Adaptive, Emotional, and Family Functioning of Children With Obsessive-Compulsive Disorder and Comorbid Attention Deficit Hyperactivity Disorder
Abstract
OBJECTIVE: The purpose of the study was to examine adaptive, emotional, and family functioning in a well-characterized group of children and adolescents with obsessive-compulsive disorder (OCD) and to evaluate the influence of comorbid attention deficit hyperactivity disorder (ADHD) on the levels of impairment in various functional domains. METHOD: The study group included 287 children and adolescents (191 boys, 96 girls) ages 7–18 years. Fifty-six subjects had a diagnosis of OCD only, 43 had both OCD and ADHD, 95 had ADHD, and 93 were unaffected comparison children. Best estimate DSM-IV diagnoses were assigned on the basis of structured interviews and clinical ratings. The children’s functioning was evaluated with a comprehensive battery of well-established, standardized measures, including the Vineland Adaptive Behavior Scales, parents’ ratings of social and family functioning, and children’s self-reports of emotional adjustment. RESULTS: The children with OCD only were more impaired than were unaffected comparison subjects in most areas of adaptive functioning and emotional adjustment. Children with OCD plus ADHD had additional difficulties in social functioning, school problems, and self-reported depression. Impairment in daily living skills, reduced number of activities, and self-reported anxiety were uniquely associated with the diagnosis of OCD. Family dysfunction was associated with ADHD but not with OCD. CONCLUSIONS: Children and adolescents with OCD are impaired in multiple domains of adaptive and emotional functioning. When comorbid ADHD is present, there is an additional burden on social, school, and family functioning.
Obsessive-compulsive disorder (OCD) is a neuropsychiatric condition characterized by distressing and intrusive thoughts, impulses, or images (obsessions) and repetitive overt or covert behaviors (compulsions) performed to reduce distress. A diagnosis of OCD requires that the symptoms cause marked distress or significantly interfere with the person’s functioning. OCD is present in 2%–4% of adolescents (1, 2), although it is probably less common in prepubescent children (3). In groups of OCD subjects drawn from clinical settings, the lifetime rates of comorbidity with depression, anxiety, and tic disorders have been estimated to be as high as 80%, 70%, and 60%, respectively (4–7). Clinical accounts often reflect that children with OCD are impaired in their daily routine, emotional adjustment, family and peer relationships, and academic performance. Although many reports of the phenomenology and clinical features of childhood OCD are available, many studies have failed to use standardized measures of adaptive functioning, and they have been limited by small size of the study groups and the absence of comparison groups (8–13).
Comorbidity with attention deficit hyperactivity disorder (ADHD), a common childhood psychiatric disorder, has been relatively neglected in the research on childhood OCD. In reports on groups of subjects in clinical settings, the rate of co-occurrence of the two conditions varied from 10% to 50% (6, 9, 12, 14, 15). In one population-based study, ADHD was present in two (10%) of 20 adolescents with OCD (16), and in another study 11 (44%) of 25 children with OCD were found to have a disruptive behavior disorder (17). The adverse influence of ADHD on children’s social, academic, and family functioning has been well documented (18). In addition, comorbid ADHD in children with various psychiatric disorders has been associated with greater functional impairment (19, 20). Comorbid ADHD was associated with greater global impairment and with a high rate of educational problems in children with OCD (21, 22). However, the effects of co-occurring ADHD in specific areas of adaptive, family, and emotional functioning of children with OCD have not been examined.
The goals of this study were to examine the levels of adaptive, emotional, and family functioning in a well-characterized group of children and adolescents with OCD and to evaluate the effect of comorbid ADHD. Four groups of children were studied: children with OCD only, children with OCD plus ADHD, children with ADHD only, and healthy comparison subjects. It was hypothesized that relative to the healthy comparison subjects and OCD-only groups, children with OCD plus ADHD would have greater levels of impairment in adaptive, emotional, and family functioning. We also explored how much of the impairment was added by the presence of ADHD after statistically controlling for the diagnosis of OCD.
Method
Subjects
Subjects included 287 children and adolescents (191 boys, 96 girls; mean age=11.5 years, SD=2.5) who participated in one or more studies of childhood neuropsychiatric disorders conducted at the Yale Child Study Center between 1993 and 2001. Fifty-six subjects had a diagnosis of OCD only, and 43 had OCD plus ADHD. Also included were 95 children with ADHD and 93 unaffected comparison children. The OCD subjects were ascertained through the Tic Disorders/OCD Specialty Clinic and through the local chapter of the Obsessive-Compulsive Foundation. Across the two OCD groups, 48 subjects also met the criteria for Tourette’s disorder. Subjects with a primary diagnosis of ADHD were recruited either through the Yale outpatient clinic or through a local chapter of Children and Adults With Attention Deficit Disorder. Unaffected comparison children were recruited from randomly selected names on a telemarketing list of approximately 10,000 families in the local community and were selected to group-match the affected children with respect to age, gender, income, and ethnicity. Children from approximately 10% of families who were contacted participated, and they received the same diagnostic evaluation as other subjects. Children with a history of neurological illness, past seizures or history of head trauma with loss of consciousness, mental retardation, pervasive developmental disorder, psychosis, or severe major depression were excluded. Additional exclusionary criteria for unaffected comparison subjects were any history of OCD, ADHD, tic disorder, or current axis I disorder. Socioeconomic status was estimated with the Hollingshead four-factor index (23); the majority of the families were middle to upper-middle class. After complete description of the study to the subjects, written informed consent was obtained from the parents and assent was obtained from the children.
Procedures
The main sources of information to establish a diagnosis of OCD were in-person structured interviews, the subject’s medical record, and the Children’s Yale-Brown Obsessive Compulsive Scale (11), administered by an experienced master’s-level clinician as an interview with each child and parent. Comorbid psychiatric diagnoses were established through comprehensive clinical evaluation and administration of the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version (24), the Yale Global Tic Severity Scale (25), and the Children’s Depression Rating Scale Revised (26). The parents’ scale of the Conners’ Teachers and Parents Rating Scales (27) was used to obtain the 10-item hyperactivity index. After a review of all available information, two senior clinicians independently assigned DSM-IV diagnoses using best-estimate procedures (28). Kappa statistics for OCD and ADHD were 1.00 and 0.66, respectively (29). All subjects also completed a comprehensive battery of standardized self-report and parent-rated measures. Research assistants administering these measures were blind to the diagnostic status of the subjects. During these evaluation procedures, children who received medication continued to take their usual dose and type of medication.
Dependent Measures
The Vineland Adaptive Behavior Scales Survey Form (30) is a semistructured interview used to measure the performance of daily activities required for personal and social sufficiency. It was developed for individuals from birth through age 19 years and standardized with a large national sample (mean=100, SD=15). Extensive reliability and validity information is available for this instrument. Three domain indices were included in this study. The communication domain reflects receptive, expressive, and written communication skills. The daily living skills domain samples personal living habits, domestic task performance, and behavior in the community. The socialization domain assesses interaction with others, including friendships, play, and social appropriateness.
The Child Behavior Checklist (31) is a standardized parent-rated instrument that measures competencies in three areas of adaptive functioning (activities, social, and school) and also measures emotional and behavioral problems. Most items are answered on a 3-point Likert-type scale, several items are dichotomous, and T scores (mean=50, SD=10) provide a numeric unit that is similar for all scales. The activities competence scale reflects the number of sports, hobbies, and clubs in which the child participates, as well as the parent’s perception of how well the child performs in these activities, compared to other children. The social competence scale assesses the number of friends, amount of time spent with friends, and the extent to which the child gets along with peers. The school competence scale is a parent report of the child’s grades in academic subjects and the child’s history of special education services, repeated grades, or school problems. The internalizing problems scale was used as a broad index of emotional adjustment.
The Family Environment Scale (32) is a parent-rated scale that consists of 10 nine-item subscales evaluating various aspects of family functioning. Three subscales pertaining to family relations were used in this study. The cohesion subscale pertains to the degree of commitment, help, and support family members provide to each other. The conflict subscale measures the degree to which family members openly express anger, aggression, and disagreement toward each other. The control subscale evaluates the number of family rules and the extent to which family rules are expected to be followed. All items are answered in a true/false response format, and scores are reported as averages.
Two children’s self-report scales were used to measure emotional adjustment. The Children’s Depression Inventory (33) is a 27-item measure that assesses a range of depressive symptoms in children and adolescents. Items are scored on a 3-point scale (0=no symptom, 1=mild symptom, and 2=definite symptom). The Children’s Manifest Anxiety Scale—Revised (34) consists of 37 items answered on a yes/no scale. A sum of “yes” responses to the 28 anxiety items determines the total anxiety score. Extensive norms and T scores are available for both scales.
Data Analysis
Separate multivariate analyses of covariance (MANCOVAs), with age, gender, and a diagnosis of Tourette’s disorder as covariates, were used to examine the differences among the four diagnostic groups in scores on the Child Behavior Checklist, the Vineland Adaptive Behavior Scales, the Family Environment Scale, and emotional adjustment measures. The multivariate tests were followed by post hoc multiple comparisons with the Holm adjustment for each dependent variable. Pearson’s product-moment correlations were used to examine the associations among normally distributed continuous variables, and chi-square statistics were used to test the differences between categorical variables. Hierarchical regression analyses were used to examine the unique contributions of OCD and ADHD diagnostic status to the measures of adaptive functioning and emotional adjustment. Diagnostic status was coded as a categorical variable with four values (1=OCD, 2=OCD plus ADHD, 3=ADHD, and 4=unaffected comparison subjects) for the analyses of variance and as two dichotomous variables for the OCD and ADHD diagnoses (0=absent and 1=present) for the regression analyses. SPSS version 11.5 (SPSS, Inc., Chicago) was used for all data analyses, and an alpha level of p<0.05 (two-tailed) was used. List-wise deletion of missing values was used in the MANCOVAs and in the regression analyses, and pairwise deletion of missing values was used in univariate comparisons, chi-square tests, and Pearson’s product-moment correlations. In a preliminary analysis, the differences in age, gender, race, and comorbid diagnoses, as well as all dependent measures, between the subjects with and without the diagnosis of Tourette’s disorder were examined by using independent sample t tests and chi-square tests, and no significant differences were found (data not shown). Consequently, all individuals with OCD were considered together in the primary analyses, and a diagnosis of Tourette’s disorder (absent/present) was used as a statistical covariate. Because age was inversely associated with family coherence and positively associated with children’s reports of depression and anxiety, it was also included as a covariate in all subsequent analyses.
Results
The demographic and clinical characteristics of the four diagnostic groups are reported in Table 1. Significant differences were found in gender distributions across the four diagnostic groups, and subsequent analyses were conducted with adjustment for this difference. No significant differences were detected among the diagnostic groups in age or race. Table 1 also presents the scores on the Children’s Yale-Brown Obsessive Compulsive Scale, the Yale Global Tic Severity Scale, and the hyperactivity index based on the parents’ scale of the Conners’ Teachers and Parents Rating Scales. The groups with OCD only and OCD plus ADHD did not differ significantly in the severity of obsessive-compulsive symptoms. Likewise, the OCD-plus-ADHD and ADHD groups were similar in scores on the hyperactivity index. All three diagnostic groups were similar in measures of tic severity. The OCD-only and OCD-plus-ADHD groups, subjects who had OCD without Tourette’s disorder, and subjects who had an additional diagnosis of Tourette’s disorder did not differ significantly on any dependent measures (data not shown).
To minimize the number of comparisons, four separate MANCOVAs (with a diagnosis of Tourette’s disorder, age, and gender as covariates) were performed with the four groups of dependent variables. Multivariate effects of diagnostic status were significant for the Vineland Adaptive Behavior Scales domains (Pillai’s trace=0.28; F=6.51 df=3, 184, p<0.0001), the Child Behavior Checklist scales (Pillai’s trace=0.52; F=10.98, df=3, 213, p<0.0001), the Family Environment Scale subscales (Pillai’s trace=0.14; F=3.84, df=3, 237, p<0.0001), and the measures of depression and anxiety (Pillai’s trace=0.24; F=10.61, df=3, 238, p<0.0001). Post hoc univariate analyses and pairwise comparisons are reported in Table 2. All dependent variables yielded significant main effects of diagnostic status.
Adaptive Functioning
The OCD-only group had significantly lower scores than the unaffected comparison subjects on the communication, daily living skills, and socialization domains of the Vineland Adaptive Behavior Scales. The children with ADHD only and OCD plus ADHD scored significantly lower than the children with OCD only in the socialization domain. No other significant differences were detected between diagnostic groups on the Vineland Adaptive Behavior Scales. Similar results were found with the Child Behavior Checklist competencies scales. The OCD-only group scored significantly below the unaffected comparison subjects in social and school competencies. Similar to the results obtained with the Vineland Adaptive Behavior Scales socialization domain, the Child Behavior Checklist scales detected significant differences between the children with OCD only and the children with OCD plus ADHD, who had significantly lower scores in social and school competencies. Children with OCD plus ADHD also scored significantly below the unaffected comparison subjects on the Child Behavior Checklist activities scale.
Emotional Adjustment
Significant main effects of diagnostic status were observed for the parent-rated and self-report measures of emotional adjustment. The parents’ reports of emotional problems revealed the greatest differences among the groups. The OCD-plus-ADHD group had significantly more impairment as measured by the Child Behavior Checklist broad-band internalizing problems scale, compared with the other three groups. By contrast, the OCD-only group scored higher than the unaffected comparison subjects on internalizing problems but did not differ from the ADHD group on this measure. Self-report measures of depression and anxiety did not reveal significant differences among the three diagnostic groups, which all had scores well above those in the unaffected comparison group.
Family Functioning
The families of children with OCD only did not differ from the families of unaffected comparison subjects on the subscales of conflict and cohesion. By contrast, children with OCD plus ADHD lived in families with significantly greater levels of family dysfunction than did the unaffected comparison subjects, as evidenced by higher scores on the conflict scale and lower scores on the cohesion scale. The children with OCD plus ADHD had lower scores on the cohesion scale than did the children with OCD only. No significant differences were detected between the OCD-plus-ADHD and ADHD-only groups in any area of family functioning. The OCD-only group had a mean score on the family control scale that was significantly below the scores of the unaffected comparison subjects and of the OCD-plus-ADHD and ADHD groups.
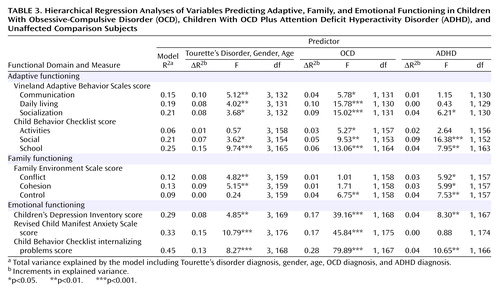
Unique Contributions of OCD and ADHD Diagnoses to Functioning
Hierarchical regression analyses were conducted to examine the effect of OCD and ADHD diagnostic status on measures of adaptive, family, and emotional functioning. The ADHD-only group (N=95) was excluded from these analyses. The effects of each variable were examined, controlling for the previously entered variables. All models were adjusted for age, gender, and comorbid Tourette’s disorder diagnosis. Table 3 presents the multiple regression coefficients for each dependent variable and R2 change, the increment in squared semipartial correlation of the criterion variable (e.g., Vineland socialization) with the predictor variable (e.g., OCD diagnosis) entered after adjustment for the variance accounted for by the predictor variables entered in the previous steps. A diagnosis of OCD correlated significantly with impairment on the measures of adaptive functioning and emotional adjustment. However, OCD did not have a significant negative influence on family functioning. ADHD, on the other hand, had significant negative influences on social functioning, school functioning, and self-reported depression over and above the diagnosis of OCD. ADHD also correlated uniquely and significantly with measures of family dysfunction. Impaired daily living skills and self-reported anxiety were associated with the diagnosis of OCD, and ADHD did not add a significant contribution over and above the impairment conferred by OCD.
Discussion
This study reports on functional impairment in a large, well-characterized group of children and adolescents with OCD with and without comorbid ADHD. Children with OCD only were more impaired than unaffected comparison subjects in multiple areas of adaptive functioning and emotional adjustment. Children with OCD plus ADHD were similar to the ADHD group in all areas of functional impairment and were more impaired than the OCD-only group in school and social functioning. Having a diagnosis of either OCD or ADHD contributed to impaired social functioning, school problems, and self-reported depression. By contrast, impairments in daily living skills, a low number of activities, and self-reported anxiety were uniquely associated with the diagnosis of OCD. Family dysfunction was associated with ADHD but not with OCD. These results are consistent with previous reports in which children with OCD were impaired and similar to matched psychiatric comparison subjects on global ratings of functioning (13).
Our results are consistent with earlier reports showing social impairment and academic underachievement in children with OCD (9, 11, 15). Consistent with reports of ADHD-related social impairments (35), our data suggest that OCD and ADHD have additive contributions to social disability. Moreover, comorbid ADHD contributes independently to the level of school maladjustment (21). In contrast to previous reports (8, 12, 36, 37), children with OCD only did not show significant family dysfunction. Our data suggest that family dysfunction is associated with ADHD rather than with the core symptoms of OCD. Parents of children with OCD only reported greater flexibility in family rules and decision making, compared to the other three groups. This result is somewhat unexpected and contradicts reports that parents of children with OCD tend to be controlling and discouraging of independence (38, 39). It is possible that in the absence of family conflict associated with co-occurring ADHD, parents of children with OCD learn to use adaptive parenting strategies that accommodate their children’s symptoms.
In accord with other studies, we found that children with OCD showed higher levels of self-reported depression and anxiety. The three groups with psychiatric diagnoses in our study did not differ significantly on self-report measures of negative affect or in clinicians’ ratings of depression. However, regression analyses revealed that a diagnosis of OCD had a greater influence on emotional adjustment and particularly on self-reported anxiety than did a diagnosis of ADHD. By contrast, parents reported higher levels of internalizing problems in children with OCD plus ADHD than in children with either one of these disorders alone. This finding suggests that ADHD, which is associated with poor emotion regulation (40, 41), may have an additive adverse effect on emotional adjustment in children with OCD.
Children with OCD and ADHD presented with similar levels of impairment in daily living skills as measured by the Vineland Adaptive Behavior Scales. Although adaptive functioning deficits in children with ADHD are well documented (18), in the current study ADHD did not contribute significantly to levels of impairment in daily living over and above the level of impairment conferred by OCD. Further studies are needed to examine whether different subdomains of daily living skills are differentially affected by OCD and ADHD. Utilizing measures developed for use with individuals with OCD (42) may help in examining whether some areas of adaptive functioning are more likely than others to be impaired.
The results of this study should be considered in light of its methodological limitations. Because the subjects with OCD were ascertained from a specialty clinic, they may not reflect the full breadth of OCD phenomenology. The association between the presence of OCD and functional impairment could be confounded by the child’s medication status. Psychotropic medications could have affected the severity of OCD or ADHD, of any comorbid symptoms, and of functional impairment. Indeed, scores for current obsessive-compulsive symptoms were in the range of mild to moderate severity, which may have limited our ability to see the full effects of OCD on functional variables such as family functioning. Similarly, the ADHD subjects were ascertained primarily from the Children and Adults With Attention Deficit Disorder organization. Children in families who participate in voluntary organizations may represent a biased sample. In addition, the study included mostly middle-class Caucasian subjects, and the results may not be generalizable to other populations. Finally, the cross-sectional design made it impossible to determine the direction of associations between the variables.
The cross-sectional data also do not shed light on the developmental features of these areas of psychopathology. For example, ADHD, by definition and clinical experience, has an onset by age 7 years and tends to be chronic throughout the childhood years; hence, ADHD tends to start early and to have a cumulative effect on school performance, peer relations, and family interactions, with substantial negative effect on self-esteem and interpersonal relationships. In contrast, the onset of OCD may occur at any time in childhood or adolescence, with many children having good premorbid functioning before the onset of OCD symptoms. Age of OCD onset, duration of illness, period of worst ever symptoms, and premorbid functioning may be important variables for future studies, and longitudinal or prospective studies would provide optimal data. Similarly, the relative effects of family history of psychopathology, presence of various OCD symptom dimensions, and different subtypes of OCD on comorbidity and functional impairment also remain to be explored (10, 43, 44).
 |
 |
 |
Received Aug. 21, 2003; revisions received Sept. 24, 2003, and May 27, 2004; accepted July 19, 2004. From the Child Study Center, Yale University School of Medicine; Yale School of Nursing, New Haven, Conn.; the Department of Psychiatry, New York State Psychiatric Institute and Columbia University, New York; and the Psychiatric and Neurodevelopmental Genetics Unit, Massachusetts General Hospital and Harvard Medical School, Boston. Address correspondence and reprint requests to Dr. Sukhodolsky, Child Study Center, Yale University School of Medicine, 230 South Frontage Rd., New Haven, CT 06520-7900; [email protected] (e-mail). Supported in part by grants NIMH MH-49351 (Dr. Leckman), MH-61940 (Dr. Leckman), MH-01232 (Dr. Peterson), MH-59239 (Dr. Peterson), and MH-30929 (Mental Health Research Center at Yale), NIH grant RR-06022 to the Children’s Clinical Research Center at Yale, the Smart Family Foundation, and Jean and Jay Kaiser.
1. Flament MF, Whitaker A, Rapoport JL, Davies M, Berg CZ, Kalikow K, Sceery W, Shaffer D: Obsessive compulsive disorder in adolescence: an epidemiological study. J Am Acad Child Adolesc Psychiatry 1988; 27:764–771Crossref, Medline, Google Scholar
2. Zohar AH: The epidemiology of obsessive-compulsive disorder in children and adolescents. Child Adolesc Psychiatr Clin North Am 1999; 8:445–460Crossref, Medline, Google Scholar
3. Costello EJ, Angold A, Burns BJ, Stangl DK, Tweed DL, Erkanli A, Worthman CM: The Great Smoky Mountains Study of Youth: goals, design, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psychiatry 1996; 53:1129–1136Crossref, Medline, Google Scholar
4. Flament MF, Koby E, Rapoport JL, Berg CJ, Zahn T, Cox C, Denckla M, Lenane M: Childhood obsessive-compulsive disorder: a prospective follow-up study. J Child Psychol Psychiatry 1990; 31:363–380Crossref, Medline, Google Scholar
5. Geller DA, Biederman J, Griffin S, Jones J, Lefkowitz TR: Comorbidity of juvenile obsessive-compulsive disorder with disruptive behavior disorders. J Am Acad Child Adolesc Psychiatry 1996; 35:1637–1646Crossref, Medline, Google Scholar
6. Geller DA, Biederman J, Faraone S, Agranat A, Cradock K, Hagermoser L, Kim G, Frazier J, Coffey BJ: Developmental aspects of obsessive compulsive disorder: findings in children, adolescents, and adults. J Nerv Ment Dis 2001; 189:471–477Crossref, Medline, Google Scholar
7. Leonard HL, Lenane MC, Swedo SE, Rettew DC, Gershon ES, Rapoport JL: Tics and Tourette’s disorder: a 2- to 7-year follow-up of 54 obsessive-compulsive children. Am J Psychiatry 1992; 149:1244–1251Link, Google Scholar
8. Cooper M: Obsessive-compulsive disorder: effects on family members. Am J Orthopsychiatry 1996; 66:296–304Crossref, Medline, Google Scholar
9. Hanna GL: Demographic and clinical features of obsessive-compulsive disorder in children and adolescents. J Am Acad Child Adolesc Psychiatry 1995; 34:19–27Crossref, Medline, Google Scholar
10. Scahill L, Kano Y, King RA, Carlson A, Peller A, LeBrun U, do Rosario-Campos MC, Leckman JF: Influence of age and tic disorders on obsessive-compulsive disorder in a pediatric sample. J Child Adolesc Psychopharmacol 2003; 13(suppl 1):S7-S17Google Scholar
11. Scahill L, Riddle MA, McSwiggin-Hardin M, Ort SI, King RA, Goodman WK, Cicchetti D, Leckman JF: Children’s Yale-Brown Obsessive Compulsive Scale: reliability and validity. J Am Acad Child Adolesc Psychiatry 1997; 36:844–852Crossref, Medline, Google Scholar
12. Swedo SE, Rapoport JL, Leonard H, Lenane M, Cheslow D: Obsessive-compulsive disorder in children and adolescents: clinical phenomenology of 70 consecutive cases. Arch Gen Psychiatry 1989; 46:335–341Crossref, Medline, Google Scholar
13. Thomsen PH, Mikkelsen HU: Course of obsessive-compulsive disorder in children and adolescents: a prospective follow-up study of 23 Danish cases. J Am Acad Child Adolesc Psychiatry 1995; 34:1432–1440Crossref, Medline, Google Scholar
14. Leonard HL, Swedo SE, Lenane MC, Rettew DC, Hamburger SD, Bartko JJ, Rapoport JL: A 2- to 7-year follow-up of 54 obsessive-compulsive children and adolescents. Arch Gen Psychiatry 1993; 50:429–439Crossref, Medline, Google Scholar
15. Riddle MA, Scahill L, King R, Hardin MT, Towbin KE, Ort SI, Leckman JF, Cohen DJ: Obsessive compulsive disorder in children and adolescents: phenomenology and family history. J Am Acad Child Adolesc Psychiatry 1990; 29:766–772Crossref, Medline, Google Scholar
16. Zohar AH, Ratzoni G, Pauls DL, Apter A, Bleich A, Kron S, Rappaport M, Weizman A, Cohen DJ: An epidemiological study of obsessive-compulsive disorder and related disorders in Israeli adolescents. J Am Acad Child Adolesc Psychiatry 1992; 31:1057–1061Crossref, Medline, Google Scholar
17. Heyman I, Fombonne E, Simmons H, Ford T, Meltzer H, Goodman R: Prevalence of obsessive-compulsive disorder in the British nationwide survey of child mental health. Br J Psychiatry 2001; 179:324–329Crossref, Medline, Google Scholar
18. Hinshaw SP: Is ADHD an impairing condition in childhood and adolescence? in Attention Deficit Hyperactivity Disorder: State of the Science, Best Practices. Edited by Jensen PS, Cooper JR. Kingston, NJ, Civic Research Institute, 2002, pp 5.1–5.21Google Scholar
19. Pliszka SR, Carlson CL, Swanson JM: ADHD With Comorbid Disorders: Clinical Assessment and Management. New York, Guilford, 1999Google Scholar
20. Sukhodolsky DG, Scahill L, Zhang H, Peterson BS, King RA, Lombroso PJ, Katsovich L, Findley D, Leckman JF: Disruptive behavior in children with Tourette’s syndrome: association with ADHD comorbidity, tic severity, and functional impairment. J Am Acad Child Adolesc Psychiatry 2003; 42:98–105Crossref, Medline, Google Scholar
21. Geller DA, Coffey B, Faraone S, Hagermoser L, Zaman NK, Farrell CL, Mullin B, Biederman J: Does comorbid attention-deficit/hyperactivity disorder impact the clinical expression of pediatric obsessive-compulsive disorder? CNS Spectr 2003; 8:259–264Crossref, Medline, Google Scholar
22. Geller DA, Biederman J, Faraone SV, Cradock K, Hagermoser L, Zaman N, Frazier JA, Coffey BJ, Spencer TJ: Attention-deficit/hyperactivity disorder in children and adolescents with obsessive-compulsive disorder: fact of artifact? J Am Acad Child Adolesc Psychiatry 2002; 41:52–58Crossref, Medline, Google Scholar
23. Hollingshead AB: Four-Factor Index of Social Status. New Haven, Conn, Yale University, Department of Sociology, 1975Google Scholar
24. Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N: Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 1997; 36:980–988Crossref, Medline, Google Scholar
25. Leckman JF, Riddle MA, Hardin MT, Ort SI, Swartz KL, Stevenson J, Cohen DJ: The Yale Global Tic Severity Scale: initial testing of a clinician-rated scale of tic severity. J Am Acad Child Adolesc Psychiatry 1989; 28:566–573Crossref, Medline, Google Scholar
26. Poznanski EO, Mokros H: Children’s Depression Rating Scale Revised (CDRS-R). Los Angeles, Western Psychological Services, 1996Google Scholar
27. Conners CK: Conners’ Rating Scales Manual. North Tonawanda, NY, Multi-Health Systems, 1989Google Scholar
28. Leckman JF, Sholomskas D, Thompson WD, Belanger A, Weissman MM: Best estimate of lifetime psychiatric diagnosis: a methodological study. Arch Gen Psychiatry 1982; 39:879–883Crossref, Medline, Google Scholar
29. Schultz RT, Carter AS, Gladstone M, Scahill L, Leckman JF, Peterson BS, Zhang H, Cohen DJ, Pauls D: Visual-motor integration functioning in children with Tourette syndrome. Neuropsychology 1998; 12:134–145Crossref, Medline, Google Scholar
30. Sparrow SS, Balla DA, Cicchetti DV: Vineland Adaptive Behavior Scales. Circle Pines, Minn, American Guidance Clinic, 1984Google Scholar
31. Achenbach TM: Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington, University of Vermont, Department of Psychiatry, 1991Google Scholar
32. Moos RH, Moos BM: Family Environment Scale Manual. Palo Alto, Calif, Consulting Psychologists Press, 1986Google Scholar
33. Kovacs M: The Children’s Depression Inventory (CDI). Psychopharmacol Bull 1985; 21:995–998Medline, Google Scholar
34. Reynolds CR, Richmond B: Revised Children’s Manifest Anxiety Scale (RCMAS) Manual. Los Angeles, Western Psychological Services, 1985Google Scholar
35. Greene RW, Biederman J, Faraone SV, Ouellette CA, Penn C, Griffin SM: Toward a new psychometric definition of social disability in children with attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 1996; 35:571–578Crossref, Medline, Google Scholar
36. Chambless DL, Steketee G: Expressed emotion and behavior therapy outcome: a prospective study with obsessive-compulsive and agoraphobic outpatients. J Consult Clin Psychol 1999; 67:658–665Crossref, Medline, Google Scholar
37. Hibbs ED, Hamburger SD, Kruesi MJ, Lenane M: Factors affecting expressed emotion in parents of ill and normal children. Am J Orthopsychiatry 1993; 63:103–112Crossref, Medline, Google Scholar
38. Barrett P, Shortt A, Healy L: Do parent and child behaviours differentiate families whose children have obsessive-compulsive disorder from other clinic and non-clinic families? J Child Psychol Psychiatry 2002; 43:597–607Crossref, Medline, Google Scholar
39. Valleni-Basile LA, Garrison CZ, Jackson KL, Waller JL, McKeown RE, Addy CL, Cuffe SP: Family and psychosocial predictors of obsessive compulsive disorder in a community sample of young adolescents. J Child Fam Studies 1995; 4:193–206Crossref, Google Scholar
40. Barkley RA: Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull 1997; 121:65–94Crossref, Medline, Google Scholar
41. Braaten EB, Rosen LA: Self-regulation of affect in attention deficit-hyperactivity disorder (ADHD) and non-ADHD boys: differences in empathic responding. J Consult Clin Psychol 2000; 68:313–321Crossref, Medline, Google Scholar
42. Piacentini J, Bergman RL, Keller M, McCracken J: Functional impairment in children and adolescents with obsessive-compulsive disorder. J Child Adolesc Psychopharmacol 2003; 13(suppl 1):S61-S69Google Scholar
43. King RA, Leckman J, Scahill L: Associated forms of psychopathology: obsessive-compulsive disorder, anxiety, and depression, in Tourette’s Syndrome—Tics, Obsessions, Compulsions: Developmental Psychopathology and Clinical Care. Edited by Leckman JF, Cohen DJ. New York, John Wiley & Sons, 1999, pp 43–62Google Scholar
44. Mataix-Cols D, do Rosario-Campos MC, Leckman JF: A multidimensional model of obsessive-compulsive disorder. Am J Psychiatry 2005; 162:228–238Link, Google Scholar



