Symptom Dimensions of Depression Following Myocardial Infarction and Their Relationship With Somatic Health Status and Cardiovascular Prognosis
Abstract
OBJECTIVE: The reporting of depressive symptoms following myocardial infarction may be confounded by complaints originating from the myocardial infarction. Therefore, it is difficult to estimate the effects of post-myocardial infarction depression and its treatment on cardiovascular prognosis. The authors’ goal was to study the relationship between depressive symptom dimensions following myocardial infarction and both somatic health status and prospective cardiovascular prognosis. METHOD: In two studies of myocardial infarction patients (N=494 and 1,972), the Beck Depression Inventory was used to determine the dimensional structure of depressive symptoms following myocardial infarction. Three symptom dimensions—somatic/affective, cognitive/affective, and appetitive—were compared with baseline left ventricular ejection fraction, Charlson comorbidity index, Killip class, and previous myocardial infarction. The relationship between depressive symptom dimensions and prospective cardiovascular mortality and cardiac-related readmissions was also examined (mean follow-up duration=2.5 years). RESULTS: Somatic/affective symptoms were associated with poor health status (left ventricular ejection fraction, Charlson comorbidity index, Killip class, and previous myocardial infarction) and predicted cardiovascular mortality and cardiac events. Cognitive/affective symptoms were only marginally associated with somatic health status and not with cardiovascular death and cardiac events. Appetitive symptoms were related to somatic health status but did not predict cardiovascular death or cardiac events. CONCLUSIONS: Somatic/affective depressive symptoms following myocardial infarction were confounded by somatic health status yet were prospectively associated with cardiac prognosis even after somatic health status was controlled. Cognitive/affective depressive symptoms were only marginally related to health status and not to cardiac prognosis. These findings suggest that treatment of depression following myocardial infarction might improve cardiovascular prognosis when it reduces somatic/affective symptoms.
Depression following myocardial infarction has been extensively studied since Frasure-Smith and colleagues reported its prospective association with cardiac prognosis (1–4). However, whether the reporting of depressive symptoms following myocardial infarction reflects actual depression or rather somatic complaints originating from the myocardial infarction itself (such as fatigue, sleeping problems, or appetitive symptoms) has been the subject of debate (5, 6). Recently, the debate has been reopened in the context of depression following myocardial infarction being a risk factor for post-myocardial infarction mortality (7–10). If post-myocardial infarction depressive complaints originate even partially from the myocardial infarction, the relationship between post-myocardial infarction depression and cardiovascular prognosis would be confounded, and depression would not be an independent risk factor for post-myocardial infarction prognosis.
A recent meta-analysis of 22 studies (11) suggested that the effects of depression following myocardial infarction on cardiac prognosis were at least partly confounded by the severity of the infarction. Overall, post-myocardial infarction depression was associated with a 2–2.5 times increased risk of all-cause mortality, cardiac mortality, and new cardiovascular events. However, of the studies that reported a significant effect and controlled for the severity of the myocardial infarction or the patient’s somatic health status (1–3, 12–19), four studies (2, 3, 12, 17) found a completely independent relationship (no reduction of the effect size), whereas in four others (1, 13, 18, 19) the effect was reduced. In the remaining studies (14–16), the effect of depression was no longer statistically significant.
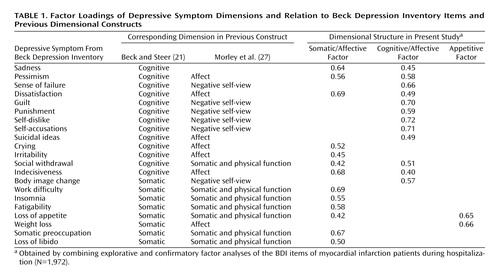
To date, it is unclear which aspects of depression are associated with somatic health status and myocardial infarction prognosis. The Beck Depression Inventory (BDI) is the most frequently used instrument to assess depressive symptoms, and its factor structure has been studied in many different populations since its first publication in 1961 (20). When the instrument has been used in medical patients, Beck and Steer’s distinction between somatic and cognitive symptoms (21) has regularly been referred to by researchers (22–28). In chronic pain patients, Morley et al. (27) distinguished three factors: somatic and physical function, negative view of the self, and a less coherent affective factor. Similarly, in male cardiac outpatients, a factor structure of the BDI distinguishing negative self-attitudes, physiological symptoms, and sadness has been reported by Campbell et al. (28). In order to clarify the relationship between post-myocardial infarction depression and cardiovascular prognosis, we explored the structure of depressive symptoms following myocardial infarction in relation to baseline somatic health status and prospective cardiovascular prognosis. We hypothesized that 1) confounding of depressive symptoms by myocardial infarction severity would occur with somatic symptoms and less so with cognitive symptoms, and 2) both cognitive and somatic symptoms of depression would be prospectively associated with cardiovascular prognosis even after myocardial infarction severity was controlled.
Method
We employed data from two studies conducted in the Netherlands with highly similar inclusion criteria and assessments: the Myocardial INfarction and Depression-Intervention Trial (MIND-IT) and the Depression After Myocardial Infarction study. Cross-sectional data from the MIND-IT were supplemented with data regarding prospective cardiovascular prognosis derived from the Depression After Myocardial Infarction study.
Design and Patients
The MIND-IT was a large, multicenter, randomized controlled trial that investigated the prognostic influence of antidepressive treatment for a depressive disorder following myocardial infarction compared with care as usual (29). Eligible patients were 18 years of age or older, had had an acute myocardial infarction between September 1999 and March 2003, and had been admitted to one of 10 participating hospitals. Myocardial infarction was defined as the presence of increased cardiac enzymes and either electrocardiographic changes or chest pain. Exclusion criteria were the occurrence of myocardial infarction while the patient was hospitalized for another reason (except for unstable angina pectoris), lacking capability to participate in study procedures (e.g., unable to communicate or not available for follow-up), any noncardiovascular disease likely to influence short-term survival, receiving psychiatric treatment for depression, or participation in any clinical trial that might intervene with the study objectives or safety of the patient. Consenting eligible patients were screened with the BDI for the presence of depressive symptoms during hospitalization and at 3-month follow-up. Myocardial infarction patients with significant depressive symptoms (BDI score ≥10) underwent an additional psychiatric evaluation. Patients experiencing a depressive episode following myocardial infarction according to the interview were randomly assigned to an intervention condition (i.e., antidepressive treatment) after 3 months. A total of 4,780 patients were assessed for eligibility, of whom 2,603 were excluded (1,403 did not meet inclusion criteria and 1,200 did not provide informed consent), leaving 2,177 for the study. Complete BDI assessments during hospitalization were available for 1,972 (90.6%) of these patients.
The Depression After Myocardial Infarction study was a naturalistic follow-up study of the impact of depression on cardiac prognosis in myocardial infarction patients in four hospitals in the northern region of the Netherlands. Inclusion and exclusion criteria were the same as in the MIND-IT. During the period from September 1997 to September 2000, depressive symptoms were assessed during hospitalization. The follow-up period was variable and for all patients lasted until the end of the study in April 2002. All patients received usual aftercare for their myocardial infarction. A total of 1,166 patients were screened, and inclusion criteria were met by 882 patients. Of these, 528 patients provided informed consent, with complete baseline and follow-up assessments available for 494 (93.6%).
Assessments
Depression
We used the BDI questionnaire to screen for depressive symptoms during hospitalization. Respondents were instructed to rate each symptom on a 0 to 3 scale, with 0 representing “absence” and 1–3 representing increasing levels of severity of the symptom. The BDI yields a total score ranging from 0 to 63, with higher scores indicating greater levels of depressive symptoms. Depressive disorder was assessed with version 2.1 of the Composite International Diagnostic Interview (CIDI), a standardized psychiatric diagnostic interview, during the first year after myocardial infarction. The CIDI is a fully structured interview that examines whether the ICD-10 diagnostic criteria for depression are met. For depression, the interrater reliability has been demonstrated to be excellent and the test-retest reliability and validity good. The CIDI is available in many languages. We used the Dutch version of the CIDI that is supported by the Dutch CIDI center, which offered a training program for our interviewers. The CIDI data is inputted via standard data entry, and the computer algorithm provides the diagnostic criteria that are met. The interviews were conducted at the patient’s home, and to determine clinical depression we used all ICD-10 unipolar depression disorders.
Somatic health status
Severity of infarction was represented by the left ventricular ejection fraction after myocardial infarction, measured either by echocardiography or nuclear radiography (MIND-IT categories: <30%, 30%–44%, 45%–60%, and >60%; Depression After Myocardial Infarction study categories: >40% and <40%). At admission, Killip class was used to indicate the presence of heart failure (measured on a 4-point scale in MIND-IT and categorized as 0–1 versus ≥2 in the Depression After Myocardial Infarction study). The presence of a previous myocardial infarction (before the index myocardial infarction) was extracted from the medical file. The cumulative burden of medical comorbidity was assessed in the MIND-IT with the Charlson comorbidity index, following the recent adaptation for myocardial infarction patients (26) and was categorized as 0, 1–2, 3–4, or ≥5, with higher scores indicating more comorbid diseases.
Cardiovascular prognosis
In the Depression After Myocardial Infarction study, study endpoints were cardiovascular mortality and cardiac-related readmissions after discharge from the hospital. Potential endpoints were identified in regular post-myocardial infarction control visits (1, 3, and 12 months after myocardial infarction) and patient interviews at 3 and 12 months after myocardial infarction (face-to-face interviews) and thereafter every 6 months until end of follow-up (telephone interviews). Information on potential endpoints was recorded from hospital records, the treating physician, and the patient’s primary care physician. Two cardiologists, blind to the depression status of the patient, independently evaluated the nature (cardiovascular or not) and onset of endpoints, and decisions were made by unanimity. The average follow-up period for the 494 patients was 2.5 years (SD=0.9). A cardiovascular event (fatal or nonfatal) was experienced by 112 patients (22.7%): unstable angina pectoris (12.3%, N=61), recurrent myocardial infarction (3.8%, N=19), sustained arrhythmia (2.4%, N=12), heart failure (2.2%, N=11), and other cardiovascular events needing hospitalization such as cerebrovascular accident or peripheral arterial disease (1.8%, N=9). Twenty-one patients (4.3%) had a fatal cardiovascular event: angina pectoris during a coronary artery bypass grafting procedure (N=1), recurrent myocardial infarction (N=6), sustained arrhythmia (N=4), heart failure (N=5), and other cardiovascular events such as cerebrovascular accident and sudden cardiac death outside the hospital (N=5).
Exploration and Validation of Factor Structure
The dimensional structure of depressive symptoms following myocardial infarction was obtained by combining explorative and confirmatory factor analyses of the BDI items of myocardial infarction patients during hospitalization (MIND-IT: N=1,972; the Depression After Myocardial Infarction study: N=494) and at a 3-month follow-up evaluation (MIND-IT: N=1,941). Based on the scree plot and the criterion of Eigenvalue >1, we determined the optimal number of factors to be three, which together explained 42.3% of variance. The three factors, the loadings for which are presented in Table 1, were interpreted as 1) somatic/affective (a combination of the somatic items from the BDI manual, the affective items in the Morley model [27], and the items crying and irritability), 2) cognitive/affective (a combination of the cognitive items from the BDI manual and the items reflecting “negative view of the self” or “negative affect” in the Morley model), and 3) appetitive. When comparing our factors to the ones reported by Campbell et al. (28), our somatic/affective factor is a combination of their factors “physiological symptoms” and “sadness,” and our cognitive/affective factor is a combination of their factor “negative self-attitudes” and “sadness.”
Our three-factor model was cross-validated in a multisample structural equation model (30–33), supporting its generalizability across time of assessment (depressive symptoms during hospital stay versus 3-month follow-up evaluation) and study group (MIND-IT versus the Depression After Myocardial Infarction study). The internal consistency coefficients (Cronbach’s alpha) for the first two factors were satisfactory, 0.81 and 0.82 respectively (not calculated for the third factor because of the too small number of items). Factor scores were calculated on the basis of unstandardized item factor loadings and z-transformed (mean subtracted and divided by standard deviation) for purpose of interpretation.
Multivariate logistic regression analysis of the MIND-IT data assessed whether the z-transformed factor scores were related to the presence of an ICD-10 depressive disorder during the first 3 months after myocardial infarction. Patients scoring below 10 on the BDI were considered as noncases, which is justified by the very high negative predictive value of BDI’s cutoff value of 10 being 97.9% (34); therefore, we misclassified only 2.1% of the ICD-10 depression cases. Analysis of variance in the MIND-IT data tested whether baseline left ventricular ejection fraction, Charlson comorbidity index, Killip class, or previous myocardial infarctions were associated with the factor scores. In the Depression After Myocardial Infarction study dataset, the factor scores were used to predict time-related occurrence of death and events in univariate and multivariate Cox regression analyses, with left ventricular ejection fraction (<40%), Killip class (≥2), and previous myocardial infarction controlled and simultaneous inclusion of the three factor scores, which resulted in adjusted hazard rates with 95% confidence intervals (CIs). In all analyses, p values of <0.05 were considered to indicate statistically significant differences.
Results
Correlation of Factors With Clinical Depression and Baseline Somatic Health Status
The logistic regression model predicting the presence of clinical depression according to ICD-10 criteria at the 1-year follow-up evaluation (N=216 of 1,972) resulted in significant odds ratios for the somatic/affective (odds ratio=3.07, 95% CI=2.43–3.81) and cognitive/affective (odds ratio=1.85, 95% CI=1.54–2.22) dimensions but not for appetitive (odds ratio=0.99; 95% CI=0.85–1.16). The cognitive/affective dimension was virtually unrelated to baseline health status except for left ventricular ejection fraction, but the somatic/affective and appetitive dimensions were associated with poor left ventricular ejection fraction, high Charlson comorbidity index, high Killip class, and previous myocardial infarction (Table 2); the strongest associations were found with respect to the somatic/affective dimension.
Association of Factor Scores With Cardiovascular Prognosis
Relating the three symptom dimensions to time-related cardiovascular death and cardiac-related readmissions resulted in significant associations for somatic/affective symptoms but not cognitive/affective or appetitive symptoms (Table 2). The association of the somatic/affective dimension with cardiovascular death remained statistically significant when the three factors entered the logistic regression model simultaneously and left ventricular ejection fraction, Killip class, and previous myocardial infarction were controlled. A negative association of the cognitive/affective dimension with cardiovascular death (p=0.04) was found in the multivariate analyses (i.e., cognitive/affective symptoms protective for cardiovascular death), suggesting that the effects of cognitive/affective symptoms are being (over)corrected by the somatic/affective symptoms. The association between somatic/affective symptoms and cardiovascular events lost statistical significance (p=0.10) in the multivariate analyses, but the strength of the association only slightly decreased (from odds ratio=1.39 to odds ratio=1.30).
In order to visualize the prospective association of the BDI factor scores with the time-related outcomes, we recoded the factor scores in dummy variables with approximately 20% of the highest scoring individuals receiving a “1” and the others a “0.” In Figure 1, the temporal relationship between the dummy variables with combined prospective cardiovascular events or cardiovascular death is shown. The corresponding log-rank tests to assess the significance of the relationships were 8.33 for the somatic-affective (p=0.004), 1.69 for the cognitive-affective (p=0.17), and 0.26 for the appetitive symptoms (p=0.67). With varying cutoff points, i.e., based on the 90th and 75th percentiles, significant associations between depression and time-related outcomes were found only with respect to somatic/affective symptoms.
Discussion
In two large groups of myocardial infarction patients, we related three depressive symptom dimensions to baseline somatic health status and prospective cardiovascular prognosis. Somatic/affective symptoms were associated with poor baseline somatic health status, adding fuel to the discussion of whether depression is an independent factor after myocardial infarction or one that is confounded by myocardial infarction-related complaints. Although we do not know whether the post-myocardial infarction somatic/affective symptoms were already present before the myocardial infarction (about a quarter of post-myocardial infarction depressed patients reported a major depressive episode in the month preceding the myocardial infarction), our findings showed that the somatic/affective depressive symptoms following myocardial infarction were associated with the severity of the myocardial infarction. The cognitive/affective symptoms of depression were only marginally associated with poor somatic health at baseline. Appetitive symptoms—the third symptom dimension—were not related to the presence of depression in the first 3 months after myocardial infarction, which suggests that these symptoms may not represent clinical depression in myocardial infarction patients.
Watkins et al. (26) previously reported that medical comorbidity was related to somatic depression symptoms (r=0.24) and virtually unrelated to cognitive depression symptoms (r=0.06). However, this distinction between symptom groups has not been validated, and the somatic symptoms seem to especially consist of several marginally related complaints. For example, Irvine and colleagues (5) reported an internal consistency of only 0.67, which is insufficient to warrant a reliable sum score. In line with the study by Watkins and colleagues, when two equally reliable depressive symptom dimensions were used (somatic/affective: 0.81; cognitive/affective: 0.82), we showed that only the somatic/affective symptoms were associated with medical comorbidity, left ventricular ejection fraction, heart failure, and presence of a previous myocardial infarction.
It is interesting that the somatic/affective dimension of depressive symptoms was the only one of the three factors associated with cardiovascular death and cardiac-related readmissions during an average follow-up of 2.5 years. Although the somatic/affective symptoms of depression were confounded by the patient’s somatic health status, they did have a prospective relationship with poor cardiovascular prognosis even after baseline somatic health status was controlled.
Presumably, the statistical association between somatic/affective symptoms and cardiovascular prognosis comprises two components. One component might be the effect of myocardial infarction severity on cardiovascular prognosis and the covariation of myocardial infarction severity with somatic/affective symptoms. Their combination produces a statistical association between somatic/affective symptoms and cardiovascular prognosis. The second component might result from an influence of somatic/affective symptoms on cardiovascular prognosis that is independent of the effect of myocardial infarction severity. This independent effect also produces statistical association between somatic/affective symptoms and prognosis. In comparison, Barefoot and colleagues (35) found that negative affective symptoms of depression (sadness, crying, suicidal ideas, irritability, restlessness)—but not well-being, somatic, or appetitive symptoms—predicted mortality in coronary artery disease patients after severity of cardiovascular disease was controlled. In our model, most of the items referred to by Barefoot and colleagues as negative affective symptoms of depression were incorporated in the somatic/affective factor (e.g., sadness, crying, irritability, indecisiveness). This prospective association suggests that the somatic/affective component has an independent effect on cardiac prognosis, an effect that the cognitive/affective component has not. Figure 2 shows schematically our position. In model A, no distinction between the components of depression is made, whereas one is made in model B.
Our findings have implications for the treatment of depression following myocardial infarction because they suggest that antidepressive treatment needs to be effective in reducing the somatic/affective symptoms in order to have the potential to affect cardiac prognosis. Effective treatment of the cognitive/affective symptoms is probably not sufficient, since these are not associated with cardiac prognosis unless their treatment also leads to remission of the somatic/affective symptoms. The null results of the Enhancing Recovery in Coronary Heart Disease Patients trial (36)—effective treatment of post-myocardial infarction depression did not lead to a better cardiac prognosis—can be understood in a theoretical framework in which depression consists of some aspects related to cardiovascular prognosis and some that are not. It is interesting that in that study it was found that cognitive behavior therapy decreased depression and improved social support more than usual care, without affecting the primary endpoint of death and nonfatal infarction. However, in secondary analyses, the prescription of specific serotonin reuptake inhibitors was associated with less cardiac events. A similar but nonsignificant trend was observed in the Sertraline AntiDepressant Heart Attack Trial in which post-myocardial infarction depressed patients were treated with sertraline and compared with patients who received placebo (37). To date, this issue has not been resolved, and we can only speculate on the effects of antidepressant medication on each symptom dimension and, subsequently, on cardiovascular prognosis.
By combining the strengths of two studies—the MIND-IT contained a large patient group with an extensive baseline assessment of somatic health status, and the Depression After Myocardial Infarction study contained a long-term follow-up of depressed and nondepressed myocardial infarction patients—we clarified the way in which the relationship between post-myocardial infarction depression and cardiovascular prognosis may be confounded by baseline somatic health status. Research on the bidirectional relationship between depression and cardiac diseases has extended explosively in the last decade, with evidence for an increased risk of heart disease following depression, an increased risk of depression following heart disease, and a worsened cardiac prognosis when both are present.
 |
 |
Received Aug. 12, 2004; revision received Nov. 26, 2004; accepted Jan. 24, 2005. From the University of Groningen Departments of Psychiatry, Internal Medicine, and Cardiology; the Department of Psychiatry, University Hospital Amsterdam; the Department of Psychiatry, St. Lucas Andreas Hospital, Amsterdam; and the Department of Cardiology, University Hospital Maastricht, Maastricht, the Netherlands. Address correspondence and reprint requests to Dr. de Jonge, Department of Psychiatry, University of Groningen, P.O. Box 30.001, 9700 RB Groningen, the Netherlands; [email protected] (e-mail). The Myocardial INfarction and Depression-Intervention Trial (MIND-IT) was funded by a grant from the Netherlands Heart Foundation (97.016) to Dr. J. Ormel. In addition, the MIND-IT received small educational grants from Organon (the Netherlands) and Lundbeck (Denmark). See the online version of this article for additional information on the MIND-IT and Depression After Myocardial Infarction studies.
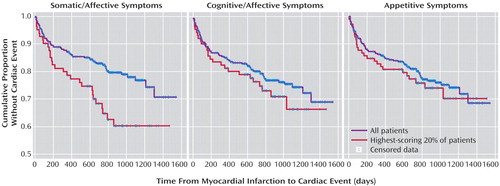
Figure 1. Event-Free Survival Days Following Myocardial Infarction and Relationship With Depressive Symptoms (N=494)
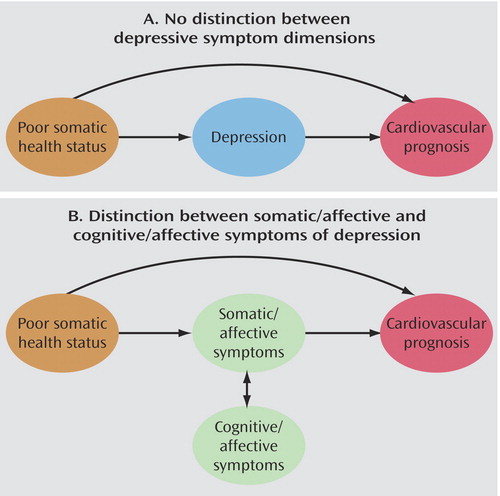
Figure 2. Models for the Relationship Between Depression and Cardiovascular Prognosis Following Myocardial Infarction
1. Frasure-Smith N, Lesperance F, Talajic M: Depression following myocardial infarction: impact on 6-month survival. JAMA 1993; 270:1819–1825Crossref, Medline, Google Scholar
2. Lesperance F, Frasure-Smith N, Talajic M: Major depression before and after myocardial infarction: its nature and consequences. Psychosom Med 1996; 58:99–110Crossref, Medline, Google Scholar
3. Frasure-Smith N, Lesperance F, Talajic M: Depression and 18-month prognosis after myocardial infarction. Circulation 1995; 91:999–1005Crossref, Medline, Google Scholar
4. Hemingway H, Marmot M: Evidence based cardiology: psychosocial factors in the aetiology and prognosis of coronary heart disease: systematic review of prospective cohort studies. BMJ 1999; 318:1460–1467Crossref, Medline, Google Scholar
5. Irvine J, Basinski A, Baker B, Jandciu S, Paquette M, Cairns J, Connolly S, Roberts R, Gent M, Dorian P: Depression and risk of sudden cardiac death after acute myocardial infarction: testing for the confounding effects of fatigue. Psychosom Med 1999; 61:729–737Crossref, Medline, Google Scholar
6. Mendes de Leon CF: Depression and social support in recovery from myocardial infarction: confounding and confusion. Psychosom Med 1999; 61:738–739Crossref, Medline, Google Scholar
7. Lane D, Carroll D, Lip GYH: Anxiety, depression and prognosis after myocardial infarction: is there a causal relationship? J Am Coll Cardiol 2003; 42:1801–1810Crossref, Medline, Google Scholar
8. Carney RM, Freedland KE, Jaffe AS, Frasure-Smith N, Lesperance F, Sheps DS, Glassman AH, O’Connor CM, Blumenthal JA, Kafman PG, Czajkowski SM: Depression as a risk factor for post-MI mortality. J Am Coll Cardiol 2004; 44:472Google Scholar
9. Pickering TG, Davidson K, Shimbo D: Is depression a risk factor for coronary heart disease? (letter). J Am Coll Cardiol 2004; 44:472–473Google Scholar
10. Lane D, Carroll D, Lip GYH: Reply to TG Pickering, K Davidson, Shimbo D: Is depression a risk factor for coronary heart disease? (letter). J Am Coll Cardiol 2004; 44:473–474Crossref, Google Scholar
11. Van Melle JP, de Jonge P, Spijkerman TA, Tijssen JGP, Ormel J, van Veldhuisen DJ, van den Berg MP: Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis. Psychosom Med 2004; 66:814–822Crossref, Medline, Google Scholar
12. Bush DE, Ziegelstein RC, Tayback M, Richter D, Stevens S, Zahalsky H, Fauerbach JA: Even minimal symptoms of depression increase mortality risk after acute myocardial infarction. Am J Cardiol 2001; 88:337–341Crossref, Medline, Google Scholar
13. Ladwig KH, Kieser M, Konig J, Breithardt G, Borggrefe M: Affective disorders and survival after acute myocardial infarction: results from the post-infarction late potential study. Eur Heart J 1991; 12:959–964Medline, Google Scholar
14. Frasure-Smith N, Lesperance F, Talajic M: The impact of negative emotions on prognosis following myocardial infarction: is it more than depression? Health Psychol 1995; 14:388–398Crossref, Medline, Google Scholar
15. Sydeman SJ: Impact of negative emotions on recurrent cardiovascular events following hospitalization for myocardial infarction or unstable angina. Dissertation Abstracts International B: The Sciences and Engineering 1999Google Scholar
16. Kaufmann MW, Fitzgibbons JP, Sussman EJ, Reed JF III, Einfalt JM, Rodgers JK, Fricchione GL: Relation between myocardial infarction, depression, hostility, and death. Am Heart J 1999; 138:549–554Crossref, Medline, Google Scholar
17. Shiotani I, Sato H, Kinjo K, Nakatani D, Mizuno H, Ohnishi Y, Hishida E, Kijima Y, Hori M, Sato H: Depressive symptoms predict 12-month prognosis in elderly patients with acute myocardial infarction. J Cardiovasc Risk 2002; 9:153–160Crossref, Medline, Google Scholar
18. Lauzon C, Beck CA, Huynh T, Dion D, Racine N, Carignan S, Diodati JG, Charbonneau F, Dupuis R, Pilote R: Depression and prognosis following hospital admission because of acute myocardial infarction. CMAJ 2003; 168:547–552Medline, Google Scholar
19. Carney RM, Blumenthal JA, Catellier D, Freedland KE, Berkman LF, Watkins LL, Czajkowski SM, Hayano J, Jaffe AS: Depression as a risk factor for mortality after acute myocardial infarction. Am J Cardiol 2003; 92:1277–1281Crossref, Medline, Google Scholar
20. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J: An inventory for measuring depression. Arch Gen Psychiatry 1961; 4:561–571Crossref, Medline, Google Scholar
21. Beck AT, Steer RA: Manual for the Revised Beck Depression Inventory. San Antonio, Tex, Psychological Corp, 1987Google Scholar
22. Clark DC, Cavanaugh SVA, Gibbons RD: The core symptoms of depression on medical and psychiatric patients. J Nerv Ment Dis 1983; 171:705–713Crossref, Medline, Google Scholar
23. Huber SJ, Freidenberg DL, Paulson GW, Shuttleworth EC, Christy JA: The pattern of depressive symptoms varies with progression of Parkinson’s disease. J Neurol Neurosurg Psychiatry 1990; 53:275–278Crossref, Medline, Google Scholar
24. Johnson SK, DeLuca J, Natelson BJ: Depression in fatiguing illness: comparing patients with chronic fatigue syndrome, multiple sclerosis and depression. J Affect Disord 1996; 39:21–30Crossref, Medline, Google Scholar
25. Soderman E, Lisspers J: Diagnosing depression in patients with physical diseases using the Beck Depression Inventory (BDI). Scand J Behav Ther 1997; 26:102–112Crossref, Google Scholar
26. Watkins LL, Schneiderman N, Blumenthal JA, Sheps DS, Catellier D, Taylor CB, Freedland KE: Cognitive and somatic symptoms of depression are associated with medical comorbidity in patients after acute myocardial infarction. Am Heart J 2003; 146:48–54Crossref, Medline, Google Scholar
27. Morley S, Williams AC, Black S: A confirmatory factor analysis of the Beck Depression Inventory in chronic pain. Pain 2002; 99:289–298Crossref, Medline, Google Scholar
28. Campbell IM, Burgess PM, Finch SJ: A factorial analysis of BDI scores. J Clin Psychol 1984; 40:992–996Crossref, Medline, Google Scholar
29. van den Brink RH, van Melle JP, Honig A, Schene AH, Crijns HJ, Lambert FP, Ormel J: Treatment of depression after myocardial infarction and the effects on cardiac prognosis and quality of life: rationale and outline of the Myocardial INfarction and Depression-Intervention Trial (MIND-IT). Am Heart J 2002; 144:219–225Crossref, Medline, Google Scholar
30. Joreskog KG: Simultaneous factor analysis in several populations. Psychometrika 1971; 36:409–426Crossref, Google Scholar
31. Cudeck R, Browne MW: Cross-validation of covariance structures. Multivariate Behav Res 1983; 18:147–167Crossref, Google Scholar
32. Bentler PM: Multivariate analysis with latent variables: causal modeling. Ann Rev Psychol 1980; 31:419–456Crossref, Google Scholar
33. Marsh HW, Balla JR, McDonald RP: Goodness-of-fit indexes in confirmatory factor analysis: the effect of sample size. Psychol Bull 1988; 103:391–410Crossref, Google Scholar
34. Strik JJ, Honig A, Lousberg R, Denollet J: Sensitivity and specificity of observer and self-report questionnaires in major and minor depression following myocardial infarction. Psychosomatics 2001; 42:423–428Crossref, Medline, Google Scholar
35. Barefoot JC, Brummett BH, Helms MJ, Mark DB, Siegler IC, Williams RB: Depressive symptoms and survival of patients with coronary artery disease. Psychosom Med 2000; 62:790–795Crossref, Medline, Google Scholar
36. Berkman LF, Blumenthal J, Burg M, Carney RM, Catellier D, Cowan MJ, Czajkowski SM, DeBusk R, Hosking J, Jaffe A, Kaufmann PG, Mitchell P, Norman J, Powell LH, Raczynski JM, Schneiderman N: Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) randomized trial. JAMA 2003; 289:3106–3116Crossref, Medline, Google Scholar
37. Glassman AH, O’Connor CM, Califf RM, Swedberg K, Schwartz P, Bigger JT, Krishnan KR, van Zyl LT, Swenson JR, Finkel MS, Landau C, Shapiro PA, Pepine CJ, Mardekian J, Harrison WM, Barton D, Mclvor M: Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA 2002; 288:701–709Crossref, Medline, Google Scholar



