Toward a Comprehensive Developmental Model for Major Depression in Women
Abstract
OBJECTIVE: Major depression is a multifactorial disorder with many etiologic variables that are interrelated through developmental pathways. The authors used structural equation modeling to generate a developmental model for the etiology of major depression in women. METHOD: Data from 1,942 adult female twins, interviewed up to four times over a 9-year period, were used to construct a developmental model to predict depressive episodes in the year before the most recent interview. Eighteen risk factors in five developmental tiers were considered: 1) childhood (genetic risk, disturbed family environment, childhood sexual abuse, and childhood parental loss), 2) early adolescence (neuroticism, self-esteem, and early-onset anxiety and conduct disorder), 3) late adolescence (educational attainment, lifetime traumas, social support, and substance misuse), 4) adulthood (history of divorce and past history of major depression), and 5) the last year (marital problems, difficulties, and stressful life events). RESULTS: The best fitting model included six correlations and 64 paths, provided an excellent fit to the data, and explained 52% of the variance in liability to episodes of major depression. The findings suggest that the development of risk for major depression in women results from three broad pathways reflecting internalizing symptoms, externalizing symptoms, and psychosocial adversity. CONCLUSIONS: Major depression is an etiologically complex disorder, the full understanding of which will require consideration of a broad array of risk factors from multiple domains. These results, while plausible, should be treated with caution because of problems with causal inference, retrospective recall bias, and the limitations of a purely additive statistical model.
Major depression is a prototypical multifactorial disorder. An individual’s probability of suffering from an episode of major depression is affected by many factors including predisposing genetic influences (1–3), exposure to a disturbed family environment (4, 5), childhood sexual abuse (6), premature parental loss (7), predisposing personality traits (8–10), early-onset anxiety or conduct disorder (11–13), dysfunctional self-schemata (14), exposure to traumatic events and major adversities (15–18), low social support (19), substance misuse (12), marital difficulties (20), a prior history of major depression (21–23), and recent stressful life events and difficulties (24, 25).
Several influential reviews have emphasized the importance of combining these diverse risk factor domains into an integrated etiologic model (e.g., references 26–28). However, few studies have addressed the etiologic complexity that is likely realistic for major depression. Furthermore, an important goal of such models is the elucidation of the developmental pathways through which the risk factors lead to illness (29).
In 1993, we published a preliminary step in this direction that used data from two waves of interviews in our ongoing longitudinal study of female-female twin pairs ascertained from the Virginia Twin Registry (30). We expand here on our previous effort by utilizing improved statistical methods and a broader array of risk factors assessed in two additional waves of personal interviews.
Method
Sample
The data used in this report derive from an ongoing study of Caucasian twin pairs from the Virginia Twin Registry (31, 32)—a population-based register formed from a review of all birth certificates in the Commonwealth of Virginia. Female-female twin pairs born during 1933–1972 were initially ascertained through a questionnaire (termed FFQ) mailed to female twin pairs in the Registry in 1987–1988, the response to which was ~64% (N=2,354). Twins were then interviewed face-to-face in 1988–1989 (FF1 interview), at which time the refusal rate was ~12%. These twins completed three more telephone interviews in 1990–1991 (FF2), 1992–1994 (FF3), and 1995–1997 (FF4), with cooperation rates ranging from 85%–93%. This report is based on data for the 1,942 twins who completed at least two interview waves, including FF4. At the FF4 interview, these subjects were a mean age of 35.8 years (SD=8.2) and had a mean of 14.3 years (SD=2.2) of education. The subjects’ mean time from the FF1 interview to the FF4 interview was 7.1 years (SD=1.6). To assess test-retest reliability, 190 randomly selected twins were reinterviewed a mean of 4.3 weeks (SD=1.5) after their initial interview. In addition, in 1990–1991, at the time of the FF2 interviews, we attempted to interview face-to-face all living biological parents of the twin pairs and succeeded in interviewing 90.2% of those who were alive and traceable (N=1,632).
Outcome Variable
Our goal in this model was to predict episode onset of major depression in the last year. Major depression was treated as a dichotomous variable with an assumed underlying normal liability distribution. In the FF4 interview, all twins were asked about the occurrence, at any time in the last year, of 15 individual symptoms that reflected all elements of criterion A for major depressive episode in DSM-III-R. They were then asked to aggregate these symptoms in time, to report the total number of episodes experienced and to give dates, to the nearest month, for the onset and offset of each episode. For the purposes of this study, we counted the first reported episode that met DSM-III-R criteria for major depression unless there were multiple episodes and the first episode began in the first 2 months of the year before the interview. In that case, we counted the next reported episode.
Model Variables
The selection of variables began with those that had been used in our 1993 study (30), which was based on data collected at FFQ, FF1, and FF2. Several of these variables could be improved with new information obtained in later waves. We had also collected information on several key variables lacking in our earlier model, especially childhood sexual abuse, conduct disorder, and substance misuse. Finally, we included other variables—based on the literature and their availability in our data—to expand the domains examined (e.g., self-esteem to include a “self-concept” variable and early-onset anxiety because of its strong demonstrated link to risk for subsequent major depression [11]).
Our final list included 18 predictor variables that we attempted to order in a tentative developmental sequence. For ease of presentation, we organized these predictors into five “tiers” that roughly approximated five developmental periods: 1) childhood (genetic risk, disturbed family environment, childhood sexual abuse, and childhood parental loss), 2) early adolescence (neuroticism, self-esteem, and early-onset anxiety and conduct disorder), 3) late adolescence (educational attainment, lifetime traumas, social support, and substance misuse), 4) adulthood (history of divorce and past history of major depression), and 5) the last year (marital problems, difficulties, and stressful life events that were either dependent on or independent of the respondent’s own behavior). Of these 18 predictor variables, five were latent and were constructed, by using a measurement model, from other observed variables. We here outline briefly the nature of each variable.
Genetic risk was assessed by a composite measure of the lifetime history of major depression in the co-twin (assessed at FF1, FF3, and FF4) and in the mother and father (assessed in 1990–1991). Parents were divided into those who were affected and those who were unaffected. Co-twins were divided into four categories reflecting the number of interviews at which they received a diagnosis of lifetime major depression. To correct for varying base rates and degree of genetic relatedness in these relatives, we calculated the modified midrank score for the lifetime history of major depression and adjusted these scores to account for the varying genetic correlation with the proband twin (+1.00 for monozygotic co-twins and +0.50 for dizygotic co-twins and parents). We then took the mean of these three scores.
Disturbed family environment was assessed by a measurement model with two manifest continuous variables: mean parental warmth (measured with a modified version of the Parental Bonding Instrument [33, 34]) and mean family environment score (measured by 14 items chosen from the Family Environment Scale [35]). The Parental Bonding Instrument assessed parent-child relationships up to when the twins were age 16. The Family Environment Scale reflected the general emotional tone of the home when the twins “were growing up.” Mean parental warmth was calculated for each twin pair as the mean of the self-report and co-twin report of maternal and paternal warmth (assessed at FF2 and reversed-coded to reflect lack of warmth). For the family environment, we summed the items reflecting family tension (e.g., “family members would get so angry sometimes that they would throw things or hit each other”) and the reverse scoring of items reflecting family integration (e.g., “family members really helped and supported one another”). We then took the mean of the standardized scores of the twin and co-twin assessed at FF2 and the separately standardized score of mother and father assessed in 1990–1991. These four reports were then averaged and restandardized to create a single Family Environmental Scale score for the family.
Childhood sexual abuse was a binary variable based on twin self-report at FF4 (36). Our previous analysis of these data (37) suggested that the increased risk of major depression was associated largely with the more severe forms of abuse. Therefore, in these analyses, twins were assigned a score of 1 if they reported, before the age of 16, an unwanted sexual contact with an older individual that included “touching or fondling your private parts,” “making you touch them in a sexual way,” or “attempting or having sexual intercourse.” Validating the assessments of childhood sexual abuse is inherently problematic, but the agreement between self-report and co-twin-report in this sample far exceeded chance expectation (contingency coefficient=0.50, weighted kappa=0.40, 95% confidence interval [CI]=0.33–0.47).
Parental loss was a binary measure scored 1 if the twin reported that one or both parents left the nuclear home due to death, divorce, or parental separation before the twin was age 17. This was assessed with high reliability (98.5% agreement between twins [38]).
Neuroticism was assessed with a measurement model utilizing the short (12-item) version of the Revised Eysenck Personality Questionnaire (39) and data obtained at FFQ, FF1, and FF3. Because of the resulting J-shaped distribution, it was scored as a five-level ordinal measure.
Self-esteem was assessed with a measurement model based on the full Rosenberg Self-Esteem Scale (40) by using data obtained at FF1 and FF3. Transformation was not needed because of the data’s symmetric distribution. This variable was reversed so that higher scores reflected lower self-esteem.
Early-onset anxiety disorder was a binary variable scored 1 for subjects with an onset before age 18 of panic disorder (data from FF1 or FF2), generalized anxiety disorder (data from FF1 or FF4), or phobia (data from FF1, FF2, or FF4). Panic disorder and generalized anxiety disorder were diagnosed with DSM-III-R criteria, except that we reduced the minimum duration of the latter disorder from 6 months to 1 month. Phobia was defined as the presence of an irrational fear that impacted in an objective and significant way on the behavior of the twin (41).
Conduct disorder was treated as an ordinal variable that reflected the number of DSM-IV conduct disorder criteria met before age 18 that were endorsed at FF4.
The number of years of education was treated as a continuous variable, scored from 1 to 20 at the FF4 interview. It was reverse-scored to reflect low educational attainment.
The measure of lifetime traumas was based on data from FFQ and reflected the number of 10 possible items describing traumatic events that had ever occurred in the respondent’s lifetime, including physical assault, unexpected death of a loved one, and abortion. The distribution was skewed so that this measure was treated as an ordinal variable.
Social support was assessed by using a measurement model with information from the FF1 and FF3 interviews. We summed those dimensions of social support that related most strongly to risk for depression: problems with relatives and church and club attendance (30). This measure, which was scored to reflect lack of social support, was relatively symmetric and was treated as a continuous variable.
Substance misuse was assessed with a measurement model derived from three binary manifest variables: 1) a lifetime diagnosis of DSM-III-R alcohol abuse or dependence assessed at FF3 or FF4, 2) a lifetime diagnosis of DSM-IV drug abuse or dependence at FF4 (separate assessments were made for cannabis, sedatives, stimulants, cocaine, opiates, hallucinogens, inhalants, and “over-the-counter” medications), and 3) lifetime nicotine dependence, assessed by a score of ≥7 on the Fagerstrom Tolerance Questionnaire (42) for the period of heaviest smoking, by using data collected at FF3 or FF4.
Ever divorced was a binary measure scored 1 for women who reported a lifetime history of divorce at the FF1, FF3, or FF4 interviews. Never having been married was scored 0.
Prior history of major depression was a binary measure reflecting the presence or absence of a lifetime history of DSM-III-R major depression prior to 1 year before the FF1 interview (at the mean age of 28 years).
Marital problems in the last year was constructed as a three-level ordinal variable. In a piecewise regression that used seven items assessing the level of marital satisfaction in the last year from the Social Interaction Scale (43), an elevated risk for onset of major depression was associated with levels of satisfaction in the lower 20%. Those who were unmarried or not living with a partner at FF4 were assigned an intermediate risk. Thus, the variable was constructed as follows: 0=upper 80% of marital satisfaction, 1=unmarried, and 2=lower 20% of marital satisfaction.
Difficulities in the last year, dependent stressful life events, and independent stressful life events were assessed by using our stressful life event measures. In the FF4 interview, each twin was systematically asked about the occurrence, at any time in the preceding 12 months, of 11 “personal” events (i.e., events occurring primarily to the informant): assault, divorce/separation, major financial problem, serious housing problems, serious illness or injury, job loss, legal problems, loss of confidant, serious marital problems, robbery, and serious difficulties at work. We also assessed four classes of “network” events: 1) serious trouble getting along with an individual in the network, 2) a serious personal crisis of someone in the network, 3) death of an individual in the network, and 4) serious illness of someone in the network. These events were presented separately for different relationships in their network (e.g., parents, siblings, offspring, etc.). Each reported event was dated to the nearest month with high interrater reliability (44, 45). The dependence of a stressful life event, reflecting the probability that the respondent’s own behavior contributed to the stressful life event, was rated on a 4-point scale: clearly independent, probably independent, probably dependent, and clearly dependent, with demonstrated good interrater reliability (46). In these analyses, we dichotomized stressful life events into those clearly or probably independent versus those clearly or probably dependent.
For an individual with a reported onset of major depression in the year preceding her FF4 interview, we counted, separately, the number of dependent and independent stressful life events occurring in that month and the 2 preceding months—the time period associated with an increased risk of depressive onset in this sample (45). If the only episode occurred in the first or second month of the year (N=14), the number of stressful life events reported was multiplied, respectively, by 3 or 1.5. For individuals reporting no depressive onset, a random 3-month window was used to assess the occurrence of stressful life events. The number of stressful life events was treated as an ordinal variable. Difficulties in the last year reflected the sum of all stressful life events reported at other times during the year before the FF4 interview.
Statistical Methods
Our structural equation model consisted of two parts: 1) a measurement model that consisted of factor loadings for the observed variables that index the five latent variables and 2) a structural model that consisted of path and correlation coefficients connecting the five latent and the 14 observed variables of the model proper. Model fitting was done by using Mplus, version 2 (47), because of its ability to combine categorical, ordinal, and continuous data. The fit function was weighted least squares.
As in most longitudinal studies, missing data were a major problem. Excluding data from all subjects for whom one or more data points were missing would have resulted in unacceptable sample shrinkage. Therefore, the raw data was first put through multiple imputation by using IVEware (48), which utilizes a multivariate sequential regression approach encompassing linear regression for continuous variables, Poisson regression for count variables (e.g., numbers of stressful life events, symptoms of conduct disorder), and logistic regression for ordinal and binary variables (49). Five imputed data sets were created and then combined for analysis in Mplus, each being treated as one group in a multigroup analysis. The measurement model was not constrained across groups, and we did not attempt to simplify it in any way.
For the structural model, we began with a fully saturated model and used a combination of four approaches to produce a model with the optimal balance of explanatory power and parsimony. First, observing the significance levels of individual paths, we fixed sets of paths to zero when the associated z value was <1.96. Second, because our sample size was so large, some paths that remained significant were, in our judgment, too small to be meaningful. Therefore, our second step was to set all paths to zero with a value of <0.05, regardless of z value. In our third step, we further “trimmed” our model by setting paths to zero and looking for those where the increase in the model chi-square value was less than 3.84. As a last check, taking final results from an earlier iteration of the model, we added and subtracted a number of paths that were marginal by significance and/or magnitude to see if we could arrive at a better overall fit and indeed produced a modest improvement in fit and explanatory power.
We utilized three fit indices that reflect, in different ways, the success of the model in balancing explanatory power and parsimony: the Tucker-Lewis index (50), the comparative fit index (51), and the root mean square error of approximation (52). For the Tucker-Lewis index and comparative fit index, values between 0.90 and 0.95 are considered acceptable and values ≥0.95 as good. For the root mean square error of approximation, good models have values ≤0.05, while values >0.10 are considered poor.
Results
Model Fitting
Of the 1,942 female twins who participated in the fourth interview wave, 176 (9.1%) reported a depressive episode meeting DSM-III-R criteria in the last year. The best fitting model predicting the occurrence of these episodes (fit to five replicates) produced a chi-square of 5,074.4 with 1,603 degrees of freedom. This model, which accounted for 52.1% of the variance in liability to major depression in the last year, produced the following fit indices: comparative fit index=0.951, Tucker-Lewis index=0.950, and root mean square error of approximation=0.033.
Parameter Estimates
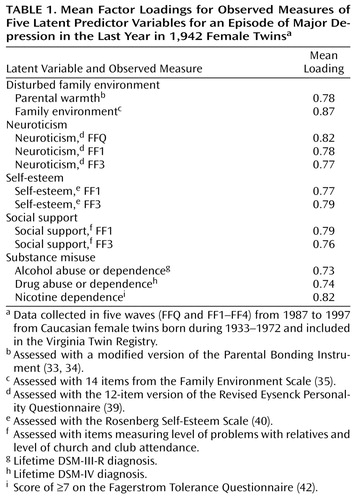
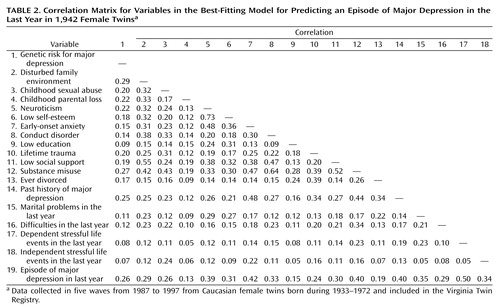
As seen in Table 1, the loadings of the different manifest measures on each of the five latent variables were similar, ranging from 0.73 to 0.87. The parameter estimates of the best-fit structural model are depicted in Figure 1, and the expected correlations among the 19 variables are shown in Table 2. We review the results of this model one variable at a time. In this model, the predicted path coefficients reflect the unique relationship between variables adjusting for all the other possible relationships through other parameters in the model.
Childhood Risk Factors
Substantial interfactor correlations were seen between the four childhood risk factors. In particular, high genetic risk for major depression was associated with increased levels of disturbed family environment, childhood sexual abuse, and childhood parental loss.
As seen in Figure 2, high genetic risk for major depression was uniquely predictive of elevated levels of neuroticism—a key “temperamental” risk factor for later depression—substance misuse, and exposure to lifetime traumas and divorce. The level of genetic risk for major depression also uniquely predicted both a past history of major depression and the probability of a depressive episode in the last year.
A disturbed family environment uniquely predicted all four early adolescent risk factors, with the strongest effect on conduct disorder, followed by neuroticism (Figure 1). Disturbed family environment strongly predicted level of social support. Controlling for other variables in the model, disturbed family environment also increased the probability of exposure to three “environmental” risk factors: lifetime trauma, marital problems in the last year, and difficulties in the last year.
Childhood sexual abuse uniquely predicted three of the four early adolescent and three of the four late adolescent risk factors, with its strongest effects on conduct disorder and lifetime trauma. In addition, childhood sexual abuse was associated with both difficulties and independent stressful life events in the last year.
Controlling for other variables in the model, childhood parental loss uniquely predicted only low educational attainment.
Risk Factors of Early Adolescence
Neuroticism had a particularly strong relationship with low self-esteem and early-onset anxiety disorders. High levels of neuroticism also predicted low levels of social support and marital problems in the last year. After the two classes of stressful life events, neuroticism was the strongest predictor of risk of onset of major depression.
Low self-esteem had a substantial influence on low educational attainment as well as predicting marital difficulties in the last year.
Early-onset anxiety disorder increased the risk for conduct disorder, low social support, and substance misuse, as well as exposure to lifetime trauma and independent stressful events in the last year. Along with the measured genetic risk factors, early-onset anxiety disorder was the only variable to uniquely predict risk both for past history of major depression and for depressive episodes in the last year.
Conduct disorder symptoms increased the risk for lifetime traumas, low social support and, especially strongly, substance use. In addition, a history of conduct disorder was a direct and independent risk factor for the onset of major depression in the past year.
Risk Factors of Late Adolescence
Low educational attainment uniquely predicted lifetime traumas, substance misuse, and the risk for divorce. Lifetime trauma also predicted divorce, past history of major depression, and difficulties and independent stressful life events in the last year. Low social support was a unique predictor only of substance misuse.
Substance misuse, the most “connected” variable in the model, was the second strongest predictor of a history of major depression and predicted exposure to three “environmental” risk factors: history of divorce, last year difficulties, and dependent stressful life events.
Adult Risk Factors
Ever being divorced and past history of major depression were both predicted by an array of upstream variables. Ever being divorced uniquely predicted only past history of major depression and last-year marital problems, while past history of major depression predicted last-year dependent stressful life events and risk for an episode of major depression in the last year.
Last-Year Risk Factors
Our model included four measures of environmental adversity in the last year. Two represented difficulties and were not timed relative to episode onset. In contrast, two represented stressful life events that had to occur in temporal proximity to the onset of major depression. All four of these risk factors were uniquely related to risk for major depression, with the impact of events being stronger than difficulties.
Episode of Major Depression in the Last Year
As depicted in Figure 3, the unique influences on risk for major depression are diverse and include genetic risk, three risk factors from early adolescence, past history of major depression, and all four last-year risk factors. Quantitatively, the three strongest risk factors were dependent and independent stressful life events in the last year and neuroticism.
Discussion
The goal of this report was to derive empirically an integrated, developmental model for the etiology of major depression in women that improved in several significant ways on the model presented in our previous report (30). Given the sample size and the complexity of our model, its fit, as assessed by three different indices, was quite good. These results suggested that we succeeded in our attempt to identify a model with a good balance of parsimony and explanatory power. It is relatively rare in the human behavioral literature to explain more than 50% of the variance for an outcome such as major depression, especially when it is assessed over as short an interval as 1 year.
Methodologic Limitations
Our efforts should, however, be interpreted in the context of six potentially critical methodologic limitations. First, our analytic model assumed a causal relationship between predictor variables (at the top of arrows) and dependent variables (at the bottom of arrows). The probable validity of this assumption varies across our model. For example, the path from genetic risk to neuroticism could only plausibly go in one direction. By contrast, the relationship between low self-esteem and low educational attainment or between divorce and past history of major depression is likely bidirectional. In some instances, the temporal ordering of our assessments over the four waves of interviews provided some confidence in our causal assumptions. Furthermore, after the completion of our model, we experimented with shifting the order of variables. The overall fit of the model consistently declined, and little change was seen in path estimates. It is unlikely that our parameter estimates are far off because of assumptions of directions of causality. However, it is probable that in some parts of our model, intervariable relationships that we assume take the form of A→B may be truly either A←B or, more likely, A↔B.
Second, some variables were assessed by long-term retrospective recall. Numerous studies have suggested that such data are subject to recall bias that is more likely to overestimate than to underestimate causal relationships (53–55). Ideally, this study should have been done prospectively with a twin cohort followed from birth, but this strategy was not feasible. Within the limits of a longitudinal design beginning with a cohort in early to mid-adulthood, we did several things to minimize this problem. We combined reports across raters (including parents for the key variable of disturbed family environment), thereby reducing the impact of individual rater bias. Many variables were assessed in a prospective fashion, i.e., we asked about the variables during the interviews that occurred before the interview at which the prevalence of major depression in the last year was assessed. This strategy should have reduced some aspects of reporting bias. The reference period for several key variables was the last year, keeping the time frame of recall to a minimum. For stressful life events, individual dates were required, which may have improved recall. Three key variables (childhood parental loss, educational attainment, and history of divorce) were relatively objective and probably subject to less recall bias. Finally, many important variables such as neuroticism and social support were assessed at multiple waves, thereby reducing the bias expected from any one time of reporting.
Third, the models we employed assumed that multiple independent variables act additively and linearly in their impact on a dependent variable. This is unlikely to be true for the etiology of major depression (e.g., 24, 44, 56). Although we could have included interactions in our model, the analysis and subsequent interpretation of the very large number of such possible interactions among these variables is daunting.
Fourth, the subjects consisted of epidemiologically sampled adult white female twins born in the Commonwealth of Virginia. We (57, 58) and others (59) have found that, with respect to the rates of psychopathology, including depressive symptoms and major depression, twins are representative of the general population. Furthermore, the 1-year prevalence of major depression in our study (mean=9.1%, SD=0.7%) is in the range of rates reported for women in two previous large U.S. national studies (5.0% [60] and 12.9% [61]) and nearly identical to that recently reported in a general population study of women in Norway (mean=9.7%, SD=0.9%) (62). It is likely that our sample is broadly representative of white North American and perhaps Northern European women. However, the results for men or women from other ethnic groups might differ substantially.
Fifth, our model is likely to underestimate the impact of genetic factors on the etiology of major depression in two ways. First, our measure of genetic risk for major depression was indirect and did not incorporate the most powerful use of the twin model—the direct comparison of correlations between monozygotic and dizygotic twins. Second, we did not include in our model the well-known genetic influences on neuroticism (63, 64), anxiety disorders (65), conduct disorder (66, 67), or substance use (32, 68, 69).
Sixth, in the evaluation of direct paths to last-year depression, a model of this complexity has a built-in bias. Upstream variables, such as childhood risk factors, have many more possible indirect pathways to risk for major depression than do downstream variables. Thus, all other factors being equal, direct paths will tend to be weaker for upstream variables and become progressively stronger for downstream variables closer in the model to the depressive onsets.
Summary and Implications of Findings
These results, which strongly support previous work suggesting that major depression is a complex, multifactorial disorder, suggest three major pathways to major depression: internalizing (Figure 4), externalizing (Figure 5), and adversity (Figure 6). The internalizing pathway is anchored by two variables: neuroticism and early-onset anxiety disorders. The externalizing pathway is similarly anchored by two variables: conduct disorder and substance misuse. The adversity pathway is more extensive, beginning with the three childhood risk factors of disturbed family environment, childhood sexual abuse, and parental loss, flowing through low educational attainment, lifetime trauma, and low social support to ever divorced and then influencing all four last-year environmental risk factors. This last pathway might be better termed “adversity-interpersonal difficulties,” as many of the depressogenic consequences of the earlier adversities appear to be in the realm of troubled interpersonal relationships.
These three pathways are interlinked in four important ways. First, genetic risk factors for major depression contribute to all three pathways. Second, childhood adversities are strong risk factors for externalizing disorders. Third, externalizing disorders are substantial predictors for later adversity. Finally, to a more modest extent, internalizing variables also predispose to future adversity.
Of the many points that could be emphasized in this rich set of results, we specifically comment on eight. First, this model illustrates the problem that in studying nuclear families, genetic and environmental risk factors for major depression are confounded. Substantial correlations were seen between measures of genetic risk and indices of childhood environmental adversity.
Second, our model accounted for 52% of the variation in liability to onset of major depression in a 1-year period. Although this result reflects a high level of predictability for the behavioral sciences, it can be legitimately asked why the model did not account for more variance. One reason is that major depression was not diagnosed with perfect accuracy. In our short-term test-retest sample, the kappa coefficient (70) and the tetrachoric correlation for diagnosis of major depression were 0.60 (SD=0.09) and 0.86 (SD=0.06), respectively, suggesting that about 15% of the variance in liability to major depression was measurement error. Many of our predictor variables themselves contained error, and our list of such variables was hardly exhaustive. For example, neuroticism and self-esteem are unlikely to capture fully the temperamental and cognitive substrates of liability to major depression. We had no measures of defense styles, coping strategies, or biological markers of vulnerability. Some of the unexplained variance in liability could result from interactions between risk factors that were not captured in our additive model. A year is a relatively short sampling period, and our predictability might increase if we examined a longer time period.
Third, our results illustrate the probable intricacy of the “gene-to-phenotype” pathway for complex psychiatric disorders such as major depression. Of the nine paths from genetic risk factors in our model, three involved correlations with key childhood environmental adversities. These relationships could be mediated through the genotype of the parents or the genotype of the twin. In the former, parents of affected twins would, on average, have high liability to major depression, which would predispose directly to family discord and divorce. In the latter, the twin’s own childhood temperament, influenced by genetic factors, would directly contribute to familial disturbances. Two of the nine paths involve more unambiguously what we have previously termed “genetic control of exposure to the environment” (71), in which individuals at high genetic risk for major depression select themselves into lifetime traumas and divorce, which in turn increase the risk for depressive episodes. Consistent with prior work (72), one path suggests that genetic risk factors for major depression act in part by influencing personality. Substance misuse was also an important intervening variable between genes and major depression in our model. Finally, in addition to having an indirect influence on these pathways, genetic risk factors directly increase the probability for both prior and last-year episodes of major depression. Genetic factors were the only childhood risk factor to directly influence the latter outcome.
Fourth, consistent with prior results (37), childhood sexual abuse in women had a unique, diverse, and substantial impact on a wide range of risk factors for major depression that could not be accounted for by the observed positive correlations with disturbed family environment, parental loss, or genetic risk. It is noteworthy that, unlike disturbed family environment, childhood sexual abuse uniquely contributed to lower educational attainment and substance misuse.
Fifth, several negative results are worthy of comment. When the analysis controlled for level of neuroticism, low self-esteem was not a major predictor of other risk factors or of major depression itself. In this data set, stable negative self-schemata were not a potent unique risk factor for major depression. Neither educational status, used partly as a proxy for social class, nor social support had more than a modest and indirect effect on risk for major depression.
Sixth, consistent with prior findings (11), early-onset anxiety disorder in women was a unique and potent risk factor for both past history and last-year major depression, independent of the trait neuroticism with which it was highly correlated. Given prior results in this sample, we were surprised that the final model did not include a direct path from genetic risk factors to early-onset anxiety. This path was present in early versions of the model, but in the reduced version it was subsumed into the indirect path from genetic risk to neuroticism to early-onset anxiety.
Seventh, as shown previously (30), in the prediction of episodes of major depression over short time periods, recent environmental adversity remained the strongest risk factor. However, the probability of exposure to stressful life events was in turn at least weakly predicted by a range of upstream variables in the model.
Last, although several prior twin analyses with this sample showed no evidence for a familial-environmental contribution to the etiology of major depression (31, 73, 74), the present results suggest that a disturbed family environment may play an important role in the developmental cascade leading to depression. Two possible explanations for this apparent discrepancy are noteworthy. First, family environment in twin studies is defined as those environmental factors that impact on liability equally in both members of the twin pair. As Plomin and colleagues (75, 76) have pointed out, many aspects of the family are likely to impact differently on different children, either because one child is singled out or because the children react differently to the same stressor owing to differences in temperament or maturity. Furthermore, we found only modest twin concordance for childhood sexual abuse in this sample (37), suggesting that this key risk factor will—from the perspective of twin modeling—contribute more to individual-specific than to familial-environmental effects. Second, twin modeling for dichotomous traits with realistic sample sizes is a blunt tool. Power analyses showed that, in our female-female twin cohort, given the presence of substantial genetic effects, we could easily miss familial-environmental factors that could account for up to 20% of the variance in liability (77).
 |
 |
Received Sept. 10, 2001; revision received Jan. 30, 2002; accepted Feb. 26, 2002. From the Virginia Institute for Psychiatry and Behavioral Genetics and the Departments of Psychiatry and Human Genetics, Medical College of Virginia of Virginia Commonwealth University. Address reprint requests to Dr. Kendler, Department of Psychiatry, PO Box 980126, Medical College of Virginia, Richmond, VA 23298-0126; [email protected] (e-mail). Supported by NIH grants MH-40828, AA-09095, AA-00236, DA-11287, and MH/AA/DA-49492. The authors acknowledge the contribution of the Virginia Twin Registry, now part of the Mid-Atlantic Twin Registry (MATR), to ascertainment of subjects for this study. The MATR, directed by Drs. L. Corey and L. Murrelle, has received support from the National Institutes of Health, the Carman Trust, and the W.M. Keck, John Templeton, and Robert Wood Johnson Foundations. The authors thank Alan Gruenberg, M.D., and Patrick Sullivan, M.D., for comments on an earlier version of this paper.
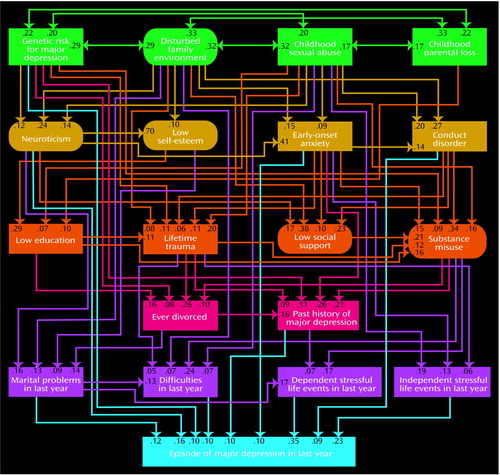
Figure 1. Path and Correlation Estimates of the Best-Fitting Model for Predicting an Episode of Major Depression in the Last Year in 1,942 Female Twinsa
aTwo-headed arrows represent correlation coefficients, and one-headed arrows represent path coefficients or standardized partial regression coefficients. Latent variables—indexed by observed variables in a measurement model—are depicted in ovals, and observed variables are depicted in rectangles. All variables have estimated residual variance that is not depicted in the figure. See text for a description of each variable.
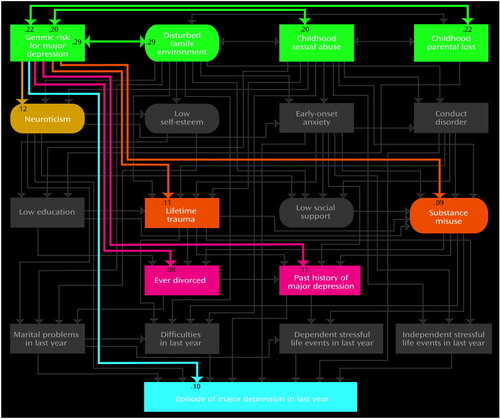
Figure 2. Paths and Correlations Involving Genetic Risk for Major Depression in the Best-Fitting Model for Predicting an Episode of Major Depression in the Last Year in 1,942 Female Twins
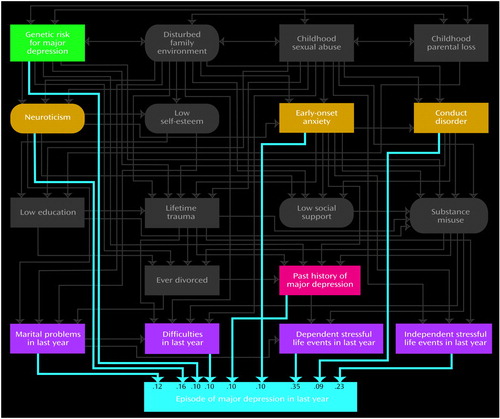
Figure 3. Paths Involving Episode of Major Depression in the Last Year in the Best-Fitting Model for Predicting an Episode of Major Depression in the Last Year in 1,942 Female Twins
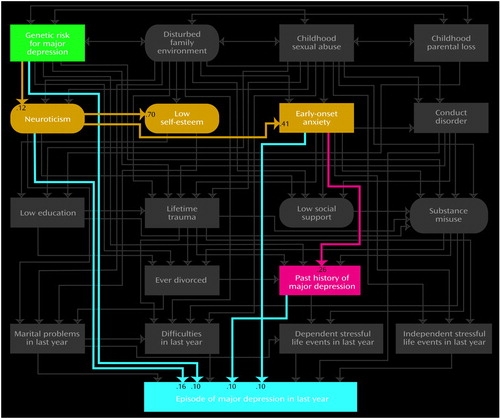
Figure 4. Paths Reflecting a Broad Internalizing Pathway to Major Depression in the Best-Fitting Model for Predicting an Episode of Major Depression in the Last Year in 1,942 Female Twins
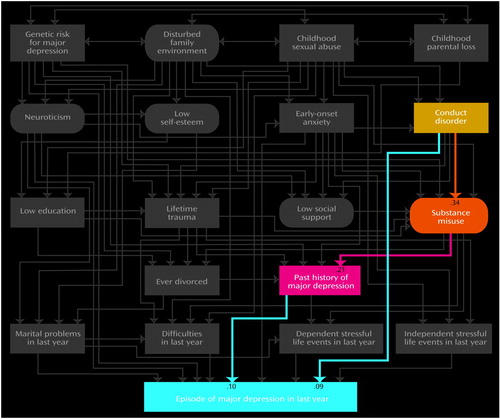
Figure 5. Paths Reflecting a Broad Externalizing Pathway to Major Depression in the Best-Fitting Model for Predicting an Episode of Major Depression in the Last Year in 1,942 Female Twins
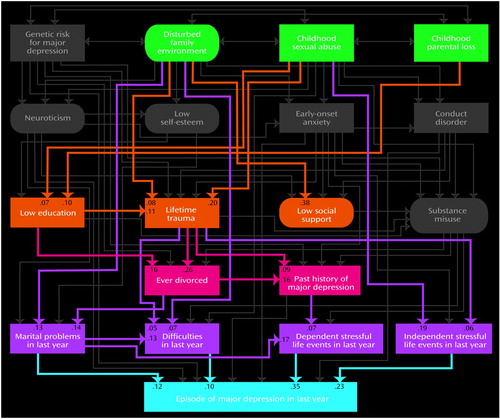
Figure 6. Paths Reflecting a Broad Adversity/Interpersonal Difficulty Pathway to Major Depression in the Best-Fitting Model for Predicting an Episode of Major Depression in the Last Year in 1,942 Female Twins
1. Tsuang MT, Faraone SV: The Genetics of Mood Disorders. Baltimore, Johns Hopkins University Press, 1990Google Scholar
2. McGuffin P, Katz R, Watkins S, Rutherford J: A hospital-based twin register of the heritability of DSM-IV unipolar depression. Arch Gen Psychiatry 1996; 53:129-136Crossref, Medline, Google Scholar
3. Sullivan PF, Neale JM, Kendler KS: Genetic epidemiology of major depression: review and meta-analysis. Am J Psychiatry 2000; 157:1552-1562Link, Google Scholar
4. Parker G: Parental characteristics in relation to depressive disorders. Br J Psychiatry 1979; 134:138-147Crossref, Medline, Google Scholar
5. Holmes SJ, Robins LN: The role of parental disciplinary practices in the development of depression and alcoholism. Psychiatry 1988; 51:24-36Crossref, Medline, Google Scholar
6. Fergusson DM, Mullen PE: Childhood Sexual Abuse: An Evidence Based Perspective. Thousand Oaks, Calif, Sage Publications, 1999Google Scholar
7. Tennant C: Parental loss in childhood: its effect in adult life. Arch Gen Psychiatry 1988; 45:1045-1050Crossref, Medline, Google Scholar
8. Hirschfeld RM, Klerman GL, Lavori P, Keller MB, Griffith P, Coryell W: Premorbid personality assessments of first onset of major depression. Arch Gen Psychiatry 1989; 46:345-350Crossref, Medline, Google Scholar
9. Boyce P, Parker G, Barnett B, Cooney M, Smith F: Personality as a vulnerability factor to depression. Br J Psychiatry 1991; 159:106-114Crossref, Medline, Google Scholar
10. Angst J, Clayton P: Premorbid personality of depressive, bipolar, and schizophrenic patients with special reference to suicidal issues. Compr Psychiatry 1986; 27:511-532Crossref, Medline, Google Scholar
11. Breslau N, Schultz L, Peterson E: Sex differences in depression: a role for preexisting anxiety. Psychiatry Res 1995; 58:1-12Crossref, Medline, Google Scholar
12. Kessler RC, Nelson CB, McGonagle KA, Liu J, Swartz M, Blazer DG: Comorbidity of DSM-III-R major depressive disorder in the general populaton: results from the US National Comorbidity Survey. Br J Psychiatry Suppl 1996; 30:17-30Medline, Google Scholar
13. Moffitt TE, Caspi A, Rutter M, Silva PA: Sex Differences in Antisocial Behaviour: Conduct Disorder, Delinquency, and Violence in the Dunedin Longitudinal Study. Cambridge, UK, Cambridge University Press, 2001Google Scholar
14. Ingram RE, Miranda J, Segal ZV: Cognitive Vulnerability to Depression. New York, Guilford Press, 1998Google Scholar
15. Cutler SE, Nolen-Hocksema S: Accounting for sex differences in depression through female victimization: childhood sexual abuse. Sex Roles 1991; 24:425-438Crossref, Google Scholar
16. Wyatt GE, Powell GJ: Identifying the lasting effects of child sexual abuse: an overview, in Lasting Effects of Child Sexual Abuse. Edited by Wyatt GE, Powell GJ. Newbury Park, Calif, Sage Publications, 1988, pp 11-18Google Scholar
17. Keane TM, Wolfe J: Comorbidity in post-traumatic stress disorder: an analysis of community and clinical studies. J Appl Soc Psychol 1990; 20:1776-1788Crossref, Google Scholar
18. Kessler RC, Magee WJ: Childhood adversities and adult depression: basic patterns of association in a US national survey. Psychol Med 1993; 23:679-690Crossref, Medline, Google Scholar
19. Henderson A: Social support and depression, in The Meaning and Measurement of Social Support. Edited by Veiel H, Baumann U. New York, Hemisphere, 1992, pp 85-92Google Scholar
20. Whisman MA, Sheldon CT, Goering P: Psychiatric disorders and dissatisfaction with social relationships: does type of relationship matter? J Abnorm Psychol 2000; 109:803-808Crossref, Medline, Google Scholar
21. Lewinsohn PM, Hoberman HM, Rosenbaum M: A prospective study of risk factors for unipolar depression. J Abnorm Psychol 1988; 97:251-264Crossref, Medline, Google Scholar
22. Harrington R, Fudge H, Rutter M, Pickles A, Hill J: Adult outcomes of childhood and adolescent depression, I. psychiatric status. Arch Gen Psychiatry 1990; 47:465-473Crossref, Medline, Google Scholar
23. Lavori PW, Keller MB, Klerman GL: Relapse in affective disorders: a reanalysis of the literature using life table methods. J Psychiatr Res 1984; 18:13-25Crossref, Medline, Google Scholar
24. Brown GW, Harris TO: Social Origins of Depression: A Study of Psychiatric Disorder in Women. London, Tavistock, 1978Google Scholar
25. Kessler RC: The effects of stressful life events on depression. Ann Rev Psychology 1997; 48:191-214Crossref, Medline, Google Scholar
26. Akiskal HS, McKinney WT Jr: Depressive disorders: toward a unified hypothesis. Science 1973; 182:20-29Crossref, Medline, Google Scholar
27. Akiskal HS, McKinney WT Jr: Overview of recent research in depression: integration of ten conceptual models into a comprehensive clinical frame. Arch Gen Psychiatry 1975; 32:285-305Crossref, Medline, Google Scholar
28. Whybrow PC, Akiskal HS, McKinney WT Jr: Toward a psychobiological integration: affective illness as a final common path to adaptive failure, in Mood Disorders: Toward a New Psychobiology. Edited by Whybrow PC, Akiskal HS, McKinney WT Jr. New York, Plenum, 1984, pp 173-203Google Scholar
29. Rutter M: Longitudinal data in the study of causal processes: some uses and some pitfalls, in Studies of Psychosocial Risk: The Power of Longitudinal Data. Edited by Rutter M. New York, Cambridge University Press, 1988, pp 1-28Google Scholar
30. Kendler KS, Kessler RC, Neale MC, Heath AC, Eaves LJ: The prediction of major depression in women: toward an integrated etiologic model. Am J Psychiatry 1993; 150:1139-1148Link, Google Scholar
31. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ: A population-based twin study of major depression in women: the impact of varying definitions of illness. Arch Gen Psychiatry 1992; 49:257-266Crossref, Medline, Google Scholar
32. Kendler KS, Prescott CA: Cannabis use, abuse, and dependence in a population-based sample of female twins. Am J Psychiatry 1998; 155:1016-1022Link, Google Scholar
33. Parker G, Tupling H, Brown LB: A parental bonding instrument. Br J Med Psychol 1979; 52:1-10Crossref, Google Scholar
34. Kendler KS: Parenting: a genetic-epidemiologic perspective. Am J Psychiatry 1996; 153:11-20Link, Google Scholar
35. Moos R, Moos B: Family Environment Scale Manual, 2nd ed. Palo Alto, Calif, Consulting Psychologists Press, 1986Google Scholar
36. Martin J, Anderson J, Romans S, Mullen P, O’Shea M: Asking about child sexual abuse: methodological implications of a two-stage survey. Child Abuse Neglect 1993; 17:383-392Crossref, Medline, Google Scholar
37. Kendler KS, Bulik CM, Silberg JL, Hettema JM, Myers J, Prescott CA: Childhood sexual abuse and adult psychiatric and substance use disorders in women: an epidemiological and cotwin control analysis. Arch Gen Psychiatry 2000; 57:953-959Crossref, Medline, Google Scholar
38. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ: Childhood parental loss and adult psychopathology in women: a twin study perspective. Arch Gen Psychiatry 1992; 49:109-116Crossref, Medline, Google Scholar
39. Eysenck SBG, Eysenck HJ, Barrett P: A revised version of the psychoticism scale. Person Indiv Dif 1985; 6:21-29Crossref, Google Scholar
40. Rosenberg CM: Determinants of psychiatric illness in young people. Br J Psychiatry 1969; 115:907-915Crossref, Medline, Google Scholar
41. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ: The genetic epidemiology of phobias in women: the inter-relationship of agoraphobia, social phobia, situational phobia, and simple phobia. Arch Gen Psychiatry 1992; 49:273-281Crossref, Medline, Google Scholar
42. Fagerstrom KO, Schneider NG: Measuring nicotine dependence: a review of the Fagerstrom Tolerance Questionnaire. J Behav Med 1989; 12:159-182Crossref, Medline, Google Scholar
43. Schuster TL, Kessler RC, Aseltine RH Jr: Supportive interactions, negative interactions, and depressed mood. Am J Community Psychol 1990; 18:423-438Crossref, Medline, Google Scholar
44. Kendler KS, Kessler RC, Walters EE, MacLean C, Neale MC, Heath AC, Eaves LJ: Stressful life events, genetic liability and onset of an episode of major depression in women. Am J Psychiatry 1995; 152:833-842Link, Google Scholar
45. Kendler KS, Karkowski LM, Prescott CA: Stressful life events and major depression: risk period, long-term contextual threat, and diagnostic specificity. J Nerv Ment Dis 1998; 186:661-669Crossref, Medline, Google Scholar
46. Kendler KS, Thornton LM, Gardner CO: Stressful life events and previous episodes in the etiology of major depression in women: an evaluation of the “kindling” hypothesis. Am J Psychiatry 2000; 157:1243-1251Link, Google Scholar
47. Muthen LK, Muthen BO: Mplus User’s Guide. Edited by Muthen LK and Muthen BO. Los Angeles, Muthen & Muthen, 1998Google Scholar
48. Raghunathan TE, Solenberger P, Van Hoewyk D: IVEware: Imputation and Variance Estimation Software (User’s Guide). Ann Arbor, University of Michigan, Institute for Social Research, 2000Google Scholar
49. Schafer JL: Analysis of Incomplete Multivariate Data. New York, Chapman & Hall, 1997Google Scholar
50. Bentler PM: Comparative fit indexes in structural models. Psychol Bull 1990; 107:238-246Crossref, Medline, Google Scholar
51. Bentler PM, Bonett DG: Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull 1980; 88:588-606Crossref, Google Scholar
52. Steiger JH: Structural model evaluation and modification: an interval estimation approach. Multivar Beh Res 1990; 25:173-180Crossref, Google Scholar
53. Bradburn NM, Rips LJ, Shevell SK: Answering autobiographical questions: the impact of memory and inference on surveys. Science 1987; 236:157-161Crossref, Medline, Google Scholar
54. Henry B, Moffitt TE, Caspi A, Langley J, Silva PA: On the “remembrance of things past”: a longitudinal evaluation of the restrospective method. Psychol Assess 1994; 6:92-101Crossref, Google Scholar
55. Maughan B, Rutter M: Retrospective reporting of childhood adversity: assessing long-term recall. J Pers Disord 1997; 11:19-33Crossref, Google Scholar
56. Cohen S, Wills TA: Stress, social support, and the buffering hypothesis. Psychol Bull 1985; 98:310-357Crossref, Medline, Google Scholar
57. Kendler KS, Martin NG, Heath AC, Eaves LJ: Self-report psychiatric symptoms in twins and their nontwin relatives: are twins different? Am J Med Genet 1995; 60:588-591Crossref, Medline, Google Scholar
58. Kendler KS, Pedersen NL, Farahmand BY, Persson PG: The treated incidence of psychotic and affective illness in twins compared with population expectation: a study in the Swedish Twin and Psychiatric Registries. Psychol Med 1996; 26:1135-1144Crossref, Medline, Google Scholar
59. Rutter M, Redshaw J: Annotation: growing up as a twin: twin-singleton differences in psychological development. J Child Psychol Psychiatry 1991; 32:885-895Crossref, Medline, Google Scholar
60. Weissman MM, Bruce ML, Leaf PJ, Florio LP, Holzer C: Affective disorders, in Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. Edited by Robins LN, Regier DA. New York, Free Press, 1991, pp 53-80Google Scholar
61. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8-19Crossref, Medline, Google Scholar
62. Kringlen E, Torgersen S, Cramer V: A Norwegian psychiatric epidemiological study. Am J Psychiatry 2001; 158:1091-1098Link, Google Scholar
63. Loehlin JC: Genes and Environment in Personality Development. Newbury Park, Calif, Sage Publications, 1992Google Scholar
64. Heath AC, Neale MC, Kessler RC, Eaves LJ, Kendler KS: Evidence for genetic influences on personality from self-reports and from informant ratings. J Pers Soc Psychol 1992; 63:85-96Crossref, Medline, Google Scholar
65. Kendler KS, Walters EE, Neale MC, Kessler RC, Heath AC, Eaves LJ: The structure of the genetic and environmental risk factors for six major psychiatric disorders in women: phobia, generalized anxiety disorder, panic disorder, bulimia, major depression and alcoholism. Arch Gen Psychiatry 1995; 52:374-383Crossref, Medline, Google Scholar
66. Slutske WS, Heath AC, Dinwiddie SH, Madden PA, Bucholz KK, Dunne MP, Statham DJ, Martin NG: Modeling genetic and environmental influences in the etiology of conduct disorder: a study of 2,682 adult twin pairs. J Abnorm Psychol 1997; 106:266-279Crossref, Medline, Google Scholar
67. Goldstein RB, Prescott CA, Kendler KS: Genetic and environmental factors in conduct problems and adult antisocial behavior among adult female twins. J Nerv Ment Dis 2001; 189:201-209Crossref, Medline, Google Scholar
68. Tsuang MT, Lyons MJ, Eisen SA, Goldberg J, True W, Meyer JM, Toomey R, Faraone SV, Eaves L: Genetic influences on DSM-III-R drug abuse and dependence: a study of 3,297 twin pairs. Am J Med Genet 1996; 67:473-477Crossref, Medline, Google Scholar
69. Kendler KS, Heath AC, Neale MC, Kessler RC, Eaves LJ: A population-based twin study of alcoholism in women. JAMA 1992; 268:1877-1882Crossref, Medline, Google Scholar
70. Cohen J: A coefficient of agreement for nominal scales. Educ Psychol Meas 1960; 20:37-46Crossref, Google Scholar
71. Kendler KS, Eaves LJ: Models for the joint effect of genotype and environment on liability to psychiatric illness. Am J Psychiatry 1986; 143:279-289Link, Google Scholar
72. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ: A longitudinal twin study of personality and major depression in women. Arch Gen Psychiatry 1993; 50:853-862Crossref, Medline, Google Scholar
73. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ: The lifetime history of major depression in women: reliability of diagnosis and heritability. Arch Gen Psychiatry 1993; 50:863-870Crossref, Medline, Google Scholar
74. Kendler KS, Gardner CO, Neale MC, Prescott CA: Genetic risk factors for major depression in men and women: similar or different heritabilities and same or partly distinct genes? Psychol Med 2001; 31:605-616Crossref, Medline, Google Scholar
75. Plomin R, Daniels D: Why are children in the same family so different from each other? Behav Brain Sci 1987; 10:1-16Crossref, Google Scholar
76. Reiss D, Plomin R, Hetherington EM, Howe GW, Rovine M, Tryon A, Hagan MS: The separate worlds of teenage siblings: an introduction to the study of the nonshared environment and adolescent development, in Separate Social Worlds of Siblings: The Impact of Nonshared Environment on Development. Edited by Hetherington EM, Reiss D, Plomin R. Hillsdale, NJ, Lawrence Erlbaum, 1994, pp 63-109Google Scholar
77. Neale MC, Eaves LJ, Kendler KS: The power of the classical twin study to resolve variation in threshold traits. Behav Genet 1994; 24:239-258Crossref, Medline, Google Scholar



