Quality of Care for Primary Care Patients With Anxiety Disorders
Abstract
OBJECTIVE: This study evaluated quality of care for primary care patients with anxiety disorders in university-affiliated outpatient clinics in Los Angeles, San Diego, and Seattle. METHOD: Three hundred sixty-six primary care outpatients who were diagnosed with panic disorder, generalized anxiety disorder, social phobia, and/or posttraumatic stress disorder (with or without major depression) were surveyed about care received in the prior 3 months. Quality indicators were mental health referral, anxiety counseling, and use of appropriate antianxiety medication during the previous 3 months. RESULTS: Approximately one-third of patients with anxiety disorders had received counseling from their primary care provider in the prior 3 months. Fewer than 10% had receiving counseling from a mental health professional that included multiple elements of cognitive behavior therapy. Approximately 40% had received appropriate antianxiety medications in the previous 3 months, although only 25% had received them at a minimally adequate dose and duration. Overall, fewer than one in three patients had received either psychotherapy or pharmacotherapy that met a criterion for quality care. In multivariate analyses, patients with comorbid depression and/or medical illness were more likely—and patients from ethnic minorities were less likely—to receive appropriate antianxiety medications. CONCLUSIONS: Rates of quality care for anxiety disorders are moderate to low in university-affiliated primary care practices. Although an appropriate type of pharmacotherapy was frequently used, it was often of inadequate duration. Cognitive behavior therapy was markedly underused. These findings emphasize the need for practice guidelines and implementation of quality improvement programs for anxiety disorders in primary care.
Anxiety disorders are common (a 12-month prevalence of 19.3%), costly, and associated with substantial disability (1–6). The prevalence of anxiety disorders in primary care settings is severalfold greater than in community settings (7–13). Patients with mood and anxiety disorders are likely to receive their only health care from general medical providers (14, 15). Although the quality of care for primary care patients with depression has been carefully scrutinized and found wanting (16–18)—leading to new guidelines for screening (19) and the testing of new intervention models (20–24)—relatively little research has been conducted to address the quality of care for anxious patients in primary care.
There is evidence to suggest that the quality of care for anxiety disorders in primary care settings may be particularly poor (25) and that anxious patients frequently leave the physician-patient transaction with substantial dissatisfaction, resulting from perceived unmet need (26). In a nationally representative sample, despite over 80% of adults with anxiety disorders having seen their primary care physicians, only approximately 20% received appropriate pharmacotherapy, and even fewer (approximately 10%) received appropriate counseling (25). In that population-based study, as in a study in the general medical sector (27), anxiety disorders co-occurring with depression increased the likelihood of counseling and the use of psychotropic medication in the general medical sector. To our knowledge, there are no prior studies that have focused primarily on the types and quality of care received by patients with a broad array of anxiety disorders in primary care settings.
The purpose of this study was to evaluate the process and quality of care for primary care patients with anxiety disorders in university-affiliated outpatient clinics in three West Coast U.S. cities (Los Angeles, San Diego, and Seattle). It was hypothesized that relatively few patients would be receiving evidence-based psychotherapies or pharmacotherapies but that the presence of comorbid major depression—which might be better recognized by primary care physicians, given the educational emphasis placed on detection of this disorder (19, 28)—would enhance the likelihood of receiving quality care. Other potential determinants of quality care (e.g., gender, ethnicity, income) were also examined, with the goal of identifying such patient characteristics that might then become the target for future efforts at quality improvement.
Method
Setting and Subjects
Data are from the baseline phase of the Collaborative Care for Anxiety and Panic Study, a randomized controlled trial of pharmacotherapy and cognitive behavior therapy for patients with panic disorder in primary care (29). The settings for this study were university-affiliated primary care clinics in Seattle, San Diego, and Los Angeles. The Seattle and Los Angeles clinics were internal medicine clinics, whereas San Diego also included family medicine clinics. The clinics were predominantly staffed by board-certified physicians, with a minority of care (between 15% and 30%) delivered by residents-in-training under attending supervision. Insurance was a mix of private (50%–80%) and public.
Eligible subjects were patients at these clinics who 1) were between 18 and 70 years old, 2) were English speaking, and 3) had access to a telephone. The subjects were recruited in clinic waiting rooms on high-volume days with the use of a brief self-report questionnaire that requested information about demographic characteristics, chronic medical illness, and anxiety and depressive symptoms. The latter included validated screening questions for panic disorder, social phobia, posttraumatic stress disorder (PTSD), generalized anxiety disorder, and major depressive disorder; positive predictive values for these instruments range from ∼0.6 to 0.8 (30, 31).
A total of 8,315 patients were screened in the waiting room. Those screened positive for any anxiety disorder and a random sample of subjects who screened positive for no disorder were invited to participate in a diagnostic telephone interview intended to confirm DSM-IV diagnoses and provide additional information about illness and care characteristics. The participation rate in the diagnostic interview was 60.7% (801 of 1,319 eligible). The patients (N=366) who met DSM-IV criteria for panic disorder, social phobia, PTSD, or generalized anxiety disorder are the subjects of this report. The study was approved by the institutional review boards of all three universities (the University of Washington, the University of California, Los Angeles, and the University of California, San Diego).
Diagnostic Interview and Quality-of-Care Indicators
The diagnostic interview was conducted on the telephone with modules from the telephone-validated World Health Organization’s 12-Month Composite International Diagnostic Interview (32, 33), which we modified (with several additional prompts) to enhance its ability to distinguish between panic disorder and social phobia (34). Diagnostic modules for panic disorder, social phobia, PTSD, and major depression were administered to all subjects; the generalized anxiety disorder module was added midway through the study and was administered to a subset of only 130 subjects. The Composite International Diagnostic Interview was followed by a more detailed set of questions about symptoms, comorbid conditions, health-related quality of life, and the use of services, including medications.
The telephone interview questioned respondents about the care they had received during the previous 3 months with their primary care physician. These questions were modeled after those administered in the Partners in Care study, for which data on the quality of care for depression in primary care have been published (18). Items assessed were
| 1. | Whether the clinician had counseled the patient for at least 5 minutes about a personal or emotional problem | ||||
| 2. | Whether the clinician had referred the patient to a mental health specialist for counseling (or whether such counseling was ongoing) | ||||
| 3. | Whether counseling that included any elements of cognitive behavior therapy (derived from a checklist that included examples of exposure instructions, etc.) had been provided by a mental health professional | ||||
| 4. | Whether the clinician had initiated medication for personal or emotional problems (or whether such treatment was ongoing) | ||||
From those measures, we derived an indicator of having any anxiety care (i.e., any treatment or counseling that might be relevant for anxiety) and retained separate indicators of anxiety counseling by the primary care physician, mental health referral, mental health counseling with any cognitive behavior therapy elements, and psychotropic medication management—all of which we considered to be quality indicators. With patient reports of the name and daily dose of each prescribed medication used in the previous 3 months, we derived separate indicators of
| 1. | The use of any psychotropic medication | ||||
| 2. | The use of any antianxiety medication (i.e., an antidepressant or a benzodiazepine; buspirone, which was prescribed to only six [1.6%] of the 366 patients in the study, was not included in this category because evidence for its efficacy is limited to generalized anxiety disorder, for which we had incomplete data) | ||||
| 3. | The use of any antianxiety medication in an appropriate daily dose for any duration | ||||
| 4. | The use of any antianxiety medication in an appropriate daily dose for at least 6 weeks | ||||
Determination of what was an antianxiety medication and what was an appropriate daily dose was made a priori by consensus of the psychiatrist investigators in the study based on consensus statements and their knowledge of the evidence-based pharmacotherapy literature for anxiety (35–39).
Statistical Analysis
In addition to describing overall levels of care, we used multivariate logistic regression analyses to estimate patterns of association between particular aspects of care and respondent demographic characteristics, comorbid illness attributes (i.e., chronic physical illness, major depression), and study site. Explanatory variables included patient demographic characteristics, depression and physical health status, and study site. The patient demographic variables examined were sex, education (high school or less versus more), age (50 or younger versus older), and income (below the poverty line versus at or above the poverty line). The sites were dichotomized as Seattle versus Southern California because we detected, using chi-square tests, significant (p<0.05) differences in race/ethnicity (Caucasian versus other) and income in the Seattle area versus either of the Southern California sites. The presence or absence of comorbid major depression (but not dysthymia, as this diagnostic module was not included in the study) was determined by the Composite International Diagnostic Interview. By using survey questions on the prevalence of chronic medical conditions (asthma, arthritis, lung disease, diabetes, hypertension, advanced coronary artery disease, heart failure, other heart disease, neurological conditions, gastrointestinal problems, eye problems, or migraines), we constructed a count of the number of reported conditions and, based on their distribution in this group, dichotomized subjects as having zero or one versus two or more chronic medical conditions.
We also compared the main quality indicators across anxiety diagnostic groups by using a separate multivariate logistic regression analysis in which the presence or absence of each diagnostic group was dummy-coded and included in a model that also contained site, ethnicity, medical illness, and depression as predictors. This analysis enabled us to determine if there were substantive differences in care received based on the presence or absence of particular anxiety disorders. Models were run with and without generalized anxiety disorder (which reduced the group size for the analyses because it was assessed only in a subgroup of subjects); the inferences were the same in either case.
For the multivariate logistic regression analyses, although a formal Bonferroni correction was not used, we considered predictors significant at the p<0.005 level to be statistically significant, and we interpreted the results in this statistical context. Adjusted odds ratios for the predictors, derived from the multivariate logistic regression analyses, are presented, along with 95% confidence intervals (CI).
Results
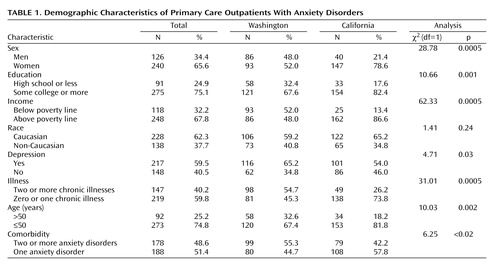
The demographic characteristics of the patients are shown in Table 1. The group was predominantly women, relatively well educated, and middle-aged or younger. The patients from Seattle (where half attended a public-sector hospital clinic) were significantly more likely to be below the poverty line (χ2=62.33, df=1, p<0.0005), men (χ2=28.78, df=1, p<0.0005), and physically sicker (χ2=31.01, df=1, p<0.0005) than patients from the other sites. Site (i.e., Seattle versus Southern California) was therefore used as a covariate in subsequent logistic regression analyses intended to identify predictors of types and quality of care.
There were 366 patients with one or more DSM-IV anxiety disorders included in the study. Of these, 255 (69.7%) had panic disorder with or without agoraphobia, 179 (48.9%) had social phobia, 122 (33.3%) had PTSD, and 77 (59.2% of the subgroup who were administered the Composite International Diagnostic Interview generalized anxiety disorder module) had generalized anxiety disorder; these numbers are not mutually exclusive and reflect extensive comorbidity. In fact, approximately one-half (N=178, 48.6%) of the patients had more than one anxiety disorder, with PTSD having the highest levels of anxiety comorbidity (106 of 122 cases, or 86.9%) and panic disorder the lowest (146 of 255 cases, or 57.3%).
Types and Quality of Care Received
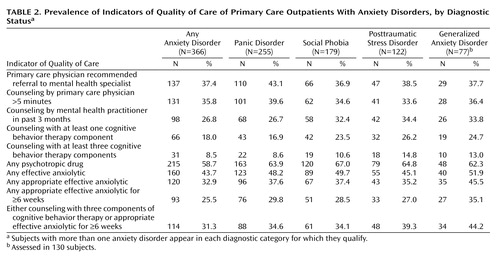
The unadjusted prevalence rates of the various types of care received, by diagnostic status, are shown in Table 2. In the preceding 3 months, according to their self-reports, 131 (35.8%) had been counseled by their primary care physician for at least 5 minutes, and 137 (37.4%) had been referred by their primary care physician to see a mental health specialist. Counseling by a mental health professional had been provided to 98 patients (26.8%), but only 31 (8.5%) reported that the counseling included three or more elements that would make it likely to be indicative of adequate quality cognitive behavior therapy. In terms of medication treatment, although more than half (58.7%) of the patients reported being prescribed a psychotropic medication in the previous 3 months and 160 (43.7%) reported receiving either an antidepressant or a benzodiazepine, only 93 (25.5%) had received these at an appropriate dose and for a minimally appropriate duration (i.e., 6 weeks). With the provision of counseling with three or more cognitive behavior therapy elements or appropriate pharmacotherapy at a minimally adequate dose or duration as indicative of quality care, only 114 patients (31.3%) had received care that met this criterion.
Care Received and Anxiety Disorder Type
Among the anxiety disorders, the presence of panic disorder was associated with increased odds of referral to a mental health practitioner (adjusted odds ratio=2.31, 95% CI=1.36–3.91, p=0.002), increased odds of receiving any psychotropic medication in the prior 3 months (adjusted odds ratio=2.76, 95% CI=1.60–4.77, p<0.0005), and increased odds of receiving quality pharmacotherapy in the prior 3 months (adjusted odds ratio=2.94, 95% CI=1.52–5.66, p=0.001). The presence of more than one anxiety disorder was not associated with a significantly increased likelihood of receiving either quality pharmacotherapy or psychotherapy.
Patient Characteristics and Quality of Care
A number of individual characteristics (apart from anxiety disorder diagnoses) were assessed within the group of patients with anxiety disorders as to whether they were differentially associated with the receipt of counseling by a mental health professional, counseling with at least three cognitive behavior therapy components (i.e., quality psychotherapy) (40), any antianxiety medicine, and appropriate pharmacotherapy at a minimally adequate dose or duration (i.e., quality pharmacotherapy). As noted earlier, these analyses used a multivariate model that included sex, ethnicity, age, poverty level, education level, site, comorbid medical illness, and comorbid depression to predict each quality outcome.
The presence of comorbid depression (i.e., major depression as diagnosed by the Composite International Diagnostic Interview) was the only consistent predictor of receipt of counseling from a mental health professional (34% with depression versus 17% without depression) (adjusted odds ratio=1.97, 95% CI=1.14–3.40, p<0.02) and of receiving counseling that included at least three cognitive behavior therapy components (12% with depression versus 3% without depression) (adjusted odds ratio=3.63, 95% CI=1.19–11.14, p<0.03), although neither of these relationships achieved our predetermined level of statistical significance of p<0.005.
The likelihood of receiving any antianxiety medicine was higher in the patients with comorbid depression (52% with depression versus 31% without depression) (adjusted odds ratio=1.89, 95% CI=1.16–3.07, p=0.01) or a greater burden of chronic disease (58% of the persons with two or more self-reported chronic physical conditions versus 34% with fewer self-reported chronic physical conditions) (adjusted odds ratio=2.02, 95% CI=1.20–3.40, p=0.009). It was significantly lower in non-Caucasians—our group was composed predominantly of Hispanics and African Americans, although both groups were too small to test separately—than in Caucasians (34% versus 50%) (adjusted odds ratio=0.42, 95% CI=0.26–0.68, p=0.001). Ethnicity was not, however, a significant predictor of the likelihood of receiving quality pharmacotherapy (adjusted odds ratio=0.59, 95% CI=0.34–1.04, p<0.07), whereas comorbid depression (35% of depressed versus 12% of nondepressed patients) (adjusted odds ratio=3.17, 95% CI=1.71–5.87, p<0.0005) was associated with a higher likelihood of receiving quality pharmacotherapy.
Discussion
There is a strong sentiment that the quality of American medical care is not what it should be and that improvements must be made (41, 42). In a survey of health care consumers in 12 U.S. metropolitan areas, quality was noted to vary widely across disorders, ranging from 79% of recommended care for senile cataract to 11% of recommended care for alcohol dependence (43). These provocative findings highlight the need to better understand the rates and determinants of quality care as they apply to the most common category of mental disorders—the anxiety disorders.
The majority of individuals with anxiety disorders receive most or all of their mental health care from primary care physicians (25). In this study of patients attending a university-affiliated primary care practice, we found that the rates of appropriate care for anxiety disorders were moderate to low. The rates of appropriate pharmacotherapy were somewhat lower (25%) than have been reported for depressed patients (35% to 42%) seen in managed care primary care settings (18), and the rates of appropriate psychotherapy (i.e., including at least several elements of cognitive behavior therapy) (44) were even lower. These findings are supportive of those obtained in a nationally representative sample of persons with probable anxiety disorders (25), which together call for studies to better understand the reasons underlying these low rates of quality care and the implementation of measures to improve upon them.
The low rates of quality care provided in the primary care setting should not be seen as impugning the efforts of primary care physicians. In fact, there is considerable evidence to suggest that even in specialty mental health settings, relatively few patients with anxiety disorders receive guideline-concordant, evidence-based pharmacotherapy or psychotherapy (44–46). For example, in a study of New Hampshire Medicare recipients, only 23% of the patients with PTSD who were treated in community mental health centers were given prescriptions for selective serotonin reuptake inhibitors, the only class of medications with strong evidence of efficacy for this condition (47). Thus, the problem of poor-quality care is by no means restricted to primary care settings and speaks to a much larger need to disseminate evidence-based mental health treatments to the practitioners who provide the majority of care for anxiety (and mood) disorders (48).
Physician characteristics have been shown to influence adherence to clinical practice guidelines (49), but these were not the focus of the present investigation, which looked at patient-related determinants of care. Several patient characteristics influenced the likelihood of receiving particular elements of care for anxiety. Non-Caucasians were less likely than Caucasians to receive any pharmacotherapy. These observations are consistent with studies in depression and may well reflect a lower preference for pharmacotherapeutic solutions to mental health problems among Hispanics and African Americans (50), although treatment biases on the part of clinicians are also a possibility. To the best of our knowledge, this is the first study to examine differences in rates of pharmacotherapy provision for anxiety disorders according to ethnic status. Consequently, our observations must be replicated and, if they are real, explained and addressed.
The patient characteristic that had the most robust relationship with a variety of care outcomes was the presence of comorbid major depression. Patients with anxiety disorders who also had major depression were more likely to receive counseling and much more likely to receive quality pharmacotherapy. We hypothesize that the past decade of educational efforts has, indeed, had an impact on practice patterns and that primary care physicians are attuned to the presence of depressive symptoms more than they are to anxiety symptoms at this point in time. Thus, the presence of depression increases the likelihood that appropriate treatments (which overlap, especially in the domain of pharmacotherapy) will be received. Of interest, the presence of comorbid medical disorders also increased the likelihood of receiving an antianxiety medication. It is unclear how and why medical illness would influence the provision of antianxiety pharmacotherapy, and this deserves to be further explored. One possibility is that patients who are physically sicker are seen more frequently by their primary care physicians, thereby providing more opportunities for mental disorders to be detected and treated. Given the finding that outcomes for depression may be worse when accompanied by chronic medical illness (51), this relationship between anxiety and chronic medical illness should be further studied.
A number of factors should be considered in interpreting our findings. First, it must be noted that many patients had, presumably, not been diagnosed by their primary care physician as suffering from an anxiety disorder. A limitation of our study is that we did not have reliable data about mental disorder diagnoses made by the primary care physician and were therefore unable to comment on the extent to which “knowledge” of diagnosis might have influenced the care provided. As has been noted elsewhere (25, 52, 53), primary care physicians have the difficult job of detecting mental disorders among persons who may not be coming in for psychological treatment, making the implementation of appropriate interventions all the more challenging. It remains to be seen whether the use of diagnostic aids (e.g., as part of routine screening, as has been proposed for depression) (19) to improve the recognition of anxiety disorders will lead to improved quality of care in this setting. Efforts in this regard in the case of depression treatment, it should be noted, have generally not yielded salutary effects (17), and preliminary observations in the case of panic disorder would lead to a similar conclusion (54).
Several other limitations of our work deserve mention. Our study group was a convenience group rather than a strictly random sample of patients seen in primary care. The representativeness of our group is therefore subject to question. It is conceivable that “sicker” patients agreed to participate in the study, which would bias our group to patients with more severe anxiety disorders. If this were the case, then our survey of care received might be skewed toward treatment of more severely ill patients, and the care received by less ill patients might systematically differ. The expectation would be, however, that less symptomatic patients would have even lower levels of care; as such, our estimate of the rates of quality of care could be considered an upper boundary on the true range of quality of care provided. The same caveat would apply to the characteristics of our clinics (i.e., university-affiliated clinics in major metropolitan areas) and the patients they serve (e.g., the average level of education was quite high) in that it might be predicted that the quality of care provided would be even lower in rural settings or with less educated patients.
We are limited to reports of care during the prior 3 months; it is possible that care might have been better (or worse) at other points in time. An additional limitation is that all information about care received is based on self-reports. As such, the data are subject to response and recall biases that might influence the findings in uncertain ways. In particular, we are sensitive to the difficulty in ascertaining whether elements of cognitive behavior therapy were correctly recalled and must therefore consider the possibility that the low reported rates of quality psychotherapy reflect a problem with measurement of this construct. In future work, the use of standardized procedures for assessing psychotherapy procedures according to patient report (55) would be well advised. We have greater confidence, however, in the veracity of our medication reporting, in part, because we asked respondents to confirm the names and dosages of their medicines by reading pill bottle labels to us on the telephone and/or by checking with their physicians if they were still uncertain.
Our findings have implications for policy and research. Anxiety disorders are disabling conditions that have received considerably less attention than depression. The spectrum of important mental disorders in primary care goes far beyond depression, and although it is true that anxiety disorders in primary care are frequently comorbid with depressive disorders (56), an argument can be made that there has been too much of a unitary focus on depression as almost equivalent to “a mental disorder,” with primary care physicians checking for depression only. Furthermore, although major efforts have been made in the past decade to destigmatize depressive disorders, the anxiety disorders lag behind in terms of public (and, perhaps, physician) awareness. The low levels of care observed in this study, in concert with the knowledge that optimal treatment of anxiety disorders is cost-effective (57), reinforce the need to pay more attention to anxiety disorders in primary care and to develop methods to increase the rates of patients with these conditions who receive evidence-based care (58).
 |
 |
Received Dec. 29, 2003; revision received March 7, 2004; accepted March 25, 2004. From the Department of Psychiatry, University of California, San Diego; RAND, Santa Monica, Calif.; the Department of Psychology and the Department of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles; the Department of Psychiatry and Behavioral Sciences, University of Washington School of Medicine, Seattle; and the Department of Psychiatry, University of Arkansas for Medical Science, North Little Rock, Ark. Address reprint requests to Dr. Stein, Department of Psychiatry, University of California, San Diego, 9500 Gilman Dr. (0985), La Jolla, CA 92093-0985; [email protected] (e-mail). Supported by NIMH grants MH-57835 and MH-64122 (to Dr. Stein), MH-57858 and MH-065324 (to Dr. Roy-Byrne), and MH-58915 (to Dr. Craske). The authors thank Bernadette Benjamin for assistance with data management and analysis.
1. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8–19Crossref, Medline, Google Scholar
2. Leon AC, Portera L, Weissman MM: The social costs of anxiety disorders. Br J Psychiatry Suppl 1995; 27:19–22Medline, Google Scholar
3. Roy-Byrne PP, Stein MB, Russo J, Mercier E, Thomas R, McQuaid JR, Katon WJ, Craske MG, Bystritsky A, Sherbourne CD: Panic disorder in the primary care setting: comorbidity, disability, service utilization, and treatment. J Clin Psychiatry 1999; 60:492–499Crossref, Medline, Google Scholar
4. Greenberg PE, Sisitsky T, Kessler RC, Finkelstein SN, Berndt ER, Davidson JRT, Ballenger JC, Fyer AJ: The economic burden of anxiety disorders in the 1990s. J Clin Psychiatry 1999; 60:427–435Crossref, Medline, Google Scholar
5. Mendlowicz MV, Stein MB: Quality of life in individuals with anxiety disorders. Am J Psychiatry 2000; 157:669–682Link, Google Scholar
6. Stein MB, Heimberg RG: Well-being and life satisfaction in generalized anxiety disorder: comparison to major depressive disorder in a community sample. J Affect Disord 2004; 79:161–166Crossref, Medline, Google Scholar
7. Ormel J, Von Korff M, Ustun B, Pini S, Korten A, Oldenhinkel T: Common mental disorders and disability across cultures: results from the WHO Collaborative Study on Psychological Problems in General Health Care. JAMA 1994; 272:1741–1748Crossref, Medline, Google Scholar
8. Sherbourne CD, Jackson CA, Meredith LS, Camp P, Wells KB: Prevalence of comorbid anxiety disorders in primary care outpatients. Arch Fam Med 1996; 5:27–34Crossref, Medline, Google Scholar
9. Olfson M, Fireman B, Weissman MM, Leon AC, Sheehan DV, Kathol RG, Hoven C, Farber L: Mental disorders and disability among patients in a primary care group practice. Am J Psychiatry 1997; 154:1734–1740Link, Google Scholar
10. Olfson M, Shea S, Feder A, Fuentes M, Nomura Y, Gameroff M, Weissman MM: Prevalence of anxiety, depression, and substance use disorders in an urban general medicine practice. Arch Fam Med 2000; 9:876–883Crossref, Medline, Google Scholar
11. Weiller E, Bisserbe JC, Boyer P, Lepine JP, Lecrubier Y: Social phobia in general health care: an unrecognized undertreated disabling disorder. Br J Psychiatry 1996; 168:169–174Crossref, Medline, Google Scholar
12. Nisenson LG, Pepper CM, Schwenk TL, Coyne JC: The nature and prevalence of anxiety disorders in primary care. Gen Hosp Psychiatry 1998; 20:21–28Crossref, Medline, Google Scholar
13. Stein MB, McQuaid JR, Pedrelli P, Lenox R, McCahill ME: Posttraumatic stress disorder in the primary care medical setting. Gen Hosp Psychiatry 2000; 22:261–269Crossref, Medline, Google Scholar
14. Katz SJ, Kessler RC, Lin E, Wells KB: Medication management of depression in the United States and Ontario. J Gen Intern Med 1998; 13:77–85Crossref, Medline, Google Scholar
15. Regier DA, Narrow WE, Rae DS, Manderscheid RW, Locke BZ, Goodwin FK: The de facto US mental and addictive disorders service system: Epidemiologic Catchment Area prospective 1-year prevalence rates of disorders and services. Arch Gen Psychiatry 1993; 50:85–94Crossref, Medline, Google Scholar
16. Katon W, Von Korff M, Lin E, Bush T, Ormel J: Adequacy and duration of antidepressant treatment in primary care. Med Care 1992; 30:67–76Crossref, Medline, Google Scholar
17. Rost K, Zhang M, Fortney J, Smith J, Coyne J, Smith GR Jr: Persistently poor outcomes of undetected major depression in primary care. Gen Hosp Psychiatry 1998; 20:12–20Crossref, Medline, Google Scholar
18. Wells KB, Schoenbaum M, Unutzer J, Lagomasino IT, Rubenstein LV: Quality of care for primary care patients with depression in managed care. Arch Fam Med 1999; 8:529–536Crossref, Medline, Google Scholar
19. Pignone MP, Gaynes BN, Rushton JL, Burchell CM, Orleans CT, Mulrow CD, Lohr KN: Screening for depression in adults: a summary of the evidence for the US Preventive Services Task Force. Ann Intern Med 2002; 136:765–776Crossref, Medline, Google Scholar
20. Katon W, Von Korff M, Lin E, Walker E, Simon GE, Bush T, Robinson P, Russo J: Collaborative management to achieve treatment guidelines: impact on depression in primary care. JAMA 1995; 273:1026–1031Crossref, Medline, Google Scholar
21. Katon W, Von Korff M, Lin E: Stepped collaborative care for primary care patients with depression. Arch Gen Psychiatry 1999; 56:1109–1115Crossref, Medline, Google Scholar
22. Wells KB, Sherbourne C, Schoenbaum M, Duan N, Meredith L, Unutzer J, Miranda J, Carney MF, Rubenstein LV: Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA 2000; 283:212–220Crossref, Medline, Google Scholar
23. Unutzer J, Katon W, Callahan CM, Williams JW Jr, Hunkeler E, Harpole L, Hoffing M, Della Penna RD, Noel PH, Lin EH, Arean PA, Hegel MT, Tang L, Belin TR, Oishi S, Langston C: Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA 2002; 288:2836–2845Crossref, Medline, Google Scholar
24. Simon GE, Ludman EJ, Tutty S, Operskalski B, Von Korff M: Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomized controlled trial. JAMA 2004; 292:935–942Crossref, Medline, Google Scholar
25. Young AS, Klap R, Sherbourne CD, Wells KB: The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry 2001; 58:55–61Crossref, Medline, Google Scholar
26. Kroenke K, Jackson JL, Chamberlin J: Depressive and anxiety disorders in patients presenting with physical complaints: clinical predictors and outcome. Am J Med 1997; 103:339–347Crossref, Medline, Google Scholar
27. Meredith L, Sherbourne C, Jackson C, Camp P, Wells K: Treatment typically provided for comorbid anxiety disorder. Arch Fam Med 1997; 6:231–237Crossref, Medline, Google Scholar
28. Williams JW, Noel PH, Cordes JA, Ramirez G, Pignone M: Is this patient clinically depressed? JAMA 2002; 287:1160–1170Crossref, Medline, Google Scholar
29. Roy-Byrne PP, Craske MG, Stein MB, Sullivan G, Bystritsky A, Katon WJ, Golinelli D, Sherbourne CD: Cognitive behavior therapy and medication for primary care panic disorder: sustained superiority to usual care, in Abstracts of the 2003 Annual Meeting of the American College of Neuropsychopharmacology. Nashville, Tenn, ACNP, 2003, number 83Google Scholar
30. Stein MB, Roy-Byrne PP, McQuaid JR, Laffaye C, Russo J, McCahill ME, Katon W, Craske MG, Bystritsky A, Sherbourne C: Screening for panic disorder in primary care. Psychosom Med 1999; 61:359–364Crossref, Medline, Google Scholar
31. Connor KM, Kobak KA, Churchill E, Katzelnick DJ, Davidson JRT: Mini-SPIN: A brief screening assessment for generalized social anxiety disorder. Depress Anxiety 2001; 14:137–140Crossref, Medline, Google Scholar
32. World Health Organization: Composite International Diagnostic Interview (CIDI), version 2.1. Geneva, Switzerland, WHO, 1997Google Scholar
33. Reed V, Gander F, Pfister H, Wittchen H-U: To what degree does the Composite International Diagnostic Interview (CIDI) correctly identify DSM-IV disorders? testing validity issues in a clinical sample. Int J Methods Psychiatr Res 1998; 7:142–155Crossref, Google Scholar
34. Means-Christensen A, Sherbourne CD, Roy-Byrne P, Craske MG, Bystritsky A, Stein MB: The Composite International Diagnostic Interview (CIDI-Auto): problems and remedies for diagnosing panic disorder and social phobia. Int J Methods Psychiatr Res 2003; 12:167–181Crossref, Medline, Google Scholar
35. American Psychiatric Association: Practice Guideline for the Treatment of Patients With Panic Disorder. Am J Psychiatry 1998; 155(May suppl)Google Scholar
36. Roy-Byrne PP, Stein MB, Bystritsky A, Katon W: Pharmacotherapy of panic disorder: guidelines for the family practitioner. J Am Board Fam Pract 1998; 11:282–290Crossref, Medline, Google Scholar
37. Ballenger JC, Davidson JRT, Lecrubier Y, Nutt DJ, Bobes J, Beidel DC, Ono Y, Westenberg HGM: Consensus statement on social anxiety disorder from the International Consensus Group on Depression and Anxiety. J Clin Psychiatry 1999; 59:54–60Google Scholar
38. Ballenger JC, Davidson JR, Lecrubier Y, Nutt DJ, Foa EB, Kessler RC, MacFarlane AC, Shalev AY: Consensus statement on posttraumatic stress disorder from the International Consensus Group on Depression and Anxiety. J Clin Psychiatry 2000; 61(suppl 5):60–66Google Scholar
39. Stein DJ: Algorithm for the pharmacotherapy of anxiety disorders. Curr Psychiatry Rep 2003; 5:282–288Crossref, Medline, Google Scholar
40. Roy-Byrne PP, Sherbourne CD, Craske MG, Stein MB, Katon W, Sullivan G, Means-Christensen A, Bystritsky A: Moving treatment research from clinical trials to the real world. Psychiatr Serv 2003; 54:327–332Link, Google Scholar
41. Rundall TG, Shortell SM, Wang MC, Casalino L, Bodenheimer T, Gillies RR, Schmittdiel JA, Oswald N, Robinson JC: As good as it gets? chronic care management in nine leading US physician organisations. BMJ 2002; 325:958–961Crossref, Medline, Google Scholar
42. Bodenheimer T: The American health care system—the movement for improved quality in health care. N Engl J Med 1999; 340:488–492Crossref, Medline, Google Scholar
43. McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, Kerr EA: The quality of health care delivered to adults in the United States. N Engl J Med 2003; 348:2635–2645Crossref, Medline, Google Scholar
44. Goisman RM, Warshaw MG, Keller MB: Psychosocial treatment prescriptions for generalized anxiety disorder, panic disorder, and social phobia, 1991–1996. Am J Psychiatry 1999; 156:1819–1821Abstract, Google Scholar
45. Yonkers KA, Ellison JM, Shera DM, Pratt LA, Cole JO, Fierman E, Keller MB, Lavori PW: Description of antipanic therapy in a prospective longitudinal study. J Clin Psychopharmacol 1996; 16:223–232Crossref, Medline, Google Scholar
46. Salzman C, Goldenberg I, Bruce SE, Keller MB: Pharmacologic treatment of anxiety disorders in 1989 versus 1996: results from the Harvard/Brown Anxiety Disorders Research Program. J Clin Psychiatry 2001; 62:149–152Crossref, Medline, Google Scholar
47. Mellman TA, Clark RE, Peacock WJ: Prescribing patterns for patients with posttraumatic stress disorder. Psychiatr Serv 2003; 54:1618–1621Link, Google Scholar
48. Frank E, Rush AJ, Blehar M, Essock S, Hargreaves W, Hogan M, Jarrett R, Johnson R, Katon WJ, Lavori P, McNulty JP, Niederehe G, Ryan N, Stuart G, Thomas SB, Tollefson GD, Vitiello B: Skating to where the puck is going to be: a plan for clinical trials and translation research in mood disorders. Biol Psychiatry 2002; 52:631–654Crossref, Medline, Google Scholar
49. Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, Rubin HR: Why don’t physicians follow clinical practice guidelines? a framework for improvement. JAMA 1999; 282:1458–1465Crossref, Medline, Google Scholar
50. Cooper LA, Gonzales JJ, Gallo JJ, Rost KM, Meredith LS, Rubenstein LV, Wang NY, Ford DE: The acceptability of treatment for depression among African-American, Hispanic, and white primary care patients. Med Care 2003; 41:479–489Medline, Google Scholar
51. Iosifescu DV, Nierenberg AA, Alpert JE, Smith M, Bitran S, Dording C, Fava M: The impact of medical comorbidity on acute treatment in major depressive disorder. Am J Psychiatry 2003; 160:2122–2127Link, Google Scholar
52. Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS: The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA 2003; 289:3095–3105Crossref, Medline, Google Scholar
53. Kirmayer LJ, Robbins JM, Dworkind M, Yaffe MJ: Somatization and the recognition of depression and anxiety in primary care. Am J Psychiatry 1993; 150:734–741Link, Google Scholar
54. Roy-Byrne PP, Katon W, Cowley DS, Russo JE, Cohen E, Michelson E, Parrot T: Panic disorder in primary care: biopsychosocial differences between recognized and unrecognized patients. Gen Hosp Psychiatry 2000; 22:405–411Crossref, Medline, Google Scholar
55. Steketee G, Perry JC, Goisman RM, Warshaw MG, Massion AO, Peterson LG, Langford L, Weinshenker N, Farreras IG, Keller MB: The psychosocial treatments interview for anxiety disorders: a method for assessing psychotherapeutic procedures in anxiety disorders. J Psychother Pract Res 1997; 6:194–210Medline, Google Scholar
56. Rodriguez BG, Weisberg RG, Pagano ME, Machan JT, Culpepper L, Keller MB: Frequency and patterns of psychiatric comorbidity in a sample of primary care patients with anxiety disorders. Compr Psychiatry 2004; 45:129–137Crossref, Medline, Google Scholar
57. Issakidis C, Sanderson K, Corey J, Andrews G, Lapsley H: Modeling the population cost-effectiveness of current and evidence-based optimal treatment for anxiety disorders. Psychol Med 2004; 34:19–35Crossref, Medline, Google Scholar
58. Stein MB: Attending to anxiety disorders in primary care. J Clin Psychiatry 2003; 64(suppl 15):35–39Google Scholar



