Depression and Cognitive Complaints Following Mild Traumatic Brain Injury
Abstract
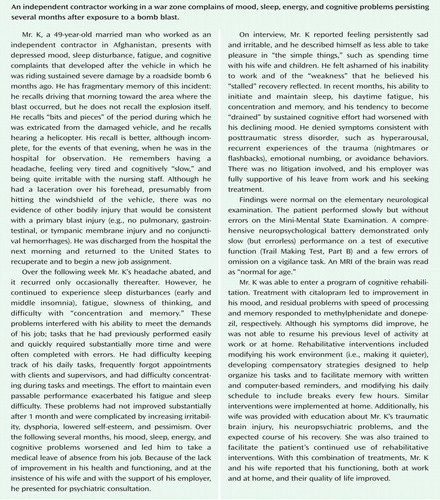
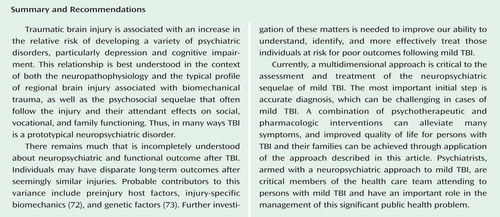
Traumatic brain injury (TBI) is a common occurrence with multiple possible neuropsychiatric sequelae, including problems with cognition, emotion, and behavior. While many individuals experience significant improvement over the first months following mild TBI, a nontrivial minority will develop persistent, functionally impairing post-TBI symptoms. Depression and cognitive impairment are among the most common such symptoms, and they may respond to a combination of rehabilitative and pharmacologic treatments. This article discusses the clinical approach to treating an individual with depression and cognitive complaints following mild TBI. Recommendations regarding the diagnosis, evaluation, and treatment of these problems are offered.
Traumatic brain injury (TBI) refers to a physiologically significant disruption of brain function resulting from the application of external physical force, including acceleration/deceleration forces. Evidence of disrupted brain function at the time force is applied may include loss of consciousness; loss of memory for events immediately before (retrograde amnesia) or after (anterograde amnesia) the event, collectively referred to as posttraumatic amnesia; an alteration in mental state (“dazed and confused”); a focal neurological deficit; or some combination of these (1 , 2) . TBI severity is divided into mild, moderate, and severe categories, primarily on the basis of the duration of loss of consciousness, duration of posttraumatic amnesia, and/or Glasgow Coma Scale (3) score at the time of admission to the emergency department or hospital. Mild TBI describes injuries that result in an admission Glasgow score in the range of 13–15; that produce a loss of consciousness of less than 30 minutes, if loss of consciousness occurs at all, and after which Glasgow scores are in the range of 13–15; and/or after which the duration of posttraumatic amnesia is less than 24 hours. Injuries that result in an admission Glasgow score <13 or that produce a duration of loss of consciousness or posttraumatic amnesia that exceeds these criteria are categorized as moderate or severe (1) .
Each year in the United States, approximately 1–2 million people sustain a TBI (4 , 5) ; most of these (about 80%) are mild TBIs (5) . Among U.S. military and civilian personnel serving in Iraq and Afghanistan, TBI is among the most common injuries, with an estimated 15%–20% of soldiers experiencing a mild TBI during their deployment in these theaters (6 , 7) .
Post-TBI cognitive, emotional, behavioral, physical, and psychosocial problems (collectively referred to here as “neuropsychiatric”) are a frequent and substantial source of at least temporary disability and stress to TBI survivors and their families (8 , 9) . These post-TBI neuropsychiatric impairments contribute to disability after TBI, which becomes a chronic problem for an estimated 3.17 million Americans (10) . Although the majority of individuals with mild TBI will recover fully, even without specific intervention (11 , 12) , a nontrivial minority of persons with mild TBI develop chronic posttraumatic neuropsychiatric problems and significant disability (13) .
Pathophysiology
Injury to the brain occurs as a result of contact (or impact) forces, inertial (acceleration or deceleration) forces, or both (14) . The anterior and inferior frontal and temporal areas of the brain are those most commonly and most severely affected by impact forces (15) . Inertial, and particularly rotational, forces stretch and strain white matter in these and other areas (the upper brainstem, the parasagittal white matter of the cerebrum, the corpus callosum, and the gray-white matter junctions of the cerebral cortex), resulting in diffuse (or, more accurately, multifocal) axonal injury (16) .
The conflicts in Iraq and Afghanistan, as well as the use of explosive devices in other regions of political unrest, have called attention to the effects of blast-related TBI (13) . Although primary blast can cause brain injury, the effect of primary blast is greatest at air-tissue interfaces. Thus, primary blast most often damages air-filled organs, such as the lungs and colon, or those at air-fluid (tissue-density) interfaces, such as the tympanic membranes and the eyes (17 , 18) . In the absence of a blast wave of a magnitude sufficient to damage the most blast-vulnerable organs, the effect of blast on the brain is uncertain and is a matter of controversy (18) . Secondary and tertiary blast effects are common mechanisms of blast-related TBI, affecting the brain via contact and inertial forces—for example, the sudden acceleration/deceleration and rotation of an individual in a vehicle displaced by the force of the blast or by objects driven by the blast through the vehicle and against the individual’s head.
Biomechanical injury is accompanied by a cascade of injurious intra- and extracellular processes (14 , 16) . Injury-induced calcium and magnesium dysregulation, excitatory amino acid excesses, calcium-regulated protein activation, mitochondrial dysfunction, free-radical formation, and proteolysis are major elements of this postinjury cytotoxic cascade and contribute to traumatically induced neuronal injury and cell death. TBI also induces excessive neurotransmitter release, including functionally disruptive elevations in cerebral glutamate, acetylcholine, dopamine, norepinephrine, and serotonin levels (19) . Although intracerebral levels of most of these neurotransmitters appear to normalize in the days to weeks following the injury, chronic cholinergic deficits, as well as chronic primary or secondary dysfunction in dopaminergic, noradrenergic, and serotonergic systems, appear to be relatively common consequences of TBI (19 , 20) .
The pathophysiology of TBI is best viewed as a product not only of biomechanical forces but also of the cytotoxic cascade, neurotransmitter disturbances, and intracranial or systemic complications. Although TBI can affect any area of the brain, there is a relatively consistent pattern of regional cerebral vulnerability to injury, whether mild or more severe. That pattern of regional vulnerability explains the types of neuropsychiatric problems commonly experienced by persons with TBI ( Table 1 ).
Evaluation for Traumatic Brain Injury
When a patient presents for evaluation of neuropsychiatric problems that may be the result of a TBI, it is important initially to determine whether the event preceding those problems in fact produced a TBI. The patient is asked first to describe the event; the clinician then determines whether the event involved the application of external physical force (e.g., a blow to the head) or acceleration/deceleration forces (e.g., sudden start, stop, or alteration of the direction of head movement). If an external physical force was present, there needs to be evidence of immediate physiologic disruption of brain function, including loss of consciousness, posttraumatic amnesia, altered mental status of any duration (dazed, confused, “seeing stars”), and/or a focal neurological deficit (2) .
There are several caveats to bear in mind when interpreting this information. First, because of the retrospective nature of evaluating a TBI—days, weeks, or months after the event—the potential for misreporting the event and its immediate neuropsychiatric manifestations is significant. Second, it is difficult to gauge accurately the mechanics, severity, and effects of an injury after the fact. In many cases, an informed but subjective clinical judgment will be required to confirm or rule out the diagnosis of TBI. Third, patients (and some clinicians) frequently misinterpret the immediate sequelae of TBI and their diagnostic implications. For example, a patient unable to recall portions of the event may misinterpret impaired recall due to posttraumatic amnesia as loss of consciousness. Fourth, the absence of evidence supporting a TBI in the medical record does not constitute evidence of absence of a TBI. Many patients with mild TBI do not go to a hospital at the time of injury. Moreover, a recent study (21) demonstrated that for those who did present to a hospital, emergency room records failed to document TBI in 56% of cases that study personnel identified as meeting the Centers for Disease Control and Prevention case definition for mild TBI. Fifth, the patient who states that he or she was “dazed,” “confused,” or “saw stars” may be reporting phenomena consistent with a mild TBI, an acute stress reaction, cerebral dysfunction produced by other injury-related physiologic disturbances (e.g., hypotension, hypoxia, toxin/gas inhalation), or some combination of these. Sixth, conventional clinical neuroimaging of the brain, including MRI, is often interpreted as “normal” in persons with mild TBI. A normal MRI of the brain after mild TBI does not suggest the absence of injury but instead indicates only that any changes in the brain caused by the TBI are below the detection threshold of conventional clinical MRI. There are techniques that may increase the sensitivity of MRI to changes in brain structure resulting from mild TBI, including fluid-attenuated inversion recovery, gradient recalled echo, and susceptibility-weighting techniques, as well as the use of high-field (3-T) scanners. Recent work suggests that diffusion tensor imaging is a promising method for detecting alterations in the integrity of white matter resulting from mild TBI (22 , 23) , although its application in clinical practice will require refinement to determine its usefulness as a diagnostic measure.
The tendency of medical personnel to miss or misunderstand mild TBI and its consequences is shared by the general public (24 , 25) . Such misconceptions raise suspicion and doubt about the veracity of TBI survivors’ clinical complaints, fueled, in part, by portrayals of mild TBI in cartoons and movies as “head injuries” or “concussions” that produce little immediate impairment and from which unrealistically rapid and complete recoveries are made.
After a diagnosis of TBI is made, the next step in the evaluation is to characterize the clinical problems with which the patient presents as well as the relationship of these problems, if any, to the TBI. The neuropsychiatric sequelae of mild TBI include problems with cognition (attention, concentration, executive functioning, memory, and speed of information processing) (19) ; psychiatric symptoms (personality changes, affective disorders, anxiety disorders, psychosis, sleep disorders, aggression, and irritability) (26) , and physical problems, such as headache, chronic pain, vision impairment, dizziness, and, rarely, epilepsy (27) . Figure 1 describes the most common posttraumatic neuropsychiatric problems following TBI. While the development and persistence of these symptoms are often described as a “postconcussion syndrome,” these symptoms occur in all severities of TBI. Moreover, it is not clear that they conform to the concept of a “syndrome”: the development of each symptom is not clearly linked to that of any other, and the symptoms’ resolution and response to treatment are frequently uncoupled; that is, they do not necessarily follow the same recovery trajectory (28) .
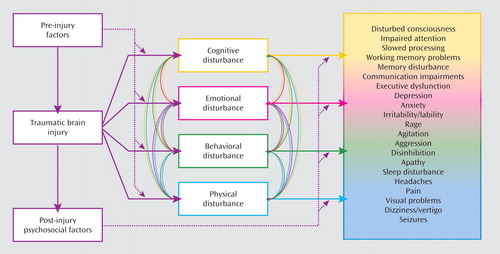
a Preinjury factors include age, gender, neurogenetics, baseline cognitive function, psychiatric conditions, substance abuse, socioeconomic environment, and risk-taking behaviors, among others. Injury characteristics, particularly location, type, and severity of neural damage, predict problems in the four domains of neuropsychiatric function: cognition, emotion, behavior, and physical function. Preinjury factors modify the development of problems in each of these neuropsychiatric domains after traumatic brain injury. The development of symptoms in one of these neuropsychiatric domains also affects the development and expression of symptoms in one or more of the other domains (e.g., depression worsens cognition, increases agitation and aggression, increases the number and perceived severity of posttraumatic physical symptoms, and so on). In combination, preinjury factors, injury characteristics, and the interactions between them produce posttraumatic neuropsychiatric symptoms (a partial list of which is presented on the right side of the figure). Postinjury factors, such as social support, timely medical and rehabilitative treatments, socioeconomic status, and medicolegal issues, also influence the expression, persistence, and remission of neuropsychiatric symptoms. Used with permission from Silver JM, Arciniegas DB: Pharmacotherapy of neuropsychiatric disturbances, in Brain Injury Medicine: Principles and Practice. Edited by Zasler ND, Katz DI, Zafonte RD. New York, Demos Medical Publishing, 2008, pp. 963–994.
In general, relatively rapid recovery is expected after mild TBI (see reference 27 for a review), with about half of patients recovering fully by the end of the first month and 80%–90% recovering by 6–12 months after sustaining the injury. Nonetheless, it is our practice to institute treatment when functionally significant neuropsychiatric symptoms are present. Education, counseling, and rehabilitative interventions may facilitate recovery and lessen the likelihood that the patient will develop persistent postconcussive symptoms (29 , 30) , and hence these are the initial components of neuropsychiatric treatment in this population. Given the absence of compelling evidence that medication treatment hastens recovery in mild TBI, we recommend that the decision to initiate pharmacotherapy be decided in partnership with the patient and his or her family. The goals of pharmacotherapy are to reduce the effects of such symptoms on the patient’s functioning, quality of life, and recovery and to limit the likelihood that the symptoms will become a chronic problem and contribute to long-term disability. Expeditious treatment of depression after TBI is particularly important, because its successful treatment may also alleviate other postconcussive symptoms, such as anergia, insomnia, irritability, and cognitive impairments; reduce suicidal thoughts and/or behavior; and improve psychosocial function and quality of life.
Depression Following Traumatic Brain Injury
Estimates of posttraumatic depression range from 10% to 77% (see reference 31 for a review). Although depression occurs most often in the first year after TBI, the risk of developing depression remains elevated for decades thereafter. Preinjury factors (such as mood and anxiety disorders, psychosocial dysfunction, and alcohol abuse), injury factors (such as left ventrolateral and dorsolateral injury and serotonergic dysfunction), and postinjury factors (such as postconcussive symptoms, psychosocial dysfunction, and lack of social supports) contribute to the development of depression after TBI, although the relevance of each factor varies among patients (32) . Early posttraumatic depression may be more strongly related to a host-injury interaction, whereas late posttraumatic depression may be more strongly influenced by psychological and psychosocial factors (33 – 35) .
Depression after mild TBI is associated with self-reported increases in the number and perceived severity of other postconcussive symptoms, including headache, dizziness, and blurred vision (36 – 38) . In persons with mild or more severe TBI, depression also increases anger, aggression, the risk of suicidality, and cognitive dysfunction (37 , 39 – 41) . However, patient perceptions of impaired daily functioning and experience of other psychosocial changes after TBI may exacerbate depressive symptoms (42) .
Treatment of Depression Following TBI
It is appropriate to use the standard diagnostic criteria for depression when evaluating persons with TBI (43 – 45) . Although many factors may produce or contribute to apparent depressive symptoms, such as sleep disturbance, fatigue (anergia), difficulty with concentration, and anhedonia (apathy), when there are sufficient symptoms to merit a diagnosis of depression—regardless of their possible causes—treatment should be initiated. Treatment should be promptly initiated both to improve mood and to mitigate its adverse effects on cognitive, behavioral, physical, and psychosocial functioning (36 , 38 , 40 , 41 , 46) .
Pharmacotherapy
Pharmacotherapy may not only alleviate the mood disturbance but also reduce other postconcussive symptoms and the patient’s experience of the severity of such symptoms (36) . When pharmacotherapy is initiated, a “start low and go slow” approach is recommended. Common clinical experience, as well as a limited body of literature (19 , 27 , 31) , suggests that persons with TBI may be more susceptible to the side effects of many psychotropic medications, suggesting a heightened need for vigilance for such effects when prescribing psychotropic agents in this context. Additionally, no medications have been approved by the U.S. Food and Drug Administration specifically for the treatment of post-TBI depression, or for any other posttraumatic neuropsychiatric problem. The use of these agents is therefore “off-label” and will in each case be a matter of empiric trial. Nonetheless, the literature describing the treatment of posttraumatic depression is a useful guide to treatment selection.
As reviewed by Warden et al. (47) , several studies, mostly small and open-label, suggest that the selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants may improve depression following TBI. Given concerns about the tolerability of tricyclic antidepressants, particularly their potentially adverse anticholinergically mediated effects on cognition (19) , the SSRIs are generally regarded as the first-line agents for treatment of depression following TBI (47) .
Among the SSRIs, the available evidence favors sertraline (25–150 mg/day) (36 , 48) or citalopram (>20 mg/day) (46) . Ashman et al. (49) , in a 10-week, double-blind, placebo-controlled study of 52 patients with remote, predominantly moderate to severe TBI, observed significant improvements in depressive symptoms in those treated with 25–200 mg of sertraline daily (mean dose not specified) or placebo. With treatment response defined as a change of 50% or more in Hamilton Depression Rating Scale score, 59% of patients receiving sertraline responded, while only 32% of those treated with placebo responded. Although the magnitude of improvement and the number of treatment responders were similar to those observed in pharmacotherapy studies performed in patients with idiopathic major depressive disorder, the response rate did not differ significantly between the number of sertraline and placebo responders. This observation most likely reflects a sample size inadequate to detect a significant difference in responder rates. The mean dose of sertraline received by these patients was not reported in the study, leaving uncertain the adequacy of antidepressant dosing.
Other SSRIs may be used to treat depression after mild TBI, although the literature provides little guidance regarding their efficacy and tolerability in this population. In everyday practice, the effectiveness and tolerability of fluoxetine does not appear to differ from that of the other SSRIs. However, its robust inhibition of cytochrome P450 (CYP450) 2D6, 2C19, and 3A, its metabolism to norfluoxetine (also an inhibitor of the P450 isoenzymes), and the prolonged half-life of this active metabolite are concerning: the risk of drug-drug interactions or metabolism-related adverse events may be higher with this SSRI than with sertraline or citalopram. Paroxetine, also a potent inhibitor of CYP450, may impair cognitive function even in healthy adults, most likely as a result of its antimuscarinic effects (50) . Paroxetine therefore is best used with caution, if at all, in persons with posttraumatic depression and cognitive complaints.
The efficacy and tolerability of other antidepressants (including “dual action” antidepressants and bupropion) in this population has not been established, but common clinical experience suggests that the benefits and adverse effects of most of the newer-generation antidepressants are similar to those of the SSRIs. The propensity of bupropion to reduce seizure threshold is a concern in the first-line use of this agent, although the risk of early and late seizures after mild TBI is relatively low (51) , and the risk of seizures with bupropion appears to be restricted to the immediate-release formulation (52) . If bupropion is used in patients with mild TBI, preference should be given to its sustained-release formulation, and vigilance for treatment-related seizures should be maintained.
In addition to effects on depressive symptoms, SSRIs may improve comorbid posttraumatic somatic, behavioral, and cognitive problems. Fann et al. (36) demonstrated sertraline-related improvements in postconcussive symptoms, including headache, fatigue, and sleep disturbance, as well as reduction in the perceived severity of injury and improvement in psychosocial functioning. Fann et al. (41) also reported that sertraline-related improvement in post-TBI depression was accompanied by improvements in psychomotor speed, recent verbal memory, recent visual memory, and general cognitive efficiency, as well as patients’ perception of the severity of their cognitive problems. Horsfield et al. (53) observed similar benefits in a small series of patients with TBI treated with fluoxetine.
The benefits of antidepressants for posttraumatic cognitive impairments have not been observed in all studies. Lee et al. (54) , comparing the effects of sertraline and methylphenidate on depression after mild to moderate TBI, reported reductions of depressive symptoms with both agents, but more substantial improvements in cognition and daytime fatigue with methylphenidate. Similar benefits of methylphenidate monotherapy for depression after TBI have been reported by other authors (55) . These observations suggest that some patients with significant depression, fatigue, and cognitive impairments after TBI may experience improvements in all of these domains in response to a single agent, methylphenidate. In practice, however, the use of methylphenidate in the treatment of depression is generally limited to augmentation of a standard antidepressant and targets residual depressive, anergic, or cognitive impairments.
Psychotherapy
Psychological and social factors contribute to the development and persistence of posttraumatic depression. Education regarding TBI and recovery expectations, reassurance, and frequent support are associated with better outcomes during the first year after the injury was sustained (29 , 30) , and multidisciplinary treatment may be particularly useful for individuals with mild TBI and prior psychiatric problems (56) . Cognitive-behavioral therapy (CBT) may be useful for a variety of posttraumatic neuropsychiatric problems. CBT has been observed to decrease depression, anxiety, and anger and to improve problem-solving skills, self-esteem, and psychosocial functioning after TBI, although the benefits of such psychological improvements on depression are observed inconsistently (57 – 59) .
Spouses, families, and caregivers of persons with TBI frequently require psychotherapeutic intervention to aid them in maintaining both their own psychological health and that of their injured family member. Depression occurs more frequently in caregivers of persons with TBI (60) , and posttraumatic depression is strongly associated with significant family dysfunction (61) . Use of problem-solving and behavioral coping strategies by the patients’ families can decrease the severity of depression (62) . Thus, engaging spouses, family members, and other care providers in the treatment of posttraumatic depression is essential. Peer support programs for persons with TBI and their families increase their knowledge about TBI, improve general outlook, enhance their ability to cope with depression, and improve quality of life after TBI (63) .
Treatment of Cognitive Impairment
After treating depression, treatment of residual cognitive problems is appropriate. Cognitive rehabilitation, usually provided by an occupational therapist, speech therapist, or neuropsychologist, is most useful for the development of compensatory strategies to address difficulties with memory, attention, interpersonal communication skills, and executive function (64 , 65) . Cognitive rehabilitation appears best suited to patients who have mild to moderate cognitive impairments, who have relatively well preserved functional independence, and who are motivated to engage in and rehearse these strategies. Pharmacotherapy may be a useful adjunct to cognitive rehabilitation.
The neuroanatomy and neurochemistry of TBI yield two general approaches to the pharmacotherapy of posttraumatic cognitive impairments: catecholaminergic augmentation and cholinergic augmentation (19) . Methylphenidate augments cerebral catecholaminergic function and is the first-line treatment for impaired speed of processing; it may also improve arousal and, to a lesser extent, attention and memory (47) . Pharmacologically similar agents, such as dextroamphetamine, may afford comparable benefits, although there are few studies offering evidence to support their use in this population.
Methylphenidate generally takes effect quickly (within 0.5–1 hour) and loses effect after a few hours. Therefore, the first issue in the administration of this agent is to determine its optimal dose and dosing frequency. Treatment generally begins at 5 mg methylphenidate once daily and is gradually increased, in 5-mg increments, until adequate benefits are achieved or medication intolerance occurs. Methylphenidate may induce mild increases in heart rate and blood pressure, although such changes are relatively infrequent and rarely require treatment discontinuation. Nonetheless, baseline pulse and blood pressure should be obtained and monitored until a final dosage is achieved. In patients with a history of stimulant abuse, the risks of abuse of methylphenidate should be considered carefully before undertaking treatment with this agent. While doses are often in the range of 10–20 mg twice daily (i.e., 0.15–0.30 mg/kg twice daily), some patients may require higher doses (e.g., 40 mg) and greater frequency (3–4 times a day). Individuals requiring relatively high and frequent doses of methylphenidate may benefit from use of longer-acting preparations. In such cases, it also may be useful to obtain blood levels of methylphenidate 90 minutes after ingestion to evaluate patient-specific pharmacokinetics and to use that information to guide considerations regarding the prescription of higher doses.
Placebo-controlled studies suggest that donepezil (66 , 67) and rivastigmine (68 , 69) may be useful in the treatment of posttraumatic cognitive impairments, and particularly memory impairments. Cholinesterase inhibitor-related improvements in attention and executive functioning have also been reported (see reference 19 for a review), and these agents are sometimes used for this purpose in clinical practice. Consistent with this suggestion, the Neurobehavioral Guidelines Working Group (47) recommended donepezil (5–10 mg daily) to enhance aspects of attention and memory for patients with moderate to severe TBI in subacute and chronic periods of recovery. Based on findings published after the Neurobehavioral Guidelines Working Group report was issued, rivastigmine (3–6 mg daily) is also suggested as an option in the treatment of chronic posttraumatic memory and perhaps attention impairments (68) . In our experience and that of others (70) , these agents—alone or in combination with those that augment catecholaminergic function—are also useful in the treatment of posttraumatic cognitive impairments in persons with mild TBI.
Treating Other Comorbid Neuropsychiatric Symptoms
Many symptoms that affect individuals with TBI may persist despite the treatments described above. As illustrated in Figure 1 , the development and persistence of these symptoms may reflect preinjury problems, the effects of injury, postinjury psychological or social problems, or some combination of these factors. The treatment of these and other posttraumatic neuropsychiatric symptoms is beyond the scope of this article, but information may be found elsewhere (see reference 71 for a review).
1. American Congress of Rehabilitation Medicine: Definition of mild traumatic brain injury. J Head Trauma Rehabil 1993; 8(3):86–87Google Scholar
2. Marr AL, Coronado VG: Central Nervous System Injury Surveillance Data Submission Standards: 2002. Atlanta, Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, 2002Google Scholar
3. Teasdale G, Jennett B: Assessment of coma and impaired consciousness: a practical scale. Lancet 1974; 2:81–84Google Scholar
4. Thurman D, Guerrero J: Trends in hospitalization associated with traumatic brain injury. JAMA 1999; 282:954–957Google Scholar
5. Thurman DJ, Alverson C, Dunn KA, Guerrero J, Sniezek JE: Traumatic brain injury in the United States: a public health perspective. J Head Trauma Rehabil 1999; 14:602–615Google Scholar
6. Warden D: Military TBI during the Iraq and Afghanistan wars. J Head Trauma Rehabil 2006; 21:398–402Google Scholar
7. Tanielian T, Jaycox LH: Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, Calif, RAND Corporation, 2008Google Scholar
8. Gordon WA, Brown M, Sliwinski M, Hibbard MR, Patti N, Weiss MJ, Kalinsky R, Sheerer M: The enigma of “hidden” traumatic brain injury. J Head Trauma Rehabil 1998; 13(6):39–56Google Scholar
9. Hibbard MR, Uysal S, Sliwinski M, Gordon WA: Undiagnosed health issues in individuals with traumatic brain injury living in the community. J Head Trauma Rehabil 1998; 13(4):47–57Google Scholar
10. Zaloshnja E, Miller T, Langlois JA, Selassie AW: Prevalence of long-term disability from traumatic brain injury in the civilian population of the United States, 2005. J Head Trauma Rehabil 2008; 23:394–400Google Scholar
11. Dikmen S, Machamer J, Temkin N: Mild head injury: facts and artifacts. J Clin Exp Neuropsychol 2001; 23:729–738Google Scholar
12. Hessen E, Nestvold K, Anderson V: Neuropsychological function 23 years after mild traumatic brain injury: a comparison of outcome after paediatric and adult head injuries. Brain Inj 2007; 21:963–979Google Scholar
13. Vanderploeg RD, Curtiss G, Luis CA, Salazar AM: Long-term morbidities following self-reported mild traumatic brain injury. J Clin Exp Neuropsychol 2007; 29:585–598Google Scholar
14. Povlishock JT, Katz DI: Update of neuropathology and neurological recovery after traumatic brain injury. J Head Trauma Rehabil 2005; 20:76–94Google Scholar
15. Bigler ED: Anterior and middle cranial fossa in traumatic brain injury: relevant neuroanatomy and neuropathology in the study of neuropsychological outcome. Neuropsychology 2007; 21:515–531Google Scholar
16. Meythaler JM, Peduzzi JD, Eleftheriou E, Novack TA: Current concepts: diffuse axonal injury-associated traumatic brain injury. Arch Phys Med Rehabil 2001; 82:1461–1471Google Scholar
17. DePalma RG, Burris DG, Champion HR, Hodgson MJ: Blast injuries. N Engl J Med 2005; 352:1335–1342Google Scholar
18. Ritenour AE, Baskin TW: Primary blast injury: update on diagnosis and treatment. Crit Care Med 2008; 36(suppl 7):S311–S317Google Scholar
19. Arciniegas DB, Silver JM: Pharmacotherapy of posttraumatic cognitive impairments. Behav Neurol 2006; 17:25–42Google Scholar
20. McAllister TW, Flashman LA, McDonald BC, Saykin AJ: Mechanisms of working memory dysfunction after mild and moderate TBI: evidence from functional MRI and neurogenetics. J Neurotrauma 2006; 23:1450–1467Google Scholar
21. Powell JM, Ferraro JV, Dikmen SS, Temkin NR, Bell KR: Accuracy of mild traumatic brain injury diagnosis. Arch Phys Med Rehabil 2008; 89:1550–1555Google Scholar
22. Kraus MF, Susmaras T, Caughlin BP, Walker CJ, Sweeney JA, Little DM: White matter integrity and cognition in chronic traumatic brain injury: a diffusion tensor imaging study. Brain 2007; 130:2508–2519Google Scholar
23. Niogi SN, Mukherjee P, Ghajar J, Johnson C, Kolster RA, Sarkar R, Lee H, Meeker M, Zimmerman RD, Manley GT, McCandliss BD: Extent of microstructural white matter injury in postconcussive syndrome correlates with impaired cognitive reaction time: a 3T diffusion tensor imaging study of mild traumatic brain injury. AJNR Am J Neuroradiol 2008; 29:967–973Google Scholar
24. Guilmette TJ, Paglia MF: The public’s misconception about traumatic brain injury: a follow up survey. Arch Clin Neuropsychol 2004; 19:183–189Google Scholar
25. Swift TL, Wilson SL: Misconceptions about brain injury among the general public and non-expert health professionals: an exploratory study. Brain Inj 2001; 15:149–165Google Scholar
26. Kim E, Lauterbach EC, Reeve A, Arciniegas DB, Coburn KL, Mendez MF, Rummans TA, Coffey EC; ANPA Committee on Research: Neuropsychiatric complications of traumatic brain injury: a critical review of the literature (a report by the ANPA Committee on Research). J Neuropsychiatry Clin Neurosci 2007; 19:106–127Google Scholar
27. Arciniegas DB, Anderson CA, Topkoff J, McAllister TW: Mild traumatic brain injury: a neuropsychiatric approach to diagnosis, evaluation, and treatment. Neuropsychiatr Dis Treat 2005; 1:311–327Google Scholar
28. McAllister TW, Arciniegas D: Evaluation and treatment of postconcussive symptoms. Neurorehabilitation 2002; 17:265–283Google Scholar
29. Snell DL, Surgenor LJ, Hay-Smith EJ, Siegert RJ: A systematic review of psychological treatments for mild traumatic brain injury: an update on the evidence. J Clin Exp Neuropsychol 2008; 2;1–19Google Scholar
30. Bell KR, Hoffman JM, Temkin NR, Powell JM, Fraser RT, Esselman PC, Barber JK, Dikmen S: The effect of telephone counselling on reducing post-traumatic symptoms after mild traumatic brain injury: a randomised trial. J Neurol Neurosurg Psychiatry 2008; 79:1275–1281Google Scholar
31. Alderfer BS, Arciniegas DB, Silver JM: Treatment of depression following traumatic brain injury. J Head Trauma Rehabil 2005; 20:544–562Google Scholar
32. Bay E, Kirsch N, Gillespie B: Chronic stress conditions do explain posttraumatic brain injury depression. Res Theory Nurs Pract 2004; 18:213–228Google Scholar
33. Jorge RE, Robinson RG, Moser D, Tateno A, Crespo-Facorro B, Arndt S: Major depression following traumatic brain injury. Arch Gen Psychiatry 2004; 61:42–50Google Scholar
34. Jorge RE, Robinson RG, Arndt SV, Starkstein SE, Forrester AW, Geisler F: Depression following traumatic brain injury: a 1 year longitudinal study. J Affect Disord 1993; 27:233–243Google Scholar
35. Jorge RE, Robinson RG, Arndt SV, Forrester AW, Geisler F, Starkstein SE: Comparison between acute- and delayed-onset depression following traumatic brain injury. J Neuropsychiatry Clin Neurosci 1993; 5:43–49Google Scholar
36. Fann JR, Uomoto JM, Katon WJ: Sertraline in the treatment of major depression following mild traumatic brain injury. J Neuropsychiatry Clin Neurosci 2000; 12:226–232Google Scholar
37. Fann JR, Katon WJ, Uomoto JM, Esselman PC: Psychiatric disorders and functional disability in outpatients with traumatic brain injuries. Am J Psychiatry 1995; 152:1493–1499Google Scholar
38. Rapoport MJ, McCullagh S, Streiner D, Feinstein A: The clinical significance of major depression following mild traumatic brain injury. Psychosomatics 2003; 44:31–37Google Scholar
39. Hibbard MR, Uysal S, Kepler K, Bogdany J, Silver J: Axis I psychopathology in individuals with traumatic brain injury. J Head Trauma Rehabil 1998; 13(4):24–39Google Scholar
40. Rapoport MJ, McCullagh S, Shammi P, Feinstein A: Cognitive impairment associated with major depression following mild and moderate traumatic brain injury. J Neuropsychiatry Clin Neurosci 2005; 17:61–65Google Scholar
41. Fann JR, Uomoto JM, Katon WJ: Cognitive improvement with treatment of depression following mild traumatic brain injury. Psychosomatics 2001; 42:48–54Google Scholar
42. Pagulayan KF, Hoffman JM, Temkin NR, Machamer JE, Dikmen SS: Functional limitations and depression after traumatic brain injury: examination of the temporal relationship. Arch Phys Med Rehabil 2008; 89:1887–1892Google Scholar
43. Starkstein SE, Lischinsky A: The phenomenology of depression after brain injury. Neurorehabilitation 2002; 17:105–113Google Scholar
44. Green A, Felmingham K, Baguley IJ, Slewa-Younan S, Simpson S: The clinical utility of the Beck Depression Inventory after traumatic brain injury. Brain Inj 2001; 15:1021–1028Google Scholar
45. Kreutzer JS, Seel RT, Gourley E: The prevalence and symptom rates of depression after traumatic brain injury: a comprehensive examination. Brain Inj 2001; 15:563–576Google Scholar
46. Rapoport MJ, Chan F, Lanctot K, Herrmann N, McCullagh S, Feinstein A: An open-label study of citalopram for major depression following traumatic brain injury. J Psychopharmacol 2008; 22:860–864Google Scholar
47. Neurobehavioral Guidelines Working Group, Warden DL, Gordon B, McAllister TW, Silver JM, Barth JT, Bruns J, Drake A, Gentry T, Jagoda A, Katz DI, Kraus J, Labbate LA, Ryan LM, Sparling MB, Walters B, Whyte J, Zapata A, Zitnay G: Guidelines for the pharmacologic treatment of neurobehavioral sequelae of traumatic brain injury. J Neurotrauma 2006; 23:1468–1501Google Scholar
48. Turner-Stokes L, Hassan N, Pierce K, Clegg F: Managing depression in brain injury rehabilitation: the use of an integrated care pathway and preliminary report of response to sertraline. Clin Rehabil 2002; 16:261–268Google Scholar
49. Ashman TA, Cantor JB, Gordon WA, Spielman L, Flanagan S, Ginsberg A, Engmann C, Egan M, Ambrose F, Greenwald B: A randomized controlled trial of sertraline for the treatment of depression in individuals with traumatic brain injury. Arch Phys Med Rehabil (in press)Google Scholar
50. Schmitt JA, Kruizinga MJ, Riedel WJ: Non-serotonergic pharmacological profiles and associated cognitive effects of serotonin reuptake inhibitors. J Psychopharmacol 2001; 15:173–179Google Scholar
51. Frey LC: Epidemiology of posttraumatic epilepsy: a critical review. Epilepsia 2003; 44(suppl 10):11–17Google Scholar
52. Alper K, Schwartz KA, Kolts RL, Khan A: Seizure incidence in psychopharmacological clinical trials: an analysis of Food and Drug Administration (FDA) summary basis of approval reports. Biol Psychiatry 2007; 62:345–354Google Scholar
53. Horsfield SA, Rosse RB, Tomasino V, Schwartz BL, Mastropaolo J, Deutsch SI: Fluoxetine’s effects on cognitive performance in patients with traumatic brain injury. Int J Psychiatry Med 2002; 32:337–344Google Scholar
54. Lee H, Kim SW, Kim JM, Shin IS, Yang SJ, Yoon JS: Comparing effects of methylphenidate, sertraline, and placebo on neuropsychiatric sequelae in patients with traumatic brain injury. Hum Psychopharmacol 2005; 20:97–104Google Scholar
55. Gualtieri CT, Evans RW: Stimulant treatment for the neurobehavioural sequelae of traumatic brain injury. Brain Inj 1988; 2:273–290Google Scholar
56. Ghaffar O, McCullagh S, Ouchterlony D, Feinstein: A randomized treatment trial in mild traumatic brain injury. J Psychosom Res 2006; 61:153–160Google Scholar
57. Anson K, Ponsford J: Evaluation of a coping skills group following traumatic brain injury. Brain Inj 2006; 20:167–178Google Scholar
58. Anson K, Ponsford J: Who benefits? outcome following a coping skills group intervention for traumatically brain injured individuals. Brain Inj 2006; 20:1–13Google Scholar
59. Anson K, Ponsford J: Coping and emotional adjustment following traumatic brain injury. J Head Trauma Rehabil 2006; 21:248–259Google Scholar
60. Harris JK, Godfrey HP, Partridge FM, Knight RG: Caregiver depression following traumatic brain injury (TBI): a consequence of adverse effects on family members? Brain Inj 2001; 15:223–238Google Scholar
61. Groom KN, Shaw TG, O’Connor ME, Howard NI, Pickens A: Neurobehavioral symptoms and family functioning in traumatically brain-injured adults. Arch Clin Neuropsychol 1998; 13:695–711Google Scholar
62. Leach LR, Frank RG, Bouman DE, Farmer J: Family functioning, social support, and depression after traumatic brain injury. Brain Inj 1994; 8:599–606Google Scholar
63. Hibbard MR, Cantor J, Charatz H, Rosenthal R, Ashman T, Gundersen N, Ireland-Knight L, Gordon W, Avner J, Gartner A: Peer support in the community: initial findings of a mentoring program for individuals with traumatic brain injury and their families. J Head Trauma Rehabil 2002; 17:112–131Google Scholar
64. Cicerone KD, Dahlberg C, Kalmar K, Langenbahn DM, Malec JF, Bergquist TF, Felicetti T, Giacino JT, Harley JP, Harrington DE, Herzog J, Kneipp S, Laatsch L, Morse PA: Evidence-based cognitive rehabilitation: recommendations for clinical practice. Arch Phys Med Rehabil 2000; 81:1596–1615Google Scholar
65. Cicerone KD, Dahlberg C, Malec JF, Langenbahn DM, Felicetti T, Kneipp S, Ellmo W, Kalmar K, Giacino JT, Harley JP, Laatsch L, Morse PA, Catanese J: Evidence-based cognitive rehabilitation: updated review of the literature from 1998 through 2002. Arch Phys Med Rehabil 2005; 86:1681–1692Google Scholar
66. Zhang L, Plotkin RC, Wang G, Sandel ME, Lee S: Cholinergic augmentation with donepezil enhances recovery in short-term memory and sustained attention after traumatic brain injury. Arch Phys Med Rehabil 2004; 85:1050–1055Google Scholar
67. Kim YW, Kim DY, Shin JC, Park CI, Lee JD: The changes of cortical metabolism associated with the clinical response to donepezil therapy in traumatic brain injury. Clin Neuropharmacol (Epub ahead of print, Oct 23, 2008)Google Scholar
68. Silver JM, Koumaras B, Chen M, Mirski D, Potkin SG, Reyes P, Warden D, Harvey PD, Arciniegas D, Katz DI, Gunay I: Effects of rivastigmine on cognitive function in patients with traumatic brain injury. Neurology 2006; 67:748–755Google Scholar
69. Silver JM, Koumaras B, Meng X, Potkin SG, Reyes Patricio, Harvey PD, Katz D, Gunay I, Arciniegas DB: Long-term effects of rivastigmine capsules in patients with traumatic brain injury. Brain Injury 2009; 23:123–132Google Scholar
70. Tenovuo O: Central acetylcholinesterase inhibitors in the treatment of chronic traumatic brain injury: clinical experience in 111 patients. Prog Neuropsychopharmacol Biol Psychiatry 2005; 29:61–67Google Scholar
71. Silver JM, McAllister TW, Yudofsky SC: Textbook of Traumatic Brain Injury. Washington, DC, American Psychiatric Publishing, Inc, 2005Google Scholar
72. Greenwald RM, Gwin JT, Chu JJ, Crisco JJ: Head impact severity measures for evaluating mild traumatic brain injury risk exposure. Neurosurgery 2008; 62:789–798Google Scholar
73. McAllister TW, Flashman LA, Harker Rhodes C, Tyler AL, Moore JH, Saykin AJ, McDonald BC, Tosteson TD, Tsongalis GJ: Single nucleotide polymorphisms in ANKK1 and the dopamine D2 receptor gene affect cognitive outcome shortly after traumatic brain injury: a replication and extension study. Brain Inj 2008; 22:705–714Google Scholar




