Basal Ganglia High-Energy Phosphate Metabolism in Neuroleptic-Naive Patients With Schizophrenia: A 31-Phosphorus Magnetic Resonance Spectroscopic Study
Abstract
OBJECTIVE: This study used 31-phosphorus magnetic resonance spectroscopy (31P MRS) to investigate basal ganglia abnormalities in neuroleptic-naive patients with schizophrenia. METHOD: Nineteen schizophrenia patients and 31 age- and sex-matched healthy comparison subjects underwent 31P MRS. RESULTS: The phosphocreatine/total phosphorus and phosphocreatine/total ATP ratios in both basal ganglia were significantly lower in patients. CONCLUSIONS: Schizophrenia patients showed features of increased metabolism in the basal ganglia consistent with impaired activity of the frontostriatal pathways.
Several studies have implicated basal ganglia in the pathophysiology of schizophrenia (1–3). Decrease in caudate volumes has been reported in neuroleptic-naive patients with schizophrenia (4). Findings from 31-phosphorus magnetic resonance spectroscopy (31P MRS) studies have been inconclusive, perhaps due to differences in MRS methodology and medication status of the patients (5, 6).
We conducted a 31P MRS study of the basal ganglia in neuroleptic-naive patients with schizophrenia and matched healthy comparison subjects. Considering that dopaminergic activity is increased in schizophrenia in subcortical structures (7), we hypothesized that basal ganglia metabolism would be increased in the schizophrenia patients.
Method
Subjects
The study group consisted of 19 right-handed inpatients and 31 healthy comparison subjects. Patients and comparison subjects did not significantly differ in terms of age (patients: mean=27 years [SD=7.6]; healthy subjects: mean=29 years [SD=6.1]) or sex (15 male and four female patients and 21 male and 10 female healthy comparison subjects). Diagnosis of DSM-IV schizophrenia was determined by a psychiatrist with the Structured Clinical Interview for DSM-IV (paranoid: N=8; catatonic: N=3; disorganized: N=2; undifferentiated: N=6). Illness duration ranged between 6 and 120 months (mean=44, SD=35). No patient was ever previously treated for psychiatric illness. Mean age at onset of psychosis was 23.6 years (SD=6.4, range=15–39). Their mean Positive and Negative Syndrome Scale (8) score was 84 (SD=18, range=53–119). None had involuntary movements. MRS studies were conducted before starting antipsychotic treatment. Agitation was treated, where necessary, with lorazepam 2–6 mg/day in divided doses.
Healthy comparison subjects were screened using the 12-item General Health Questionnaire (9). None of the patients or healthy comparison subjects had a history of recent alcohol use (previous week) or scored positive on the CAGE questionnaire (10), and none used stimulants or opiate drugs. No subject had a history of epilepsy or any other neurological or medical disorder. All subjects provided written informed consent. The Institute’s ethics committee approved the study.
Spectroscopy
31P MRS was done on a 1.5 T scanner. Two-dimensional chemical shift imaging with image-guided in vivo spectroscopic localization and volume-selective adiabatic high-frequency pulses were used. The volume of interest was placed on representative slices of the brain in all three orthogonal planes interactively and simultaneously to avoid the ventricles. The volume of interest was localized to the basal ganglia with a mean size of 25×25×50 mm3 (Figure 1). The magnetic field shimming for homogeneity was done to achieve a line width less than 0.15 ppm. The technical parameters were repetition time of 1500 msec, free induction decay (FID) sampling rate of 1500 Hz, sampling points of 1024, and 12 measurements.
The average FID signal in the spectra was processed using proprietary software by the rater (P.N.J.) blind to clinical data, with phosphocreatine as the reference marker. The spectra were quantified as integral values by an inbuilt program of fitting curves. The integrated area of phosphocreatine, inorganic phosphate, αATP, βATP, and γATP were measured. Phosphocreatine/total phosphorus and phosphocreatine/total ATP ratios in right and left basal ganglia were computed. The ratios were compared between the two groups using independent sample t tests and between the right and left basal ganglia within each group using paired t tests. Significance was set at p<0.05.
Results
No significant differences were seen in phosphocreatine ratios between the right and left basal ganglia in patients or healthy comparison subjects. The average of the two sides was therefore used for analyses. Patients had lower mean phosphocreatine ratios than healthy comparison subjects (phosphocreatine/total phosphorus ratio: mean=0.25 [SD=0.064] versus 0.31 [SD=0.082], respectively [t=2.62, df=48, p<0.02]; phosphocreatine/ATP ratio: mean=0.70 [SD=0.18] versus 0.94 [SD=0.25] [t=3.64, df=48 p=0.001]; phosphocreatine/βATP ratio: mean=18.85 [SD=23.75] versus 40.26 [SD=48.86] [t=2.1, df=46.2, p=0.04], with correction for unequal variance]). The ATP/inorganic phosphate ratio was not different between patients (mean=70.02, SD=52.79) and healthy comparison subjects (mean=75.53, SD=44.88). After Bonferroni correction, phosphocreatine/total phosphorus and phosphocreatine/ATP ratios remained significantly different between patients and healthy comparison subjects. Phosphocreatine ratios of the patients not receiving lorazepam (N=5) did not differ from the rest (N=14) (phosphocreatine/total phosphorus ratio: mean=0.24 [SD=0.058] and 0.28 [SD=0.078], respectively; phosphocreatine/ATP ratio: mean=0.68 [SD=0.16] and 0.75 [SD=0.23]). Illness duration did not correlate with the phosphocreatine/total phosphorus ratio (r=0.22, df=17, p=0.36) or the phosphocreatine/ATP ratio (r=0.07, df=17, p=0.77).
Discussion
The main findings of this study were decreased phosphocreatine/total phosphorus, phosphocreatine/ATP, and phosphocreatine/βATP ratios in basal ganglia of the patients relative to healthy comparison subjects. When ATP is consumed during metabolism, phosphocreatine is converted to ATP to maintain energy balance. Hence, in metabolically more active tissues, the phosphocreatine would be lower. It suggests that basal ganglia metabolism is elevated in schizophrenia. This finding in neuroleptic-naive schizophrenia patients excludes medication effects. The lack of correlation with illness duration is consistent with the possibility of a nonprogressive (possibly developmental) dysfunction in schizophrenia (11). The cortical atrophy seen in schizophrenia patients (12) could result in reduced inhibitory corticostriatal transmission leading to hypermetabolism in basal ganglia (13). Alternatively, lower phosphocreatine may also be due to reduced synthesis, perhaps related to mitochondrial dysfunction in basal ganglia reported in schizophrenia (14, 15). The metabolic dysfunction of the basal ganglia is also corroborated by the membrane phospholipid abnormalities in this sample reported elsewhere (16).
The strength of the study is the use of neuroleptic-naive schizophrenia patients. Although some patients received lorazepam, phosphocreatine ratios of patients receiving lorazepam (N=5) were not different from the rest (N=14). Interassay reliabilities were not available. Some tissue heterogeneity (gray and white matter) is inevitable in the voxels, and intravoxel segmentation to separate tissue classes would have been useful. Finally, absolute values of metabolites were not measured. Nevertheless, ratio measures compare favorably with absolute measures (17).
In summary, neuroleptic-naive schizophrenia patients demonstrated increased high-energy phosphate metabolism in basal ganglia. The finding is consistent with impaired activity of corticostriatal pathways in schizophrenia.
Received April 22, 2002; revisions received Nov. 25, 2002, and Dec. 10, 2003; accepted Dec. 23, 2003. From the Department of Neuroimaging and Interventional Neuroradiology, the Department of Psychiatry, and the Department of Biostatistics, National Institute of Mental Health and Neurosciences, Bangalore, India; and the Department of Psychiatry, Western Psychiatric Institute and Clinic, Pittsburgh. Address reprint requests to Dr. P.N. Jayakumar, Professor and Head, Department of Neuroimaging and Interventional Radiology, National Institute of Mental Health and Neurosciences, Hosur Road, Bangalore, 5600 29, India; [email protected] (e-mail). Supported by Indo-US project 1 R43 04370-01A1 (1997–2001).
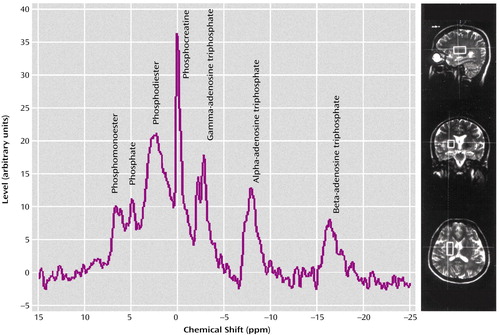
Figure 1. Basal Ganglia Phosphate Metabolism as Measured With 31P MRSa
aThe volume of interest in representative slices of the brain in all three orthogonal planes is shown in the images on the right.
1. Heckers S: Neuropathology of schizophrenia: cortex, thalamus, basal ganglia and neurotransmitter-specific projection systems. Schizophr Bull 1997; 23:403–421Crossref, Medline, Google Scholar
2. Kraepelin E: Dementia Praecox and Paraphrenia. Translated by Barclay RM; edited by Robertson GM. Edinburgh, E & S Livingstone, 1919Google Scholar
3. Walker E, Lewine RJ: Prediction of adult-onset schizophrenia from childhood home movies of the patients. Am J Psychiatry 1990; 147:1052–1056Link, Google Scholar
4. Keshavan MS, Rosenberg D, Sweeney JA, Pettegrew JW: Decreased caudate volume in neuroleptic-naive psychotic patients. Am J Psychiatry 1998; 155:774–778Abstract, Google Scholar
5. Deicken RF, Calabrese G, Merrin EL, Meyerhoff DJ, Dillon WP, Weiner MW, Fein G: 31Phosphorus magnetic resonance spectroscopy of the frontal and parietal lobes in chronic schizophrenia. Biol Psychiatry 1994; 36:503–510Crossref, Medline, Google Scholar
6. Fujimoto T, Nakano T, Takano T, Hokazono Y: Study of chronic schizophrenics using 31P magnetic resonance chemical shift imaging. Acta Psychiatr Scand 1992; 86:455–462Crossref, Medline, Google Scholar
7. Laruelle M, Abi-Dargham A: Dopamine as the wind of the psychotic fire: new evidence from brain imaging studies. J Psychopharmacol 1999; 13:358–371Crossref, Medline, Google Scholar
8. Kay SR, Opler LA, Lindenmayer JP: The Positive and Negative Syndrome Scale (PANSS): rationale and standardisation. Br J Psychiatry Suppl 1989; 7:59–67Medline, Google Scholar
9. Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, Rutter C: The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 1997; 27:191–197Crossref, Medline, Google Scholar
10. Ewing JA: Detecting alcoholism: the CAGE questionnaire. JAMA 1984; 252:1905–1907Crossref, Medline, Google Scholar
11. Weinberger DR: Implications of normal brain development for the pathogenesis of schizophrenia. Arch Gen Psychiatry 1987; 44:660–669Crossref, Medline, Google Scholar
12. Ross CA, Pearson GD: Schizophrenia, the heteromodal associating neocortex and development: potential for a neurogenetic approach. Trends Neurosci 1996; 19:171–176Crossref, Medline, Google Scholar
13. Seeman P, Guan H-C, Van Tol HHM: Dopamine D4 receptors elevated D2 dopamine receptors in drug-naive schizophrenics. Science 1986; 234:1558–1563Crossref, Medline, Google Scholar
14. Prince JA: Mitochondrial function is differentially altered in the basal ganglia of chronic schizophrenics. Neuropsychopharmacology 1999; 21:372–379Crossref, Medline, Google Scholar
15. Maurer I: Evidence for a mitochondrial oxidative phosphorylation defect in brain from patients with schizophrenia. Schizophr Res 2001; 48:125–136Crossref, Medline, Google Scholar
16. Jayakumar PN, Gangadhar BN, Subbakrishna DK, Janakiramaiah N, Srinivas JS, Keshavan MS: Membrane phospholipid abnormalities of basal ganglia in never-treated schizophrenia: a 31P magnetic resonance spectroscopy study. Biol Psychiatry 2003; 54:491–494Crossref, Medline, Google Scholar
17. Klunk WE, Xu CJ, Panchalingam K, McClure RJ, Pettegrew JW: Analysis of magnetic resonance spectra by mole percent: comparison of absolute units. Neurobiol Aging 1994; 15:133–140Crossref, Medline, Google Scholar



