Evaluation of Bipolar Disorder in Inpatients With Prelingual Deafness
Abstract
OBJECTIVE: This study retrospectively examined the occurrence of bipolar disorder in patients with prelingual deafness who were hospitalized for a psychiatric disorder. METHOD: The hospital charts since 1983 of all psychiatrically admitted deaf patients were retrospectively evaluated for diagnoses by using DSM-IV criteria. Those with a best-estimate diagnosis of bipolar disorder were compared to those with other diagnoses. RESULTS: There were 28 patients with prelingual deafness who had at least one psychiatric diagnosis from 1983 to 1998. Upon chart review, 11 (39.3%) were diagnosed with bipolar disorder. Patients with bipolar disorder and deafness had rates of inaccurate discharge diagnoses that were similar to those of other deaf patients (70.8% versus 56.7%). CONCLUSIONS: Bipolar disorder may be more common in inpatients with prelingual deafness than has been previously described in the literature. Further research regarding the sources contributing to misdiagnosis of psychiatric disorders in this population is warranted.
The literature regarding prelingual deafness (occurring before age 3) and bipolar disorder is sparse. In 1984, Markowitz and Nininger (1) published a case report describing a teenager with congenital deafness who presented with a first manic episode. In 1971, Altshuler (2) reported that in the 15 years of his experience in the New York state system with deaf patients, “there has been only one truly depressive episode followed by a manic phase.” Most recently, Haskins (3) reviewed the charts of 54 inpatients with psychosis and deafness and found five (9.3%) with bipolar disorder.
Several factors may contribute to the lack of reported bipolar disorder in individuals with prelingual deafness. First, it is possible that overemphasis of overt behavioral manifestations of manic psychosis may lead to a diagnosis of schizophrenia instead of bipolar disorder (4). Second, there are many potential pitfalls in diagnosing and treating deaf patients, including lack of and utilization of experienced interpreters, grammatical and syntactic translation problems between American Sign Language and English, and differences in how a deaf individual displays feelings and perceives mental health and the mental health community (5–9). To better understand the frequency and presentation of bipolar disorder in deaf individuals, we conducted a retrospective diagnostic survey of deaf psychiatric inpatients at our center. We hypothesized that bipolar disorder occurs in deaf patients more often than previously reported.
METHOD
The charts of all identified deaf psychiatric inpatients at the University of Cincinnati Hospital during the last 15 years (1983 to 1998) were evaluated by a psychiatrist (M.P.D.) who was blind to the patients’ diagnoses and the hypothesis of the study. The charts had all references to diagnoses redacted, and the blind reviewer followed a forced-diagnosis format whereby all patients ultimately received the DSM-IV axis I diagnoses that most closely matched their symptoms and history. The blind reviewer used strict DSM-IV criteria. After the charts had been reviewed, two additional psychiatrists (N.A.S., T.D.G.) reevaluated the charts to critically evaluate all diagnoses given by the blind reviewer. All of the deaf patients whose charts were reviewed had the same experienced interpreter involved in their treatment. Since there was one patient with definite postlingual deafness and one patient with probable postlingual deafness, the diagnostic data from these patients were excluded from the analyses.
RESULTS
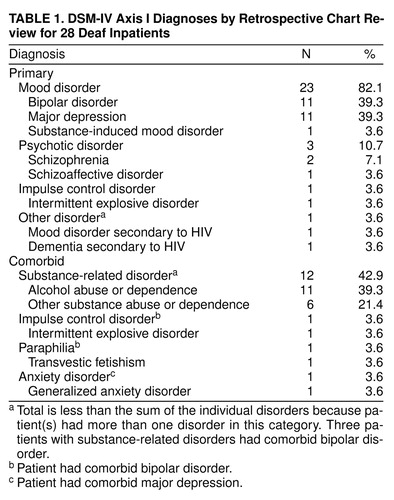
The blind reviewer’s diagnoses of the 28 patients with prelingual deafness were judged to be accurate by the additional reviewing psychiatrists (N.A.S., T.D.G.) in all cases (kappa=0.85). As shown in Table 1, the retrospective survey of charts of 28 patients with prelingual deafness revealed 11 (39.3%) who met the diagnostic criteria for bipolar disorder, 11 (39.3%) with major depressive disorder, two (7.1%) with schizophrenia; and one (3.6%) each with schizoaffective disorder, intermittent explosive disorder, substance-induced mood disorder, and mood disorder and dementia secondary to HIV. Twelve patients (42.9%) had comorbid lifetime substance-related disorders; three of these also had bipolar disorder. One patient who had bipolar disorder also had transvestic fetishism and intermittent explosive disorder. Additionally, one patient with major depression had generalized anxiety disorder. Eight (72.7%) of 11 patients currently diagnosed with bipolar disorder were men, and eight (47.1%) of 17 patients with other diagnoses were men. The cause of deafness was known in eight of 11 patients diagnosed with bipolar disorder; five had congenital deafness, and three were deaf from postnatal causes such as head trauma and infection. The known cause of deafness was congenital in 12 of 17 patients with other diagnoses.
Original discharge diagnoses varied for each patient and were often different from the retrospective diagnoses derived from DSM-IV criteria. Discrepant discharge diagnoses for each hospitalization occurred at similar rates in deaf bipolar patients and in other deaf patients (70.8% versus 56.7%) (χ2=1.15, df=1, p=0.28). The 11 patients diagnosed with bipolar disorder in this study were hospitalized 24 times at University Hospital (mean=2.2, SD=1.5, for each patient) and diagnosed at discharge with bipolar disorder only seven times (29.2%). The most common discrepant discharge diagnoses were psychosis (25%, N=6), schizoaffective disorder (16.7%, N=4), and intermittent explosive disorder (8.3%, N=2). The 17 patients diagnosed with other disorders were hospitalized 30 times (mean=1.8, SD=0.8, for each patient), and discharge diagnoses were consistent with retrospective diagnoses only 13 times (43.3%). The most common discrepant discharge diagnoses were psychosis (16.6%, N=5), adjustment disorder (10.0%, N=3), and schizophrenia (6.7%, N=2). In nine of 11 of the hospitalizations during which the diagnosis of “psychosis” was given at discharge, patients had a clear-cut mood disorder (bipolar or major depression).
For individual patients, there was no evidence of greater diagnostic precision with multiple hospitalizations in the bipolar group or in the nonbipolar group (p=0.74 and p=0.74, respectively, Fisher’s exact test). Two of the deaf patients committed suicide. Both had retrospective diagnoses of bipolar disorder; neither received this diagnosis at discharge from any of their combined three hospitalizations.
DISCUSSION
This study provides preliminary evidence that mood disorders and, in particular, bipolar disorder in the patients with prelingual deafness are common and frequently underdiagnosed. Other psychiatric disorders also appeared to be misdiagnosed. The major limitations of this study are its small size, its retrospective nature, and the fact that DSM-IV criteria have only been available since 1994. However, it is important to note that the diagnoses of the blind reviewer were believed to be accurate by the additional reviewing psychiatrists in all cases; patients generally had clear-cut diagnoses.
Inpatients with prelingual deafness and bipolar disorder often appeared to have changes in their signing behavior (such as rapid signing or flights of ideas displayed with their hands). These gesticulations were often seen solely as psychotic behaviors and not as a change in mood by clinicians, although patients also frequently exhibited multiple symptoms of bipolar disorder (e.g., grandiosity, lack of sleep, distractibility) that were documented with the help of the interpreter and observations from the inpatient staff. Clinicians appeared to place more diagnostic emphasis on how the patient appeared than on other documented symptoms and collateral information. The accuracy of diagnosing bipolar disorder and other disorders did not improve with multiple hospitalizations of the same patient.
The results of this study suggest that a careful psychiatric evaluation of patients with prelingual deafness, including a critical evaluation of each patient’s symptoms by using interpreters and collateral information, is important in the diagnosis of these individuals. Further research using cross-sectional, prospective, structured clinical interviews to accurately assess DSM-IV diagnoses in individuals with prelingual deafness appears warranted.
Received Sept. 3, 1998; revision received Dec. 28, 1998; accepted Feb. 4, 1999. From the Department of Psychiatry, University of Cincinnati College of Medicine. Address reprint requests to Dr. Shapira, Department of Psychiatry, University of Florida Brain Institute, 100 Newell Dr., Suite L4-100, Gainesville, FL 32611, [email protected] (e-mail). The authors thank Abbott Laboratories for the unrestricted educational grant that supported this research.
 |
1. Markowitz JC, Nininger JE: A case report of mania and congenital deafness. Am J Psychiatry 1984; 141:894–895Link, Google Scholar
2. Altshuler KZ: Studies of the deaf: relevance to psychiatric theory. Am J Psychiatry 1971; 127:1521–1526Google Scholar
3. Haskins BG: Clinical features of psychosis in deaf adults, in 1998 Annual Meeting New Research Program and Abstracts. Washington, DC, American Psychiatric Association, 1998, p 165Google Scholar
4. Pope HJ Jr, Lipinski JF Jr: Diagnosis in schizophrenia and manic-depressive illness: a reassessment of the specificity of “schizophrenic” symptoms in the light of current research. Arch Gen Psychiatry 1978; 35:811–828Crossref, Medline, Google Scholar
5. Elliot E, Glass L, Evans JW: Mental Health Assessment of Deaf Clients: A Practical Manual. Boston, College-Hill Press, 1987Google Scholar
6. Steinberg AG, Sullivan VJ, Loew RC: Cultural and linguistic barriers to mental health service access: the deaf consumer’s perspective. Am J Psychiatry 1998; 155:982–984Link, Google Scholar
7. Ebert DA, Heckerling PS: Communication with deaf patients: knowledge, beliefs, and practices of physicians. JAMA 1995; 273:227–229Crossref, Medline, Google Scholar
8. McEwen E, Anton-Culver H: The medical communication of deaf patients. J Fam Pract 1988; 26:289–291Medline, Google Scholar
9. Lass LG, Franklin RR, Bertrand WE, Baker J: Health knowledge, attitudes, and practices of the deaf population in greater New Orleans: a pilot study. Am Ann Deaf 1978; 123:960–967Medline, Google Scholar



