A Norwegian Psychiatric Epidemiological Study
Abstract
OBJECTIVE: This study reports results of a large-scale epidemiological investigation of the prevalence of mental disorder in Oslo. METHOD: A random sample of Oslo residents age 18–65 years was drawn from the Norwegian National Population Register. A total of 2,066 subjects, 57.5% of the original sample, were interviewed with the Composite International Diagnostic Interview in 1994–1997. The mean age of the interviewed subjects was 39.3 years. RESULTS: The 12-month prevalence of all mental disorders was 32.8%, and the lifetime prevalence was 52.4%. Alcohol abuse/dependence and major depression had the highest lifetime prevalence and 12-month prevalences. All mental disorders were more prevalent in women than in men, with the exception of alcohol and drug abuse/dependence. Severe psychopathology (e.g., three or more diagnoses) was found in 14%–15% of the respondents. The lifetime and 12-month prevalences for all diagnostic categories except drug abuse/dependence were similar to those found in the United States Comorbidity Survey. CONCLUSIONS: Epidemiological data for Oslo show that the lifetime and 12-month prevalences of mental disorder are quite high, with alcohol abuse/dependence and major depression particularly frequent. The rates for women are higher than those for men for all diagnostic categories, except for alcohol and drug abuse/dependence.
The history of psychiatric epidemiology can be divided into three phases. In the first phase, which originated in German psychiatry, it was assumed that psychiatric illnesses were mainly hereditary in etiology, and research was focused on hospitalized patients with severe mental illness. After World War II, psychiatric epidemiology was strongly influenced by sociological and social-anthropological thinking, especially in the United States. Many of the studies that were carried out in this second phase—the most famous of which are the Midtown Manhattan study (1) and the Stirling County (Canada) study of Leighton and colleagues (2)—did not focus on psychiatric diagnoses but on “psychiatric impairment.”
During the 1970s psychiatric epidemiology entered a new phase. The study by Weissman and Myers (3, 4), which developed from the Midtown Manhattan study, was the first American epidemiological study with a random sample of households and the first to use a structured diagnostic instrument (the Schedule for Affective Disorders and Schizophrenia—Lifetime Version). This was followed by the U.S. Epidemiologic Catchment Area (ECA) study (5, 6). In connection with the ECA study, a comprehensive structured interview, the National Institute of Mental Health Diagnostic Interview Schedule (DIS), was developed; this instrument could be administered by trained interviewers who were not necessarily psychiatrists or psychologists (7). The ECA study reports described the psychiatric illness picture in the United States in the early 1980s. The results showed that at one time or another 32% of adult Americans had experienced a diagnosable DSM-III psychiatric illness and that 20% had a psychiatric illness at the time of the study. Of great interest was the higher prevalence of psychopathology in younger compared with older respondents, an apparent cohort effect.
Similar research using the DIS has been carried out in New Zealand, the Caribbean, and Canada, with varying results. The New Zealand study examined psychiatric ill health in the town of Christchurch, which had a population of 30,000 in the 1980s (8). The design and methods resembled those of the ECA study, including the use of randomly chosen households. For the most part, the results were in accordance with the those of ECA study, although a much higher prevalence of depression and compulsive drinking was recorded. As in the ECA study (5, 6), the highest prevalence for most psychiatric disturbances was in the 25–44-year age group, although in general the differences in prevalences between age groups were slight.
A study in Puerto Rico using the DIS was done in 1984 (9). Six-month prevalence figures did not differ much from the ECA figures (for St. Louis, New Haven, and Baltimore), with the exception of higher rates of cognitive impairment, somatoform disorder, and compulsive drinking. The lifetime prevalence for all mental illnesses, except for psychosexual dysfunction, was 28%; the 6-month prevalence was 16%.
In a study in Edmonton, Alberta, Canada, the DIS and the General Health Questionnaire were administered to a random sample of 3,258 adults (10, 11). A lifetime prevalence of 33.8% was found for one or more psychiatric diagnoses, with the exception of DSM-III drug abuse. The most common diagnosis was alcohol abuse, followed by phobias and major depression. Women had the highest rates for depression, anxiety, and somatic conditions, while men had the highest rates for alcohol and drug abuse, as well as for antisocial personality disorder. The 6-month prevalence was 17.1% for all mental illnesses, which was in accord with the findings of the ECA study (5, 6), with the exception of the much higher rates of alcohol abuse for both men and women and higher rates of drug abuse and antisocial personality disorder for men. As in the ECA study, a considerably lower lifetime prevalence of mental disorder was found among the elderly than among younger people, which may have been related to memory loss due to age, institutionalization of elderly persons, or a cohort effect.
The Nordic countries—Denmark, Finland, Iceland, Norway, and Sweden—have a long tradition with regard to psychiatric epidemiology. Most of the early studies from these countries were based on hospitalized populations, but later, general population samples were also studied. Essen-Møller and co-workers (12) embarked on a community study in southern Sweden in 1947. This investigation was followed up by Essen-Møller and later by Hagnell (13), who estimated that the lifetime risk of developing a mental illness was 43% for men and 73% for women.
The Finnish UKK Institute study (14) included 1,000 persons age 15–64 years in 1969–1971 and in 1985–1987. The yearly incidence of mental disorder was 17 per 1,000 in female respondents and 14 per 1,000 in male respondents. In contrast to observations in the United States, this study showed that younger cohorts were healthier than older ones, which might be related to the harsh times the Finnish population experienced during and after World War II. The Mini-Finland Health Survey (15) (1978–1980) included a random sample of 8,000 persons over age 30 who were surveyed with regard to both somatic and mental illness. The prevalence of mental disorder was 17.4%, with a somewhat higher rate for women than for men. The highest prevalence in women was in the 50–64-year age group; the highest figure for men was in the 60–65-year age group. Extremely high prevalences were reported for divorced women. In a random sample of 1,000 adults in Oslo in the 1970s, Dalgard (16) found considerable variation in the prevalence of mental illness, from 29% in an impoverished district of the city to 9% in a stable, well-to-do district.
While the ECA study (6) was the first large epidemiological survey in the United States to apply modern diagnostic procedures, the National Comorbidity Survey (17) in the late 1980s went a step further. Here, the diagnoses were based on the DSM-III-R criteria, which superseded the DSM-III criteria and which can be used to generate diagnoses according to the current classification systems, DSM-IV and ICD-10. The ECA study was primarily a descriptive study of prevalence and incidence, while the National Comorbidity Survey was a more extensive analytical study that included an evaluation of parental psychopathology, family problems, social networks, and external stress. A random sample of 8,090 subjects between age 15–54 years was selected, excluding institutionalized individuals. The response rate was 82.6%. The National Comorbidity Survey used a modified version of the Composite International Diagnostic Interview (18), a highly structured instrument that combined aspects of the DIS and the Present State Examination (19) and was designed for use by trained lay interviewers. Almost 50% of the participants met criteria for at least one lifetime disorder, and almost 30% had at least one mental illness in the past year. The most common disorders were severe depression, compulsive drinking, and social and simple phobias. More than half of the lifetime disorders were evident in the 14% of the population with three or more DSM-III-R mental disorders. Women had an increased risk for affective and anxiety disorders, and men had an increased risk for drug and alcohol problems, as well as antisocial personality disorder. The extent of mental illness decreased with increasing age and higher social status. Noteworthy were the findings that mental illness was more common than previously thought and, furthermore, that ill health was strongly concentrated in 14% of the population. The highest prevalence was found in the 25–34-year age group, with lower rates in older age groups. This pattern was in accord with the results of the ECA study (6), which also documented high rates of psychopathology in younger cohorts.
The ECA study (5, 6) has been criticized for methodological flaws that may have been responsible for findings of a considerably high rate of schizophrenia and an unusually low rate of depression. The finding of a high rate of schizophrenia has been attributed to the use of lay people as interviewers and the use of the DIS, which has low discriminatory ability, resulting in a high rate of false positive cases (20). It is difficult to explain why the ECA figures should be so different from those reported in other studies.
In the Netherlands Mental Health Survey and Incidence Study, a representative sample of 7,076 persons age 18–64 years were interviewed with the Composite International Diagnostic Interview at home in 1996 (21, 22). The net response rate to the first wave of interviews was 69.7%. Follow-up interviews in the same sample were scheduled at 12 and 36 months. The study found that 41.2% of the adult population under age 65 had at least one lifetime DSM-III-R disorder, and 23.3% had experienced at least one disorder in the preceding year. No gender differences in overall morbidity were found. Depression, anxiety, and alcohol abuse and dependence were most prevalent, and there was a high degree of comorbidity of these disorders. Mood disorders, especially dysthymia, were almost twice as common among women than among men, and women were also more than twice as likely to suffer from anxiety disorders. Men had higher rates of alcohol and drug use. A consistent finding for all disorders was that the oldest age group (55–64 years old) had the lowest prevalence. The highest rate for mood disorders (9.3%) was recorded for the 35–44-year age group. For the anxiety disorders, there was little difference in rates between the age groups.
The study reported here addresses the following two questions:
1. What is the 12-month and lifetime prevalence of mental illness in Oslo?
2. What are the gender- and age-specific prevalences of different disorders identified according to DSM-III-R criteria?
Method
Sample
From the National Population Register of Norway we obtained a random sample of 3,590 individuals, age 18–65 years, from the total population of 308,237 in Oslo, with no stratification on the basis of age, gender, or household. The National Population Register is a central, governmental database that includes all individuals who are residents of Norway, irrespective of citizenship. The national register was established as a computerized database in 1964, but as early as 1906, its predecessor, the Population Register of Oslo, had been used for administrative as well as for statistical and scientific purposes. The national register is continuously updated by notification from primary sources such as maternity clinics and probate courts and with data collected from individual immigrants to Norway.
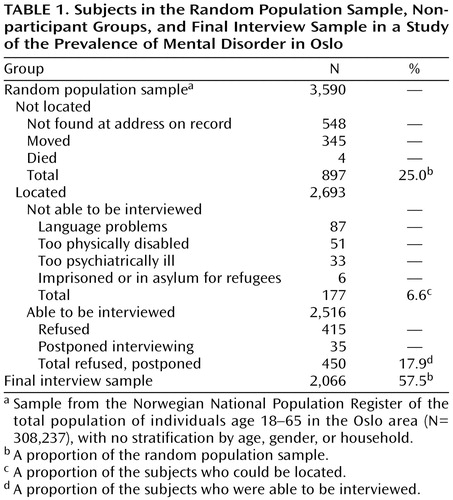
As Table 1 shows, 25.0% of the potential subjects could not be interviewed; 345 had moved out of Oslo, 548 were not found at the address on record, either because they had given an incorrect address to the authorities or because they had moved to another residence without notifying the authorities, and four had died. Of those who could be located, 51 were too physically ill (hospitalized or experiencing extreme disability) to be interviewed. Thirty-three were too psychiatrically ill to be interviewed (five of the those 33 were hospitalized). A few were in prison or staying at a reception center for refugees. Eighty-seven could not speak a Scandinavian language, English, French, or German well enough to respond to the survey. Thus, close to 7% of the located individuals could not be interviewed. Of the 2,516 subjects who could have been interviewed, 450 refused to participate or postponed the interview beyond the study period. Thus, 2,066 subjects, 57.5% of the original random sample of 3,590, were interviewed.
In addition to interviewing subjects who were found at home, we sought to contact subjects through repeated home visits and telephone calls. Without these additional efforts, the size of the interviewed sample would have been much smaller.
Of the interviewed sample, 44.9% were men and 55.1% were women. A majority of those we were not able to locate were men (57.0%), which was statistically significantly different from the proportion of male subjects among those who were interviewed (44.9%) (χ2=35.74, df=1, p<0.00001). The gender distribution in the group who could not be interviewed because of illness or language problems did not differ from that in the group who were interviewed. The proportion of men in the group who refused or postponed the interview was higher than that in the group who were interviewed (52.9% versus 44.9%), a statistically significant difference (χ2=9.07, df=1, p<0.01). In the overall group of subjects who were not interviewed, 54.1% were men, which was significantly different from the proportion of men in the overall interview sample (44.9%) (χ2=32.20, df=1, p<0.0001).
The mean age of the interviewed subjects was 39.3 years (SD=12.5). The mean age for the other groups was as follows: 35.3 years (SD=11.2) for those who could not be located, 40.6 years (SD=11.8) for those who refused to participate. Overall, the mean age of those in the original sample who were not interviewed was 37.7 years (SD=11.8). The interviewed subjects were significantly younger than those who could not be located (F=61.7, df=1, 2961, p<0.0001) and those who refused or postponed the interview (F=3.85, df=1, 2514, p<0.05) but did not differ significantly in age from those who were not interviewed because of illness or language problems. Overall, those who were not interviewed were significantly younger than those who were interviewed (F=16.0, df=1, 3567, p=0.0001). Most subjects who could not be located lived in the center of Oslo, whereas those who were too ill or who had language problems tended to live in the poorer eastern periphery of Oslo. Subjects who refused to participate tended to live in the relatively prosperous area west of Oslo.
In general, the highest percentage of interviews was obtained in the socioeconomically stable middle class suburbs of Oslo, and the lowest percentage was obtained in the center of Oslo. Conversely, in the part of the city where we recorded the lowest rate of psychiatric disorders, we obtained the best response rate. Thus, factors that obstruct interviewing appeared to be correlated with mental disability. Accordingly, our prevalence figures represent an underestimate of the true values, as is likely the case in all psychiatric epidemiological studies. Although it is possible to adjust epidemiological results for sex, age, and sample location, such adjustments are nearly always inadequate.
Diagnostic Assessment
At the study outset, there were 23 interviewers, most of whom were nurses and a smaller number of whom were sociology or psychology students. Interviewers were trained by practicing the Composite International Diagnostic Interview, initially with nonpatients and later in video interviews with patients from the Department of Psychiatry, Vinderen. By using this procedure, we were able to test the interviewers’ formal qualifications as well as evaluate their ability to handle the subjects. After a comprehensive evaluation, half of the original interviewers were dismissed, leaving 12 interviewers. The interviews were carried out between May 1, 1994, and Nov. 1, 1997.
The psychiatric diagnoses we report were based on DSM-III-R criteria and were generated with the Composite International Diagnostic Interview, World Health Organization (WHO) version 1.1 (23). The Composite International Diagnostic Interview gives detailed information about current and lifetime mental health. Its scoring system allows the interviewer to score individual symptoms as 1) not present, 2) present but not significant, 3) significant but explained by alcohol or drugs, 4) significant but explained by physical disease, or 5) a probable symptom of mental disorder. The DSM-III-R diagnoses generated in this study included major depression, bipolar disorder, dysthymic disorder, panic disorder, agoraphobia, social phobia, simple phobia, generalized anxiety disorder, somatoform disorder, alcohol abuse, alcohol dependence, drug abuse, drug dependence, and nonaffective psychosis. The WHO field trials of the Composite International Diagnostic Interview have documented good interrater reliability, test-retest reliability, and validity for almost all diagnostic categories (18).
Results
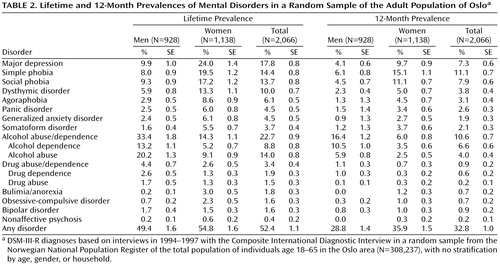
Table 2 shows the lifetime prevalences of mental disorders in Oslo for both sexes. The lifetime prevalence of a disorder is the proportion of the sample who reported having experienced symptoms of the disorder at some time in their life. The findings are based on the respondents’ answers to questions about specific symptoms. Since the mean age of the sample was less than 40 years, several respondents had not passed the risk period for emergence of some mental illnesses, e.g., depression.
As Table 2 shows, the most prevalent lifetime psychiatric diagnosis was alcohol abuse/dependence, with a 22.7% lifetime prevalence. The prevalence of this diagnosis was considerably higher for men than for women. As would be expected, the frequency of alcohol abuse was higher than the frequency of alcohol dependence. The next most prevalent lifetime disorder was major depression, found in 17.8% of the respondents. The prevalence for women was more than two times higher than that for men. The prevalences of dysthymic disorder and simple phobia were more than twice as high in women than in men. Social phobia, which causes significantly greater social impairment than simple phobia, was found in nearly twice as many women as men. The prevalences of agoraphobia, panic disorder, and generalized anxiety disorder were nearly three times higher in women than in men.
The less frequently occurring disorders included somatoform disorder, eating disorders (bulimia and anorexia), and obsessive-compulsive disorder (OCD). Patients with somatoform disorders are major consumers of health services. In this investigation, 3.7% of the respondents (more women than men) received this lifetime diagnosis. Eating disorders, most frequently bulimia, were found in 1.8% of respondents (3.0% of female respondents). Eating disorders were practically nonexistent in men. The lifetime prevalence of OCD was 1.6% but was considerably higher in women than in men.
The lifetime prevalence of nonaffective psychoses, i.e., schizophrenic and paranoid conditions, was very low, undoubtedly because we excluded individuals who were hospitalized or too ill to be interviewed.
Table 2 also shows the 12-month prevalences of DSM-III-R diagnoses in Oslo. The rates are lower than the lifetime prevalences, as would be expected. Similarities between 12-month and lifetime prevalences would suggest the presence of chronic disorders or lost memory of previous episodes of mental illness. A large difference between the lifetime and 12-month prevalences of alcohol abuse/dependence was found. The proportion of respondents who had misused alcohol at some time in the past was more than twice the proportion who had misused alcohol during the preceding 12 months.
There was also a considerable difference between the lifetime and 12-month prevalences of major depression, suggesting that many cases of major depression are episodic. The difference between the lifetime and 12-month prevalence of dysthymia was surprisingly large for a chronic condition. With regard to agoraphobia, panic disorder, and generalized anxiety disorder, the lifetime prevalence was about twice as high as the 12-month prevalence.
Our data show that the most severe psychopathology is concentrated in 14%–15% of the population. Almost half of the sample (47.4%) had never experienced mental symptoms to the degree that a DSM-III-R diagnosis was warranted, 25.7% received one lifetime diagnosis, 11.9% had two, and 14.9% had three or more.
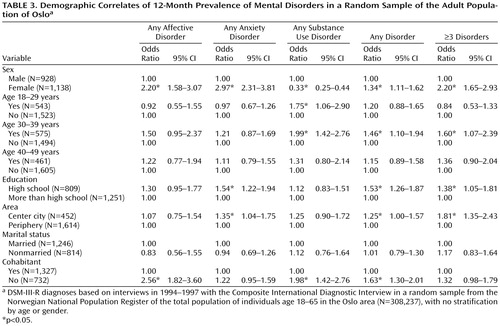
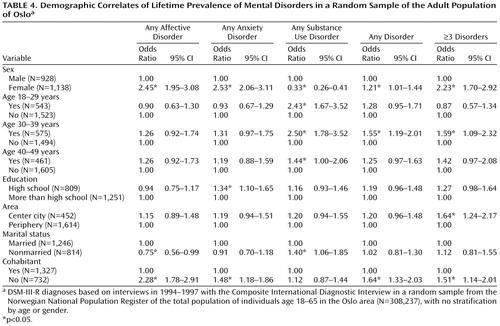
Table 3 and Table 4 show the odds ratios and confidence intervals for the relationships between demographic variables and mental disorders. The odds ratios were based on logistic regression analyses that took into account the mutual relationships among the demographic variables.
Female subjects were nearly 2.5 times more likely than male subjects to have a lifetime affective disorder. In addition, those who were married but did not live together were especially likely to have a lifetime affective disorder.
Female subjects were also more prone to have a lifetime episode of anxiety disorder. The risk was more than 2.5 times higher in female subjects than in male subjects. Those with a lower level of education were more likely to have a lifetime anxiety disorder; the same was true for people living alone. A lifetime substance use disorder was more common in men, those under age 50, and nonmarried individuals.
Any lifetime mental disorder was more common in female subjects, those between 30 and 39 years of age, and those living alone. The same demographic correlates were associated with having three or more lifetime disorders. In addition, those living in the center of the city were more likely to have three or more lifetime disorders than those living in the periphery.
Similarly, any disorder in the preceding year was more likely to have occurred in female subjects, those between 30 and 39 years of age, those with less education, those living without a partner, and those living in the center of the city. The risk of having three or more disorders during the last year was related to the same variables, except that not living with a partner did not have a statistically significant effect.
In general, gender was a powerful predictor of mental disorder. The same was true for having no current live-in partner. Marital status had virtually no importance for risk of mental disorder. Both a lower level of education and living in the center of the city had some predictive value, and age between 30 and 39 years seemed to heighten the susceptibility for mental disorders. Age over 50 years was associated with somewhat less psychiatric morbidity.
With regard to lifetime prevalence of specific disorders, including alcohol abuse and major depression, there was a general clustering of cases in the center of Oslo, with lower rates in the peripheral areas (data not shown).
Discussion
Alcohol abuse, depression, and phobias were the most frequent mental disorders in the general population of Oslo, both with regard to lifetime prevalence and 12-month prevalence. The most severe psychopathology (the presence of three or more disorders) was found in 14%–15% of the sample. Almost half of the sample (47.4%) had no psychiatric diagnosis, 25.7% received one diagnosis, and 11.9% received two diagnoses. All types of mental disorder were more prevalent in women than in men, with the exception of alcohol and drug abuse/dependence. Considering the great differences in prevalences of alcohol abuse for men and women in earlier studies, the magnitude of the sex difference in this investigation was lower than one would expect. The lifetime prevalence of alcohol abuse was more than twice as high as the 12-month prevalence. This finding seems to corroborate the impression that many individuals drink heavily in their younger years but reduce their consumption as they age. The highest lifetime and 12-month prevalences of substance use disorders were observed in the 30–39-year age group.
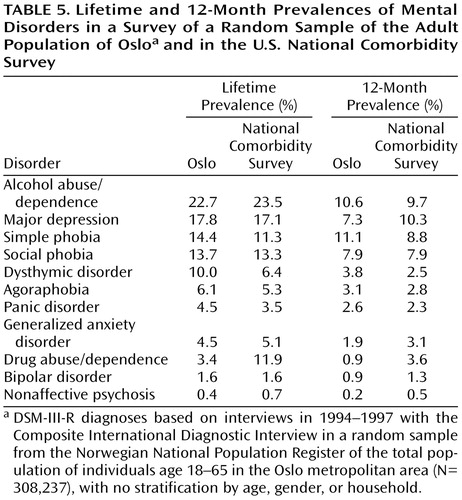
How do our findings compare with those of other investigations? Differences in prevalence and incidence among studies can be ascribed to variations in sampling and/or methods of diagnostic assessment. Here, we compare our findings with those of the U.S. National Comorbidity Study (17), since both studies dealt with representative samples from the general population and both studies used the Composite International Diagnostic Interview.
As Table 5 shows, lifetime prevalence figures from our study in Oslo are quite similar to the American figures. (The National Comorbidity Survey did not include OCD, somatoform disorder, and eating disorders.) The sole exception is drug abuse/dependence, for which the U.S. figures were three to four times higher than those for Oslo. The difference would be expected, given that the modern drug epidemic started in the United States and is known to have had an extensive effect there. The 12-month prevalences show the same pattern, with almost identical rates for alcohol abuse, major depression, and social phobia in the two countries, and far higher rates for drug abuse/dependence in the United States. The gender differences also follow the same pattern (data not shown), with somewhat higher figures for lifetime and 12-month alcohol abuse/dependence and major depression in U.S. men and somewhat lower figures for these diagnoses in U.S. women, compared with the Oslo sample. With regard to alcohol abuse/dependence, the figures were almost identical. The highest lifetime and 12-month prevalences of alcohol abuse/dependence was observed in the 25–34-year age group in Oslo, with a fall after that age.
The percentages of subjects with no lifetime DSM-III-R diagnoses, one diagnosis, two diagnoses, or three or more diagnoses, respectively, were similar in the two studies. Thus, 47.4% (SD=1.1%) of the Oslo sample and 52.0% (SD=1.1%) of the National Comorbidity Survey sample had no diagnosis, 25.7% (SD=1.0%) and 21.0% (SD=0.6%), respectively, had one diagnosis, 11.9% (SD=0.7%) and 13.0% (SD=0.5%), respectively, had two diagnoses, and 14.9% (SD=0.8%) and 14.0% (SD=0.7%), respectively, had three or more diagnoses.
Thus, there is now considerable agreement with regard to the prevalence of mental disorders in the community, in contrast to the disparity in rates reported 25 years ago (24). More recent studies have found lifetime prevalences between 30% and 50% and 12-month prevalences between 20% and 30%, depending on the methods used. The rates are considerably higher in women than in men, except for alcohol and drug abuse/dependence, and younger cohorts have more psychopathology than older cohorts (5, 6, 8, 9, 22).
Like all epidemiological and clinical investigations, this investigation had its limitations and sources of error. We did not obtain equivalent proportions of subjects in all demographic strata, e.g., older men living in the center of the city are underrepresented. Our study focused attention on the population of Oslo, the largest city of Norway. Therefore, the prevalence figures cannot be generalized to the whole country. It is well known that Oslo has more social problems than the rest of the country. Thus, one would expect a higher prevalence of anxiety, depression, and alcohol and drug problems in Oslo than in the rest of the country. One important question with regard to lifetime prevalence is the degree to which people remember past psychiatric episodes. A lower likelihood of remembering past symptoms would lead to lower lifetime prevalences. The lifetime prevalences reported here likely underestimate actual rates of illness.
In summary, the large-scale psychiatric epidemiological study of Oslo reported here found lifetime and 12-month prevalences of mental disorder of 52.4% and 32.8%, respectively. The lifetime prevalence was 22.7% for alcohol abuse and 17.8% for major depression; the 12-month prevalences for these disorders were 10.6% and 7.3%, respectively. Clear gender differences were found, with considerably higher prevalences for all diagnostic categories in women compared with men, with the exception of alcohol and drug abuse/dependence. Severe psychopathology was concentrated in 14%–15% of the population. These figures correspond well with those reported by the U.S. National Comorbidity Survey.
 |
 |
 |
 |
 |
Received Dec. 10, 1999; revisions received June 14, July 27, and Dec. 12, 2000; accepted Jan. 9, 2001. From the Department of Psychiatry, Vinderen, University of Oslo. Address reprint requests to Dr. Kringlen, Psykiatrisk Institutt, Postboks 85, Vinderen, 0319 Oslo, Norway. The study was supported by the Norwegian Council for Mental Health (Rådet for psykisk helse). The authors thank Philip Holzman, Ph.D., and Deborah Levy, Ph.D., for constructive help in editing the paper.
1. Srole L, Langner TS, Michael ST, Opler MK, Rennie TAC: Mental Health in the Metropolis: The Midtown Manhattan Study. New York, McGraw-Hill, 1962Google Scholar
2. Leighton DC, Harding JS, Macklin DB, Macmillan AM, Leighton AH: The Character of Danger: Psychiatric Symptoms in Selected Communities. New York, Basic Books, 1963Google Scholar
3. Weissman MM, Myers JK, Harding PS: Psychiatric disorders in a US urban community:1975-1976. Am J Psychiatry 1978; 135:459-462Google Scholar
4. Weissman M, Myers JK: Affective disorder in a United States urban community: the use of research diagnostic criteria in an epidemiological survey. Arch Gen Psychiatry 1978; 35:1304-1311Google Scholar
5. Blazer D, George LK, Landerman R, Pennybacker M, Melville ML, Woodbury M, Manton KG, Jordan K, Locke B: Psychiatric disorders: a rural/urban comparison. Arch Gen Psychiatry 1986; 42:651-656Crossref, Google Scholar
6. Robins LN, Helzer JE, Weissman MM, Orvaschel H, Gruenberg E, Burke JD Jr, Regier DA: Lifetime prevalence of specific psychiatric disorders in three sites. Arch Gen Psychiatry 1984; 41:949-958Crossref, Medline, Google Scholar
7. Robins LN, Helzer JE, Croughan J, Ratcliff KS: The National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Arch Gen Psychiatry 1981; 38:381-389Crossref, Medline, Google Scholar
8. Wells JE, Bushnell JA, Hornblow AR, Joyce PR, Oakley-Browne MA: Christchurch Psychiatric Epidemiology Study, part I: methodology and lifetime prevalence for specific psychiatric disorders. Aust NZ J Psychiatry 1989; 23:315-326Crossref, Medline, Google Scholar
9. Canino GJ, Bird HR, Shrout PE, Rubio-Stipec M, Bravo M, Martinez R, Sesman M, Guevara LM: The prevalence of specific psychiatric disorders in Puerto Rico. Arch Gen Psychiatry 1987; 44:727-735Crossref, Medline, Google Scholar
10. Bland RC, Newman SC, Orn H (eds): Epidemiology of Psychiatric Disorders in Edmonton. Acta Psychiatr Scand Suppl 1988; 338Google Scholar
11. Bland RC, Newman SC, Russel JM, Orn HT (eds): Epidemiology of Psychiatric Disorders in Edmonton: Phenomenology and Comorbidity. Acta Psychiatr Scand Suppl 1994; 376Google Scholar
12. Essen-Møller E, Larsson H, Uddenberg CE: Individual Traits and Morbidity in a Swedish Rural Population. Acta Psychiatr Neurol Scand Suppl 1956; 100Google Scholar
13. Hagnell O: A Prospective Study of the Incidence of Mental Disorder. Lund, Svenska Bokförlaget, 1966Google Scholar
14. Lehtinen V, Veijola J, Lindholm T, Moring J, Puuka P, Vaisanen E: Incidence of mental disorders in the Finnish UKKI study. Br J Psychiatry 1996; 168:672-678Crossref, Medline, Google Scholar
15. Lehtinen V, Joukama M, Lathela K, Raitasalo R, Jyrkinen E, Maatela J, Aromaa A: Prevalence of mental disorders among adults in Finland: basic results from the Mini-Finland Health Survey. Acta Psychiatr Scand 1990; 81:418-425Crossref, Medline, Google Scholar
16. Dalgard OS: Bomiljø og psykisk helse. Oslo, Universitetsforlaget, 1980Google Scholar
17. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8-19Crossref, Medline, Google Scholar
18. Robins LN, Wing J, Wittchen HU, Helzer JE, Babor TF, Burke J, Farmer A, Jablenski A, Pickens R, Regier DA, Sartorius N, Towle LH: The Composite International Diagnostic Interview: an epidemiologic instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch Gen Psychiatry 1988; 45:1069-1077Google Scholar
19. Wing JK, Cooper JE, Sartorius N: The Measurement and Classification of Psychiatric Symptoms: An Instructional Manual for the PSE and CATEGO Programs. New York, Cambridge University Press, 1974Google Scholar
20. Burvill PW: An appraisal of the NIMH Epidemiologic Catchment Area program. Aust NZ J Psychiatry 1987; 21:175-184Crossref, Medline, Google Scholar
21. Bijl RV, van Zessen G, Ravelli A, de Rijk K, Langendoen Y: The Netherlands Mental Health Survey and Incidence Study (NEMESIS): objectives and design. Soc Psychiatry Psychiatr Epidemiol 1998; 33:581-586Crossref, Medline, Google Scholar
22. Bijl RV, Ravelli A, van Zessen G: Prevalence of psychiatric disorder in the general population: results of the Netherlands Mental Health Survey and Incidence Study (NEMESIS). Soc Psychiatry Psychiatr Epidemiol 1998; 33:587-595Crossref, Medline, Google Scholar
23. World Health Organization: Composite International Diagnostic Interview (CIDI), core version 1.1. Geneva, WHO, 1993Google Scholar
24. Dohrenwend BP, Dohrenwend BS: Social and cultural influences on psychopathology. Annu Rev Psychol 1974; 25:417-452Crossref, Medline, Google Scholar



