Double-Blind Comparison of Sertraline, Imipramine, and Placebo in the Treatment of Dysthymia: Effects on Personality
Abstract
OBJECTIVE: Although previous studies have shown that dysthymia, or chronic depression, commonly responds to antidepressant medications (with improvements in depressive symptoms and psychosocial functioning), there have been no systematic studies of the impact of antidepressant treatment on personality variables in patients with this disorder. METHOD: In a multicenter study, 410 patients with early-onset primary dysthymia were treated in a randomized prospective fashion with sertraline, imipramine, or placebo. The data were analyzed in terms of the subjects’ scores on the Tridimensional Personality Questionnaire, a 100-item self-report instrument that measures four temperamental dimensions: harm avoidance, reward dependence, novelty seeking, and persistence. RESULTS: At baseline, the harm avoidance scores of the dysthymic subjects were approximately 1.5 standard deviations higher than those of a previously reported community sample. After treatment, there was a significant decrease in harm avoidance scores, with no significant between-group differences. Remission of dysthymia was associated with significantly greater improvement in harm avoidance, with the greatest numerical change found in the patients treated with sertraline. Subjects’ Tridimensional Personality Questionnaire scores were correlated at a 0.50 level with the Social Adjustment Scale both pre- and posttreatment, suggesting that a high degree of harm avoidance may be associated with poor social functioning. CONCLUSIONS: Before treatment, chronically depressed patients demonstrate an abnormality in temperament, as measured by elevated degrees of harm avoidance. Remission of dysthymia is associated with improvement in this aspect of temperament.
The psychosocial impairment of chronically depressed individuals has been amply demonstrated. The Medical Outcomes Study (1) demonstrated the high degree of functional disability associated with depression, reporting it to be equal to or greater than that for chronic medical conditions such as diabetes. Poor functioning was not only found among patients with identifiable major depression but also in those without an identifiable disorder but who had depressed mood. Research has shown that depression has a major impact on job performance and absenteeism (2). Clinical samples of patients with dysthymia have a disproportionally high frequency of single marital status (3), suggesting that chronic depression may interfere with the development of intimate relationships. A high incidence of axis II personality disorders, including those within cluster C (avoidant, dependent, and obsessive-compulsive), has also been noted (4). Hence, optimal treatment response for patients with dysthymia would include beneficial “personality” effects, along with relief of traditionally noted depressive symptoms such as reduced interest and energy levels, anhedonia, or somatic symptoms.
Despite the many studies on the efficacy of various antidepressant medications, there is a paucity of data about the effect of medication on personality. Psychopharmacology studies traditionally focus on symptom reduction; only a small minority have assessed psychosocial functioning. Even fewer have assessed the effect of successful antidepressant treatment on personality variables. Furthermore, existing studies refer primarily to the acute or episodic disorder of major depression. Yet personality is a concept related to enduring characteristics. In chronic axis I disorders, such as dysthymia or generalized anxiety disorder, disabling symptoms may have been present for decades before treatment; persistent depressive or anxious states may have become indistinguishable from personality traits. Dysthymia has been demonstrated to respond to antidepressant treatment in 50%–60% of patients (5–7). Does “personality” change in such patients? If so, in what ways?
Cloninger (8) proposed as a model of personality a “complex hierarchic system that can be naturally decomposed into distinct psychobiological dimensions of temperament and character.” Temperament consists of factors that are “independently heritable, manifest early in life, and involve preconceptual biases in perceptual memory and habit formation” (9). In Cloninger’s original model (8), temperament included three independent dimensions: harm avoidance, reward dependence, and novelty seeking. These dimensions were based on factors derived from the Tridimensional Personality Questionnaire, a 100-item self-report questionnaire normed on a national community sample of 1,019 individuals (10) with demonstrated adequate psychometric properties (8, 10). Subsequently, Cloninger et al. added a fourth dimension of temperament, persistence, which previously had been a subscale of reward dependence (9).
Svrakic et al. (11) related the Tridimensional Personality Questionnaire dimensions to various emotional traits. An individual with a high degree of harm avoidance would show emotional traits such as fearfulness, doubt, timidity, dismay, disgust, and fatigability, whereas someone with a low degree of harm avoidance would be relaxed, self-assured, bold, daring, dauntless, and vigorous. An individual with a high degree of reward dependence would be loving, sensitive, warm, dedicated, and depressed if separated, whereas someone with a low degree of reward dependence would appear unfriendly, insensitive, cool, irresolute, and indifferent if alone. A person scoring high on the novelty-seeking dimension would appear impulsive, quick-tempered, and disorderly, whereas a low degree of novelty seeking would indicate an individual who was reflective, stoical, and slow-tempered.
Studies of the Tridimensional Personality Questionnaire in clinical populations suggest that some temperamental factors vary depending on mood states. Patients with major depression have significantly higher harm avoidance scores than nondepressed comparison subjects at baseline (12), and scores for harm avoidance (and its factors shyness and fatigability) decrease significantly after 6 weeks of antidepressant treatment. Studies have shown a correlation between harm avoidance scores and changes in depression ratings (11, 13, 14). Research has found temperament type to be a strong predictor of antidepressant response (14–16). For instance, in a group of patients with unipolar depression, Joffe et al. (14) found that baseline harm avoidance scores were significantly lower in those who went on to show antidepressant response.
Previous reports (5–7) have suggested that tricyclic antidepressants and selective serotonin reuptake inhibitors (SSRIs) successfully treat dysthymic symptoms in 50% or more of patients and that psychosocial functioning (4, 17) may improve. A small study of Dunner et al. (18) found elevated harm avoidance scores in dysthymic patients that decreased after fluoxetine treatment but not after cognitive therapy. As a large, multicenter, prospective, placebo-controlled, double-blind study, this investigation offers the opportunity of assessing the effect of antidepressant treatment on temperamental factors.
In a group of patients with dysthymia, we tested the following hypotheses. First, we hypothesized that baseline scores on the Tridimensional Personality Questionnaire would be abnormal in the dysthymic patients (compared to those from a nonpsychiatric community sample); specifically, we expected to find elevated harm avoidance scores at baseline. We speculated that these higher harm avoidance scores would be greater in patients with comorbid axis II or anxiety disorders but also would be elevated in dysthymic patients without such comorbidity relative to the nonpsychiatric community sample. After treatment, we expected that remission of dysthymia would be associated with a decrease in harm avoidance score. In addition, we expected that temperament scores at baseline (e.g., initial harm avoidance, reward dependence) would be predictive of treatment response. Finally, we hypothesized that social functioning (as measured by the Social Adjustment Scale) would be associated with harm avoidance score at baseline and that improved social functioning after treatment would be associated with changes in harm avoidance score.
Method
Study Design
This report draws on data from a randomized, multicenter, double-blind, placebo-controlled parallel group study of sertraline, imipramine, and placebo in the treatment of early-onset dysthymia. More complete details regarding the study’s design have been reported elsewhere (7). Briefly, study inclusion criteria required a DSM-III-R diagnosis of early-onset dysthymia of at least 5 years’ duration (with the patient not having been without symptoms for more than 2 months at a time) as well as an initial score of 12 or higher on the 29-item Hamilton Depression Rating Scale, Seasonal Affective Disorders Version (19), at the end of a 1-week single-blind placebo washout. Exclusion criteria were major depression (current or within the preceding 6 months), pregnancy or lactation, history of drug or alcohol dependency or abuse within the preceding 6 months, serious risk of suicide, a current primary diagnosis of panic disorder or generalized anxiety disorder, and a lifetime diagnosis of bipolar disorder, obsessive-compulsive disorder, or any psychotic disorder. Patients who had failed to respond to two or more prior antidepressant trials were excluded, as were those who received a prior adequate trial of imipramine or previous sertraline treatment. Individuals who met the above criteria then provided written informed consent to participate in the study after having been provided a complete description of the study.
The study was conducted at 17 university-affiliated sites in the United States. The study protocol was approved by each site’s institutional review board. During the active treatment phase, subjects were randomly assigned to once-daily double-blind treatment with sertraline (beginning at 50 mg/day and titrated after weeks 4, 6, and 7 to a maximum of 200 mg/day); imipramine (beginning at 50 mg/day and titrated weekly to a maximum of 300 mg/day); or placebo. The dosage achieved at week 7 was continued through week 12. In order to maintain blind conditions, all patients received four identical capsules (which contained placebo, 50 mg of sertraline, or 50 or 100 mg of imipramine) for each day’s medication treatment. Dose increases were made (by 50-mg increments for both sertraline and imipramine) when patients had not yet responded to treatment and when there were no dose-limiting side effects.
Remission criteria were prospectively defined as 1) a score of 0 on item 1 of the Hamilton depression scale (depressed mood), and 2) the subject no longer meeting the DSM-III-R criteria for dysthymia (7).
Rating Instruments
Study ratings included both patient- and clinician-rated inventories. Axis I and II disorders were assessed with the Structured Clinical Interview for DSM-III-R—Patient Version (20) and the Structured Clinical Interview for DSM-III-R Personality Disorders (21). Clinician-rated instruments administered pre- and posttreatment included the Hamilton depression scale (22), the Longitudinal Interval Follow-Up Evaluation (23), the Montgomery-Åsberg Depression Rating Scale (24), the Clinical Global Impression (CGI) (25), and the Global Assessment of Functioning Scale (from DSM-IV). Patient-rated instruments included the Tridimensional Personality Questionnaire (8); the HSCL (26); SCL-90-R (27); the Social Adjustment Scale, self-rated version (28); the Inventory for Depressive Symptomatology (29); and the Quality of Life Enjoyment and Satisfaction Questionnaire (30). The Hamilton depression scale and the CGI were administered at each medication visit. All instruments were administered at baseline (week 0), before medication administration, and at the end of week 8 and week 12. For the week 12 assessments, including for the Tridimensional Personality Questionnaire, subjects were instructed to respond according to how their condition was during the preceding month (the questions on the standard Tridimensional Personality Questionnaire are not limited to a particular time period, since the scale was designed to measure enduring temperamental characteristics).
The Tridimensional Personality Questionnaire is a 100-item paper-and-pencil, true/false, self-rated inventory that takes approximately 15 minutes to complete. It assesses the personality dimensions of novelty seeking, harm avoidance, reward dependence, and persistence, which were defined by Cloninger et al.’s unified biosocial theory of personality (9). Cloninger et al. hypothesized that novelty seeking, harm avoidance, and reward dependence dimensions relate to the functioning of dopamine, serotonin, and norepinephrine, respectively. Normative values for this scale were established in a national sample of 1,019 respondents who completed the Tridimensional Personality Questionnaire as part of the 1987 General Social Survey (10). Scores were normally distributed, and the scales were minimally correlated with each other. There was an acceptable level of internal consistency of the scales and good test-retest correlations for the factors of reward dependence (0.70), novelty seeking (0.76), and harm avoidance (0.79) (10).
Statistical Methods
All longitudinal analyses were performed on the intent-to-treat patient population, i.e., the set of patients who were randomly assigned to treatment, received at least one dose of study drug, and had data from at least one follow-up visit. For patients who discontinued prematurely, their last nonmissing observations were carried forward to successive time points. In addition, study analyses were performed on the completer population, which was defined as those who completed 10 weeks of treatment (on the basis of data that have suggested this time period as an adequate therapeutic trial of medication [6]). Analyses of the completer population were examined for consistency with findings from the intent-to-treat population.
The Tridimensional Personality Questionnaire was scored according to the manual of Cloninger (31). If any questionnaire contained five or more missing item responses, the entire questionnaire was dropped from the analysis. For questionnaires missing one to four items, the subscale scores were computed on the basis of available data. No adjustment was made, since scores derived from the nonmissing items have essentially the same psychometric properties (reliability, validity) as scores from a questionnaire with complete data (1997 personal communication with T.R. Przybeck). Of 398 subjects, 46 (11.6%) had one (N=32), two (N=9), three (N=3), or four (N=2) missing items. These were fairly well balanced across treatment groups, so the potential for bias was minimal. Of note, the original Tridimensional Personality Questionnaire scale was revised by Cloninger et al., who added a fourth dimension of persistence, which had previously been a subscale of reward dependence (9).
Associations among categorical variables were assessed by using chi-square tests, while differences in continuous variables were examined by using t tests or linear models. Changes from baseline in Tridimensional Personality Questionnaire item scores were analyzed by using analysis of covariance (ANCOVA) models that included treatment group and remission status as main effects with the baseline measurement as covariate. If the ANCOVA assumption of homogeneity of slopes was not met, then changes from baseline in Tridimensional Personality Questionnaire item scores were analyzed by using ANCOVA models with separate slopes for each subgroup. Treatment group-by-remission status interactions were included in the first step of all models described above and checked for statistical significance; if the interactions were not significant at the 0.05 level, they were dropped from subsequent analyses. SAS version 6 software (SAS, Inc., Cary, N.C.) was used throughout, and type III sums of squares were used to test all hypotheses. Pair-wise comparisons in the linear models were made only if the overall F test was significant.
The analysis of predictors of remission was performed by using stepwise logistic regression, with a significance level of 0.05 to enter and to stay in the model. The dependent variable, remission, was as defined earlier. All statistical tests were two-sided, and statistical significance was declared at the p=0.01 level, which represents a Bonferroni correction based on the multiple tests that were performed.
Results
Patient Group Characteristics
Of the 618 patients who were screened for inclusion in the study, 202 failed to meet eligibility requirements or refused participation. Eligible patients were entered in a 1-week single-blind placebo washout phase. Among those 202 nonparticipants were 17 patients who were considered placebo responders at the end of the washout period and were discontinued from the study. Of the 416 patients randomly assigned to treatment, 412 received double-blind medication. The intent-to-treat sample for this study consisted of the 410 subjects (134 given sertraline, 136 given imipramine, and 140 given placebo) who had at least one postbaseline evaluation. Table 1 shows demographic and clinical data of the study population. Of the initial 410 subjects, 381 had a classifiable remission status (remission: 40.9% [N=156]; no remission: 59.1% [N=225]), and 355 were classifiable for remission and also had Tridimensional Personality Questionnaire data available. Remission rates of patients given sertraline (50.0%, N=63 of 126) and imipramine (45.2%, N=57 of 126) were significantly higher than for those given placebo (27.9%, N=36 of 129) (sertraline versus placebo:χ2=12.87, df=1, p<0.05; imipramine versus placebo:χ2=7.86, df=1, p<0.05). The dropout rate for patients given sertraline (16%) was significantly lower than that of those given placebo (24%) and imipramine (33%) (χ2=11.2, df=2, p=0.004) (7).
Baseline scores on the Tridimensional Personality Questionnaire compared to population norms (10) are shown in Table 2. These indicate that the mean harm avoidance score for this group of dysthymic patients was approximately 1.5 standard deviations above the mean of a community population. Scores on the other factors were more similar to the means of the community sample. Of note is that harm avoidance scores for men and women did not differ in the dysthymic patient group, whereas Cloninger et al.’s community sample showed higher scores among women (which may reflect gender differences in the prevalence of depression).
At baseline, 269 (65.6%) of the subjects were diagnosed as having a comorbid axis II disorder, whereas 137 (33.4%) had no diagnosed axis II disorder. Patients with an axis II disorder showed significantly higher baseline harm avoidance scores than did those without an axis II diagnosis (mean=23.0 [SD=5.7] versus mean=19.7 [SD=5.9], respectively; t=–5.32, df=395, p<0.0001) as well as lower reward dependence scores (mean=11.5 [SD=4.1] versus mean=12.7 [SD=4.3]; t=2.86, df=395, p=0.005). No differences were seen for novelty seeking or persistence scores. Of the 269 subjects with a comorbid axis II disorder, 168 had diagnoses from cluster A (N=9), cluster B (N=16), or cluster C (N=143) only. Baseline harm avoidance scores differed among the axis II clusters (cluster A: mean=21.3, SD=4.2; cluster B: mean=19.0, SD=6.7; cluster C: mean=23.3, SD=6.0), with a significant difference between cluster B and cluster C (t=2.72, df=157, p=0.007).
There were 116 (28.3%) subjects who met the DSM-III-R criteria for a secondary anxiety disorder at baseline (including generalized anxiety disorder, social phobia, or panic disorder). Baseline harm avoidance scores for the dysthymic patients with an anxiety disorder were significantly higher than those of patients without an anxiety disorder (mean=23.6 [SD=5.7] versus mean=21.2 [SD=5.9], respectively; t=–3.79, df=399, p=0.0002). However, the baseline presence of an anxiety disorder was not associated with remission after treatment, as 47.6% (N=39 of 82) of those with an anxiety disorder and 48.1% (N=113 of 235) of those without an anxiety disorder experienced a remission from dysthymia.
Changes in Personality Dimensions
Impact of treatment
We present here results of the intent-to-treat analyses. Although results from the completer population are not presented here, they were similar to the findings observed with the intent-to-treat patient population. Since dropouts, who tend to have higher depression scores, might skew findings between groups, the completer population analyses provided a confirmation that findings were not a result of differential dropout rates observed for the three treatments in this study. The assumption of homogeneity of slopes was violated for novelty seeking and reward dependence; therefore, ANCOVA models with separate slopes for each subgroup were used for analyses.
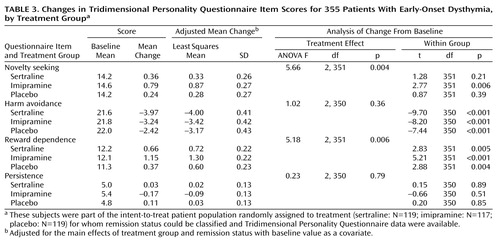
Table 3 presents the changes in Tridimensional Personality Questionnaire item scores by treatment group (sertraline, imipramine, placebo). A significant decrease in harm avoidance scores was seen at 12 weeks in all treatment groups with no between-group differences. The overall F statistic was significant for novelty seeking and reward dependence, indicating a treatment effect, although pair-wise comparisons were not significant. There was a significant increase in novelty seeking scores for the imipramine-treated group only and significant increases in reward dependence scores for all three groups. There was no change in persistence for any of the three treatment groups.
Impact of remission
Table 4 presents the changes in Tridimensional Personality Questionnaire item scores by remission status, with treatment included in the model. Both remitters and nonremitters demonstrated within-group improvement in harm avoidance scores, with significantly more improvement among remitters. Reward dependence showed improvement for remitters with significantly more improvement than among nonremitters. The increase in novelty seeking for both remitters and nonremitters was not significant at the 0.01 level; there was no between-group difference.
Impact of treatment, remission, and their interaction
Table 5 presents a continuation of these analyses by remitter status and treatment type. Significant remission effects were found for harm avoidance and reward dependence, but there were no significant treatment or remission-by-treatment interactions. The greatest change in harm avoidance (–6.43) was among sertraline-treated remitters, and the greatest change in reward dependence (2.30) was among imipramine-treated remitters.
Harm Avoidance
Impact of treatment type
In a further analysis, we calculated the baseline scores for the four harm avoidance subscales (11) and the impact of treatment on them. Significant changes were found only among female subjects. The greatest improvements were seen on the harm avoidance subscale “anticipatory worry versus uninhibited optimism” (sertraline: –1.90 points, imipramine: –1.25, and placebo: –0.65) (F=7.26, df=2, 226, p=0.0009). There were decreases on the harm avoidance subscales “fear of uncertainty versus confidence” and “shyness with strangers versus gregariousness” (sertraline: –0.74 and –0.86, respectively; imipramine: –0.21 and –0.37; and placebo: –0.39 and –0.33), but the changes were not statistically significant. There was no overall treatment effect on the harm avoidance subscale “fatigability and asthenia versus vigor.” Analyses that used pair-wise comparisons between treatment groups demonstrated gender and treatment differences. For example, for “anticipatory worry versus uninhibited optimism,” sertraline-treated women had significantly more improvement than placebo-treated women (t=–3.81, df=151, p=0.0002), and sertraline was superior to imipramine for “fear of uncertainty versus confidence” (t=–2.66, df=153, p=0.008). Men on the other hand did not demonstrate differences in any harm avoidance factor.
Operationalizing a concept of “harm avoidance response.”
Considering that this group of patients with dysthymia had a mean baseline score for harm avoidance approximately 1.5 standard deviations above the mean score of a large community sample and that high harm avoidance scores have been associated with significant psychopathology, we believe it would be clinically valuable to determine whether treatment led to significant improvement in this dimension. Studies on samples of depressed patients commonly define treatment responders or nonresponders on the Hamilton depression scale on the basis of criteria such as a 50% drop from baseline value or a final score of 7 or lower. In an exploratory analysis, we defined harm avoidance response as a decrease of at least one standard deviation in harm avoidance from the baseline score after treatment. According to this definition, there were 98 “harm avoidance responders” (27.5%) and 259 nonresponders (72.5%). Harm avoidance response rates were 35.8% (N=43 of 120) for sertraline, 29.1% (N=34 of 117) for imipramine, and 17.5% (N=21 of 120) for placebo (overall χ2=10.35, df=2, p=0.006). Significantly more sertraline-treated subjects were harm avoidance responders than placebo-treated subjects (sertraline versus placebo: χ2=10.31, df=1, p=0.001). A sensitivity analysis was then performed, in which the criteria for harm avoidance response were varied between 0.8 and 1.2 standard deviations of baseline score. Active medication was associated with a significantly higher degree of harm avoidance response at levels from 0.9 to 1.2 standard deviations.
Social Functioning and Predictors of Remission
We hypothesized an association between social adjustment and harm avoidance in dysthymic patients both pre- and posttreatment. At baseline, data showed a correlation between Social Adjustment Scale scores (mean=2.3, SD=0.4) and harm avoidance scores (mean=21.9, SD=6.0) (r=0.46, df=399, p<0.001). After treatment, correlations were seen between Social Adjustment Scale and harm avoidance scale scores for both those who remitted (mean=1.7 [SD=0.3] and 15.7 [SD=6.5], respectively; r=0.46, df=147, p<0.001) and those who did not (mean=2.2 [SD=0.5] and 20.7 [SD=6.1]; r=0.54, df=209, p<0.001).
Tridimensional Personality Questionnaire factors were analyzed as univariate predictors of remission (among the 373 subjects on whom there were baseline Tridimensional Personality Questionnaire data), with the finding that baseline harm avoidance scores were associated with remission (for remitters: mean=20.8, SD=6.4; for nonremitters: mean=22.6, SD=5.5) (t=2.70, df=289, p=0.01, Satterthwaite’s approximation). Thus, lower baseline harm avoidance scores were associated with achieving remission by week 12.
However, when we performed a logistic regression in order to determine which pretreatment factors might predict treatment remission, harm avoidance was no longer predictive of remission. The regression included the following factors: baseline total scores for the Tridimensional Personality Questionnaire items of 1) novelty seeking, 2) harm avoidance, 3) reward dependence, and 4) persistence; 5) any active treatment (i.e., sertraline or imipramine) versus placebo; 6) age; 7) sex; 8) family oriented (married or cohabiting versus single); 9) employed (yes or no); 10) education; 11) Global Assessment of Functioning score at baseline; 12) Quality of Life total score at baseline; and 13) Social Adjustment Scale total score at baseline. The final three factors were derived from the Longitudinal Interval Follow-Up Evaluation: 14) patients’ baseline rating of social adjustment in preceding month, 15) clinician’s baseline rating of social adjustment in preceding month, and 16) overall level of satisfaction in preceding month. In this predictive model, active treatment entered the model first, and Social Adjustment Scale total score entered the model next. Harm avoidance was no longer significantly predictive of remission (perhaps because Social Adjustment Scale and harm avoidance scores were so highly correlated). However, if the logistic regression was performed without the Social Adjustment Scale, then harm avoidance entered the model; that is, although initial harm avoidance is predictive of treatment response, harm avoidance does not explain an independent (or additional) amount of variance beyond the Social Adjustment Scale score.
Discussion
This study focused on the pre- and posttreatment Tridimensional Personality Questionnaire scores of 410 patients with early-onset dysthymia of at least 5 years’ duration who were randomly assigned to 12 weeks of treatment with sertraline, imipramine, or placebo. Overall treatment results have been reported (7) as well as the impact of treatment on psychosocial functioning (4). Our current study demonstrated significant baseline abnormalities of temperament in this large group of patients with early-onset dysthymia. Specifically, these patients had high harm avoidance scores before antidepressant treatment. The magnitude of this elevation (approximately 1.5 standard deviations) is notable. However, this elevation does not appear to be diagnosis-specific; it is comparable to findings in other disorders, such as major depression (mean pretreatment harm avoidance score=23.2, SD=6.7) (16) and bulimia (mean pretreatment harm avoidance score=22.3, SD=7.4, among a hospitalized sample) (32). Besides the elevation in harm avoidance scores, the Tridimensional Personality Questionnaire profile for dysthymia appears to include normal novelty seeking and persistence scores and possibly decreased reward dependence. It is possible that among patients with a variety of axis I and II disorders, high harm avoidance scores could be conceptualized as a common underlying (or comorbid) state that itself might benefit from treatment.
Although comorbid anxiety disorders or axis II diagnoses had an impact on baseline Tridimensional Personality Questionnaire scale scores, these differences were small, and dysthymic patients without these disorders still had elevated harm avoidance scores when compared to those from a community sample (10). Cloninger (8) noted that there are characteristic profiles of Tridimensional Personality Questionnaire scale scores for different psychiatric disorders, both axis I and II. Current findings suggest that one important aspect of temperament is related to affective state and that if mood is abnormal for an extended time, personality (at least as measured by the Tridimensional Personality Questionnaire) may be adversely affected.
After treatment, varying degrees of change occurred in the temperamental factors harm avoidance, novelty seeking, and reward dependence. These changes varied by treatment. For instance, the changes in harm avoidance for the placebo condition may represent an effect of attention or may reflect lability in this factor, perhaps influenced by current depressive severity or by the psychosocial environment. This may be in itself clinically important. Individuals with fluctuating (and high) levels of harm avoidance may have difficulty maintaining job performance and sustaining interpersonal relationships.
Harm avoidance scores decreased to a significantly greater degree when remission occurred than when remission did not occur. Conversely, reward dependence increased when remission was achieved. On a clinical level, an individual with a high degree of harm avoidance would be described as fearful, doubting, and timid, and an individual with a low degree of reward dependence would be described as unfriendly, insensitive, cool, and indifferent if alone (11). Changes in these factors may lead to “personality” alterations observable to the individual in treatment and others in the social environment. A less fearful, less unfriendly, more sensitive individual may be expected to accomplish more and interact better with others than one who is timid and insensitive, and social functioning may thus improve.
Cloninger (8) hypothesized that the factors of the Tridimensional Personality Questionnaire are related to the activity of different neurotransmitters: serotonin (harm avoidance), dopamine (novelty seeking), and norepinephrine (reward dependence). It is possible that treatment with various pharmacological agents (with different neurotransmitter activities) will lead to different temperamental changes. In this study, there were no posttreatment between-group differences in the intent-to-treat sample. In the completer population sample, imipramine-treated subjects showed significantly more change on reward dependence than those treated with sertraline or placebo; imipramine has significant noradrenergic activity (particularly through its metabolite desipramine), which may explain this difference. Findings on the harm avoidance subscales suggest the possibility of more subtle “personality” changes from different treatments, which may additionally vary by gender; the neurochemical etiology of such changes remains to be elucidated.
Also, in our exploratory analysis, subjects treated with sertraline and imipramine showed a significantly higher rate of “harm avoidance response” (drop of one or more standard deviations in harm avoidance score from baseline) than the placebo-treated subjects. A sensitivity analysis demonstrated that this finding was fairly robust, being present from 0.9 to 1.2 standard deviations of change (although not at 0.8 standard deviation). The harm avoidance response analysis suggests that there may, in fact, be posttreatment harm avoidance differences between treatments that the ANCOVA did not detect. The failure to find a difference may be a result of poor signal detection or inadequate power rather than a lack of difference between treatments. It appears that harm avoidance scores improve when depression remits. While medication leads to a greater degree of remission of depression than placebo, harm avoidance scores also decreased in placebo responders, so it may be difficult to show medication effects.
The high baseline correlation between the Tridimensional Personality Questionnaire harm avoidance scores and Social Adjustment Scale scores is also notable in that abnormal “personality” factors may contribute to the poor baseline psychosocial functioning often found in dysthymic disorder. The correlation between harm avoidance and Social Adjustment Scale scores after treatment suggests that harm avoidance may be a risk factor for continued poor functioning, regardless of concurrent depressive symptoms (in the clinical setting, psychiatrists often encounter patients whose depression is in remission but who remain socially avoidant and risk-averse). In a univariate analysis, high harm avoidance scores predicted nonremission of depression, which is consistent with results from other studies (14–16). As such, our findings raise questions regarding the relationship among three factors: mood disorder (dysthymia), personality traits (harm avoidance), and psychosocial functioning (as measured by the Social Adjustment Scale). Is a high degree of harm avoidance a trait that predisposes to the development of chronic depression, perhaps beginning from childhood or adolescence? Or is it perhaps a result of chronic dysphoria or demoralization? Alternatively, a high degree of harm avoidance may be a mediating factor that contributes both to poor psychosocial functioning and to the development of axis I mood disorders and might play a crucial intermediary role between symptoms and psychosocial functioning. Of note, in the Medical Outcomes Study (1), dysthymic patients demonstrated increasing psychosocial impairment at 2-year follow-up, consistent with an increasing constriction of their lives over time; one can only speculate about the role of elevated harm avoidance in this phenomenon.
The findings of this study are limited by a number of factors. On a theoretical level, one might question the validity of distinctions between mood disorder, temperament, and psychosocial functioning or between DSM-IV’s axes I, II, and V. Stewart et al. (33) have delineated items on the Social Adjustment Scale that they believe to measure affective dimensions. It is similarly possible that harm avoidance may measure depression, although it is labeled as an aspect of temperament. Some aspects generally ascribed to axis II disorders may be uninterpretable in the face of axis I pathology. It may be difficult to define experiments that will definitively clarify these issues.
On a pragmatic level, only one measure of personality variables (the Tridimensional Personality Questionnaire) was used to measure personality change, whereas a comprehensive assessment of the impact of antidepressants on personality in dysthymia would require multiple measures. Only temperament, and not character, was measured; Cloninger et al.’s more recent scale, the Temperament and Character Inventory (9), assesses both areas. Also, although shown to have high test-retest reliability (34), the Tridimensional Personality Questionnaire has not been systematically studied as a repeated measure, as used in this study. In order to measure change, the study required use of the Tridimensional Personality Questionnaire for a 1-month time window. Furthermore, the duration of treatment (12 weeks) was brief in comparison to the subjects’ many years of chronic depression (mean=30 years, SD=11); patients may require longer treatment in order to achieve remission of dysthymia or a change in temperament scores. Data collected in a 9-month continuation phase of the current study may clarify some of these issues.
Conclusions
The data from this study suggest that for many dysthymic patients, remission of depression may be associated with changes in the temperamental aspect of personality (9). The changes observed include partial normalization of temperamental abnormalities (such as overall harm avoidance score, harm avoidance subscale scores, and reward dependence). Similar normalization of personality variables was found in a recent study of SSRI medicines in outpatients with major depression (35). Such findings raise questions about the boundaries between axis I and axis II diagnoses. We believe that these changes do not represent what has been referred to in the popular literature (36) as “cosmetic psychopharmacology” but instead represent an important aspect of achieving remission of a debilitating disorder. In the future, effective treatment of mood disorders may require not only symptom remission and improved social functioning but also the correction of depression-induced personality abnormalities (35, 37–39). It is of interest that in this study, the specific treatment-induced personality changes appear to vary depending on medication type and gender. This suggests the potential benefit of more systematic research on medication effects on temperament and the possibility that specific temperamental abnormalities might eventually be treated effectively with highly targeted psychotropic medications.
 |
 |
 |
 |
 |
Presented in part at the 151st annual meeting of the American Psychiatric Association, Toronto, May 30–June 4, 1998, and the 36th annual meeting of the American College of Neuropsychopharmacology, Kamuela, Hawaii, Dec. 8–12, 1997. Received Dec. 29, 1998; revisions received Aug. 17, 1999, and Feb. 15, 2000; accepted March 8, 2000. From Beth Israel Medical Center. Address reprint requests to Dr. Hellerstein, Outpatient Mental Health Services, Beth Israel Medical Center, First Avenue and 16th St., New York, NY 10003; dhellerstein@ bethisraelny.org (e-mail). Supported by a series of grants from Pfizer Inc, New York.
1. Wells KB, Stewart A, Hays RD, Burnam MA, Rogers W, Daniels M, Berry S, Greenfield S, Ware J: The functioning and well-being of depressed patients: results from the Medical Outcomes Study. JAMA 1989; 262:914–919Crossref, Medline, Google Scholar
2. Broadhead WE, Blazer DJ, George LK, Tse CK: Depression, disability days, and days lost from working: a prospective epidemiological survey. JAMA 1990; 264:2524–2538Google Scholar
3. Friedman RA: Social impairment in dysthymia. Psychiatr Annals 1993; 23:632–637Crossref, Google Scholar
4. Kocsis JH, Zisook S, Davidson J, Shelton R, Yonkers K, Hellerstein DJ, Rosenbaum J, Halbreich U: Double-blind comparison of sertraline, imipramine, and placebo in the treatment of dysthymia: psychosocial outcomes. Am J Psychiatry 1997; 154:390–395Link, Google Scholar
5. Kocsis JH, Frances AJ, Voss CB, Mann JJ, Mason BJ, Sweeney J: Imipramine for treatment of chronic depression. Arch Gen Psychiatry 1988; 45:253–257Crossref, Medline, Google Scholar
6. Hellerstein DJ, Yanowitch P, Rosenthal J, Samstag LW, Maurer M, Kasch K, Burrows L, Poster M, Cantillon M, Winston A: A randomized double-blind study of fluoxetine versus placebo in treatment of dysthymia. Am J Psychiatry 1993; 150:1169–1175Google Scholar
7. Thase ME, Fava M, Halbreich U, Kocsis JH, Koran L, Davidson J, Rosenbaum J, Harrison W: A placebo-controlled, randomized clinical trial comparing sertraline and imipramine for the treatment of dysthymia. Arch Gen Psychiatry 1996; 53:777–784Crossref, Medline, Google Scholar
8. Cloninger CR: A systematic method for clinical description and classification of personality variants. Arch Gen Psychiatry 1987; 44:573–588Crossref, Medline, Google Scholar
9. Cloninger CR, Svrakic DM, Przybeck TR: A psychobiological model of temperament and character. Arch Gen Psychiatry 1993; 50:975–990Crossref, Medline, Google Scholar
10. Cloninger CR, Przybeck TR, Svrakic DM: The Tridimensional Personality Questionnaire: US normative data. Psychol Rep 1991; 69:1047–1057Google Scholar
11. Svrakic DM, Przybeck TR, Cloninger CR: Mood states and personality traits. J Affect Disord 1992; 24:217–226Crossref, Medline, Google Scholar
12. Mulder RT, Joyce PR: Relationships of the Tridimensional Personality Questionnaire to mood and personality measures for depressed patients. Psychol Rep 1994; 75:1315–1325Google Scholar
13. Strakowski SM, Dunayevich E, Keck PE Jr, McElroy SL: Affective state dependence of the Tridimensional Personality Questionnaire. Psychiatry Res 1995; 57:209–214Crossref, Medline, Google Scholar
14. Joffe RT, Bagby RM, Levitt AJ, Regan JJ, Parker JDA: The Tridimensional Personality Questionnaire in major depression. Am J Psychiatry 1993; 150:959–960Link, Google Scholar
15. Nelson EC, Cloninger CR: The Tridimensional Personality Questionnaire as a predictor of response to nefazodone treatment of depression. J Affect Disord 1995; 35:51–57Crossref, Medline, Google Scholar
16. Joyce PR, Mulder RT, Cloninger CR: Temperament predicts clomipramine and desipramine response in major depression. J Affect Disord 1994; 30:35–46Crossref, Medline, Google Scholar
17. Kocsis JH, Sutton BM, Frances AJ: Long-term follow-up of chronic depression treated with imipramine. J Clin Psychiatry 1991; 52:56–59Medline, Google Scholar
18. Dunner DL, Schmaling KB, Hendrickson H, Becker J, Lehman A, Bea C: Cognitive therapy versus fluoxetine in the treatment of dysthymic disorder. Depression 1996; 4:34–41Crossref, Medline, Google Scholar
19. Williams JBW, Link MJ, Rosenthal NE, Amira L, Terman M: Structured Interview Guide for the Hamilton Depression Rating Scale, Seasonal Affective Disorders Version (SIGH-SAD), revised ed. New York, New York State Psychiatric Institute, 1994Google Scholar
20. Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-III-R—Patient Version (SCID-P). New York, New York State Psychiatric Institute, Biometrics Research, 1988Google Scholar
21. Spitzer RL, Williams JBW, Gibbon M: Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II). New York, New York State Psychiatric Institute, Biometrics Research, 1987Google Scholar
22. Hamilton M: A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23:56–62Crossref, Medline, Google Scholar
23. Shapiro R, Keller M: Longitudinal Interval Follow-Up Evaluation (LIFE). Boston, Lindemann Mental Health Center, 1979Google Scholar
24. Montgomery SA, Åsberg M: A new depression scale designed to be sensitive to change. Br J Psychiatry 1979; 134:382–389Crossref, Medline, Google Scholar
25. Guy W (ed): ECDEU Assessment Manual for Psychopharmacology: Publication ADM 76-338. Washington, DC, US Department of Health, Education, and Welfare, 1976, pp 218–222Google Scholar
26. Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L: The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci 1974; 19:1–15Crossref, Medline, Google Scholar
27. Derogatis LR: SCL-90-R: Administration, Scoring, and Procedures Manual, II. Towson, Md, Clinical Psychometric Research, 1983Google Scholar
28. Weissman MM, Bothwell S: Assessment of social adjustment by patient self-report. Arch Gen Psychiatry 1976; 33:1111–1115Google Scholar
29. Rush AJ, Giles DE, Schlesser MA, Fulton CL, Weissenberger J, Burns C: The Inventory for Depressive Symptomatology (IDS): preliminary findings. Psychiatry Res 1986; 18:65–87Crossref, Medline, Google Scholar
30. Endicott J, Nee J, Harrison W, Blumenthal R: Quality of Life Enjoyment and Satisfaction Questionnaire: a new measure. Psychopharmacol Bull 1993; 29:321–326Medline, Google Scholar
31. Cloninger CR: The Tridimensional Personality Questionnaire, Version IV. St. Louis, Washington University School of Medicine, Department of Psychiatry, 1987Google Scholar
32. Kleifeld EI, Sunday S, Hurt S, Halmi KA: The effects of depression and treatment on the Tridimensional Personality Questionnaire. Biol Psychiatry 1994; 36:68–70Crossref, Medline, Google Scholar
33. Stewart JW, Quitkin FM, McGrath PJ, Rabkin JG, Markowitz JS, Tricamo E, Klein DF: Social functioning in chronic depression: effect of 6 weeks of antidepressant treatment. Psychiatry Res 1988; 25:213–222Crossref, Medline, Google Scholar
34. Brown SL, Svrakic DM, Przybeck TR, Cloninger CR: The relationship of personality to mood and anxiety states: a dimensional approach. J Psychiatr Res 1992; 26:197–211Crossref, Medline, Google Scholar
35. Ekselius L, von Knorring L: Change in personality traits during treatment with sertraline or citalopram. Br J Psychiatry 1999; 174:444–448Crossref, Medline, Google Scholar
36. Kramer P: Listening to Prozac. New York, Viking Press, 1993Google Scholar
37. Black KJ, Sheline YI: Personality disorder scores improve with effective pharmacotherapy of depression. J Affect Disord 1997; 43:11–18Crossref, Medline, Google Scholar
38. Goldman RG, Skodol AE, McGrath PJ, Oldham JM: Relationship between the Tridimensional Personality Questionnaire and DSM-III-R personality traits. Am J Psychiatry 1994; 151:274–276Link, Google Scholar
39. Thayer RE: The Biopsychology of Mood and Arousal. New York, Oxford University Press, 1989Google Scholar



