi H, Ahola V, Syvalahti E: Effect of smoking on neuroleptics in schizophrenia. Schizophr Res 1997; 23:55–60Crossref, Medline, Google Scholar
60. Goff DC, Henderson DC, Amico E: Cigarette smoking in schizophrenia: relationship to psychopathology and medication side effects. Am J Psychiatry 1992; 149:1189–1194Link, Google Scholar
61. Pan L, Vander Stichele R, Rosseel MT, Berlo JA, De Schepper N, Belpaire FM: Effects of smoking, CYP2D6 genotype, and concomitant drug intake on the steady state plasma concentrations of haloperidol and reduced haloperidol in schizophrenic inpatients. Ther Drug Monit 1999; 21:489–497Crossref, Medline, Google Scholar
62. Shimoda K, Someya T, Morita S, Hirokane G, Noguchi T, Yokono A, Shibasaki M, Takahashi S: Lower plasma levels of haloperidol in smoking than in nonsmoking schizophrenic patients. Ther Drug Monit 1999; 21:293–296Crossref, Medline, Google Scholar
63. Ohara K, Tanabu S, Yoshida K, Ishibashi K, Ikemoto K, Shibuya H: Effects of smoking and cytochrome P450 2D6*10 allele on the plasma haloperidol concentration/dose ratio. Prog Neuropsychopharmacol Biol Psychiatry 2003; 27:945–949Crossref, Medline, Google Scholar
64. Brockmoller J, Kirchheiner J, Schmider J, Walter S, Sachse C, Muller-Oerlinghausen B, Roots I: The impact of the CYP2D6 polymorphism on haloperidol pharmacokinetics and on the outcome of haloperidol treatment. Clin Pharmacol Ther 2002; 72:438–452Crossref, Medline, Google Scholar
65. Kelly DL, Conley RR, Tamminga CA: Differential olanzapine plasma concentrations by sex in a fixed-dose study. Schizophr Res 1999; 40:101–104Crossref, Medline, Google Scholar
66. Callaghan JT, Bergstrom RF, Ptak LR, Beasley CM: Olanzapine: pharmacokinetic and pharmacodynamic profile. Clin Pharmacokinet 1999; 37:177–193Crossref, Medline, Google Scholar
67. Carrillo JA, Herraiz AG, Ramos SI, Gervasini G, Vizcaino S, Benitez J: Role of the smoking-induced cytochrome P450 (CYP)1A2 and polymorphic CYP2D6 in steady-state concentration of olanzapine. J Clin Psychopharmacol 2003; 23:119–127Crossref, Medline, Google Scholar
68. Skogh E, Reis M, Dahl ML, Lundmark J, Bengtsson F: Therapeutic drug monitoring data on olanzapine and its N-demethyl metabolite in the naturalistic clinical setting. Ther Drug Monit 2002; 24:518–526Crossref, Medline, Google Scholar
69. Gex-Fabry M, Balant-Gorgia AE, Balant LP: Therapeutic drug monitoring of olanzapine: the combined effect of age, gender, smoking, and comedication. Ther Drug Monit 2003; 25:46–53Crossref, Medline, Google Scholar
70. Lane HY, Chang YC, Chang WH, Lin SK, Tseng YT, Jann MW: Effects of gender and age on plasma levels of clozapine and its metabolites: analyzed by critical statistics. J Clin Psychiatry 1999; 60:36–40Crossref, Medline, Google Scholar
71. Palego L, Biondi L, Giannaccini G, Sarno N, Elmi S, Ciapparelli A, Cassano GB, Lucacchini A, Martini C, Dell’Osso L: Clozapine, norclozapine plasma levels, their sum and ratio in 50 psychotic patients: influence of patient-related variables. Prog Neuropsychopharmacol Biol Psychiatry 2002; 26:473–480Crossref, Medline, Google Scholar
72. Wilner KD, Tensfeldt TG, Baris B, Smolarek TA, Turncliff RZ, Colburn WA, Hansen RA: Single- and multiple-dose pharmacokinetics of ziprasidone in healthy young and elderly volunteers. Br J Clin Pharmacol 2000; 49(suppl 1):15S-20SGoogle Scholar
73. Yukawa E, Ichimaru R, Maki T, Matsunaga K, Anai M, Yukawa M, Higuchi S, Goto Y: Interindividual variation of serum haloperidol concentrations in Japanese patients—clinical considerations on steady-state serum level-dose ratios. J Clin Pharm Ther 2003; 28:97–101Crossref, Medline, Google Scholar
74. Linnet K, Olesen OV: Free and glucuronidated olanzapine serum concentrations in psychiatric patients: influence of carbamazepine comedication. Ther Drug Monit 2002; 24:512–517Crossref, Medline, Google Scholar
75. Miceli JJ, Anziano RJ, Robarge L, Hansen RA, Laurent A: The effect of carbamazepine on the steady-state pharmacokinetics of ziprasidone in healthy volunteers. Br J Clin Pharmacol 2000; 49(suppl 1):65S-70SGoogle Scholar
76. Gorski JC, Wang Z, Haehner-Daniels BD, Wrighton SA, Hall SD: The effect of hormone replacement therapy on CYP3A activity. Clin Pharmacol Ther 2000; 68:412–417Crossref, Medline, Google Scholar
77. Belle DJ, Callaghan JT, Gorski JC, Maya JF, Mousa O, Wrighton SA, Hall SD: The effects of an oral contraceptive containing ethinyloestradiol and norgestrel on CYP3A activity. Br J Clin Pharmacol 2002; 53:67–74Crossref, Medline, Google Scholar
78. Muirhead GJ, Harness J, Holt PR, Oliver S, Anziano RJ: Ziprasidone and the pharmacokinetics of a combined oral contraceptive. Br J Clin Pharmacol 2000; 49(suppl 1):49S-56SGoogle Scholar
79. Wang Z, Gorski JC, Hamman MA, Huang SM, Lesko LJ, Hall SD: The effects of St John’s wort (Hypericum perforatum) on human cytochrome P450 activity. Clin Pharmacol Ther 2001; 70:317–326Medline, Google Scholar
80. Balant-Gorgia AE, Gex-Fabry M, Genet C, Balant LP: Therapeutic drug monitoring of risperidone using a new, rapid HPLC method: reappraisal of interindividual variability factors. Ther Drug Monit 1999; 21:105–115Crossref, Medline, Google Scholar
81. Brosen K, Skjelbo E, Rasmussen BB, Poulsen HE, Loft S: Fluvoxamine is a potent inhibitor of cytochrome P450 1A2. Biochem Pharmacol 1993; 45:1211–1214Crossref, Medline, Google Scholar
82. Back DJ, Orme ML: Pharmacokinetic drug interactions with oral contraceptives. Clin Pharmacokinet 1990; 18:472–484Crossref, Medline, Google Scholar
83. Altamura AC, Sassella F, Santini A, Montresor C, Fumagalli S, Mundo E: Intramuscular preparations of antipsychotics: uses and relevance in clinical practice. Drugs 2003; 63:493–512Crossref, Medline, Google Scholar
84. Daniel WA: Mechanisms of cellular distribution of psychotropic drugs: significance for drug action and interactions. Prog Neuropsychopharmacol Biol Psychiatry 2003; 27:65–73Crossref, Medline, Google Scholar
85. Koyama H, Mori S, Sugioka N, Nishihara T, Nakajima K: Age-related alteration of haloperidol-serum protein binding. J Pharm Pharmacol 2003; 55:77–83Crossref, Medline, Google Scholar
86. Casey D: Neuroleptic drug-induced extrapyramidal syndromes and tardive dyskinesia. Schizophr Res 1991; 4:109–120Crossref, Medline, Google Scholar
87. Morgenstern H, Glazer W: Identifying risk factors for tardive dyskinesia among long-term outpatients maintained with neuroleptic medication. Arch Gen Psychiatry 1993; 50:723–733Crossref, Medline, Google Scholar
88. Yassa R, Jeste D: Gender differences in tardive dyskinesia: a critical review of the literature. Schizophr Bull 1992; 18:701–715Crossref, Medline, Google Scholar
89. Kamijo Y, Soma K, Nagai T, Kurihara K, Ohwada T: Acute massive pulmonary thromboembolism associated with risperidone and conventional phenothiazines. Circ J 2003; 67:46–48Crossref, Medline, Google Scholar
90. Priori SG, Schwartz PJ, Napolitano C, Bloise R, Ronchetti E, Grillo M, Vicentini A, Spazzolini C, Nastoli J, Bottelli G, Folli R, Cappelletti D: Risk stratification in the long-QT syndrome. N Engl J Med 2003; 348:1866–1874Crossref, Medline, Google Scholar
91. Hatta K, Takahashi T, Nakamura H, Yamashiro H, Asukai N, Matsuzaki I, Yonezawa Y: The association between intravenous haloperidol and prolonged QT interval. J Clin Psychopharmacol 2001; 21:257–261Crossref, Medline, Google Scholar
92. Seeman MV: Schizophrenic men and women require different treatment programs. J Psychiatr Treat Eval 1983; 5:143–148Google Scholar
93. Russell JM, Mackell JA: Bodyweight gain associated with atypical antipsychotics: epidemiology and therapeutic implications. CNS Drugs 2001; 15:537–551Crossref, Medline, Google Scholar
94. Homel P, Casey D, Allison DB: Changes in body mass index for individuals with and without schizophrenia, 1987–1996. Schizophr Res 2002; 55:277–284Crossref, Medline, Google Scholar
95. Allison DB, Mentore JL, Heo M, Chandler LP, Cappelleri JC, Infante MC, Weiden PJ: Antipsychotic-induced weight gain: a comprehensive research synthesis. Am J Psychiatry 1999; 156:1686–1696Abstract, Google Scholar
96. Baptista T, Kin NM, Beaulieu S, De Baptista EA: Obesity and related metabolic abnormalities during antipsychotic drug administration: mechanisms, management and research perspectives. Pharmacopsychiatry 2002; 35:205–219Crossref, Medline, Google Scholar
97. Hedenmalm K, Hagg S, Stahl M, Mortimer O, Spigset O: Glucose intolerance with atypical antipsychotics. Drug Saf 2002; 25:1107–1116Crossref, Medline, Google Scholar
98. Sernyak MJ, Leslie DL, Alarcon RD, Losonczy MF, Rosenheck R: Association of diabetes mellitus with use of atypical neuroleptics in the treatment of schizophrenia. Am J Psychiatry 2002; 159:561–566Link, Google Scholar
99. Jin H, Meyer JM, Jeste DV: Phenomenology of and risk factors for new-onset diabetes mellitus and diabetic ketoacidosis associated with atypical antipsychotics: an analysis of 45 published cases. Ann Clin Psychiatry 2002; 14:59–64Crossref, Medline, Google Scholar
100. Jensen DM, Damm P, Sorensen B, Molsted-Pedersen L, Westergaard JG, Ovesen P, Beck-Nielsen H: Pregnancy outcome and prepregnancy body mass index in 2,459 glucose-tolerant Danish women. Am J Obstet Gynecol 2003; 189:239–244Crossref, Medline, Google Scholar
101. Watkins ML, Rasmussen SA, Honein MA, Botto LD, Moore CA: Maternal obesity and risk for birth defects. Pediatrics 2003; 111:1152–1158Medline, Google Scholar
102. Kuruvilla A, Peedicayil J, Srikrishna G, Kuruvilla K, Kanagasabapathy AS: A study of serum prolactin levels in schizophrenia: comparison of males and females. Clin Exp Pharmacol Physiol 1992; 19:603–606Crossref, Medline, Google Scholar
103. Naidoo U,Kinon BJ, Gilmore JA, Liu H, Halbreich UM: Hyperprolactinemia in response to antipsychotic drugs: characterization across comparative clinical trials. Psychoneuroendocrinology 2003; 28(suppl 2):69–82Google Scholar
104. Wieck A, Haddad PM: Antipsychotic-induced hyperprolactinaemia in women: pathophysiology, severity and consequences: selective literature review. Br J Psychiatry 2003; 182:199–204Crossref, Medline, Google Scholar
105. Becker D, Liver O, Mester R, Rapoport M, Weizman A, Weiss M: Risperidone, but not olanzapine, decreases bone mineral density in female premenopausal schizophrenia patients. J Clin Psychiatry 2003; 64:761–766Crossref, Medline, Google Scholar
106. Abraham G, Paing WW, Kaminski J, Joseph A, Kohegyi E, Josiassen RC: Effects of elevated serum prolactin on bone mineral density and bone metabolism in female patients with schizophrenia: a prospective study. Am J Psychiatry 2003; 160:1618–1620Link, Google Scholar
107. Goff DC, Klibanski A: Hyperprolactinemia and bone mineral density: the potential impact of antipsychotic agents. Psychoneuroendocrinology 2003; 28(suppl 2):97–108Google Scholar
108. Aizenberg D, Sigler M, Weizman A, Barak Y: Anticholinergic burden and the risk of falls among elderly psychiatric inpatients: a 4-year case-control study. Int Psychogeriatr 2002; 14:307–310Crossref, Medline, Google Scholar
109. Hankinson SE, Willett WC, Michaud DS, Manson JE, Colditz GA, Longcope C, Rosner B, Speizer FE: Plasma prolactin levels and subsequent risk of breast cancer in postmenopausal women. J Natl Cancer Inst 1999; 91:629–634Crossref, Medline, Google Scholar
110. Wang PS, Walker AM, Tsuang MT, Orav EJ, Glynn RJ, Levin R, Avorn J: Dopamine antagonists and the development of breast cancer. Arch Gen Psychiatry 2002; 59:1147–1154Crossref, Medline, Google Scholar
111. Oksbjerg Dalton S, Munk Laursen T, Mellemkjaer L, Johansen C, Mortensen PB: Schizophrenia and the risk for breast cancer. Schizophr Res 2003; 62:89–92Crossref, Medline, Google Scholar
112. Compton MT, Miller AH: Sexual side effects associated with conventional and atypical antipsychotics. Psychopharmacol Bull 2001; 35:89–108Medline, Google Scholar
113. Compton MT, Miller AH: Antipsychotic-induced hyperprolactinemia and sexual dysfunction. Psychopharmacol Bull 2002; 36:143–164Medline, Google Scholar
114. Compton MT, Miller AH: Priapism associated with conventional and atypical antipsychotic medications: a review. J Clin Psychiatry 2001; 62:362–366Crossref, Medline, Google Scholar
115. Bobes J, Garc A-Portilla MP, Rejas J, Hern Ndez G, Garcia-Garcia M, Rico-Villademoros F, Porras A: Frequency of sexual dysfunction and other reproductive side-effects in patients with schizophrenia treated with risperidone, olanzapine, quetiapine, or haloperidol: the results of the EIRE study. J Sex Marital Ther 2003; 29:125–147Crossref, Medline, Google Scholar
116. Miller LJ: Sexuality, reproduction, and family planning in women with schizophrenia. Schizophr Bull 1997; 23:623–635Crossref, Medline, Google Scholar
117. Goldstein DJ, Corbin LA, Fung MC: Olanzapine-exposed pregnancies and lactation: early experience. J Clin Psychopharmacol 2000; 20:399–403Crossref, Medline, Google Scholar
118. Ito S, Lee A: Drug excretion into breast milk—overview. Adv Drug Deliv Rev 2003; 55:617–627Crossref, Medline, Google Scholar
119. Burt VK, Suri R, Altshuler L, Stowe Z, Hendrick VC, Muntean E: The use of psychotropic medications during breast-feeding. Am J Psychiatry 2001; 158:1001–1009Link, Google Scholar
120. Della-Giustina K, Chow G: Medications in pregnancy and lactation. Emerg Med Clin North Am 2003; 21:585–613Crossref, Medline, Google Scholar
121. Gardiner SJ, Kristensen JH, Begg EJ, Hackett LP, Wilson DA, Ilett KF, Kohan R, Rampono J: Transfer of olanzapine into breast milk, calculation of infant drug dose, and effect on breast-fed infants. Am J Psychiatry 2003; 160:1428–1431Link, Google Scholar
122. Croke S, Buist A, Hackett LP, Ilett KF, Norman TR, Burrows GD: Olanzapine excretion in human breast milk: estimation of infant exposure. Int J Neuropsychopharmacol 2002; 5:243–247Crossref, Medline, Google Scholar
123. Yoshida K, Smith B, Craggs M, Kumar R: Neuroleptic drugs in breast-milk: a study of pharmacokinetics and of possible adverse effects in breast-fed infants. Psychol Med 1998; 28:81–91Crossref, Medline, Google Scholar
124. Pinkofsky HB: Effects of antipsychotics on the unborn child: what is known and how should this influence prescribing? Paediatr Drugs 2000; 2:83–90Crossref, Medline, Google Scholar
125. Nilsson E, Lichtenstein P, Cnattingius S, Murray RM, Hultman CM: Women with schizophrenia: pregnancy outcome and infant death among their offspring. Schizophr Res 2002; 58:221–229Crossref, Medline, Google Scholar
126. Bennedsen BE, Mortensen PB, Olesen AV, Henriksen TB: Congenital malformations, stillbirths, and infant deaths among children of women with schizophrenia. Arch Gen Psychiatry 2001; 58:674–679Crossref, Medline, Google Scholar
127. Bennedsen BE, Mortensen PB, Olesen AV, Henriksen TB, Frydenberg M: Obstetric complications in women with schizophrenia. Schizophr Res 2001; 47:167–175Crossref, Medline, Google Scholar
128. Altshuler LL, Cohen L, Szuba MP, Burt VK, Gitlin M, Mintz J: Pharmacologic management of psychiatric illness during pregnancy: dilemmas and guidelines. Am J Psychiatry 1996; 153:592–606Link, Google Scholar
129. Olney JW, Farber NB, Wozniak DF, Jevtovic-Todorovic V, Ikonomidou C: Environmental agents that have the potential to trigger massive apoptotic neurodegeneration in the developing brain. Environ Health Perspect 2000; 108(suppl 3):383–388Google Scholar
130. Reidenberg MM: Evolving ways that drug therapy is individualized. Clin Pharmacol Ther 2003; 74:197–202Crossref, Medline, Google Scholar



