Cautious Optimism for a New Treatment Option for Body-Focused Repetitive Behavior Disorders
In this issue, Grant et al. (1) describe strikingly positive results for a randomized, double-blind, placebo-controlled study of memantine for body-focused repetitive behavior (BFRB) disorders. On the study’s primary outcome measure—change in score on a modified version of the NIHM Trichotillomania Symptom Severity Scale—the memantine group showed a 56% reduction in severity, compared with 9% in the control group (p<0.0001, Hedges’ g=1.76), with statistically significant differences emerging at week 4. Additionally, the memantine group had a 33% reduction in score on a modified version of the self-reported Massachusetts General Hospital Hairpulling Severity Scale, compared with 16% in the control group (p=0.0003), and 60.5% participants in the memantine group had scores indicating “very much improved” or “much improved” on the Clinical Global Impressions improvement scale (CGI-I), compared with 8.3% in the control group (p<0.0001). Dropout rates were similar between the two groups (∼20%), and only two participants in the memantine group withdrew due to medication side effects (dizziness), compared with three in the control group. There were no reported serious adverse events.
BFRBs are common and include a variety of “grooming behaviors,” such as repetitive hair pulling, skin picking, cheek biting, and nail biting. They are predominantly subclinical, with upwards of 60% of individuals engaging in one or more BFRBs (2). When these behaviors are frequent despite repeated attempts to stop, cause physical impact, and lead to clinically significant distress or impairment, they are characterized as BFRB disorders, or “pathological BFRBs.” Trichotillomania and skin-picking disorder, the two BFRB disorders treated in this study, are characterized, respectively, by the pulling out of one’s hair and picking of one’s skin and an inability to stop despite the physical impact and psychosocial impairment. Although prevalence rates of pathological BFRBs vary, typically they are believed to affect between ∼1.5% and 4% of the general population.
BFRB disorders notably have both compulsive and addictive (impulsive) qualities (3). Although BFRBs are characterized as obsessive-compulsive-related disorders in DSM-5 because they share phenomenological, genetic, and neurobiological features with obsessive-compulsive disorder (OCD), BFRBs were historically characterized in DSM as impulse control disorders. BFRB disorders live at the neurobiological interface of “wanting,” “liking,” and “needing” (3) and straddle the line between what is voluntary and involuntary.
As Grant et al. point out, BFRB disorders are frequently debilitating. Individuals with pathological BFRBs can spend hours a day picking or pulling and engaging in efforts to conceal the physical impact of their symptoms. There are also significant psychosocial repercussions, including reduced quality of life, worse self-esteem, negatively impacted career aspirations, and increased rates of alcohol and substance use disorders (4–6). Despite their severe negative impact and often chronic course, BFRB disorders are underrecognized, understudied, and undertreated. Although behavioral treatments for BFRB disorders (e.g., habit reversal therapy) have demonstrated a significant benefit (effect size, 1.1) (7), finding an accessible and experienced habit reversal therapist is often difficult. Pharmacological treatment trials have generally been few in number, and disappointing in outcome. In a large study that explored self-reported functional impairment and treatment utilization, only 15% of adults with trichotillomania reported improvement from treatments received in the community (8).
For this reason, studies that address treatment options for pathological BFRBs are greatly needed. At present, there are no pharmacological options approved by the U.S. Food and Drug Administration for BFRB disorders. Candidate pharmacological interventions for trichotillomania have included a variety of selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants, anticonvulsants, dopamine-blocking agents, antioxidants, glutamate modulators, atypical antidepressants, and opioid antagonists (9). Regarding trichotillomania in particular, there is preliminary, albeit limited, evidence for N-acetylcysteine (NAC), a glutamate modulator/antioxidant, and for clomipramine (10) and olanzapine (11). However, the vast majority of the randomized controlled clinical trials have been negative, and those that have been positive often involve small sample sizes and lack replication. Clearly, individuals suffering from BFRB disorders are greatly in need of well-tolerated, reliably effective medication treatment options.
In the Grant et al. study, 100 adults with trichotillomania and/or skin-picking disorder were randomized in a 1:1 ratio to receive either memantine (up to 20 mg/day) or placebo. Participants with commonly co-occurring conditions, such as anxiety, depression, and OCD, were included, as were those engaged in additional treatments, so long as these treatments were stable and not adjusted during the study. The memantine and control groups did not differ statistically from one another in demographic measures or baseline clinical characteristics. Of note, almost 45% of participants in both groups were taking antidepressant medications, and almost 25% of participants in both groups were already engaged in some form of nonpharmacological therapy.
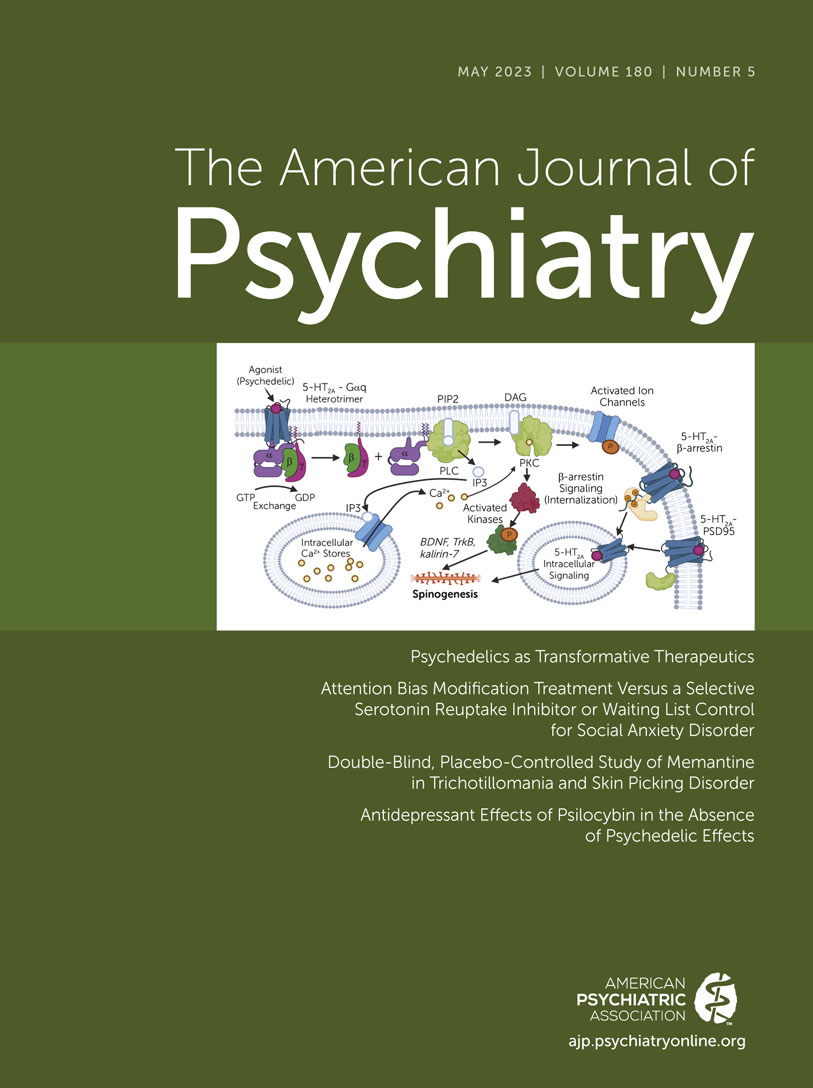
Considering the significant results reported by Grant et al., memantine would be a welcome addition to the meager set of pharmacologic options we currently have for pathological BFRBs. Glutamate modulators are generally safe and well-tolerated and are often used for prolonged periods of time (e.g., in dementia treatment). As a glutamatergic agent, memantine also aligns with the putative pathophysiological dysregulation of the neural circuity implicated in pathological BFRBs, namely, the frontocortical-striatal-thalamo-cortical circuitry. This circuitry is believed to be involved in habit formation and inhibitory control, and as its primary excitatory neurotransmitter is glutamate, modulation of glutamate is a fitting treatment target.
Grant and colleagues’ study has many strengths, including a large sample size, inclusive inclusion criteria that could allow for better generalization, and balanced groups with regard to clinical and demographic characteristics. Additionally, the reduction of 60.5% in score on the modified NIHM Trichotillomania Symptom Severity Scale in the memantine group was consistent with trichotillomania treatment response criteria (12). However, while this study is very promising, there are a few aspects that warrant further examination prior to suggesting that memantine be considered as a first-line treatment for BFRB disorders.
For instance, the authors combined trichotillomania and skin-picking disorder into a single treatment-targeting category, which does not have precedence in BFRB treatment research. While trichotillomania and skin-picking disorder do have significant overlap and are conceptualized as similar disorders, there are indeed differences between the two that would suggest the importance of individual analyses, particularly in a treatment study. For example, it has been hypothesized that skin-picking disorder may have more overlap with OCD, which we know responds to SSRIs, compared to trichotillomania (13, 14), and different responses to medications in trichotillomania and skin-picking disorder have been reported (15).
Another factor worth considering is that only 6% of this study’s participants had an OCD diagnosis. This contrasts with 29% of individuals reporting OCD in a large trichotillomania convenience sampling study (16), and an average of 15% reporting co-occurring OCD across multiple trichotillomania studies (5). This discrepancy raises questions as to whether the results would generalize to a BFRB population with a more typical comorbidity profile.
A reported finding worth noting is the rather low placebo response rate in this study. Previous randomized controlled trials of BFRB disorders, particularly trichotillomania, have shown high placebo response rates, in one study averaging 31% across pooled samples from several trials (17). The finding of a very low placebo response rate (8%) in this trial likely contributed to the statistically significant superior performance of memantine. In contrast, in three recently failed double-blind, placebo-controlled treatment studies from Grant and colleagues’ group, placebo response rates (based on CGI-I score) were 35.3% (vs. 42% for inositol), 31% (vs. 41% for milk thistle), and 50% (vs. 67% for dronabinol) (18–20). Further information that can help us better understand the unusually low placebo response findings reported in this study might guide future studies to employ similar methods. Alternatively, future studies could consider utilizing a crossover design to facilitate intra-individual comparisons for memantine versus placebo. An additional variable that may influence findings is the typical waxing and waning of symptoms commonly seen in BFRB disorders. Longer-term outcome data could help adjust for naturalistic variation in symptom severity.
It is also prudent to consider this study in the context of previous work examining glutamate modulators in the treatment of obsessive-compulsive-related disorders, including pathological BFRBs. As we noted above, targeting the glutamate pathways, which are believed to be mechanistically implicated in the neurobiology of impulsive-compulsive repetitive behaviors, is rational. However, despite some early successes, mainly in open-label trials, larger, well-controlled studies using glutamate modulators (e.g., riluzole, memantine, lamotrigine, NAC) have been less encouraging (21). For example, despite NAC being widely regarded as a first-line non-behavioral treatment for BFRBs, a recent literature review (22) summarized the doubtful state of NAC’s contribution to the field, finding that the data on NAC in these disorders are “derived from few clinical trials and case reports assessing small numbers of patients” and that “longer studies with longer durations are needed to fully establish the efficacy of NAC in these disorders.” The present memantine study thus appears to be a welcome exception to the extant literature.
Positive studies, such as that reported here by Grant et al., are important and help pave the way for further interest and treatment trials for pathological BFRBs, including further exploration of mechanistically informed treatment targets. Despite the reservations noted above regarding a potential new treatment for disorders that have historically been so difficult to treat, this is an encouraging finding that should permit cautious optimism for those who suffer with BFRB disorders.
1. : Double-blind placebo-controlled study of memantine in trichotillomania and skin-picking disorder. Am J Psychiatry 2023; 180:348–356Abstract, Google Scholar
2. : Body-focused repetitive behaviors: more prevalent than once thought? Psychiatry Res 2018; 270:389–393Crossref, Medline, Google Scholar
3. : Disentangling reward processing in trichotillomania: “wanting” and “liking” hair pulling have distinct clinical correlates. J Psychopathol Behav Assess 2019; 41:271–279Crossref, Medline, Google Scholar
4. : Trichotillomania: impact on psychosocial functioning and quality of life. Behav Res Ther 2005; 43:869–884Crossref, Medline, Google Scholar
5. : Comorbidity and quality of life in adults with hair pulling disorder. Psychiatry Res 2016;239:12–19Crossref, Medline, Google Scholar
6. : Trichotillomania: a current review. Clin Psychol Rev 2010; 30:181–193Crossref, Medline, Google Scholar
7. : Systematic review: pharmacological and behavioral treatment for trichotillomania. Biol Psychiatry 2007; 62:839–846Crossref, Medline, Google Scholar
8. : The Trichotillomania Impact Project (TIP): exploring phenomenology, functional impairment, and treatment utilization. J Clin Psychiatry 2006; 67:1877–1888Crossref, Medline, Google Scholar
9. : Pharmacotherapy for trichotillomania. Cochrane Database Syst Rev 2021; 9:CD007662Medline, Google Scholar
10. : Pharmacological and behavioral treatment for trichotillomania: an updated systematic review with meta-analysis. Depress Anxiety 2020; 37:715–727Crossref, Medline, Google Scholar
11. : A randomized, double-blind, placebo-controlled trial of olanzapine in the treatment of trichotillomania. J Clin Psychiatry 2010; 71:1336–1343Crossref, Medline, Google Scholar
12. : Identifying standardized definitions of treatment response in trichotillomania: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry 2019; 89:446–455Crossref, Medline, Google Scholar
13. : Prevalence and predictors of hair pulling disorder and excoriation disorder in Tourette syndrome. Eur Child Adolesc Psychiatry 2018; 27:569–579Crossref, Medline, Google Scholar
14. : How related are hair pulling disorder (trichotillomania) and skin picking disorder? A review of evidence for comorbidity, similarities, and shared etiology. Clin Psychol Rev 2012; 32:618–629Crossref, Medline, Google Scholar
15. : Assessment and treatment of trichotillomania (hair pulling disorder) and excoriation (skin picking) disorder. Clin Dermatol 2018; 36:728–736Crossref, Medline, Google Scholar
16. : Prevalence, gender correlates, and co-morbidity of trichotillomania. Psychiatry Res 2020; 288:112948Crossref, Medline, Google Scholar
17. : Placebo response in trichotillomania. Int Clin Psychopharmacol 2017; 32:350–355Crossref, Medline, Google Scholar
18. : Milk thistle treatment for children and adults with trichotillomania: a double-blind, placebo-controlled, crossover negative study. J Clin Psychopharmacol. 2019; 39:129–134Crossref, Medline, Google Scholar
19. : Tetrahydrocannabinol fails to reduce hair pulling or skin picking: results of a double-blind, placebo-controlled study of dronabinol. Int Clin Psychopharmacol 2022; 37:14–20Crossref, Medline, Google Scholar
20. : A double-blind, placebo-controlled study of inositol in trichotillomania. Int Clin Psychopharmacol 2017; 32:107–114Crossref, Medline, Google Scholar
21. : Harmonizing the neurobiology and treatment of obsessive-compulsive disorder. Am J Psychiatry 2021; 178:17–29Link, Google Scholar
22. : The potential of N-acetylcysteine for treatment of trichotillomania, excoriation disorder, onychophagia, and onychotillomania: an updated literature review. Int J Environ Res Public Health 2022; 19:6370Crossref, Medline, Google Scholar