Psychiatric Comorbidity, Family Dysfunction, and Social Impairment in Referred Youth With Oppositional Defiant Disorder
Abstract
OBJECTIVE: The authors sought to achieve an improved understanding of the diagnosis of oppositional defiant disorder independent of its association with conduct disorder. METHOD: Family interactions, social functioning, and psychiatric comorbidity were compared in clinically referred male and female subjects with oppositional defiant disorder alone (N=643) or with comorbid conduct disorder (N=262) and a psychiatric comparison group with neither oppositional defiant disorder nor conduct disorder (N=695). RESULTS: Oppositional defiant disorder youth with or without conduct disorder were found to have significantly higher rates of comorbid psychiatric disorders and significantly greater family and social dysfunction relative to psychiatric comparison subjects. Differences between subjects with oppositional defiant disorder alone and those with comorbid conduct disorder were seen primarily in rates of mood disorders and social impairment. Oppositional defiant disorder was a significant correlate of adverse family and social outcomes when comorbid disorders (including conduct disorder) were controlled. CONCLUSIONS: These results support the validity of the oppositional defiant disorder diagnosis as a meaningful clinical entity independent of conduct disorder and highlight the extremely detrimental effects of oppositional defiant disorder on multiple domains of functioning in children and adolescents.
Oppositional defiant disorder refers to a recurrent pattern of developmentally inappropriate levels of negativistic, defiant, disobedient, and hostile behavior toward authority figures. The behaviors associated with oppositional defiant disorder—including actively defying or refusing to comply with adult rules and requests, frequent temper outbursts, and excessive arguing—can significantly impede adaptive adult-child and child-peer interactions (1–7). Indeed, parents of children with oppositional defiant disorder are more likely to utilize child mental health services than parents of children with other disruptive behavior disorders (8).
Despite its clinical relevance, surprisingly little is known about oppositional defiant disorder. This may be due, in part, to a tendency to view oppositional defiant disorder simply as a variant of conduct disorder (9, 10). Indeed, most studies on disruptive behavior disorders have combined children with oppositional defiant disorder and conduct disorder into a single generic category, often called “conduct problems” (11, 12). It has been argued that this practice has contributed to obscured findings and conclusions that are difficult to interpret (10).
Certainly a clear overlap has been established between conduct disorder and oppositional defiant disorder (6, 10–13), and there is evidence to suggest that oppositional defiant disorder precedes conduct disorder in a substantial percentage of cases (14). However, the majority of children with oppositional defiant disorder do not have conduct disorder (11), and many children with oppositional defiant disorder exhibit ongoing oppositional behavior without ever developing conduct disorder (11, 15). Indeed, we have previously shown that subsequent diagnoses of conduct disorder in youth with oppositional defiant disorder are quite infrequent beyond age 6 (11).
An improved understanding of oppositional defiant disorder therefore requires examination of the clinical correlates of the disorder independent of its association with conduct disorder. Such information can strengthen our understanding of oppositional defiant disorder as a meaningful nosological entity and lead to improved treatment approaches aimed at ameliorating the disorder. Toward this end, the purpose of this study was to determine the clinical significance of oppositional defiant disorder alone (i.e., independent of conduct disorder) by examining family interactions, social functioning, and psychiatric comorbidity in a group of clinically referred children with oppositional defiant disorder, either alone or with comorbid conduct disorder, and a group of children with neither disorder.
Method
Study Group
The subjects were 1,600 children and adolescents (mean age=10.7 years) referred to the child psychiatry service at Massachusetts General Hospital. There were 643 youth (468 boys, 175 girls) with oppositional defiant disorder alone, 262 youth (210 boys, 52 girls) with oppositional defiant disorder plus conduct disorder, and 695 psychiatric comparison subjects (487 boys, 208 girls) with neither oppositional defiant disorder nor conduct disorder. Although all children and adolescents were referred for clinical care, they were not selected for any specific psychiatric condition. There was also no selection based on social class or insurance restrictions. This study received institutional review board approval to review, analyze, and report anonymously on these subjects.
Assessment Procedures
DSM-III-R diagnoses were obtained through maternal report by using the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Epidemiologic Version (16). All assessments were conducted by carefully supervised research assistants who were trained to high levels of interrater reliability. Kappa coefficients of agreement were computed between these raters and experienced, board-certified child and adult psychiatrists who listened to audiotaped recordings of randomly selected interviews. Based on 61 interviews, the mean kappa was 0.90; all diagnoses had kappas higher than 0.82. Diagnoses were considered positive if, on the basis of interview results, full DSM-III-R criteria were unequivocally met. All diagnostic uncertainties were resolved by a committee of board-certified child psychiatrists who were blind to all nondiagnostic data (e.g., socioeconomic status, family and social functioning). A diagnosis of depression was made only if the depressive episode was associated with marked impairment (17). Since the anxiety disorders comprise many syndromes with a wide range of severity, we used the designation “multiple anxiety disorders” (two or more anxiety disorders) to define a relatively severe anxiety syndrome (18). Rates of disorders reported here represent lifetime prevalence.
In addition to diagnostic information, interviewers also assessed adaptive functioning by using the DSM-III-R Global Assessment of Functioning Scale, which yields a composite rating of a child’s global functioning on a scale ranging from 1 (worst) to 90 (best). Global Assessment of Functioning Scale scores were assigned to each participant on the basis of information obtained in the diagnostic interview; scores were also reviewed by the committee. Socioeconomic status was established by using categories delineated by Hollingshead and was available for 1,261 participants (oppositional defiant disorder alone: N=512, oppositional defiant disorder plus conduct disorder: N=218, psychiatric comparison group: N=531).
Social functioning was assessed by using the Social Adjustment Inventory for Children and Adolescents (19). This 76-item instrument consists of 12 subscales that assess social difficulties at school and in interactions with peers, siblings, and parents. (For the present study, two subscales related to interactions with the opposite sex were excluded from data analyses.) The Social Adjustment Inventory for Children and Adolescents was administered in interview format to mothers, who rated each item on a 4-point scale. Using the same scale, interviewers then assigned a global rating score for each subscale to summarize maternal ratings on individual item scores within each content area. A total score was then calculated as the arithmetic mean of all subscale scores. Previous studies have provided evidence of the concurrent and discriminant validity of this instrument (19–22) as well as its interrater reliability and internal consistency (23). Data from the Social Adjustment Inventory for Children and Adolescents were available for 715 participants (oppositional defiant disorder alone: N=297, oppositional defiant disorder plus conduct disorder: N=111, psychiatric comparison group: N=307).
Mothers also provided information regarding family interactions through completion of the relationship dimensions of the Family Environment Scale (24). The relationship dimensions consist of 27 true/false items that assess the quality of interpersonal relationships among family members in three domains: cohesion (the degree of commitment, help, and support provided by family members to one another), expressiveness (the extent to which family members are encouraged to act openly and express feelings directly), and conflict (the amount of openly expressed anger, aggression, and conflict among family members). Data from the Family Environment Scale were available for 668 participants (oppositional defiant disorder alone: N=283, oppositional defiant disorder plus conduct disorder: N=106, psychiatric comparison group: N=279). Statistical significance was defined at the 0.01 level.
Results
Demographic and Clinical Characteristics
As shown in Table 1, the three groups were not significantly different in age but were different in terms of socioeconomic status. Pairwise comparisons showed that the socioeconomic status of both oppositional defiant disorder groups was significantly lower than that of the psychiatric comparison subjects, and the socioeconomic status of youth with oppositional defiant disorder and conduct disorder was significantly lower than that of those with oppositional defiant disorder alone. Male representation among youth with oppositional defiant disorder and conduct disorder was somewhat greater than among youth with oppositional defiant disorder alone and was significantly greater than that of the psychiatric comparison subjects. (In view of these findings, socioeconomic status and gender were included as covariates in all analyses examining differences among the three groups.) While rates of repeated grade and remedial assistance did not differ among the three groups, the likelihood of placement in special classes did. Pairwise comparisons revealed that youth in both oppositional defiant disorder groups had a significantly greater likelihood of placement in special classes at school than did psychiatric comparison subjects, and youth with oppositional defiant disorder and conduct disorder also had significantly higher rates of such placements than did youth with oppositional defiant disorder alone.
As shown in Figure 1, oppositional defiant disorder youth with or without conduct disorder had significantly higher rates of attention deficit hyperactivity disorder (ADHD), major depression, bipolar disorder, and multiple anxiety disorders than did psychiatric comparison subjects. In addition, youth with oppositional defiant disorder and conduct disorder had significantly higher rates of severe major depression and bipolar disorder than did youth with oppositional defiant disorder alone; no other significant differences were found. Substantial rates of oppositional defiant disorder, either alone or with comorbid conduct disorder, were found within other psychiatric disorders as well (Figure 2).
With regard to adaptive and social functioning, oppositional defiant disorder youth with or without conduct disorder evidenced significantly greater impairment (relative to those with neither disorder) on the Global Assessment of Functioning Scale and the Social Adjustment Inventory for Children and Adolescents total score (Table 1) as well as in almost all domains of social functioning (Figure 3). Oppositional defiant disorder youth with conduct disorder had significantly lower scores than did those without conduct disorder on the Global Assessment of Functioning Scale and on the Social Adjustment Inventory for Children and Adolescents subscales that assessed social difficulties at school, spare-time problems, and problems in interactions with peers, siblings, and parents. Oppositional defiant disorder subjects with or without conduct disorder exhibited significantly greater impairment in family functioning than did subjects with neither disorder on the cohesion and conflict domains of the Family Environment Scale (Figure 4). No differences emerged between youth with oppositional defiant disorder alone and those with comorbid conduct disorder in any domains of family functioning.
Contribution of Oppositional Defiant Disorder, Comorbid Conditions, and Demographic Characteristics to Social and Family Functioning
We next sought to disentangle the high rates of comorbidity within oppositional defiant disorder and its overlap with conduct disorder by examining the association between oppositional defiant disorder and both social impairment and family dysfunction while we controlled for conduct disorder and other disorders. Toward this end, we used linear and logistic regression models to determine the association between oppositional defiant disorder and social and family outcomes after we controlled for conduct disorder, ADHD, bipolar disorder, major depression, multiple anxiety disorders, language impairment, pervasive developmental disorder, Tourette’s disorder, socioeconomic status, gender, and age. We first examined these variables with regard to global indices of social functioning (the Social Adjustment Inventory for Children and Adolescents total score) and family functioning (the combined sum of the three Family Environment Scale subscales, with scaling on the conflict subscale reversed [lower scores now representing poorer functioning] so as to achieve uniformity with the other two subscales). As seen in Table 2 and Table 3, both overall models were significant. For the Social Adjustment Inventory for Children and Adolescents total score, oppositional defiant disorder, conduct disorder, language impairment, pervasive developmental disorder, and age emerged as significant predictors; major depression was a borderline significant predictor. For the Family Environment Scale total score, oppositional defiant disorder, socioeconomic status, and age emerged as significant predictors and multiple anxiety disorders emerged as a borderline significant predictor.
To determine whether specific dimensions of family and social functioning were accounted for by unique predictors, we entered the same predictors into separate regression models for the four problem subscales of the Social Adjustment Inventory for Children and Adolescents (Table 2) and the three Family Environment Scale subscales (Table 3). All models were significant. Oppositional defiant disorder, ADHD, and major depression emerged as significant predictors of social problems at school, with conduct disorder and age emerging as borderline significant predictors. On the problems with peers subscale, oppositional defiant disorder, conduct disorder, language impairment, and pervasive developmental disorder emerged as significant predictors, with socioeconomic status emerging as a borderline significant predictor. On the problems with siblings subscale, oppositional defiant disorder and conduct disorder were the only significant predictors; bipolar disorder was a borderline significant predictor. Finally, on the problems with parents subscale, oppositional defiant disorder and conduct disorder were the only significant predictors, with ADHD, bipolar disorder, and major depression emerging as borderline significant predictors (Table 2). For the Family Environment Scale subscales (Table 3), oppositional defiant disorder emerged as the only significant predictor of family conflict, and oppositional defiant disorder, age, and socioeconomic status were the only significant predictors of family cohesion. Socioeconomic status and multiple anxiety disorders emerged as significant predictors on the family expressiveness subscale, with oppositional defiant disorder and bipolar disorder emerging as borderline significant predictors.
Discussion
In a carefully diagnosed, large, well-defined group of clinically referred youth, we found that the diagnosis of oppositional defiant disorder was associated with significantly higher rates of comorbid disorders, greater social impairment, and greater family dysfunction when compared with a group of clinically referred youth with neither oppositional defiant disorder nor conduct disorder. Specifically, we found that youth with oppositional defiant disorder, either with or without conduct disorder, had significantly lower Global Assessment of Functioning Scale scores. In addition, families of oppositional defiant disorder youth with or without conduct disorder were characterized by significantly poorer cohesion and significantly higher conflict. Finally, the significantly impaired social interactions of youth with oppositional defiant disorder cut across all domains of social functioning (i.e., school, parents, siblings, and peers). Oppositional defiant disorder was a consistently significant correlate of these adverse outcomes after we controlled for comorbid conditions, including conduct disorder. Significant differences between youth with oppositional defiant disorder alone or with comorbid conduct disorder emerged primarily in the social domain and in rates of mood disorders. These results support not only the validity of the oppositional defiant disorder diagnosis as a meaningful clinical entity but also the extremely detrimental effects of this disorder on multiple domains of functioning in children and adolescents.
By creating two oppositional defiant disorder groups (i.e., subjects with oppositional defiant disorder alone and those with comorbid conduct disorder) as well as a psychiatric comparison group of subjects with neither disorder, our analyses permitted the examination of the effects of oppositional defiant disorder outside the context of conduct disorder. Clearly, conduct disorder is a serious psychiatric disorder associated with high levels of morbidity. However, the common practice of combining data from oppositional defiant disorder and conduct disorder groups has obscured the unique correlates and clinical importance of oppositional defiant disorder beyond its association with conduct disorder. Prior studies of children with “conduct problems” have provided valuable information but have not clarified the clinical significance of oppositional defiant disorder in the absence of conduct disorder. The findings reported here show that oppositional defiant disorder contributes to substantial impairment in multiple domains even outside the context of conduct disorder and that this impairment is not accounted for by other psychiatric disorders. Thus, these findings highlight the high clinical and public health relevance of oppositional defiant disorder independent of its association with conduct disorder and underscore the need for further clinical and scientific effort aimed at understanding and ameliorating the adverse outcomes to which this disorder contributes.
The finding that oppositional defiant disorder is frequently comorbid with ADHD fits with previous research demonstrating significant overlap between the two disorders. Also consistent with prior research, however, is the finding that a meaningful percentage of children with ADHD did not have comorbid oppositional defiant disorder. Our findings documenting an equally large overlap between oppositional defiant disorder and mood and anxiety disorders are also congruent with the limited extant literature. Converging lines of evidence have also suggested that childhood “internalizing” (e.g., mood and anxiety) disorders frequently overlap with oppositional defiant disorder (11, 25–29). However, these associations between oppositional defiant disorder and other psychiatric disorders have typically been found in research in which the effects of comorbid conduct disorder were not isolated.
Our results suggest that oppositional defiant disorder is a highly heterogeneous disorder with varied presentations, possibly emanating from disparate and complex pathways. These findings have important scientific ramifications as we seek to identify those oppositional defiant disorder children at greatest risk for developing more severe difficulties (11) and further clarify familial transmission of the disorder (30). Such findings also have major clinical relevance, since a view of oppositional defiant disorder as a heterogeneous disorder has the potential to heighten awareness of the diverse factors that may contribute to the development of the disorder and raises the possibility that different manifestations of the disorder might require different approaches to treatment. For example, since treatment approaches for ADHD and disorders of mood and anxiety differ, their recognition in children with oppositional defiant disorder may allow clinicians a broader choice of therapeutic options (9). There is suggestion in the literature that treating symptoms coinciding with oppositional defiant disorder can produce improvements in behaviors related to oppositional defiant disorder as well. For example, in 1999, the Collaborative Multimodal Treatment Study of ADHD (31) reported that stimulant medication produced significant improvements in both ADHD-related and oppositional behaviors. Other research has provided evidence for the efficacy of mood-enhancing medication in children whose oppositional behavior is associated with obsessiveness and irritability (26). Clearly, characterization and treatment of oppositional defiant disorder on the basis of comorbid presentations is an area worthy of significant research attention.
The high prevalence of oppositional defiant disorder within other clinical populations also deserves additional attention. It has been argued that each of the disorders comorbid with oppositional defiant disorder (e.g., ADHD, mood disorders, anxiety disorders, language impairments) may stem from or contribute to impairments in the domains of affective modulation and self-regulation (9). Developmental psychologists have long underscored the importance of these two factors with regard to a child’s capacity to adapt to environmental changes or demands and internalize standards of conduct (32–35). The skill of compliance—defined as the capacity to defer or delay one’s own goals in response to the imposed goals or standards of an authority figure—can be considered one of many developmental expressions of a young child’s evolving capacities in the domains of adaptation, internalization, self-regulation, and affective modulation (36). The capacity for compliance is thought to develop in a sequence that includes, in infancy, managing the discomfort that can accompany hunger, cold, fatigue, and pain; modulating arousal while remaining engaged with the environment; and communicating with caregivers to signal that assistance is needed (35). With the development of language, more sophisticated mechanisms for self-regulation and affective modulation develop, as children learn to use language to label and communicate their thoughts and feelings, develop cognitive schemas related to cause-and-effect, and generate and internalize strategies aimed at facilitating advantageous interactions with the environment (35). It has been further argued that interventions focused solely on improving a child’s compliance neither target nor effectively treat impairments in self-regulation and affective modulation and that medical and nonmedical interventions aimed at enhancing problem-solving skills, flexibility, and frustration tolerance might be better suited to the needs of many youth with oppositional defiant disorder (9).
These findings must be interpreted in terms of their clinical significance. In the general population, prevalence rates of the disorders examined in this study tend to be quite low (i.e., below 6%) (37, 38). Given the very high rates of comorbid disorders in subjects with oppositional defiant disorder, it seems clear that, compared with the general population, oppositional defiant disorder confers clinically significant risk for psychiatric comorbidity. With psychiatric comparison subjects as the reference group, clinically significant differences were most striking within the domain of mood disorders, where oppositional defiant disorder doubled the risk of both severe major depression and bipolar disorder. Oppositional defiant disorder also appears to confer clinically significant risk for social dysfunction compared with both nonclinical populations and psychiatric comparison subjects. Normative data for the Social Adjustment Inventory for Children and Adolescents (19) suggest that scores for youth with oppositional defiant disorder fall greater than two standard deviations below the mean on most subscales and the total score relative to nonclinical populations. The current data revealed that youth with oppositional defiant disorder fell between one-half and one standard deviation below the mean of psychiatric comparison subjects. With regard to family functioning, normative data for the Family Environment Scale (24) suggest that youth with oppositional defiant disorder fall between one-half and one standard deviation below the mean for nonclinical populations of children, especially in the domains of conflict and cohesion.
These findings must also be understood in the context of methodological limitations. Cross-sectional data such as those we have reported do not permit examination of longitudinal patterns. For example, given the demonstrated sequential relationship between oppositional defiant disorder and conduct disorder, it is possible that some of the youth with oppositional defiant disorder alone in our study group would subsequently develop conduct disorder. However, we have previously shown that subsequent diagnoses of conduct disorder in youth with oppositional defiant disorder are quite low beyond age 6 (11). Given the mean age of our study group (10.8 years), we would anticipate that very few of the youth with oppositional defiant disorder alone in this data set would subsequently develop conduct disorder.
Our subjects were clinically referred and consisted primarily of Caucasian youth; thus, our results may not generalize to other groups of oppositional defiant disorder children. For example, our finding that oppositional defiant disorder is associated with significant comorbidity differs dramatically from one recent study (13), presumably because of important study group differences (subjects in the current study were both significantly older and clinically referred). Further, our data were obtained predominantly from mothers. While multiple informants provide a broader examination of a child’s functioning, in prior studies we have shown significant overlap between information gathered from mothers and other reporters (39). Finally, the findings we have described are cross-sectional; further study is required to examine the long-term sequelae of oppositional defiant disorder.
Despite these limitations, in a carefully assessed group of clinically referred youth, children with oppositional defiant disorder evidenced significantly higher rates of comorbidity and significantly greater impairment in adaptive, social, and family functioning than did children without oppositional defiant disorder, and oppositional defiant disorder was a significant correlate of such impairment even after we controlled for a wide range of comorbid conditions and demographic characteristics. These results support the validity of oppositional defiant disorder as a meaningful clinical entity independent of conduct disorder and warrant additional study of children and adolescents who are so diagnosed and a broadened examination of diverse approaches to treatment aimed at ameliorating their difficulties.
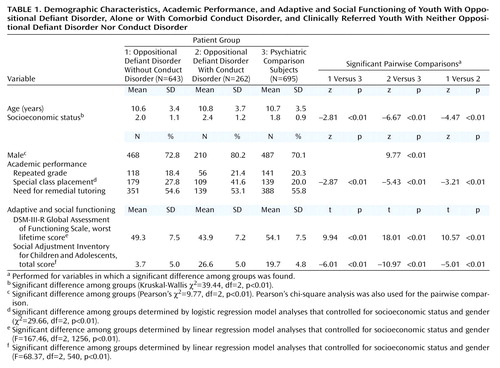 |
 |
 |
Received Sept. 6, 2000; revisions received Jan. 8 and June 15, 2001, and Feb. 5, 2002; accepted March 5, 2002. From the Clinical and Research Program in Pediatric Psychopharmacology, Massachusetts General Hospital; and the Department of Psychiatry, Harvard Medical School, Boston. Address reprint requests to Dr. Greene, Clinical and Research Program in Pediatric Psychopharmacology, Massachusetts General Hospital, ACC-725, Boston, MA 02114; [email protected] (e-mail).
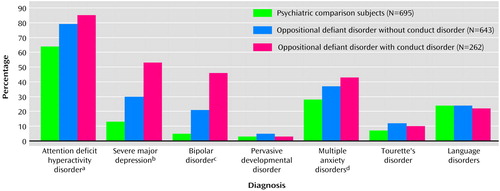
Figure 1. Psychiatric Diagnoses in Youth With Oppositional Defiant Disorder, Alone or With Comorbid Conduct Disorder, and Clinically Referred Youth With Neither Oppositional Defiant Disorder Nor Conduct Disorder
aSignificant difference among groups determined by logistic regression analysis that controlled for socioeconomic status and gender (χ2=40.22, df=2, p<0.01). Pairwise comparisons revealed that relative to the psychiatric comparison subjects, higher rates were seen in youth with oppositional defiant disorder alone (z=–5.14, p<0.01) or with comorbid conduct disorder (z=–4.98, p<0.01).
bSignificant difference among groups determined by logistic regression analysis that controlled for socioeconomic status and gender (χ2=122.46, df=2, p<0.01). Pairwise comparisons revealed that relative to the psychiatric comparison subjects, higher rates were seen in youth with oppositional defiant disorder alone (z=–6.01, p<0.01) or with comorbid conduct disorder (z=–11.06, p<0.01). The rates of the two oppositional defiant disorder groups also significantly differed (z=–6.77, p<0.01).
cSignificant difference among groups determined by logistic regression analysis that controlled for socioeconomic status and gender (χ2=128.60, df=2, p<0.01). Pairwise comparisons revealed that relative to the psychiatric comparison subjects, higher rates were seen in youth with oppositional defiant disorder alone (z=–6.20, p<0.01) or with comorbid conduct disorder (z=–11.12, p<0.01). The rates of the two oppositional defiant disorder groups also significantly differed (z=–7.07, p<0.01).
dSignificant difference among groups determined by logistic regression analysis that controlled for socioeconomic status and gender (χ2=21.08, df=2, p<0.01). Pairwise comparisons revealed that relative to the psychiatric comparison subjects, higher rates were seen in youth with oppositional defiant disorder alone (z=–2.93, p<0.01) or with comorbid conduct disorder (z=–4.45, p<0.01).
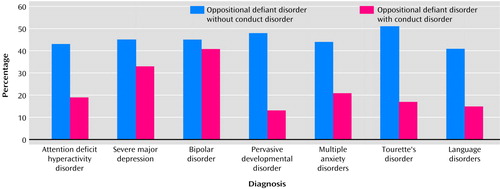
Figure 2. Oppositional Defiant Disorder, Alone or With Comorbid Conduct Disorder, in Clinically Referred Youth With Other Psychiatric Diagnoses
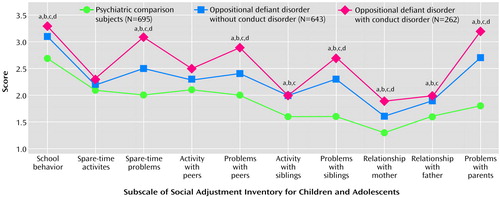
Figure 3. Social Functioning in Youth With Oppositional Defiant Disorder, Alone or With Comorbid Conduct Disorder, and Clinically Referred Youth With Neither Oppositional Defiant Disorder Nor Conduct Disorder
aSignificant difference among groups determined by linear regression analysis that controlled for socioeconomic status and gender (F=10.28–120.51, df=2, 457–540, p<0.01).
bPairwise comparisons revealed a significant difference (t test, p<0.01) between youth with oppositional defiant disorder alone and psychiatric comparison subjects.
cPairwise comparisons revealed a significant difference (t test, p<0.01) between oppositional defiant disorder youth with comorbid conduct disorder and psychiatric comparison subjects.
dPairwise comparisons revealed a significant difference (t test, p<0.01) between the two oppositional defiant disorder groups.
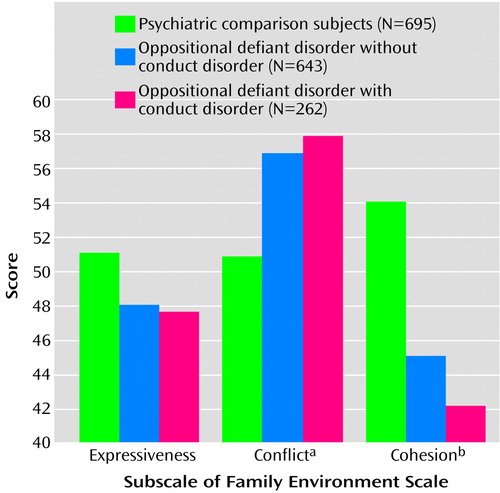
Figure 4. Family Functioning in Youth With Oppositional Defiant Disorder, Alone or With Comorbid Conduct Disorder, and Clinically Referred Youth With Neither Oppositional Defiant Disorder Nor Conduct Disorder
aSignificant difference among groups determined by linear regression analysis that controlled for socioeconomic status and gender (F=14.99, df=2, 500, p<0.01). Pairwise comparisons revealed that relative to the psychiatric comparison subjects, higher scores were seen in youth with oppositional defiant disorder alone (t=–4.97, df=413, p<0.01) or with comorbid conduct disorder (t=–4.10, df=286, p<0.01).
bSignificant difference among groups determined by linear regression analysis that controlled for socioeconomic status and gender (F=12.68, df=2, 497, p<0.01). Pairwise comparisons revealed that relative to the psychiatric comparison subjects, lower scores were seen in youth with oppositional defiant disorder alone (t=4.13, df=414, p<0.01) or with comorbid conduct disorder (t=4.30, df=289, p<0.01).
1. Anderson KE, Lytton H, Romney DM: Mothers’ interactions with normal and conduct-disordered boys: who affects whom? Dev Psychol 1986; 22:604-609Crossref, Google Scholar
2. Dumas JE, LaFreniere PJ: Mother-child relationships as sources of support or stress: a comparison of competent, average, aggressive, and anxious dyads. Child Dev 1993; 64:1732-1754Crossref, Medline, Google Scholar
3. Dumas JE, LaFreniere PJ, Serketich WJ: “Balance of power”: a transactional analysis of control in mother-child dyads involving socially competent, aggressive, and anxious children. J Abnorm Psychol 1995; 104:104-113Crossref, Medline, Google Scholar
4. Lytton H: Child and parent effects on boys’ conduct disorder: a reinterpretation. Dev Psychol 1990; 26:683-697Crossref, Google Scholar
5. Rey JM, Bashir MR, Schwarz M, Richards IN, Plapp JM, Stewart GW: Oppositional disorder: fact or fiction? J Am Acad Child Adolesc Psychiatry 1988; 27:157-162Crossref, Medline, Google Scholar
6. Schachar RJ, Wachsmuth R: Oppositional disorder in children: a validation study comparing conduct disorder, oppositional disorder and normal control children. J Child Psychol Psychiatry 1990; 31:1089-1102Crossref, Medline, Google Scholar
7. Stormschak E, Speltz M, DeKlyen M, Greenberg M: Family interactions during clinical intake: a comparison of families of normal or disruptive boys. J Abnorm Child Psychol 1997; 25:345-357Crossref, Medline, Google Scholar
8. Cohen P, Kasen S, Brook JS, Struening EL: Diagnostic predictors of treatment patterns in a cohort of adolescents. J Am Acad Child Adolesc Psychiatry 1991; 30:989-993Crossref, Medline, Google Scholar
9. Greene RW, Doyle AE: Toward a transactional conceptualization of oppositional defiant disorder: implications for treatment and assessment. Clin Child Fam Psychol Rev 1999; 2:129-148Crossref, Medline, Google Scholar
10. Kuhne M, Schachar R, Tannock R: Impact of comorbid oppositional or conduct problems on attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 1997; 36:1715-1725Crossref, Medline, Google Scholar
11. Biederman J, Faraone SV, Milberger S, Jetton JG, Chen L, Mick E, Greene RW, Russell RL: Is childhood oppositional defiant disorder a precursor to adolescent conduct disorder? findings from a four-year follow-up study of children with ADHD. J Am Acad Child Adolesc Psychiatry 1996; 35:1193-1204Crossref, Medline, Google Scholar
12. Hinshaw SP, Lahey BB, Hart EL: Issues of taxonomy and comorbidity in the development of conduct disorder. Dev Psychopathol 1993; 5:31-49Crossref, Google Scholar
13. Speltz ML, McClellan J, DeKlyen M, Jones K: Preschool boys with oppositional defiant disorder: clinical presentation and diagnostic change. J Am Acad Child Adolesc Psychiatry 1999; 38:838-845Crossref, Medline, Google Scholar
14. Lahey BB, Loeber R: Framework for a developmental model of oppositional defiant disorder and conduct disorder, in Disruptive Behavior Disorders in Childhood. Edited by Routh DK. New York, Plenum, 1994, pp 139-180Google Scholar
15. August GJ, Realmuto GM, Joyce T, Hektner JM: Persistence and desistance of oppositional defiant disorder in a community sample of children with ADHD. J Am Acad Child Adolesc Psychiatry 1999; 38:1262-1270Crossref, Medline, Google Scholar
16. Orvaschel H, Puig-Antich J: Schedule for Affective Disorders and Schizophrenia for School-Age Children—Epidemiologic Version (K-SADS-E), 4th revision. Fort Lauderdale, Fla, Nova University, Center for Psychological Studies, 1987Google Scholar
17. Weissman MM, Gershon ES, Kidd KK, Prusoff BA, Leckman JF, Dibble E, Hamovit J, Thompson WD, Pauls DL, Guroff JJ: Psychiatric disorders in the relatives of probands with affective disorders. Arch Gen Psychiatry 1984; 41:13-21Crossref, Medline, Google Scholar
18. Biederman J, Rosenbaum JF, Hirshfeld DR, Faraone SV, Bolduc EA, Gersten M, Meminger SR, Kagan J, Snidman N, Reznick JS: Psychiatric correlates of behavioral inhibition in young children of parents with and without psychiatric disorders. Arch Gen Psychiatry 1990; 53:437-446Crossref, Google Scholar
19. John K, Gammon GD, Prusoff BA, Warner V: The Social Adjustment Inventory for Children and Adolescents (SAICA): testing of a new semistructured interview. J Am Acad Child Adolesc Psychiatry 1987; 26:898-911Crossref, Medline, Google Scholar
20. Biederman J, Faraone SV, Chen W: Social Adjustment Inventory for Children and Adolescents: concurrent validity in ADHD children. J Am Acad Child Adolesc Psychiatry 1993; 32:1059-1064Crossref, Medline, Google Scholar
21. Greene RW, Biederman J, Faraone SV, Ouellette CA, Penn C, Griffin S: Toward a new psychometric definition of social disability in children with attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 1996; 35:571-578Crossref, Medline, Google Scholar
22. Greene RW, Biederman J, Faraone SV, Wilens TE, Mick E, Blier HK: Further validation of social impairment as a predictor of substance use disorders: findings from a sample of siblings of boys with and without ADHD. J Clin Child Psychol 1999; 28:349-354Crossref, Medline, Google Scholar
23. Greene RW, Biederman J, Faraone SV, Sienna J, Garcia-Jetton J: Adolescent outcome of boys with attention-deficit/hyperactivity disorder and social disability: results from a 4-year longitudinal follow-up study. J Consult Clin Psychol 1997; 65:758-767Crossref, Medline, Google Scholar
24. Moos RH, Moos BS: Manual for the Family Environment Scale. Palo Alto, Calif, Consulting Psychologists Press, 1974Google Scholar
25. Angold A, Costello EJ: Depressive comorbidity in children and adolescents: empirical, theoretical, and methodological issues. Am J Psychiatry 1993; 150:1779-1791Link, Google Scholar
26. Garland EJ, Weiss M: Case study: obsessive difficult temperament and its response to serotonergic medication. J Am Acad Child Adolesc Psychiatry 1996; 35:916-920Crossref, Medline, Google Scholar
27. Geller B, Luby J: Child and adolescent bipolar disorder: review of the past 10 years. J Am Acad Child Adolesc Psychiatry 1997; 36:1-9Crossref, Medline, Google Scholar
28. Wozniak J, Biederman J: A pharmacological approach to the quagmire of comorbidity in juvenile mania. J Am Acad Child Adolesc Psychiatry 1996; 35:826-828Crossref, Medline, Google Scholar
29. Wozniak J, Biederman J, Kiely K, Ablon JS, Faraone SV, Mundy E, Mennin D: Mania-like symptoms suggestive of childhood-onset bipolar disorder in clinically referred children. J Am Acad Child Adolesc Psychiatry 1995; 34:867-876Crossref, Medline, Google Scholar
30. Faraone SV, Biederman J, Keenan K, Tsuang MT: Separation of DSM-III attention deficit disorder and conduct disorder: evidence from a family-genetic study of American child psychiatric patients. Psychol Med 1991; 21:109-121Crossref, Medline, Google Scholar
31. MTA Cooperative Group: A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 1999; 56:1073-1086Crossref, Medline, Google Scholar
32. Crockenberg S, Litman C: Autonomy as competence in two-year olds: maternal correlates of child defiance, compliance, and self-assertion. Dev Psychol 1990; 26:961-971Crossref, Google Scholar
33. Kochanska G: Toward a synthesis of parental socialization and child temperament in early development of conscience. Child Dev 1993; 64:325-347Crossref, Google Scholar
34. Kochanska G: Children’s temperament, mothers’ discipline, and security of attachment: multiple pathways to emerging internalization. Child Dev 1995; 66:597-615Crossref, Google Scholar
35. Kopp CB: Regulation of distress and negative emotions: a developmental view. Dev Psychol 1989; 25:343-354Crossref, Google Scholar
36. Stifter CA, Spinrad TL, Braungart-Rieker JM: Toward a developmental model of child compliance: the role of emotion regulation in infancy. Child Dev 1999; 70:21-32Crossref, Medline, Google Scholar
37. Rutter M, Cox A, Tupling C, Berger M, Yule M: Attainment and adjustment in two geographical areas, I: the prevalence of psychiatric disorder. Br J Psychiatry 1975; 126:493-509Crossref, Medline, Google Scholar
38. Costello EJ, Angold A, Burns BJ, Stangl DK, Tweed DL, Erkanli A, Worthman CM: The Great Smoky Mountains study of youth: goals, design, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psychiatry 1996; 53:1129-1136Crossref, Medline, Google Scholar
39. Biederman J, Faraone S, Mick E, Moore P, Lelon E: Child Behavior Checklist findings further support comorbidity between ADHD and major depression in a referred sample. J Am Acad Child Adolesc Psychiatry 1996; 35:734-742Crossref, Medline, Google Scholar



